Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2704
Peer-review started: June 18, 2019
First decision: July 30, 2019
Revised: August 19, 2019
Accepted: August 26, 2019
Article in press: August 26, 2019
Published online: September 26, 2019
Processing time: 102 Days and 19.2 Hours
Currently, there is no uniform standard for analgesia during laparoscopic hepatectomy. Most of the analgesia schemes adopt epidural analgesia after laparotomy. Although the analgesia is effective, it has a great impact on the recovery of patients after laparoscopic hepatectomy and is not completely suitable for analgesia after laparoscopic hepatectomy. Although multimodal perioperative analgesia can significantly relieve postoperative pain, there is no relevant study of parecoxib combined with ropivacaine for post-laparoscopic hepatectomy analgesia.
To study the analgesic effect of the preoperative intravenous injection of parecoxib combined with long-acting local anesthetic ropivacaine for incision infiltration in patients undergoing laparoscopic hepatectomy.
Forty-eight patients undergoing laparoscopic hepatectomy were randomly divided into a combined group (parecoxib combined with ropivacaine) and a control group. The visual analogue scale (VAS) at rest and during movement was used to compare the analgesic effect of the two groups. Meanwhile, the cumulative sufentanil, the recovery time for enterokinesia, the length of postoperative hospital stay, and the adverse reactions (nausea and vomiting) were recorded and compared between the two groups.
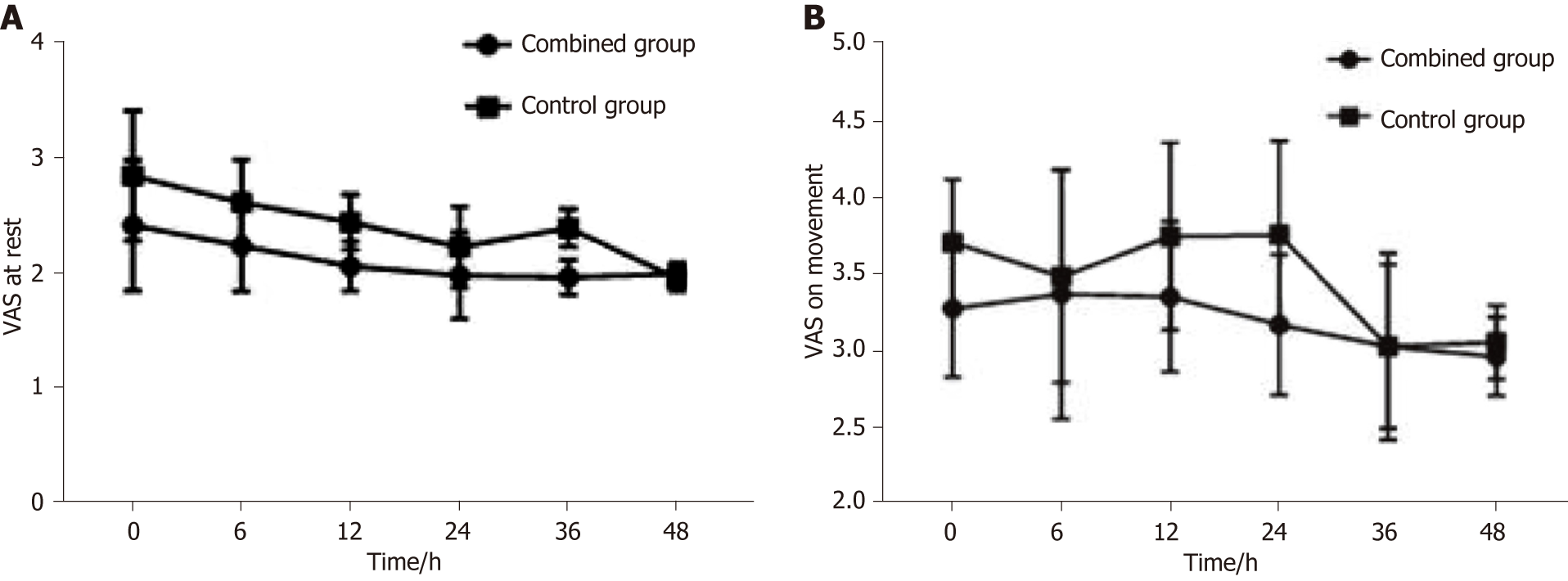
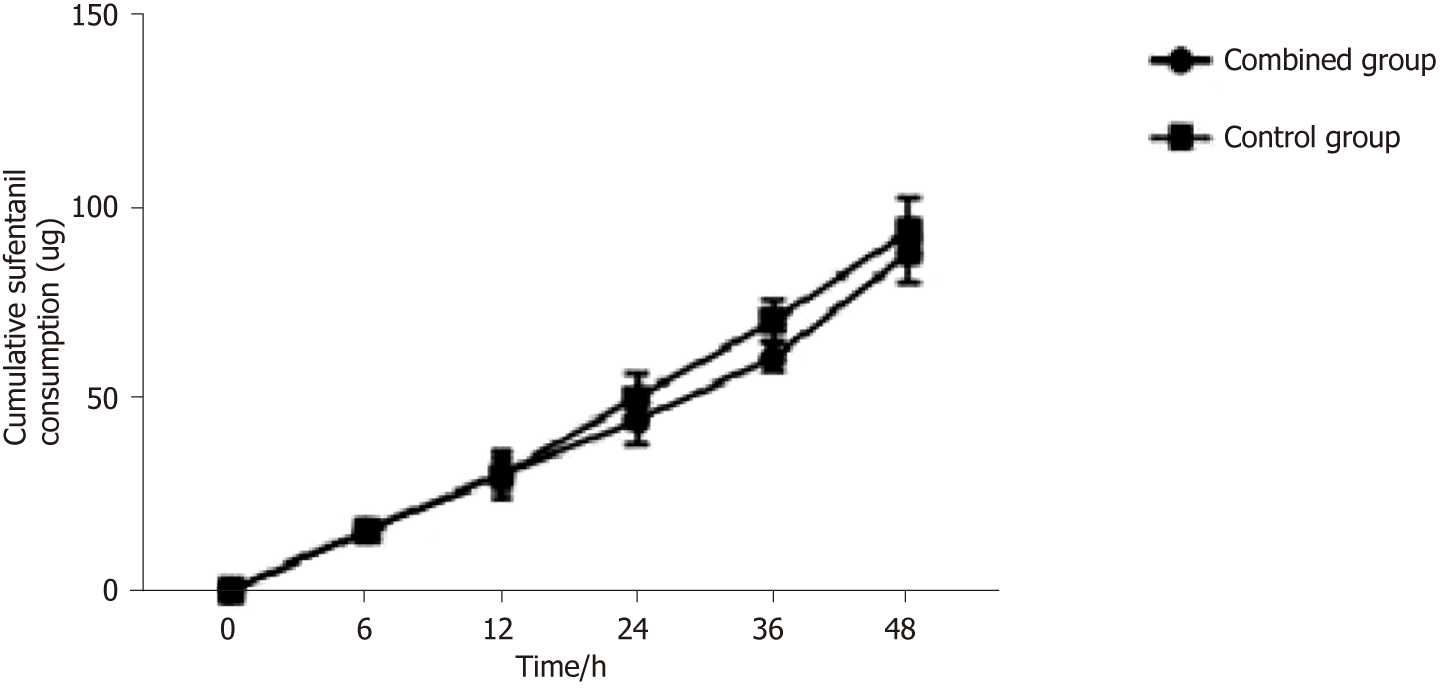
The change tendency in VAS scores for both groups was similar after operation. At rest, the VAS scores of the combined group were significantly lower than those of the control group at 0, 6, 12, 24 and 36 h, and during movement, the VAS scores of the combined group were significantly lower than those of the control group at 0, 6, 12, and 24 h. The recovery time for enterokinesia in the combined group was 2.9 d, which was significantly shorter than that in the control group. The cumulative sufentanil in the combined group decreased significantly at 24, 36, and 48 h after operation.
Preoperative intravenous injection of parecoxib combined with ropivacaine for incision infiltration is a simple and effective method for postoperative analgesia in laparoscopic hepatectomy, which could relieve pain and promote recovery.
Core tip: Forty-eight patients undergoing laparoscopic hepatectomy were randomly divided into a combined group (parecoxib combined with ropivacaine) and a control group. A visual analogue scale at rest and during movement was used to compare the analgesic effect of the two groups. Preoperative intravenous injection of parecoxib combined with the long-acting local anesthetic ropivacaine for incision infiltration is a simple and effective method for postoperative analgesia in patients undergoing laparoscopic hepatectomy, which could relieve postoperative pain and promote postoperative recovery.
- Citation: Huang SS, Lv WW, Liu YF, Yang SZ. Analgesic effect of parecoxib combined with ropivacaine in patients undergoing laparoscopic hepatectomy. World J Clin Cases 2019; 7(18): 2704-2711
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2704.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2704
Since the first laparoscopic hepatectomy was reported in 1991, this minimally invasive surgery has been introduced into the field of liver surgery[1]. With the advances of technology in more than 20 years and the improvement of surgical experience and new operative equipment, laparoscopic hepatectomy has gradually replaced open hepatectomy with incomparable advantages. Patients can quickly recover to normal function with minimal abdominal wall injury[2,3]. Nevertheless, the persistent pain due to the laparoscopy itself and the postoperative trauma affect the recovery of patients, prolong the hospital stay, and cause stress reactions and related complications, including cardiovascular and cerebrovascular accidents as well as gastrointestinal and neuroendocrine dysfunction[4,5].
Currently, there is no uniform standard for analgesia during laparoscopic hepatectomy. Most of the analgesia schemes adopt epidural analgesia after laparotomy. Although the analgesia is effective, it has a great impact on the recovery of patients after laparoscopic hepatectomy and is not completely suitable for analgesia after laparoscopic hepatectomy[6]. Recently, it has been reported that local wound infiltration with ropivacaine in open hepatectomy can significantly reduce postoperative pain and the stress response and accelerate postoperative recovery[7]. Preoperative intravenous use of parecoxib plays an important role in preemptive analgesia by inhibiting the expression of COX-2 and the synthesis of prostaglandins in the central nervous system[8]. Although multimodal perioperative analgesia can significantly relieve postoperative pain, there is no relevant study of parecoxib combined with ropivacaine for post-laparoscopic hepatectomy analgesia.
Therefore, this study aimed to observe the analgesic effect of preoperative intravenous injection of the highly selective COX-2 inhibitor parecoxib combined with the long-acting local anesthetic ropivacaine for incision infiltration in patients undergoing laparoscopic hepatectomy.
Forty-eight consecutive patients who underwent laparoscopic hepatectomy from January 2016 to December 2018 were included. The inclusion criteria included grades I–III according to the American Society of Anesthesiologists Physical Status Classification System (ASA), no history of motion sickness, nausea and vomiting, and chronic pain. Patients with gastroduodenal ulcer or coagulation dysfunction, or patients who were taking analgesics before operation were excluded from the study. This study was approved by the local Hospital Ethics Committee. Informed consent was obtained from all patients. The patients were randomly divided into two groups according to different analgesic methods: Combined group (parecoxib with ropivacaine, n = 24) and control group (n = 24). The specific clinical data of the patients are shown in Table 1.
| Characteristic | Combined group | Control group | t/χ2 value | P-value |
| Age (yr) | 48.958 ± 12.685 | 50.208 ± 9.86 | -0.381 | 0.705 |
| Gender | ||||
| Male/Female | 10/14 | 15/9 | 2.087 | 0.149 |
| Body weight (kg) | 68.368 ± 9.738 | 64.451 ± 8.652 | 1.473 | 0.148 |
| ASA grade | 0.543 | 0.762 | ||
| I/II/III | 4/15/5 | 6/13/5 | ||
| Incision length (cm) | 8.194 ± 0.415 | 7.992 ± 0.422 | 1.674 | 0.101 |
| Operative time | 136.083 ± 11.836 | 135.833 ± 11.484 | 0.074 | 0.941 |
| Intraoperative bleeding volume | 81.716 ± 14.737 | 79.116 ± 14.575 | 0.615 | 0.542 |
| Maximum diameter of tumors | 12.641 ± 5.075 | 10.705 ± 4.816 | 1.356 | 0.182 |
Preoperative Child-Pugh grade of liver function in both groups was grade A, and tracheal intubation plus combined intravenous inhalation was used. The combined group and the control group were given 20 mg of parecoxib or the same amount of saline intravenously 20 min before induction of anesthesia. Laparoscopic hepatectomy was performed by the same surgical team. Four to 5 puncture holes were assigned in the abdomen wall according to the location of the resected liver and the Joel-Cohen incision was used to take the specimen in which the length depended on the size of the specimen. In the combined group, 7.5 mg/mL ropivacaine solution was used for puncture incision infiltration, while in the control group, isotonic saline solution was used. When the abdominal puncture and Joel-Cohen incision were closed at the end of the operation, the subcutaneous tissue and deep myofascial and parietal peritoneum were infiltrated with a 20 mL solution. In addition, one or two abdominal drainage tubes were routinely placed near the hepatic section surface and fixed on the abdominal skin. Local infiltration of ropivacaine or saline was also given around the drainage tube.
All patients were given patient-controlled analgesia (PCA) to relieve pain after operation. Two hundred milliliters of 1 μg/mL of sufentanil was used in the analgesic pump. The flow rate of the pump was 2 mL/h with a bolus of 0.5 mL and 15 min of locking time. At the end of the operation, the PCA pump was inserted into the intravenous infusion tube. Sufentanil was routinely removed 48 h after the operation, and its cumulative use was recorded.
The visual analogue scale (VAS) was used to compare the analgesic effects of the two groups. The VAS scores were recorded at 0, 6, 12, 24, 36 and 48 h after the operation by those who did not know the grouping. The cumulative sufentanil, the recovery time for enterokinesia, the length of postoperative hospital stay, and the adverse reactions (nausea and vomiting) were recorded and compared between the two groups.
Statistical analyses were performed with SPSS 20.0 (SPSS Inc., Chicago, IL, United States). The measurement data are expressed as the mean ± SD. The t-test was used to compare the measurement data between the two groups, and the χ2 test was used to calculate the counting data. P < 0.05 was considered statistically significant.
All the operations were successfully completed, and all the patients recovered smoothly. Liver function recovered to normal status after the operation and all patients were discharged uneventfully. No complications such as bleeding or bile leakage occurred. The total incision length of the combined group was 8.194 ± 0.415 cm, while that of the control group was 7.992 ± 0.422 cm (P = 0.101). The operative times in the combined group and control group were 136.083 ± 11.836 min and 135.833 ± 11.484 min, respectively (P = 0.941). There were also no significant differences in age, gender, body weight, ASA grade, intraoperative bleeding, or maximum diameter of tumors between the two groups (Table 1).
The change tendency of VAS scores of the combined group and the control group were similar after operation. The VAS scores increased gradually, peaked at 24 h, and then decreased. At rest, the VAS scores of the combined group were significantly lower than those of the control group at 0, 6, 12, 24, and 36 h, while the VAS scores of the two groups had no significant difference at 48 h (Figure 1A). On movement, the VAS scores of the combined group were significantly lower than those of the control group at 0, 6, 12, and 24 h. The VAS score of the two groups had no significant difference at 36 and 48 h (Figure 1B). This indicated that the combination of parecoxib and ropivacaine could help patients get out of bed early and reduce their pain experience (Table 2).
| Characteristic | 0 h | 6 h | 12 h | 24 h | 36 h | 48 h |
| VAS score at rest | ||||||
| Combined group | 2.421 ± 0.568 | 2.24 ± 0.394 | 2.064 ± 0.215 | 1.984 ± 0.379 | 1.967 ± 0.152 | 1.997 ± 0.095 |
| Control group | 2.853 ± 0.566 | 2.619 ± 0.373 | 2.448 ± 0.24 | 2.233±0.353 | 2.398 ± 0.163 | 1.957 ± 0.108 |
| t | -2.636 | -3.427 | -5.824 | -2.353 | -9.456 | 1.349 |
| P-value | 0.011 | 0.001 | < 0.001 | 0.023 | < 0.001 | 0.184 |
| VAS score during movement | ||||||
| Combined group | 3.281 ± 0.451 | 3.375 ± 0.816 | 3.359 ± 0.492 | 3.176 ± 0.461 | 3.033 ± 0.538 | 2.967 ± 0.257 |
| Control group | 3.715 ± 0.41 | 3.49 ± 0.695 | 3.754 ± 0.614 | 3.764 ± 0.617 | 3.033 ± 0.61 | 3.061 ± 0.24 |
| t | -3.491 | -2.228 | -2.46 | -3.738 | -0.003 | -1.301 |
| P-value | 0.001 | 0.037 | 0.018 | 0.001 | 0.998 | 0.2 |
| Cumulative sufentanil (μg) | ||||||
| Combined group | - | 15.731 ± 2.472 | 30.315 ± 4.015 | 44.339 ± 6.361 | 60.661 ± 3.773 | 88.13 ± 7.49 |
| Control group | - | 15.288 ± 2.072 | 30.085 ± 5.884 | 50.408 ± 6.056 | 70.325 ± 5.423 | 94.01 ± 8.329 |
| t | - | 0.673 | 0.159 | -3.385 | -7.166 | -2.572 |
| P-value | - | 0.504 | 0.875 | 0.001 | < 0.001 | 0.013 |
The recovery time for enterokinesia in the combined group was 2.944 ± 0.896 d, which was significantly shorter than that in the control group (P < 0.001). Similarly, the length of hospital stay in the combined group was significantly shorter than that in the control group (P = 0.001). All these suggested that the combination of parecoxib and ropivacaine can promote the recovery of patients after operation (Table 3).
| Characteristic | Combined group | Control group | t | P-value |
| Recovery time for enterokinesia (d) | 2.944 ± 0.896 | 3.954 ± 0.944 | -3.804 | < 0.001 |
| PONA | 0.3345 | 0.8460 | ||
| No PONA | 13 | 11 | ||
| Nausea without vomiting | 6 | 7 | ||
| Nausea with vomiting | 5 | 6 | ||
| Hospital stay (d) | 8.625 ± 2.505 | 11.986 ± 3.908 | -3.548 | 0.001 |
Sufentanil at 1 μg/mL was delivered with an analgesic pump and any uncomfortable syndromes were monitored and recorded immediately. There was no significant difference in cumulative sufentanil at 6 and 12 h after operation, but there was a significant difference at 24, 36, and 48 h, especially at 24 and 36 h (Table 1, Figure 2). However, there was no significant difference in postoperative complications such as nausea and vomiting between the two groups (Table 3).
Since its inception in the 1990s, more than 3000 patients worldwide have undergone laparoscopic hepatectomy[9].Compared with the traditional open hepatectomy, the advantages are less bleeding, incision, and pain, faster recovery of gastrointestinal function, and shorter hospital stay[10,11]. Nevertheless, some patients after operation still suffer from visceral pain, wound prickling, shoulder pain, diaphragmatic abdominal pain, and other discomforts due to the visceral and incision trauma, carbon dioxide stimulation of abdominal visceral nerve and somatic nerve, intraoperative diaphragm traction, and other adverse factors[4,5]. Insufficient postoperative analgesia can affect the early mobilization, delay intestinal function recovery, prolong recovery time and hospital stays, delay wound healing, and increase the risk of venous thromboembolism. Conversely, effective analgesia after operation is particularly important for patients to promote the recovery of gastrointestinal function, reduce complications, and shorten the length of hospital stay. It is an important part of accelerated rehabilitation surgery[12].
Preemptive analgesia refers to taking certain measures to block the noxious stimulation and to reduce the sensitivity of the central nervous system and peripheral nervous system to these stimulations in order to relieve pain or postoperative analgesia, make the analgesic effect more obvious, and reduce the dosage of analgesics[13,14]. When the body tissues are traumatized, inflammatory mediators will be released. Prostaglandins are made through the conversion of arachidonic acid catalyzed by COX-2, which can directly lead to pain, increase the permeability of blood vessels, dilate blood vessels, create edema tissue, increase the sensitivity of effector receptors, and decrease the pain threshold, leading to peripheral hyperalgesia[15]. With the highly selective inhibitory action on COX-2, parecoxib blocks the synthesis of prostaglandins in peripheral and central regions, increases the pain threshold, inhibits hypersensitivity of pain threshold, and produces anti-inflammatory and analgesic effects. It has been reported recently that parecoxib has a good analgesic effect in laparoscopic hepatectomy[16]. However, parecoxib used in the above study was given after surgery. In our study, parecoxib was used 20 min before anesthesia induction. This not only achieved preemptive analgesic effects but also reduced the dosage of parecoxib, alleviating the side effects of medication to some extent.
Incision infiltration anesthesia is an effective and important component of multimodal postoperative analgesics, which is used in many types of surgery, including lumbar surgery, breast surgery, and inguinal hernia repair[17-19]. Local anesthetics used at the edge of the incision can block the influx of abdominal pain, reduce the sensitivity of spinal dorsal horn neurons, and provide an analgesic effect by inhibiting the spread of harmful impulses in the incision[20]. In addition, local anesthetics can inhibit local inflammation and pain receptor conduction and sensitivity in wound injury[21]. Ropivacaine, as a long-acting amide local anesthetic, is widely used in local anesthesia and postoperative analgesia. Its lipophilic reduction is related to the reduction of central nervous system toxicity and the incidence of cardiac toxicity[22]. Postoperative pain comes from the superficial structure of abdominal pain and peritoneal muscle and fascia structure, so local infiltration of ropivacaine can achieve long-term local analgesia. In this study, preoperative analgesia with parecoxib and local infiltration anesthesia with ropivacaine after operation were applied. The results showed that the combination of parecoxib and ropivacaine could effectively reduce the pain at rest and during movement after operation and promote the postoperative recovery, allowing for early discharge from the hospital. Moreover, in this study, using the Joel-Cohen incision could avoid transecting the abdominal muscles. This incision minimized the pain stimuli and considered the cosmetic results.
Opioids are commonly used intravenously for postoperative analgesia. Long-term use has potential addiction risks and serious side effects such as nausea, vomiting, constipation, respiratory depression, excessive sedation, and liver dysfunction[23]. Therefore, reducing the dosage and usage time of opioids is an appropriate way to avoid potential serious side effects. Our study showed that the cumulative sufentanil in the combined group decreased significantly. Meanwhile, the recovery time for enterokinesia in the combined group was shorter than that in the control group. This may be related to sufentanil inhibiting intestinal motility by binding to μ-2 and κ receptors in the intestine[24].
The sample size of this study is relatively small and needs to be included in future studies to further confirm the results of this study. In conclusion, preoperative intravenous injection of parecoxib combined with the long-acting local anesthetic ropivacaine for incision infiltration is a simple and effective method of postoperative analgesia to relieve postoperative pain and promote postoperative recovery after laparoscopic hepatectomy.
The analgesic effect of the preoperative intravenous injection of parecoxib combined with long-acting local anesthetic ropivacaine for incision infiltration in patients undergoing laparoscopic hepatectomy is still unknown.
Analgesic effect of parecoxib combined with ropivacaine in patients undergoing laparoscopic hepatectomy may be promising.
To study the analgesic effect of the preoperative intravenous injection of parecoxib combined with long-acting local anesthetic ropivacaine for incision infiltration in laparoscopic hepatectomy patients.
Laparoscopic hepatectomy patients were randomly divided into a combined group (parecoxib combined with ropivacaine) and a control group. The visual analogue scale (VAS) at rest and during movement was used to compare the analgesic effect of the two groups. The cumulative sufentanil, the recovery time for enterokinesia, the length of postoperative hospital stay, and the adverse reactions were recorded and compared between the two groups.
The VAS scores of the combined group were significantly lower than those of the control group. The recovery time for enterokinesia in the combined group was significantly shorter than that in the control group. The cumulative sufentanil in the combined group decreased significantly at 24, 36, and 48 h after operation.
Preoperative intravenous injection of parecoxib combined with the long-acting local anesthetic ropivacaine for incision infiltration is a simple and effective method for postoperative analgesia in laparoscopic hepatectomy patients. And it could relieve postoperative pain and promote postoperative recovery.
Injection of parecoxib combined with the long-acting local anesthetic ropivacaine for incision infiltration is useful for hepatectomy recovery.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sharma RA, Mayer RJ S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Reich H, McGlynn F, DeCaprio J, Budin R. Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991;78:956-958. [PubMed] |
| 2. | Abu Hilal M, Di Fabio F, Teng MJ, Lykoudis P, Primrose JN, Pearce NW. Single-centre comparative study of laparoscopic versus open right hepatectomy. J Gastrointest Surg. 2011;15:818-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 3. | Dagher I, Di Giuro G, Dubrez J, Lainas P, Smadja C, Franco D. Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg. 2009;198:173-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 146] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 4. | Wightman JA. A prospective survey of the incidence of postoperative pulmonary complications. Br J Surg. 1968;55:85-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 189] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Latimer RG, Dickman M, Day WC, Gunn ML, Schmidt CD. Ventilatory patterns and pulmonary complications after upper abdominal surgery determined by preoperative and postoperative computerized spirometry and blood gas analysis. Am J Surg. 1971;122:622-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 188] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Kelliher L, Jones C, Dickinson M, Scott M, Quiney N. Epidural anaesthesia and analgesia for liver resection. Anaesthesia. 2013;68:975-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Sun JX, Bai KY, Liu YF, Du G, Fu ZH, Zhang H, Yang JH, Wang B, Wang XY, Jin B. Effect of local wound infiltration with ropivacaine on postoperative pain relief and stress response reduction after open hepatectomy. World J Gastroenterol. 2017;23:6733-6740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 8. | Schug SA, Joshi GP, Camu F, Pan S, Cheung R. Cardiovascular safety of the cyclooxygenase-2 selective inhibitors parecoxib and valdecoxib in the postoperative setting: an analysis of integrated data. Anesth Analg. 2009;108:299-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 836] [Cited by in RCA: 877] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 10. | Goh BKP, Syn N, Teo JY, Guo YX, Lee SY, Cheow PC, Chow PKH, Ooi LLPJ, Chung AYF, Chan CY. Perioperative Outcomes of Laparoscopic Repeat Liver Resection for Recurrent HCC: Comparison with Open Repeat Liver Resection for Recurrent HCC and Laparoscopic Resection for Primary HCC. World J Surg. 2019;43:878-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Tsai KY, Chen HA, Wang WY, Huang MT. Long-term and short-term surgical outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma: might laparoscopic approach be better in early HCC? Surg Endosc. 2019;33:1131-1139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Ni TG, Yang HT, Zhang H, Meng HP, Li B. Enhanced recovery after surgery programs in patients undergoing hepatectomy: A meta-analysis. World J Gastroenterol. 2015;21:9209-9216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Raja S DC, Shetty AP, Subramanian B, Kanna RM, Rajasekaran S. A prospective randomized study to analyze the efficacy of balanced pre-emptive analgesia in spine surgery. Spine J. 2019;19:569-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Lieblich S. Pre-Emptive Analgesia. J Oral Maxillofac Surg. 2017;75:245-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Bajaj P, Ballary CC, Dongre NA, Baliga VP, Desai AA. Role of parecoxib in pre-emptive analgesia: comparison of the efficacy and safety of pre- and postoperative parecoxib in patients undergoing general surgery. J Indian Med Assoc. 2004;102:272, 274, 276-278. [PubMed] |
| 16. | Liu Y, Song X, Sun D, Wang J, Lan Y, Yang G, Meng F, Wang Y, Cui Y, Zhang B, Li X, Liu L. Evaluation of Intravenous Parecoxib Infusion Pump of Patient-Controlled Analgesia Compared to Fentanyl for Postoperative Pain Management in Laparoscopic Liver Resection. Med Sci Monit. 2018;24:8224-8231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Byager N, Hansen MS, Mathiesen O, Dahl JB. The analgesic effect of wound infiltration with local anaesthetics after breast surgery: a qualitative systematic review. Acta Anaesthesiol Scand. 2014;58:402-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Kjærgaard M, Møiniche S, Olsen KS. Wound infiltration with local anesthetics for post-operative pain relief in lumbar spine surgery: a systematic review. Acta Anaesthesiol Scand. 2012;56:282-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Scott NB. Wound infiltration for surgery. Anaesthesia. 2010;65 Suppl 1:67-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 20. | Brennan TJ, Zahn PK, Pogatzki-Zahn EM. Mechanisms of incisional pain. Anesthesiol Clin North Am. 2005;23:1-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 117] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 21. | Kawamata M, Takahashi T, Kozuka Y, Nawa Y, Nishikawa K, Narimatsu E, Watanabe H, Namiki A. Experimental incision-induced pain in human skin: effects of systemic lidocaine on flare formation and hyperalgesia. Pain. 2002;100:77-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Kuthiala G, Chaudhary G. Ropivacaine: A review of its pharmacology and clinical use. Indian J Anaesth. 2011;55:104-110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 207] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 23. | White PF. The changing role of non-opioid analgesic techniques in the management of postoperative pain. Anesth Analg. 2005;101:S5-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 306] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 24. | Ducrotté P, Caussé C. The Bowel Function Index: a new validated scale for assessing opioid-induced constipation. Curr Med Res Opin. 2012;28:457-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |