Published online Jun 26, 2021. doi: 10.12998/wjcc.v9.i18.4599
Peer-review started: December 9, 2020
First decision: January 17, 2021
Revised: February 24, 2021
Accepted: April 6, 2021
Article in press: April 6, 2021
Published online: June 26, 2021
Processing time: 177 Days and 21.3 Hours
The management of severe extravasation injuries is still controversial. Extravasation injuries can be treated in many ways.
To present a series of patients with severe extravasation injuries due to infusion who were managed with ethacridine lactate dressing combined with localized closure and phototherapy.
In this study, we evaluated the data of eight patients, including six from the Department of Burn, one (with colorectal carcinoma) from the Veteran Cadre Department, and one (with leukemia) from the Hematology Department. Of these, three patients were male and five were female. Age of the patients ranged from 10 mo to 72 years, including two children (10 and 19 mo of age). In this study, the infusion was stopped immediately when the extravasation was identified. The extravasation event was managed routinely using a blocking solution. A ring-shaped localized closure was performed using the blocking agents. Moreover, ethacridine lactate dressing and phototherapy were applied for 3-5 d.
In this study, the drugs contained in the infusates were iodixanol, norepinephrine, alprostadil, amino acids, fat emulsion, cefoselis, cefoxitin, and potassium chloride + concentrated sodium chloride. All of the patients achieved complete healing after treatment and no obvious adverse reactions were observed.
The treatment of severe extravasation injuries using a combination of localized closure, ethacridine lactate dressing, and phototherapy resulted in satisfactory outcomes in patients.
Core Tip: The management of severe extravasation injuries is still controversial. The treatment of severe extravasation injuries can be performed using various methods. Ethacridine lactate dressing can be used to manage skin lesions, such as ulcers. In this study, the drugs contained in the infusates were iodixanol, norepinephrine, alprostadil, amino acids, fat emulsion, cefoselis, cefoxitin, and potassium chloride + concentrated sodium chloride. All eight patients achieved healing after treatment. No obvious adverse reactions were observed. Satisfactory effects were achieved in the treatment of severe extravasation injuries with a combination of localized closure, ethacridine lactate dressing, and phototherapy.
- Citation: Lu YX, Wu Y, Liang PF, Wu RC, Tian LY, Mo HY. Efficacy of combination of localized closure, ethacridine lactate dressing, and phototherapy in treatment of severe extravasation injuries: A case series. World J Clin Cases 2021; 9(18): 4599-4606
- URL: https://www.wjgnet.com/2307-8960/full/v9/i18/4599.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i18.4599
Intravenous infusion is often used in patients for the administration of a variety of fluids and drugs. Extravasation refers to the leakage of these infused fluids from the blood vessels into the subcutaneous tissues. It may present with localized swelling and pain, fever or cold, and even local necrosis, particularly with cytotoxic drugs[1,2]. It can also compromise blood vessels and local tissues, including nerves and tendons[3,4]. Furthermore, the subsequent scarring may lead to contracture, disfigurement, loss of function, complex regional pain syndrome, deformities, and potential long-term sequelae[5]. Extravasation injuries due to infusion are common; however, most of the hospitals have insufficient data because of underreporting and a lack of centralized registry. Generally, a number of patient- and staff-specific risk factors have been recognized, which could help prevent events of extravasation[2].
Extravasation injuries can aggravate the patients’ sufferings, prolong their treatment courses, and increase the economic burden. The management of extravasation usually involves a combination of 50% magnesium sulfate wet compress, Kanghuier hydrocolloid dressing, sodium aescinate gel application, traditional Chinese herbs, and localized closure[1,2,6-10]. Sometimes, these injuries may require open decompression and surgical treatments as well[11]. Nevertheless, these single methods often have little or no effect on severe extravasation injuries, which might deteriorate further and result in a series of severe consequences, such as local tissue necrosis and dysfunction.
Studies proposed that saline washout and liposuction are effective in management of grade 3 or 4 extravasation injuries[12,13]. Nevertheless, the best and optimal approach to reduce tissue damage and its consequences is still controversial[5]. Ethacridine lactate is a disinfectant used for skin preparation and disinfection. In patients with venous leg ulcers, an antiseptic ointment containing ethacridine lactate has been shown to reduce ulcers by > 20% at 4 wk[14]. Ethacridine lactate has also been suggested for the management of dry gangrene[15].
Specific treatment has not yet been identified for severe extravasation injury. Therefore, ethacridine lactate dressing combined with localized closure and phototherapy have been tried in patients with extravasation injury due to infusion. In this study, we aimed to present a case series of patients with severe extravasation injuries due to infusion who were managed with ethacridine lactate dressing combined with localized closure and phototherapy. The results could suggest novel methods to manage severe extravasation injuries.
We conducted a retrospective review of consecutive patients with serious extravasation injuries who were treated at Xiangya Hospital of Central South University, Hunan Province, China from May 2011 to July 2017. The study was approved by the Ethics Committee of the hospital (approval No. 202001107). The patients included in this study have given written informed consent for publishing the case details.
All patients who met the following diagnostic criteria for severe extravasation injuries were included in this study[1,2]: (1) Initial signs and symptoms, such as tingling, burning, discomfort/pain, swelling, and/or redness at the injection site; and (2) Blistering and/or skin discoloration. All these patients had stage 3 or 4 extravasation injuries, manifesting as swelling, blisters, and skin discoloration[16-18] or extravasation of blistering agents, blood products, irritating agents, or corrosive drugs in accordance with the American INS infiltration degree 4[19]. Patients with allergy to lidocaine or ethacridine lactate were excluded from the study.
According to routine practice, the infusion was stopped immediately and the intravenous tube was disconnected once extravasation was recognized. The original catheter was retained, to which a 2 mL disposable syringe was connected to extract as much infiltrated fluid as possible. The catheter was then removed and the swelling site was massaged gently for an outflow of the exudate from the pinhole. A blocking solution (usually 2 mL of 2% lidocaine + 6 mL of saline + 5 mg of dexamethasone) was prepared and its dosage was determined according to the size of the lesion to be closed. Then, a syringe was filled with the solution and connected to a nylon needle to reduce the mechanical damage. A local ring-shaped closure injection was performed after the routine disinfection. The needle was injected at an angle of 15-20° alongside the area. If no blood comes out while drawing back, the needle was withdrawn while injecting the fluid, leaving the needle inside. The direction of the needle was then changed to inject the solution into another area. A puncture was made at a point opposite to the original puncture point to inject the blocking agents as explained previously, forming a ring-shaped closure[20]. In general, two to four puncture points are needed for closure and the scope should be 0.5-1 cm beyond the infiltration site. The amount of the blocking agents should be enough to bulge the skin. The closure was performed and the area was observed closely. If the symptoms of extravasation improve significantly, the closure was stopped. Another two consecutive closures were performed in every 4-6 h in case of no significant improvement (softening of the swelling area, alleviated swelling, and alleviated discoloration). The patient was observed for any adverse reactions (e.g., discomfort, vomiting, and allergies) after every closure.
The ethacridine lactate dressing was freshly prepared before use. The nurse replaced the dressing whenever it was found to be dry. The dressing was made according to the size of the wound using double-layered gauze soaked in ethacridine lactate, covering > 2 cm on each side beyond the lesion boundaries. The dressing was kept on the wound for 3-5 d. The Kanghuier hydrocolloid dressing (Coloplast A/S, Humlebæk, Denmark) was used for swelling.
During dressing of the wound, a phototherapy device (Shenzen Pumen Technology, Co., Ltd., Shenzhen, China) was used at a distance of 20 cm away from the extravasation area for 20 min/session, twice daily, for 3-5 d. The patients were asked to wear eye masks to avoid looking at the light source.
This study assessed eight patients, including six from the Department of Burn, one with colorectal carcinoma from the Veteran Cadre Department, and one with leukemia from the Department of Hematology (Table 1). Of these, three patients were male and five were female. The age of these patients ranged from 10 mo to 72 years, including two children aged 10 and 19 mo, respectively. The extravasation sites included the hand, forearm, foot, and calf. The drugs contained in the infusates were iodixanol, norepinephrine, alprostadil, amino acids, fat emulsion, cefoselis, cefoxitin, and potassium chloride + concentrated sodium chloride.
| No. | Age | Gender | Cause of hospitalization | Infusate(s) | Extravasation sites | Follow-up time after discharge |
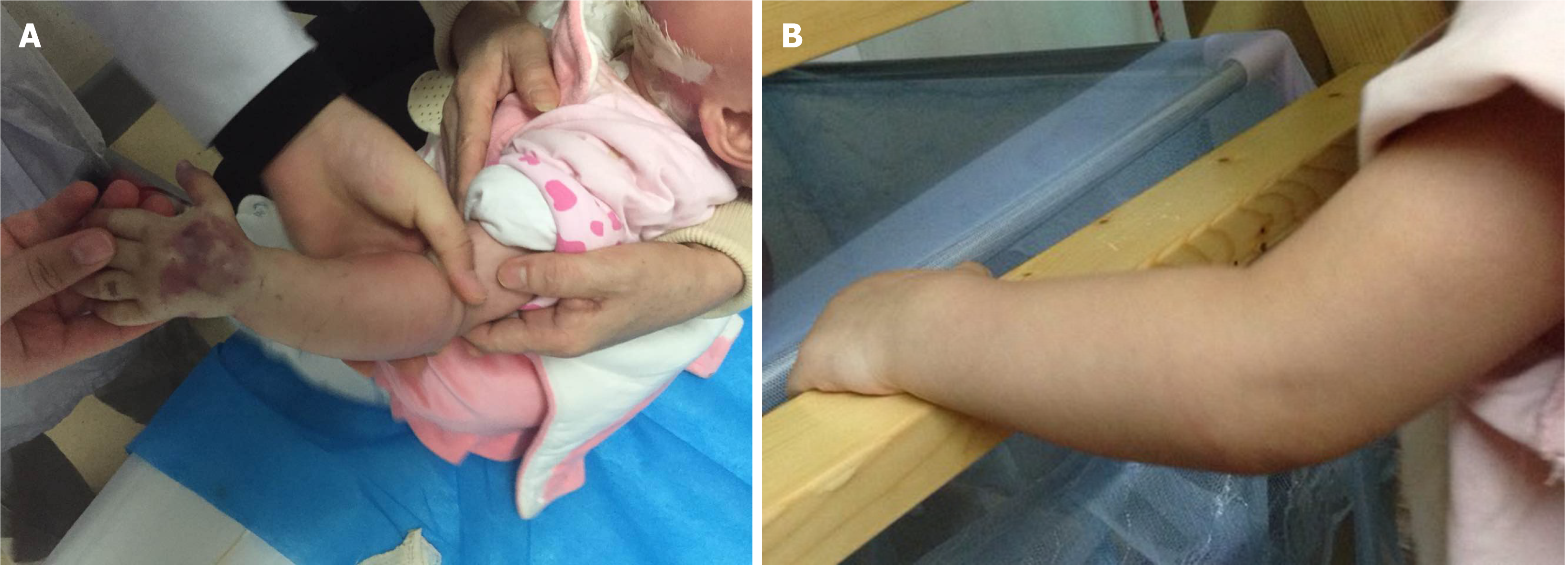
| 1 | 10 mo | Female | Scalding | Cefoselis | Cyanosis and purpling at the dorsum of left hand; swelling of the entire forearm (Figure 2) | 6 d, 21 mo (Figure 2B) |
| 2 | 19 mo | Male | Scalding | Potassium chloride + concentrated sodium chloride | Cyanosis and purpling accompanied with multiple blisters at the right medial malleolus; swelling of the distal two-thirds of the right leg and dorsum pedis; and cyanosis at the dorsum pedis and toes (Figure 1) | 11 d, 17 mo (Figure 1B) |
| 3 | 27 yr | Male | Right foot polydactyly, necrotic vein, angiitis | Alprostadil | Left forearm | 6 d |
| 4 | 72 yr | Female | Diabetic foot | Iodixanol | Right forearm | 9 d |
| 5 | 54 yr | Female | Large-area burns | Amino acids | Back of the left foot | 1 wk |
| 6 | 69 yr | Male | Colorectal carcinoma | Fat emulsion | Left arm | 1 wk |
| 7 | 35 yr | Female | Leukemia | Norepinephrine | Back of the right hand | 1 wk |
| 8 | 83 yr | Female | Necrotic skin combined with infection in the right leg | Cefoxitin | Right forearm | 10 d |
The intravenous infusion was stopped immediately and the intravenous tube was disconnected in all patients when the initial sign of extravasation was recognized. Every patient received three closures within an interval of 4-6 h. No obvious adverse reactions were observed during extravasation management.
All of the patients included in this study achieved complete healing within 21 d following the extravasation event. No obvious adverse reactions were seen in any of the patients during the hospital stay or follow-up assessment. Two typical cases of this study are shown in Figures 1 and 2. Unfortunately, the patients were not photographed immediately after healing, as this study was of retrospective nature. The pictures presented in this paper were taken at the time of writing this article. All of the patients included in this study achieved satisfactory healing without scars.
All data were tabulated and analyzed. Descriptive statistics were used for analysis and the results are expressed.
The management of severe extravasation injuries is still controversial. These injuries can have severe complications in the patient. Extravasation can be treated using various methods[11]. However, the optimal treatment method has not yet been identified. The aim of this study was to present a case series of patients, with severe extravasation injuries due to infusion, who were managed with ethacridine lactate dressing combined with localized closure and phototherapy. The results suggest that satisfactory effects were achieved in the treatment of severe extravasation injuries with a combination of localized closure, ethacridine lactate dressing, and phototherapy.
The United States ISN divides extravasation injuries into four stages[21-23]. Usually, the therapeutic effects of infiltration are satisfactory for grade 1 or 2. Nevertheless, there is no consensus for the treatment of severe extravasation injuries, that is, the extravasation injuries of grade 3 or 4 and those involving blistering agents, blood products, and irritating or corrosive drugs[24]. At present, the most commonly used method for severe extravasation injuries is saline washout combined with liposuction, as proposed by Gault[25] in 1993, which is effective but invasive and requires professional operations (or referring the patients to plastic surgery), and the incisions under anesthesia may leave scars. In contrast, the method used in this study can be performed by nurses and does not need incision under anesthesia, with no scar left. The patients can recover quickly with minimal suffering and at reduced cost.
Closure therapy is also called “localized closure,” and this pain management approach has evolved from local anesthesia, wherein a mixture of local anesthetics and hormones is injected into the pain area to protect the nervous system, relieve pain, and prevent infections[26,27]. Localized closure therapy is commonly used to treat scapulohumeral periarthritis, keloids, and chronic prostatitis[28-30] and for infusion infiltration as well[10,20,31]. At our hospital, local blockage is routinely performed using dexamethasone, lidocaine, and normal saline.
Ethacridine lactate is a topical disinfectant that inhibits Gram-positive bacteria, especially streptococci and staphylococci. It is often used in debridement and dressing of various traumas, exudations, erosive infectious wounds, and skin lesions such as venous ulcers[32]. Phototherapy can promote metabolism, increase synthesis of RNA, DNA, and protein, and promote the production of vascular endothelial and fibroblast growth factors, consequently improving microcirculation and local nutrition, and accelerating granulation tissue growth and wound healing[33,34]. Chen et al[35] believed that phototherapy instrument can improve local blood circulation, relieve redness and pain of the extravasation area, increase tissue repair and regeneration, and shorten the healing course of drug extravasation. Therefore, the combination of these three methods, including localized closure, ethacridine lactate dressing, and phototherapy, can significantly promote injury healing, relieve symptoms, quicken recovery of severe extravasation injuries, and then, effectively prevent further tissue necrosis.
When severe extravasation injuries occur, the key to successful management is to carry out the comprehensive procedure described earlier immediately, preferably within 30 min. Of eight patients with extravasation injuries, two were from other wards and were treated 1 h after extravasation. One patient receiving amino acid infusion was treated only with Conhui water colloid because of inaccurate extravasation assessment. The injury became discolored within 24 h and eventually healed after the immediate comprehensive treatment described previously. In addition, the number of closures influences healing. Li[31] reported that the different numbers of closures for chemotherapeutic drug infiltration achieved different outcomes. In the present study, all patients received three closures. Therefore, we recommend that three closures be given to achieve the best results in patients with severe extravasation injuries and infusion of blister agents, blood products, or irritating or corrosive drugs.
This study has few limitations. It was a retrospective study, conducted at a single center. The sample size was small and the follow-up time of some patients was short. The patients in this study were given intravenous infusion of different drugs, which might have affected the findings. Moreover, the patients included in this study represented a wide age range. Therefore, prospective trials with a larger number of patients are needed to assess the efficacy of this approach.
In this study, good outcomes were achieved in the treatment of severe extravasation injuries with a combination of localized closure, ethacridine lactate dressing, and phototherapy. Furthermore, the procedure can be carried out by nurses without any incision under anesthesia, leaving no scars and inducing quick recovery without obvious adverse reactions. However, this approach should be further studied to overcome the limitations and generalize the outcomes.
Intravenous infusion is a commonly used method for the administration of a variety of fluids and medication directly into the vein of a patient. Occasionally, these infused drugs may leak from the blood vessels into the subcutaneous tissues. Such a leakage is known as extravasation. This condition can result in tissue necrosis and dysfunction, contracture, disfigurement, functional compromise, deformities, and potential long-term sequelae. Therefore, an optimal approach to reduce these severe complications of extravasation is an urgent necessity.
Effective management of severe extravasation injuries is still a challenging task, and no specific treatment has yet been identified.
The objective of this study was to present a case series of patients with severe extravasation injuries due to infusion who were managed using ethacridine lactate dressing combined with localized closure and phototherapy.
A retrospective study of eight patients (three male and five female) with severe extravasation injuries was conducted. Age of the patients ranged from 10 mo to 72 years. The extravasation event was managed using a combination of ethacridine lactate dressing, localized closure, and phototherapy.
The infusates administered to patients included iodixanol, norepinephrine, alprostadil, amino acids, fat emulsion, cefoselis, cefoxitin, and potassium chloride + concentrated sodium chloride. The extravasation sites included the forearm, hand, calf, and foot. All of the patients achieved complete healing within 21 d after the extravasation event. Adverse reactions were not observed during extravasation management, hospital stay, or follow-up visit.
Patients with severe extravasation injuries can obtain satisfactory results when treated with a combination of localized closure, ethacridine lactate dressing, and phototherapy.
Treatment using ethacridine lactate dressing combined with localized closure and phototherapy could become a novel method in managing severe extravasation injuries. However, as this study was retrospective in nature, prospective multicenter trials with a larger number of patients are needed.
Manuscript source: Unsolicited manuscript
Specialty type: Dermatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yunus MHM S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Li JH
| 1. | Kreidieh FY, Moukadem HA, El Saghir NS. Overview, prevention and management of chemotherapy extravasation. World J Clin Oncol. 2016;7:87-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 106] [Cited by in RCA: 99] [Article Influence: 11.0] [Reference Citation Analysis (5)] |
| 2. | Pérez Fidalgo JA, García Fabregat L, Cervantes A, Margulies A, Vidall C, Roila F; ESMO Guidelines Working Group. Management of chemotherapy extravasation: ESMO-EONS Clinical Practice Guidelines. Ann Oncol. 2012;23 Suppl 7:vii167-vii173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 101] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 3. | Kim JT, Park JY, Lee HJ, Cheon YJ. Guidelines for the management of extravasation. J Educ Eval Health Prof. 2020;17:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 4. | Reddy SS, Somayaji S, Krishna Murthy M, Maka VV. 5-Fluorouracil induced extravasation injury. Indian J Cancer. 2020;57:467-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Gopalakrishnan PN, Goel N, Banerjee S. Saline irrigation for the management of skin extravasation injury in neonates. Cochrane Database Syst Rev. 2017;7:CD008404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Zhao F, Hong ZY, Chen LP. Clinical application of 25% magnesium sulfate in extravasation of intravenous infusion. Haixia Yaoxue. 2010;22:96-97. |
| 7. | Ying J, Gui M, Xue J. Application of Kahui transparent dressing in neurosurgery infusion. Zhongguo Shiyong Huli Zazhi. 2005;21:48. |
| 8. | Zheng R, Lu Z. Clinical observation of the effect of Compound Sodium Aescinate Gel on swelling induced by infusion infiltration. Hushi Jinxiu Zazhi. 2005;20:857-858. |
| 9. | Cao Y, Tan K, Chen R. Clinical study of the effect of Shuangbai powder in the treatment of chemotherapy extravasation lesion. Zhongyi Zazhi. 2006;24:1275. |
| 10. | Dong X, Ai Y, Li G. A comparative study on treatment effects of infusion infiltration between the local closure of dexamethasone and lidocaine and Magnesium Sulfate wet compress. Nurs Res. 2011;25:1837. |
| 11. | Al-Benna S, O'Boyle C, Holley J. Extravasation injuries in adults. ISRN Dermatol. 2013;2013:856541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 63] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Dionyssiou D, Chantes A, Gravvanis A, Demiri E. The wash-out technique in the management of delayed presentations of extravasation injuries. J Hand Surg Eur Vol. 2011;36:66-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Harrold K, Gould D, Drey N. The efficacy of saline washout technique in the management of exfoliant and vesicant chemotherapy extravasation: a historical case series report. Eur J Cancer Care (Engl). 2013;22:169-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | O'Meara S, Al-Kurdi D, Ologun Y, Ovington LG, Martyn-St James M, Richardson R. Antibiotics and antiseptics for venous leg ulcers. Cochrane Database Syst Rev. 2014;(1):CD003557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 15. | Dreiplatz G, Biro B, Kröger K. Local treatment of dry gangrene. Vasa. 2002;31:280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 16. | Reynolds PM, MacLaren R, Mueller SW, Fish DN, Kiser TH. Management of extravasation injuries: a focused evaluation of noncytotoxic medications. Pharmacotherapy. 2014;34:617-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 105] [Article Influence: 9.5] [Reference Citation Analysis (1)] |
| 17. | Amjad I, Murphy T, Nylander-Housholder L, Ranft A. A new approach to management of intravenous infiltration in pediatric patients: pathophysiology, classification, and treatment. J Infus Nurs. 2011;34:242-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Corbett M, Marshall D, Harden M, Oddie S, Phillips R, McGuire W. Treatment of extravasation injuries in infants and young children: a scoping review and survey. Health Technol Assess. 2018;22:1-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Infusion Nurses Society. Policies and Procedures for Infusion Nursing. Armeraeial: Infusion Nurses Society, 2006. [cited 10 February 2020]. Available from: https://www.ins1.org/policies-and-procedures-for-infusion-therapy/. |
| 20. | Xie Y, Su B, Gong L. Effect observation of local closure combined with Magnesium Sulfate wet compress for extravasation injury of strong irritative drugs. Zhongguo Shiyong Huli Zazhi. 2010;26:45-47. |
| 21. | Millam DA. Managing complications of i.v. therapy (continuing education credit). Nursing. 1988;18:34-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Flemmer L, Chan JS. A pediatric protocol for management of extravasation injuries. Pediatr Nurs. 1993;19:355-358, 424. [PubMed] |
| 23. | McCullen KL, Pieper B. A retrospective chart review of risk factors for extravasation among neonates receiving peripheral intravascular fluids. J Wound Ostomy Continence Nurs. 2006;33:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 24. | Kostogloudis N, Demiri E, Tsimponis A, Dionyssiou D, Ioannidis S, Chatziioannidis I, Nikolaidis N. Severe Extravasation Injuries in Neonates: A Report of 34 Cases. Pediatr Dermatol. 2015;32:830-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 25. | Gault DT. Extravasation injuries. Br J Plast Surg. 1993;46:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 158] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 26. | Cen B, Ke Z. Effect Observation of Traumatic yellow water gauze in the treatment of extravasation injury. Nanfang Huli Xuebao. 2005;12:58-59. |
| 27. | Zhuang X, Zeng Y, Chen B. Modern Anesthesiology. Beijing: People's Medical Publishing House, 2003. |
| 28. | Yang X, Ji S, Wang X. Effect observation of closure therapy combined with strontium -90 applicator in the treatment of keloids. Hebei Yiyao. 2012;34:58. |
| 29. | Wang Z. Effect analysis of blocking therapy in the treatment of chronic prostatitis. Zhongguo Linchuang Yixue. 2012;19:666-675. |
| 30. | Gong D, Chen F, Chen J. Short-term effect observation of Closure combined with exercise therapy for scapulohumeral periarthritis. Jing Yao Tong Zazhi. 2010;31:231-232. [DOI] [Full Text] |
| 31. | Li XY. Effect observation of different numbers of closures after chemotherapy drug leakage. Zhongguo Shiyong Huli Zazhi. 2003;19:5-6. |
| 32. | Junka A, Bartoszewicz M, Smutnicka D, Secewicz A, Szymczyk P. Efficacy of antiseptics containing povidone-iodine, octenidine dihydrochloride and ethacridine lactate against biofilm formed by Pseudomonas aeruginosa and Staphylococcus aureus measured with the novel biofilm-oriented antiseptics test. Int Wound J. 2014;11:730-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 33. | He HY, Zhang LY, Ye M. Effect observation of short term red light therapy on wound healing and pain. Jiefangjun Yiyao Zazhi. 2013;25:14-16. |
| 34. | Jia DB, Zhu N, Liu S, Li NM, Tang LM, Zhang YF, Wang ZL, Sun QL. Effect of red light irradiation on wound healing. Disi Junyi Daxue Xuebao. 2008;29:1195-1197. |
| 35. | Chen XM, Pan S, Hu K, Liu XC, Xu Y, Peng GQ. Clinical observation of photon therapy instrument irradiation combined with Shuangbai wet compress for 30 cases of high risk drug extravasation. Shandong Yiyao. 2015;55:69-70. [DOI] [Full Text] |