Published online Mar 16, 2021. doi: 10.12998/wjcc.v9.i8.1989
Peer-review started: November 16, 2020
First decision: December 24, 2020
Revised: January 5, 2021
Accepted: January 8, 2021
Article in press: January 8, 2021
Published online: March 16, 2021
Processing time: 104 Days and 21 Hours
Laryngeal contact granuloma (LCG) is difficult to treat and frequently associated with high persistence and recurrence, despite the availability of both surgical and pharmacological treatment options. An appropriate strategy is therefore needed to help patients with multiple recurrences of LCG to potentially avoid unnecess-ary surgery.
We describe the case of a 34-year-old male patient with recurrent LCG in which a good response was achieved through successful management of laryngophar-yngeal reflux disease using a combination pharmacotherapeutic regimen consisting of anti-reflux therapy, pepsin secretion inhibition, bile acid neutralization, and lifestyle modifications. This patient underwent surgery to excise the granuloma, then relapsed, underwent a second surgery, which was followed by a second recurrence. The granuloma then disappeared after 9 mo of combined treatment with ilaprazole enteric-coated capsules (10 mg qd), mosapride tablets (5 mg tid) and compound digestive enzyme capsules (2 tablets). The drug regimen was discontinued after one year, and no recurrence of the lesion has been reported during the one-year follow-up period.
We report a combination of pharmacotherapeutics and lifestyle modifications for the management of laryngopharyngeal reflux disease to address recurring LCG.
Core Tip: Laryngeal contact granuloma (LCG) is difficult to treat and frequently associated with high persistence and recurrence. We describe a patient with recurrent LCG in which a good response was achieved through successful management of laryngopharyngeal reflux disease using a combination pharmacotherapeutic regimen consisting of anti-reflux therapy, pepsin secretion inhibition, bile acid neutralization, and lifestyle modifications. The drug regimen was discontinued after one year, and no recurrence was observed during the one-year follow-up period. This case report highlights the efficacy of combined pharmacotherapeutics and lifestyle modifications in managing laryngopharyngeal reflux disease to address recurring LCG.
- Citation: Li K, Chen WY, Li YY, Wang TL, Tan MJ, Chen Z, Chen H. Laryngopharyngeal reflux disease management for recurrent laryngeal contact granuloma: A case report. World J Clin Cases 2021; 9(8): 1989-1995
- URL: https://www.wjgnet.com/2307-8960/full/v9/i8/1989.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i8.1989
Laryngeal contact granuloma (LCG), also called laryngeal arytenoid granuloma or vocal process granuloma, refers to non-neoplastic inflammatory granulation tissue at the medial surface of the cartilaginous vocal process[1]. Hoarseness and abnormal pharyngeal sensations are the most common complaints associated with this disease, and LCG is sometimes accompanied by airway obstruction[2]. Previous reports have indicated that 0.9%-2.7% of adults with voice disorders have LCG[3], and that the incidence in males is higher than that in females[4]. Several possible etiological factors for LCG have been proposed, such as laryngopharyngeal reflux disease (LPRD)[2,5], voice abuse, smoking, and alcohol[4,6]. However, the primary driving factor in LCG occurrence is generally thought to be reflux from the esophagus into the pharynx[7]. This difficult to treat laryngeal disease not only has various etiologies, but also a high propensity for persistence and recurrence despite multifactorial treatment alternatives[2]. This intractability may be related to repeated exposure of the granuloma site to etiological factors. Therapeutic methods for LCG include surgical treatments such as laser excision, microlaryngoscopic excision, and low-dose radiotherapy for refractory lesions. More conservative LCG treatments include anti-reflux therapy, voice therapy, antibiotics, corticosteroids, zinc supplements, and botulinum toxin injection[2]. Excision treatment is based on removing the mass granuloma, whereas conservative therapies mitigate inflammation or reduce the friction during phonation of the vocal cords. However, the selection of LCG treatments remains controversial specifically because pharmacological treatments may not relieve hoarseness, whereas granuloma excision, which can quickly restore vocal function, is accompanied by a very high rate of recurrence. Surgery has been widely adopted as the treatment of choice for LCG, and moreover, there is no consensus on the appropriate duration of drug treatment, or whether the treatments should be discontinued directly or dosages should be reduced in a stepwise fashion after the patient stabilizes.
Thus, in order to help patients with multiple recurrences of LCG, we report a combined management regimen of pharmacotherapeutic treatments and lifestyle modifications.
A 34-year-old man presented to The Second Clinical College of Guangzhou University of Chinese Medicine with no history of smoking or alcohol abuse. The chief complaint during his initial visit was hoarseness, accompanied by sore throat and acid reflux.
The patient’s symptoms started two months ago.
The patient had no previous medical history.
He was a non-smoker with no specific family history.
Indirect laryngoscopy showed a (left) vocal cord mass.
Hematological examinations were within normal limits.
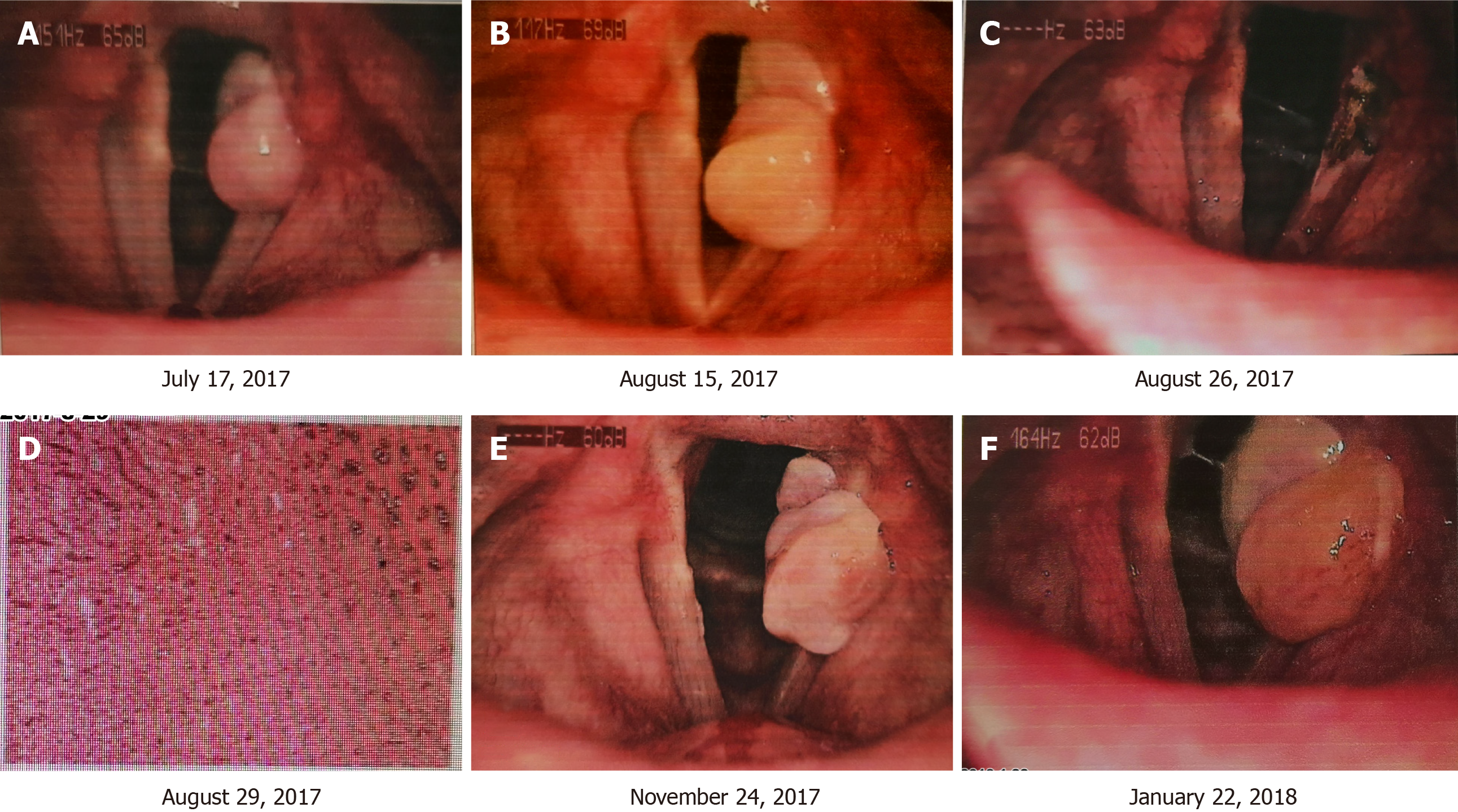
Laryngoscopy on May 2, 2017 showed a (left) vocal cord mass diagnosed as contact granuloma (Figure 1A).
LCG of the left vocal cord.
After surgery, the patient's hoarseness was alleviated, and he was prescribed proton pump inhibitor (PPI) therapy with esomeprazole enteric-coated tablets 20 mg/d for 4 wk to mitigate reflux. After treatment, the patient's acid reflux symptoms remained unresolved, and his hoarseness symptoms recurred. Re-examination by laryngoscopy showed recurrence of the left vocal cord granuloma (Figure 2A and B), similar in size to the granuloma before surgery. He was again admitted to hospital and underwent the same surgical resection of the recurring granuloma (Figure 2C and D). During hospitalization, we found that the patient had been regularly eating spicy food and desserts, such as cream cake and carbonated drinks. Combined with the laryngeal dynamics assessment, the internationally recognized Reflux Findings Score (RFS) was greater than 7, thus leading to a subsequent diagnosis of LPRD[8]. The patient was then provided with lifestyle and dietary education to address the LPRD, and after surgery he was prescribed a different PPI, at a higher dosage. After changing to rabeprazole enteric-coated capsules (20 mg bid) combined with mosapride tablets (5 mg tid) for 8 wk, the hoarseness and acid reflux symptoms subsided.
Although, the patient continued treatment, a review of the laryngoscopy at three months after the second operation revealed a recurrence of the left vocal cord mass, which was the same size as the granuloma prior to surgery (Figure 2E). We initially speculated that the PPIs had been ineffective, and therefore proposed changing the rabeprazole enteric-coated capsules to ilaprazole enteric-coated capsules (10 mg qd), still combined with mosapride tablets. After 12 wk of this regimen the chronic hoarseness and acid reflux persisted and, on January 22, 2018, a review of the laryngoscopy revealed no change in the size of the LCG (Figure 2F).
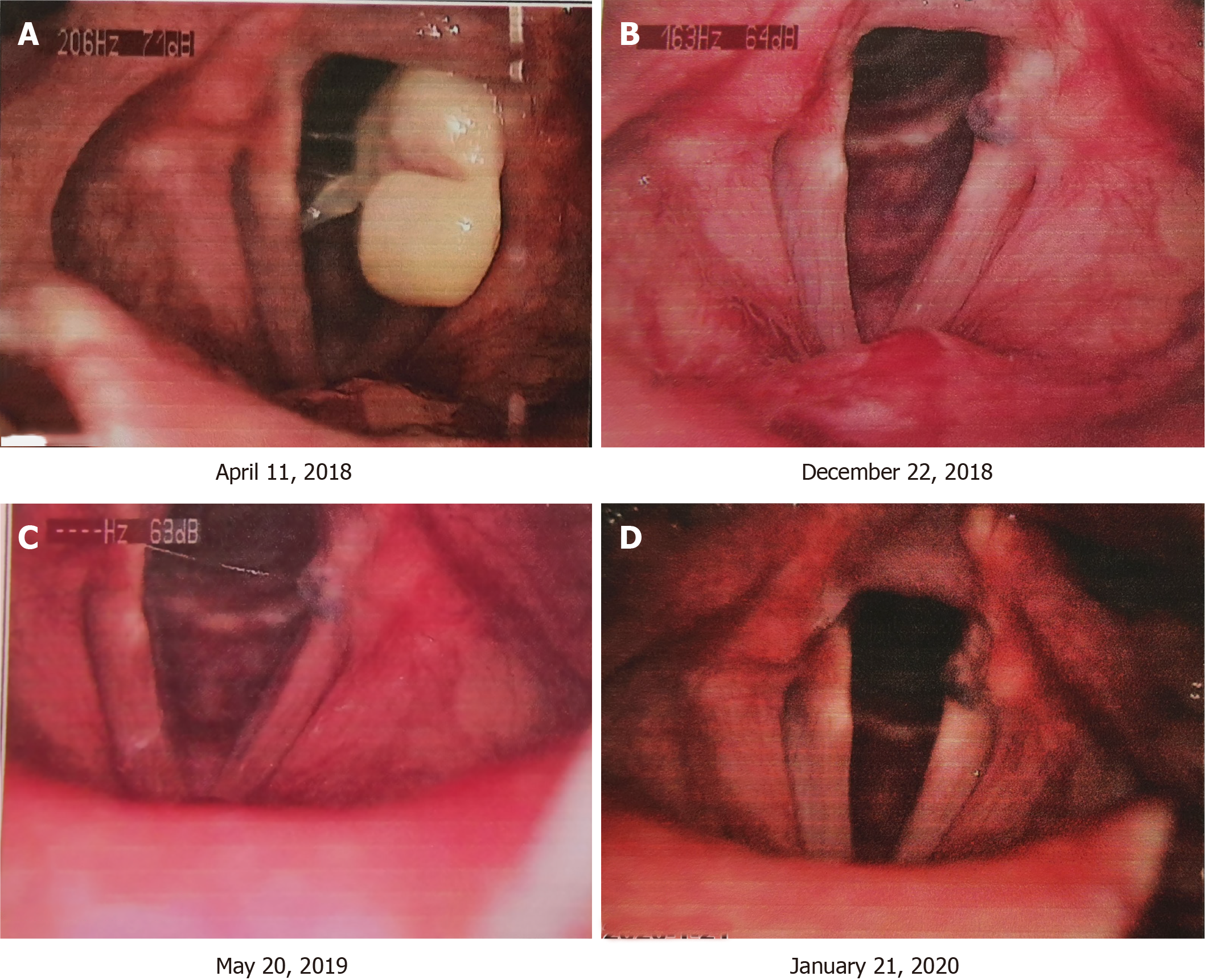
Consultation with gastroenterologists resulted in the addition of a compound digestive enzyme to the original treatment plan of ilaprazole enteric-coated capsules (10 mg qd) and mosapride tablets (5 mg tid). After 12 consecutive weeks of this combined treatment the hoarseness and acid reflux symptoms subsided. On April 11, 2018, laryngoscopy showed that the LCG size was substantially reduced (Figure 3A) and the patient was then instructed to continue treatment according to the program. A review of laryngeal dynamic microscopy conducted on October 22, 2018 showed that the LCG had disappeared (Figure 3B). The compound digestive enzyme capsules and mosapride tablets were then discontinued, while ilaprazole tablets were gradually reduced and discontinued by December 2018.
The patient has remained off medication, and as of this reporting has shown no signs of hoarseness or acid reflux. The laryngoscopy was reviewed on May 20, 2019 and again on January 21, 2020 (Figure 3C and D), both of which showed no signs of recurrence. In addition, no drug-related adverse reactions were reported throughout the treatment period or after discontinuation.
Here, we report a case with recurrent LCG in which the patient underwent surgery, relapsed, underwent a second surgery, and subsequent recurrence. At the onset of the second recurrence we recommended a treatment regimen consisting of ilaprazole enteric-coated capsules (10 mg qd) for anti-reflux therapy, mosapride tablets (5 mg tid) for pepsin secretion inhibition, compound digestive enzyme capsules (2 tablets) for bile acid neutralization, and lifestyle modifications. The granuloma disappeared and no recurrence was reported within one year of follow-up, strongly suggesting that this combination therapy may address the long-standing issue of LCG recurrence in the post-operative period.
Granulomas located on the vocal process are believed to be caused primarily by LPRD, and the persistence of LPRD contributes to the high recurrence rate of LCG[5,7]. In addition to RFS, measurements of the reflux symptoms index[9] and reflux symptom score[10] can be obtained using electronic laryngoscopy before patients receive treatment. Moreover, a Dx-pH measurement test, a new sensitive oropharyngeal pH device for the detection of pH events that begin at the distal esophagus and travel upward to the oropharynx, can also be used for the diagnosis of LPRD[11]. We therefore propose that the good outcome following treatment of recurrent LCG in this case was likely due to successful LPRD management. While the role of surgery is simply to remove the lesion, viable strategies for LCG management may also necessarily incorporate treatment of LPRD that include medications and lifestyle modifications.
A growing number of studies have recommended anti-reflux-based conservative therapy as a first-line treatment instead of surgical excision[5]. Rudman et al[12] reported that non-surgical patients are significantly more likely to experience success upon initial treatment than surgical patients. Lee et al[13] reported that based on long-term outcomes, PPI anti-reflux treatment, botulinum toxin, and voice therapy are more effective than observation alone. In contrast, surgery and steroid inhalation showed no statistically significant difference to observation alone. Karkos et al[14] reviewed LCG treatments and concluded that anti-reflux drugs combined with voice training and lifestyle changes lead to the lowest recurrence rates. In addition, Lei et al[15,16] determined that a combination of PPI and prokinetic drug therapy is more effective against LCG than botulinum toxin injection.
Anti-reflux therapy is an essential component of any conservative treatment regimen. PPIs, which irreversibly inhibit H-K-ATPase secretion in the gastric mucosa and protects the throat mucosa from gastric acid, are considered to be the most potent pharmaceutical inhibitors of gastric acid production[17], but nonetheless may be insufficient, as observed in this case. The various PPIs used in the clinic each have their own advantages, and therefore, different PPIs can be prescribed, or the dosage can be increased, when the treatment effect is poor or when there are adverse reactions[15,18]. Mosapride is a prokinetic drug that is unique among prokinetic agents because it not only accelerates gastric emptying throughout the gastrointestinal tract, but also leads to favorable effects as a PPI-based therapy[19]. However, the patient’s condition in this case did not improve after mosapride treatment, which led us to seek an alternative program, i.e, supplementation with compound digestive enzyme capsules.
Sereg-Bahar et al[20] argued that biliary reflux — the retrograde progression of bile acid contents through the stomach into the upper aerodigestive tract — may inhibit anti-reflux treatment. The compound digestive enzyme capsules administered in this case were composed of ursodeoxycholic acid (UDCA) 25 mg, pepsin 25 mg, papain 50 mg, amylase 15 mg, ursodeoxycholic acid 25 mg, cellulase 15 mg, trypsin 2550 USP units, pancreatic amylase 2550 USP units, and pancreatic lipase 412 USP units. A previous study showed that UDCA neutralizes bile acids, mitigates the damage they cause to the gastric mucosal barrier, and improves clinical symptoms[21]. Given the success of this treatment in our patient, we therefore concluded that the recurring LCG was caused by gastric acid, pepsin, and bile acid. The digestive enzymes may play an important role in the pharmacological treatment of LCG. The anti-reflux therapy in this case was necessary for management of reflux disease, which was pivotal in the resolution of LCG recurrence. Moreover, this case demonstrates that a multi-disciplinary approach is helpful in formulating the best treatment method.
In addition to medications, lifestyle changes are integral in the management of LPRD. Although it may be difficult for patients to implement and sustain large lifestyle modifications, targeted modifications directed at adjusting eating habits, alcohol/smoking cessation, and weight control may be more feasible and can provide tangible symptomatic improvement. The patient in this case was asked to make lifestyle modifications, including voice rest, abstention from spicy food and desserts, and to refrain from eating within three hours before sleep. While it may be difficult to quantify the specific contributions of these targeted modifications to resolving LCG recurrence, the potential benefits of these lifestyle changes for alleviating reflux disease are established[22], and therefore should not be ruled out when reflux drives recurrent LCG.
We describe a patient with recurrent LCG after surgery who was treated by LPRD management. The positive outcome in this case supports the use of combination therapies for LCG based on reflux suppression, pepsin secretion inhibition, bile acid neutralization, and lifestyle modifications. Additional cases are required to establish guidelines for the treatment of recurrent LCG and we will continue regular follow-up of this patient.
The investigators obtained written informed consent from the patient, and we would like to thank his dedication. We would also like to thank Dr. Li Zhou from Guangdong Provincial Hospital of Chinese Medicine for her comments on this manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Müller DT S-Editor: Zhang H L-Editor: Webster JR P-Editor: Li JH
| 1. | Carroll TL, Gartner-Schmidt J, Statham MM, Rosen CA. Vocal process granuloma and glottal insufficiency: an overlooked etiology? Laryngoscope. 2010;120:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. | Chen M, Chen J, Yang Y, Li CJ, Wu HT, Chen L. Conservative Treatment versus Surgery for Laryngeal Contact Granuloma: A Prospective Study. ORL J Otorhinolaryngol Relat Spec. 2018;80:307-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Ylitalo R, Lindestad PA. Laryngeal findings in patients with contact granuloma: a long-term follow-up study. Acta Otolaryngol. 2000;120:655-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | al-Dousary S. Vocal process granuloma. Ear Nose Throat J. 1997;76:382-386, 387. [PubMed] |
| 5. | Chang W, Xu W, Cheng L. Treatment of Laryngeal Contact Granuloma: Surgical Therapy or Conservative Treatment. ORL J Otorhinolaryngol Relat Spec. 2019;81:348-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Devaney KO, Rinaldo A, Ferlito A. Vocal process granuloma of the larynx-recognition, differential diagnosis and treatment. Oral Oncol. 2005;41:666-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Haggitt RC. Histopathology of reflux-induced esophageal and supraesophageal injuries. Am J Med. 2000;108 Suppl 4a:109S-111S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Belafsky PC, Postma GN, Koufman JA. The validity and reliability of the reflux finding score (RFS). Laryngoscope. 2001;111:1313-1317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 702] [Cited by in RCA: 686] [Article Influence: 28.6] [Reference Citation Analysis (1)] |
| 9. | Belafsky PC, Postma GN, Koufman JA. Validity and reliability of the reflux symptom index (RSI). J Voice. 2002;16:274-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 927] [Cited by in RCA: 995] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 10. | Lechien JR, Bobin F, Muls V, Thill MP, Horoi M, Ostermann K, Huet K, Harmegnies B, Dequanter D, Dapri G, Maréchal MT, Finck C, Rodriguez Ruiz A, Saussez S. Validity and reliability of the reflux symptom score. Laryngoscope. 2020;130:E98-E107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 114] [Article Influence: 22.8] [Reference Citation Analysis (1)] |
| 11. | Wiener GJ, Tsukashima R, Kelly C, Wolf E, Schmeltzer M, Bankert C, Fisk L, Vaezi M. Oropharyngeal pH monitoring for the detection of liquid and aerosolized supraesophageal gastric reflux. J Voice. 2009;23:498-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 82] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 12. | Rudman JR, McGee CS, Diaz J, Rosow DE. Assessing the utility of non-surgical treatments in the management of vocal process granulomas. J Laryngol Otol. 2020;134:68-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Lee SW, Hong HJ, Choi SH, Sun DI, Park YH, Lee BJ, Kwon SK, Park IS, Lee SH, Son YI. Comparison of treatment modalities for contact granuloma: a nationwide multicenter study. Laryngoscope. 2014;124:1187-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Karkos PD, George M, Van Der Veen J, Atkinson H, Dwivedi RC, Kim D, Repanos C. Vocal process granulomas: a systematic review of treatment. Ann Otol Rhinol Laryngol. 2014;123:314-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Lei L, Yang H, Zhang X, Ren J. Comparison of the effects of esomeprazole plus mosapride citrate and botulinum toxin A on vocal process granuloma. Am J Otolaryngol. 2017;38:593-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Lei L, Yang H, Zhao Y, Zhang XS, Zou J, Ren J, Zheng YT, Ren JJ. [A comparative study of therapy effects between esomeprazole plus mosapride citrate and botulinum toxin injection on vocal process granuloma]. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017;31:1006-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Portnoy JE, Gregory ND, Cerulli CE, Hawkshaw MJ, Lurie D, Katz PO, Sataloff RT. Efficacy of super high dose proton pump inhibitor administration in refractory laryngopharyngeal reflux: a pilot study. J Voice. 2014;28:369-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Li J, Xiao S, Li X, Lyu Q, Yan Y, Zhang L. [Explanation of the experts consensus on diagnosis and treatment of laryngopharyngeal reflux disease (2015)]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016;51:327-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Karkos PD, Wilson JA. Empiric treatment of laryngopharyngeal reflux with proton pump inhibitors: a systematic review. Laryngoscope. 2006;116:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 117] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | Sereg-Bahar M, Jerin A, Jansa R, Stabuc B, Hocevar-Boltezar I. Pepsin and bile acids in saliva in patients with laryngopharyngeal reflux - a prospective comparative study. Clin Otolaryngol. 2015;40:234-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 81] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 21. | Zhang FF, Mao LY, Xie WC. [Observation on curative effect of compound digestive enzyme capsules combined with mosapride for bile reflux gastritis]. Zhongguo Shiyong Neike Zazhi. 2017;37:24-26. [DOI] [Full Text] |
| 22. | Wright MR, Sharda R, Vaezi MF. Unmet needs in treating laryngo-pharyngeal reflux disease: where do we go from here? Expert Rev Gastroenterol Hepatol. 2016;10:995-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |