Published online Apr 6, 2023. doi: 10.12998/wjcc.v11.i10.2246
Peer-review started: January 20, 2023
First decision: February 10, 2023
Revised: February 28, 2023
Accepted: March 3, 2023
Article in press: March 3, 2023
Published online: April 6, 2023
Processing time: 69 Days and 7 Hours
Coronary artery stenosis (CAS) is the most common type of heart disease and the leading cause of death in both men and women globally. CAS occurs when the arteries that supply blood to the heart muscle harden and become narrower due to plaque buildup - cholesterol and other material - on their inner walls. As a result, the heart muscle cannot receive the blood or oxygen it needs. Most heart attacks happen when a blood clot suddenly cuts off the hearts' blood supply, causing permanent heart damage.
To analyze the relationship between the left ventricular ejection fraction (LVEF), left ventricular strain (LVS), and coronary stenosis.
A total of 190 participants were enrolled in this trail. The control group comprised 93 healthy individuals, and observation group comprised 97 patients with coronary heart disease who were hospitalized between July 2020 and September 2021. Coronary lesions were assessed using the Gensini score, and the LVEF and LVS were measured using magnetic resonance imaging (MRI). The interaction between the LVEF and LVS was examined using a linear regression model. The relationship between LVEF and coronary stenosis was examined using Spear
The LVEF of the observation group was lower than that of the control group. The left ventricular end-systolic volume (LVESV) and left ventricular end-diastolic volume (LVEDV) of the observation group were significantly higher than those of the control group (P < 0.05). The longitudinal and circumferential strains (LS, CS) of the observation group were significantly higher than those of the control group; however, the radial strain (RS) of the observation group was significantly lower than that of the control group (P < 0.05). LVS, LS, and CS were significantly negatively correlated with the LVEF, and RS was positively correlated with the LVEF. There were significant differences in the LVEF, LVESV, and LVEDV of patients with different Gensini scores; the LVEF significantly decreased and the LVESV and LVEDV increased with increasing Gensini scores (P < 0.05). In the observation group, the LVEF was negatively correlated and the LVESV and LVEDV were positively correlated with coronary stenosis (P < 0.05).
The LVEF measured using MRI is significantly linearly correlated with LVS and negatively correlated with coronary stenosis.
Core Tip: This study aimed to analyze the relationship between the left ventricular ejection fraction (LVEF), left ventricular strain (LVS), and coronary artery stenosis (CAS), 93 healthy individuals were selected as the control group, while 97 patients with coronary heart disease were selected as the observation group. Through the analysis of the Gensini score, magnetic resonance imaging, a linear regression model, and Spearman’s correlation, we found that LVEF is significantly linearly correlated with LVS and negatively correlated with CAS.
- Citation: Gui HY, Liu SW, Zhu DF. Interaction between the left ventricular ejection fraction and left ventricular strain and its relationship with coronary stenosis. World J Clin Cases 2023; 11(10): 2246-2253
- URL: https://www.wjgnet.com/2307-8960/full/v11/i10/2246.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i10.2246
Coronary artery stenosis (CAS) is a common clinical disease. As the condition worsens, myocardial cells are damaged to varying degrees, resulting in abnormal myocardial blood perfusion and changes in ventricular function and structure[1]. Therefore, a timely and effective clinical evaluation of the left ventricular function is necessary to assess the risk of coronary heart disease[2]. Currently, magnetic resonance imaging (MRI) is widely used in clinical practice as a non-invasive examination method because it can effectively assess the function and structure of the left ventricle and coronary arteries[3]; thus, MRI has gradually become the gold standard for this purpose[4]. However, there are few clinical studies on the correlation between left ventricular ejection fraction (LVEF) and other cardiac function indicators. Therefore, this study included patients with coronary heart disease admitted to our hospital and analyzed the relationship between the LVEF measured using MRI, left ventricular strain (LVS), and coronary stenosis.
This study was approved by the ethics committee of Harbin No. 4 Hospital. The observation group comprised 97 patients with coronary heart disease who were hospitalized between July 2020 and September 2021, while the control group comprised 93 healthy individuals. The observation group included 52 men and 45 women (age, 56.21 ± 7.32 years; heart rate, 64.93 ± 6.33 beats/min), while the control group included 51 men and 42 women (age, 55.91 ± 8.13 years; heart rate, 64.56 ± 7.43 beats/min). The clinical data of the groups were comparable, with no discernible differences (P > 0.05). The inclusion criteria were as follows: (1) Fulfilled the coronary computed tomography angiography diagnostic criteria for coronary heart disease; (2) available imaging results with satisfactory image quality; (3) no history of coronary intervention; and (4) provided a signed informed consent form. The exclusion criteria were as follows: (1) Congenital heart disease or valvular heart disease; (2) severe arrhythmia; (3) cardiomyopathy; (4) liver and kidney insufficiency; (5) history of hypertension (grade 3 or higher); and (6) pregnancy or breastfeeding.
All participants were examined using a Philips Ingenia 3.0 T MRI machine with a 12-channel phased-array coil while in the supine decubitus position. Sagittal, coronal, and axial scans were performed. The four-chamber long-axis view, two-chamber view, short-axis view, and the entrance and exit of the left ventricle were obtained; the heart axis was centered during imaging. The images of each slice were collected at the end of expiration, and the steady-state free precession (SSFP) scanning parameters were as follows: Left ventricular short-axis slice thickness, 8 mm; echo time (TE), 1.7 ms; repetition time (TR), 51.5 ms; field of view (FOV), 340 mm × 360 mm; matrix, 256 × 192; flip angle, 70°; and total number of plies, 8 to 10. Delayed enhanced images were obtained using Gd-DTPA as the contrast agent, which was injected via the peripheral vein with a high-pressure syringe at a rate of 4 mL/s; the contrast agent dose was 0.2 mmol/kg. An equal volume of physiological saline was also injected at the same rate. At 7 min after the injection, phase-sensitive inversion recovery (left ventricular short-axis thickness, 8 mm; TE, 2.6 ms; TR, 750 ms; FOV, 340 mm × 360 mm; matrix, 256 × 192) was performed. The inversion time (TI) was determined in real time according to the darkest layer of the myocardium. A total of 8 to 10 Layers were collected, and the slices were the same as those used for SSFP.
All images were transmitted to the supporting workstation. Two radiologists with more than 3 years of experience judged the results and post-processed the images. Using the post-processing standards published by the American Cardiovascular Magnetic Resonance Committee, the epicardium and endocardium were delineated using the SSFP images to determine the LVEF, left ventricular end-systolic volume (LVESV), and left ventricular end-diastolic volume (LVEDV). Patients with coronary artery lesions were evaluated using the Gensini score and CAS scoring standards [5]. Scores based on the degree of stenosis were as follows: 1%–25%, 1 point; > 25%–50%, 2 points; > 50%–75%, 4 points; > 75%–90%, 8 points; > 90%–< 100%, 16 points; and 100%, 32 points. Scores based on the lesion site were scored as follows: left main artery, 5 points; left anterior descending branch or proximal circumflex branch, 2.5 points; intermediate section of the left anterior descending artery, 1.5 points; distal segment of the left anterior descending artery, 1 point; intermediate and distal segments of the left circumflex artery, 1 point; right coronary artery, 1 point; and small branches, 0.5 points. The total score was the sum of the stenosis degree and lesion site scores, and patients were categorized as follows: score ≤ 30, mild disease group; score > 30–60, moderate disease group; and score > 60, severe disease group. Supporting software of Philips Ingenia 3.0T magnetic resonance instrument was used to detect myocardial strain parameters, and the epicardial and endocardial displacements were automatically tracked to quantify the left ventricular myocardial motion and analyze three-dimensional longitudinal strain (LS), circumferential strain (CS), and radial strain (RS).
Statistical analysis was performed using SPSS version 20.0 (Armonk, NY: IBM Corp). The enumeration data were expressed as percentages, and χ2 test for comparisons. The measurement data of the two groups were expressed as the mean ± SD, and a t-test was used for comparisons. Differences in measurement data among multiple groups were evaluated using an analysis of variance. The linear regression model was used to analyze the interaction between the LVEF and LVS. Spearman’s correlation was used to analyze the relationship between LVEF and coronary stenosis. P < 0.05 indicated a statistically significant difference.
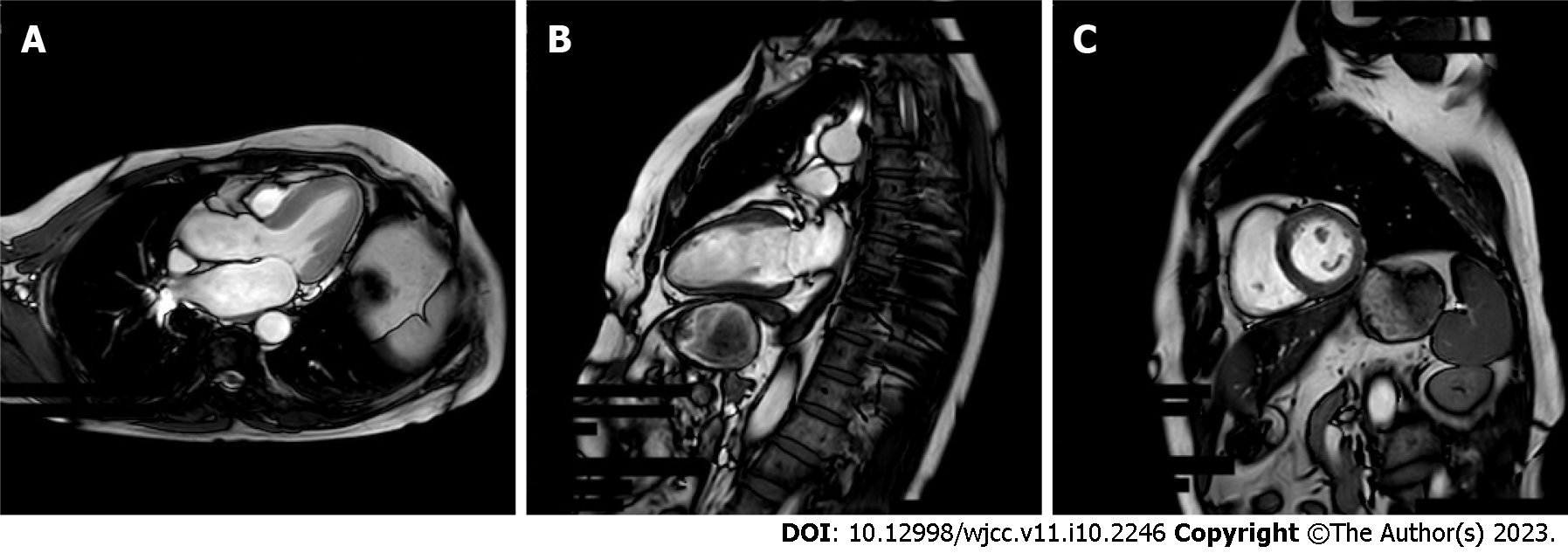
The LVESV and LVEDV of the observation group were substantially greater than those of the control group; however, the LVEF of the observation group was lower than that of the control group (P < 0.05; Table 1). The typical case diagram is shown in Figure 1.
| Group | Participants | LVEF, % | LVESV, mL | LVEDV, mL |
| Observation | 97 | 44.19 ± 9.71 | 88.51 ± 17.52 | 147.32 ± 18.32 |
| Control | 93 | 66.92 ± 10.23 | 33.64 ± 10.23 | 100.03 ± 23.19 |
| t value | 15.713 | 26.215 | 15.613 | |
| P value | 0.000 | 0.000 | 0.000 |
The LS and CS of the observation group were much greater than those of the control group; however, the RS of the observation group was lower than that of the control group (P < 0.05; Table 2).
| Groups | Participants | LS, % | CS, % | RS, % |
| Observation | 97 | -11.21 ± 3.87 | -14.85 ± 5.96 | 31.44 ± 10.45 |
| Control | 93 | -15.43 ± 2.42 | -19.83 ± 4.09 | 45.43 ± 6.12 |
| t value | 8.969 | 6.684 | 11.194 | |
| P value | 0.000 | 0.000 | 0.000 |
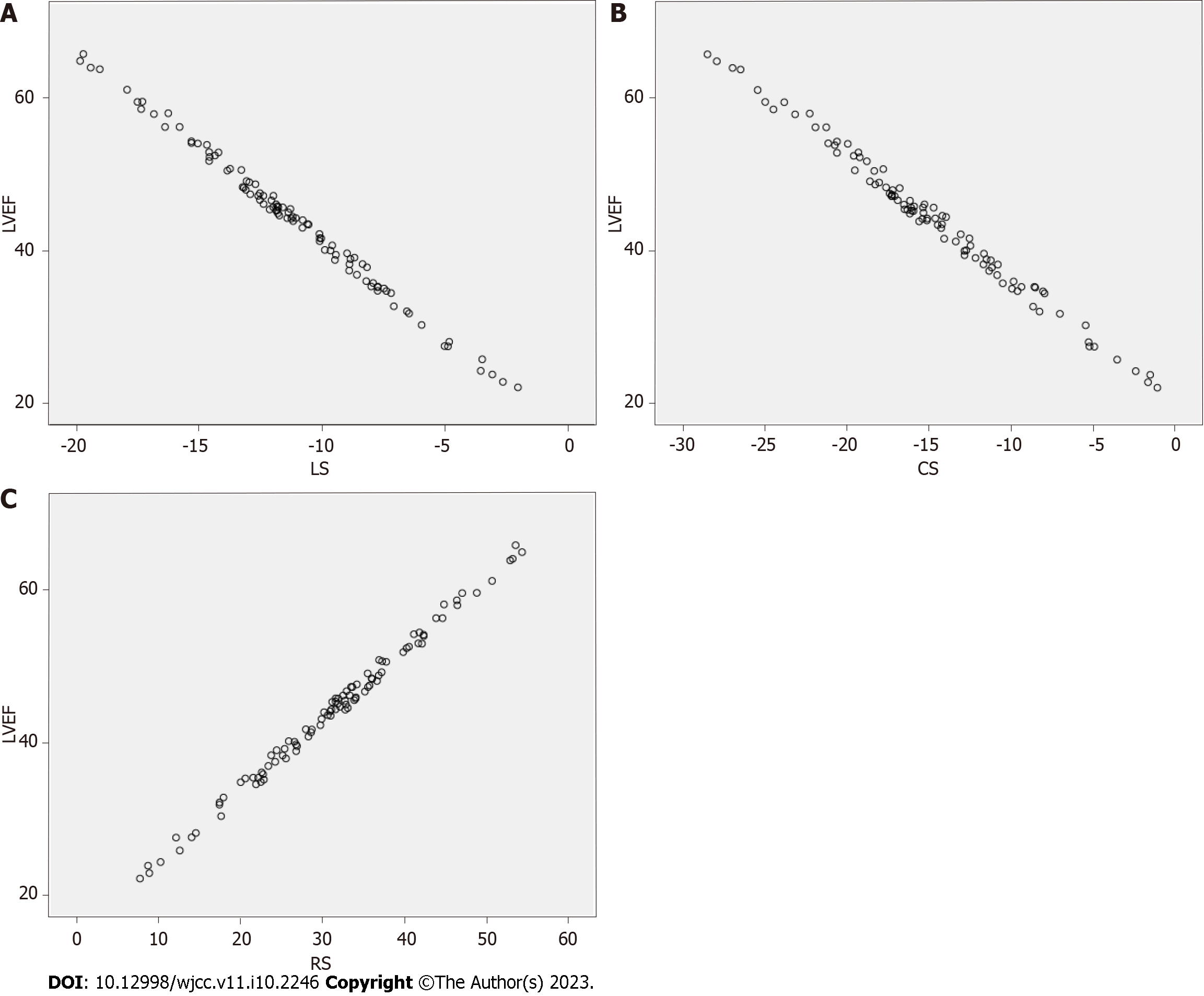
The LVS, LS, and CS were significantly negatively correlated with the LVEF, and the RS was significantly positively correlated with the LVEF (Table 3, Figure 2).
| Independent variable | Model | R2 |
| LS | y = -2.5269x + 17.285 | 0.9805 |
| CS | y = -1.6514x + 21.462 | 0.9836 |
| RS | y = 0.9325x + 16.356 | 0.9848 |
There were significant differences in the LVEF, LVESV, and LVEDV of patients with different Gensini scores. The LVEF significantly decreased and the LVESV and LVEDV significantly increased with increasing Gensini scores (P < 0.05; Table 4).
| Gensini score | Participants | LVEF, % | LVESV, mL | LVEDV, mL |
| < 5 | 12 | 54.93 ± 8.12 | 70.94 ± 15.34 | 125.49 ± 17.43 |
| 5–< 25 | 41 | 45.67 ± 7.92 | 85.21 ± 17.83 | 142.85 ± 12.93 |
| ≥ 25–< 60 | 36 | 40.88 ± 8.87 | 95.09 ± 13.21 | 155.93 ± 16.54 |
| ≥ 60 | 8 | 35.39 ± 9.05 | 102.17 ± 11.09 | 164.23 ± 13.82 |
| F value | 11.755 | 10.027 | 17.025 | |
| P value | 0.000 | 0.000 | 0.000 |
In the observation group, the LVEF (r = -0.754) was significantly negatively correlated with and the LVESV (r = -0.682) and LVEDV (r = 0.701) were significantly positively correlated with coronary stenosis (P < 0.05).
Coronary heart disease is a prevalent clinical illness and major cause of disability and death[6]. Patients with coronary heart disease often have coronary obstruction or stenosis, which can lead to angina pectoris and myocardial infarction, reduce cardiac compliance, and cause heart failure and cardiac enlargement[7,8]. Moreover, when CAS exceeds 40%, the blood flow reserve function is significantly reduced; furthermore, when the degree of vascular stenosis exceeds 75%, the coronary resting blood flow decreases significantly because of increased vascular stenosis, resulting in impaired myocardial contractility[9]. Although coronary angiography has been used as the gold standard for evaluating and analyzing coronary heart disease, clinical use and patient acceptance rates are low because of its invasiveness[10,11]. Furthermore, the rapid development of medical science has resulted in the development of additional methods of evaluating left ventricular function. For example, MRI is a non-invasive method that is widely used in clinical practice, and it is one of the most accurate methods of evaluating the left ventricular volume[12].
The LVEF, LVEDV, and LVESV are the main indicators of the ability of the heart to pump blood; furthermore, they are important for evaluating coronary heart disease and predicting the survival rate of such patients[13,14]. The LVEF is the ratio of the left ventricular stroke volume to the end-diastolic volume, and it is one of the core values used for the basic evaluation of cardiac function in clinical practice[15]. MRI is the gold standard for assessing the LVEF and left ventricular function in clinical practice[16]. Myocardial strain, which has received much attention, is a quantitative measurement used to analyze myocardial deformation and to evaluate changes in the myocardial segment length[7]: positive myocardial strain indicates prolonged myocardial thickening, while negative myocardial strain indicates that the myocardium is thinning and shortening. Myocardial strain is expressed as a percentage[17]. Tissue tracking technology can be used to calculate myocardial strain during cardiac MRI and echocardiography; these results have good reproducibility and high clinical value[18]. The LS and CS of the observation group were higher than those of the control group; however, the RS of the observation group was lower than that of the control group. The results of the linear regression model analysis showed that LVS, LS, and CS were significantly inversely correlated with the LVEF; however, the RS was positively correlated with the LVEF. Further analysis demonstrated that the LVEF of the observation group was lower than that of the control group; however, the LVESV and LVEDV of the observation group were higher than those of the control group. Patients with different degrees of coronary stenosis had significantly different LVEF, LVESV, LVEDV, and Gensini scores. The LVEF significantly decreased and the LVESV and LVEDV increased with increasing Gensini scores. In the observation group, the LVEF was significantly negatively correlated with and the LVESV and LVEDV were positively correlated with coronary stenosis. This research suggested that the degree of coronary artery disease can be systematically estimated by using MRI to detect the LVEF. Myocardial ischemia and hypoxia in patients with CAS induce degeneration and necrosis of myocardial cells and lead to impaired myocardial contractility[19]. With weakened myocardial contractility of the left atrium, the ejection capacity decreases, which causes blood to remain in the left atrium and left ventricle, resulting in increased end-systolic and end-diastolic volumes, left ventricular remodeling, and reduced cardiac systolic function. Therefore, the LVEF decreased significantly with increasing Gensini scores.
The LVEF, when measured using MRI, showed a significant linear correlation with LVS and a negative correlation with coronary stenosis. This study did not conduct a long-term follow-up of the patients, and did not include patients from other institutions. Therefore, further exploration and research are necessary in this regard.
Coronary artery stenosis (CAS) is a common term for the buildup of plaque in the heart’s arteries that could lead to a heart attack. However, the relationship between various cardiac function indicators and CAS is rarely studied.
CAS is one of the major cardiovascular diseases affecting humans worldwide. This disease has been shown to be the leading cause of death in both developed and developing countries. Exploring the correlation between cardiac function indicators and CAS will benefit the patients.
The purpose of our study was to analyze the correlation between the left ventricular ejection fraction (LVEF), left ventricular strain (LVS), and coronary stenosis.
The control group comprised 93 healthy individuals, while the observation group comprised 97 patients with coronary artery disease who were hospitalized between July 2020 and September 2021. Coronary artery disease was assessed using the Gensini score, and LVEF and LVS were measured using magnetic resonance imaging. The interaction between LVEF and LVS was investigated using a linear regression model, while the relationship between LVEF and CAS was examined using Spearman’s correlation.
The LVEF of the observation group was lower than that of the control group. The left ventricular end-systolic volume (LVESV) and left ventricular end-diastolic volume (LVEDV) of the observation group were significantly higher than those of the control group. The longitudinal strain (LS) and circumferential strain (CS) of the observation group were significantly higher than those of the control group; however, the radial strain (RS) of the observation group was lower than that of the control group. LVS, LS, and CS were significantly negatively correlated with the LVEF, while RS was positively correlated with the LVEF. There were significant differences in the LVEF, LVESV, and LVEDV of patients with different Gensini scores. The LVEF significantly decreased and the LVESV and LVEDV increased with increasing Gensini scores. In the observation group, the LVEF was negatively correlated and the LVESV and LVEDV were positively correlated with coronary stenosis.
The LVEF showed a significant linear correlation with LVS and negative correlation with coronary stenosis.
This study did not follow patients over time and did not include patients from other institutions. Therefore, further exploration and research are necessary.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jeon Y, South Korea; Kaneko T, Japan S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Pewowaruk RJ, Barton GP, Johnson C, Ralphe JC, Francois CJ, Lamers L, Roldán-Alzate A. Stent interventions for pulmonary artery stenosis improve bi-ventricular flow efficiency in a swine model. J Cardiovasc Magn Reson. 2021;23:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Calin A, Mateescu AD, Popescu AC, Bing R, Dweck MR, Popescu BA. Role of advanced left ventricular imaging in adults with aortic stenosis. Heart. 2020;106:962-969. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Marques-Alves P, Marinho AV, Teixeira R, Baptista R, Castro G, Martins R, Gonçalves L. Going beyond classic echo in aortic stenosis: left atrial mechanics, a new marker of severity. BMC Cardiovasc Disord. 2019;19:215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Ando K, Nagao M, Watanabe E, Sakai A, Suzuki A, Nakao R, Ishizaki U, Sakai S, Hagiwara N. Association between myocardial hypoxia and fibrosis in hypertrophic cardiomyopathy: analysis by T2* BOLD and T1 mapping MRI. Eur Radiol. 2020;30:4327-4336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Wang BL, Li HJ, Wu YA, Dai WR, Li YH, Guo W, Pan BS. [Correlation between serum biochemical parameters and the degree of coronary artery stenosis in patients with coronary heart disease]. Jianyan Yixue. 2020;35:12-16. [DOI] [Full Text] |
| 6. | Isaza N, Desai MY, Kapadia SR, Krishnaswamy A, Rodriguez LL, Grimm RA, Conic JZ, Saijo Y, Roselli EE, Gillinov AM, Johnston DR, Svensson LG, Griffin BP, Popović ZB. Long-Term Outcomes in Patients With Mixed Aortic Valve Disease and Preserved Left Ventricular Ejection Fraction. J Am Heart Assoc. 2020;9:e014591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Zhang LJ, Tian JF, Yang XY, Xu L, He Y, Song XT. [Clinical value of left ventricular strain analysis by cardiovascular magnetic resonance in patients with coronary chronic total occlusion]. Zhonghua Xin Xue Guan Bing Za Zhi. 2021;49:601-609. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Roumeliotis AG, Power D, Reisman AM, Sartori S, Cao D, Zhang Z, Chiarito M, Chandiramani R, Nicolas J, Goel R, Claessen B. E, Sweeny J, Dangas GD, Mehran R, Kini AS, Sharma SK. TCT CONNECT-307 Long-Term Outcomes After Coronary Intervention With Drug Eluting Stents for Unprotected Left Main Coronary Artery Stenosis According to Diabetes Mellitus Status. J Am Coll Cardiol. 2020;76:B132. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Zuo WJ, Yang MM, Chen YF, Xie AM, Chen LJ, Ma GS. [Analysis of factors related to functional ischemia based on FFR and its diagnostic value]. Linchuang Xinxueguanbing Zazhi. 2019;35:55-59. [DOI] [Full Text] |
| 10. | Dhillon AS, Narayanan MR, Tun H, Hindoyan A, Matthews R, Mehra A, Shavelle DM, Clavijo LC. In-Hospital Outcomes of Rotational Atherectomy in High-Risk Patients With Severely Calcified Left Main Coronary Artery Disease: A Single-Center Experience. J Invasive Cardiol. 2019;31:101-106. [PubMed] |
| 11. | Jerzy S, Krawczyk K, Gierlotka M. Fully percutaneous insertion and removal of the Impella CP via a subclavian approach. Postepy Kardiol Interwencyjnej. 2020;16:343-346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Yuan JH, Yang J. [The value of MRI and ultrasound in evaluating left ventricular function in patients with hypertension and ventricular hypertrophy]. Zhongguo CT he MRI Zazhi. 2019;17:40-43. [DOI] [Full Text] |
| 13. | Wang J, Shi K, Xu HY, Zhao Q, Liu X, Gao Y, Yu H, Guo YK, Yang ZG. Left Ventricular Deformation in Patients with Connective Tissue Disease: Evaluated by 3.0T Cardiac Magnetic Resonance Tissue Tracking. Sci Rep. 2019;9:17913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Kitano T, Nabeshima Y, Otsuji Y, Negishi K, Takeuchi M. Accuracy of Left Ventricular Volumes and Ejection Fraction Measurements by Contemporary Three-Dimensional Echocardiography with Semi- and Fully Automated Software: Systematic Review and Meta-Analysis of 1,881 Subjects. J Am Soc Echocardiogr. 2019;32:1105-1115.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 15. | Le TT, Ang BWY, Bryant JA, Chin CY, Yeo KK, Wong PEH, Ho KW, Tan JWC, Lee PT, Chin CWL, Cook SA. Multiparametric exercise stress cardiovascular magnetic resonance in the diagnosis of coronary artery disease: the EMPIRE trial. J Cardiovasc Magn Reson. 2021;23:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Chang MC, Wu MT, Weng KP, Chien KJ, Lin CC, Su MY, Lin KL, Chang MH, Peng HH. Biventricular myocardial adaptation in patients with repaired tetralogy of Fallot: Mechanistic insights from magnetic resonance imaging tissue phase mapping. PLoS One. 2020;15:e0237193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Schwaiger JP, Reinstadler SJ, Tiller C, Holzknecht M, Reindl M, Mayr A, Graziadei I, Müller S, Metzler B, Klug G. Baseline LV ejection fraction by cardiac magnetic resonance and 2D echocardiography after ST-elevation myocardial infarction - influence of infarct location and prognostic impact. Eur Radiol. 2020;30:663-671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Kordalis AA, Gatzoulis KA, Arsenos PP, Tsiachris DL, Tsioufis CP. Magnetic Resonance for Risk Stratification of Coronary Artery Disease Patients: Toward an Electrophysiology-Guided Approach? J Am Coll Cardiol. 2021;77:2157. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Brown J, Coulthard A, Dixon AK, Dixon JM, Easton DF, Eeles RA, Evans DG, Gilbert FG, Hayes C, Jenkins JP, Leach MO, Moss SM, Padhani AP, Pointon LJ, Ponder BA, Sloane JP, Turnbull LW, Walker LG, Warren RM, Watson W; UK MRI Breast Screening Study Advisory Group. Rationale for a national multi-centre study of magnetic resonance imaging screening in women at genetic risk of breast cancer. Breast. 2000;9:72-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |