Published online Mar 26, 2022. doi: 10.12998/wjcc.v10.i9.2733
Peer-review started: July 12, 2021
First decision: December 17, 2021
Revised: December 27, 2021
Accepted: February 19, 2022
Article in press: February 19, 2022
Published online: March 26, 2022
Processing time: 253 Days and 2.3 Hours
Despite advances in medical therapy for Crohn’s disease (CD), most patients with CD require repeated resection surgeries.
To analyze the perforating and nonperforating indications of repeated CD operations and identify the anastomosis characteristics for postoperative CD.
We retrospectively reviewed 386 patients who underwent at least one resection for CD between 2003 and 2013.Clinical characteristics of each surgery were collected. Univariate and multivariate analyses were performed to determine risk factors for recurrence.
The indication for reoperation in CD tends to be the same as that for primary operation, i.e., perforating disease tends to represent as perforating disease and nonperforating as nonperforating. Concordance was found between the first surgery and second surgery in terms of the indication for the operation (P = 0.006), and the indication for the third surgery was also correlated with that for the second surgery (P = 0.033). Even if the correlation of surgical indications between repeated operations, the rate of perforating indication for the second and third surgeries was significantly higher than that of the first surgery. In addition, the presence of perforating CD was a predictor of recurrence for both the first and second surgeries. Moreover, anastomotic lesions were the most common sites of recurrence after the operation. Based on the importance of anastomosis, anastomosis might be a new type of disease location for the classification of postoperative CD.
CD not only has stable characteristics but also progresses chronically. Perforation is a progressive surgical indication for Crohn’s disease. For CD after surgery, anastomosis may be a new classification of disease location.
Core Tip: It was well-known that Crohn’s disease (CD) is a chronic disease characterized by progressive bowel destruction. Our findings suggest that CD becomes more severe and more extensive with the increase in number of surgeries. CD not only has stable characteristics, but also progresses chronically. Perforation is a progressive surgical indication for CD. For CD after operation, anastomosis may be a new classification of disease location.
- Citation: Shen WS, Huang XH, Liu RQ, Li CY, Li Y, Zhu WM. Perforating and nonperforating indications in repeated surgeries for Crohn’s disease. World J Clin Cases 2022; 10(9): 2733-2742
- URL: https://www.wjgnet.com/2307-8960/full/v10/i9/2733.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i9.2733
Crohn’s disease (CD) is a chronic inflammatory bowel disease (IBD) of unknown etiology; it is extremely difficult to predict the clinical course of CD patients. In recent years, the incidence of CD has increased dramatically in China[1]. Despite advances in medical therapy for CD (such as antitumor necrosis factor antibodies and immunosuppressive drugs), antitumor necrosis factor antibodies can effectively promote the healing of intestinal mucosa and reduce the operation risk and hospitalization rate. However, in clinical practice, up to 30% of patients have a loss of response to biological therapy. Most CD patients still require partial bowel resection at least once during the CD course[2,3].
Surgical intervention is necessary for patients with acute perforation, internal fistulae, peritoneal abscess, intestinal obstruction, toxic dilatation, hemorrhage, and/or failed response to medical therapy[4]. Surgery is effective in removing the lesions and relieving symptoms; however, surgical resection is not curative for CD, and postoperative recurrence is common. Recurrence may occur in 25%-38% of CD patients, necessitating a second surgery within 5 years postoperatively. Moreover, a third surgery owing to recurrent CD is required in an estimated 33% of these patients[5]. Postoperative prophylaxis can reduce CD recurrence rates[6], but only patients with risk factors for earlier postoperative recurrence should be considered for postoperative prophylaxis due to the risks of immunosuppressive therapy. Therefore, to delay postoperative recurrence, it is important to analyze the clinical characteristics and predict postoperative recurrence for surgical patients. Several studies have assessed the risk factors for postoperative CD recurrence. Reported risk factors for postoperative recurrence include a smoking habit, family history, young age at diagnosis, ileocolonic disease, perianal disease, preoperative duration and perforating lesions[7-10].
The aim of the current study was to compare the clinical characteristics between the first, second and third surgeries, analyze correlations of the perforating and nonperforating indications, and identify the anastomosis characteristics for postoperative CD.
Data were retrospectively reviewed from CD patients treated between 2003 and 2013 in Jinling Hospital, Medical School of Nanjing University. All included patients were preoperatively diagnosed with CD based on conventional clinical features, abdominal computed tomography, and endoscopy, and the CD diagnosis was postoperatively confirmed by histological analysis of the surgical specimen. Patients who had undergone at least one surgical resection for CD were considered for study enrollment. Endoscopies were performed at 3 mo, 6 mo and every year after surgery. All patients were contacted by telephone and asked to participate in the study. All patients gave informed written consent. This study was approved by the Jinling Hospital Ethics Committee.
Patient age and disease location were based on the Montreal classification[11]. Indication for surgery was defined as the main reason for surgical resection based on clinical features, preoperative diagnostic examinations, and intraoperative findings. The indications were classified into two categories based on the report by Simillis et al[12] perforating indications included acute free perforation, internal or external fistula, and abscess; nonperforating indications included intestinal obstruction, medical intractability, and hemorrhage. Recurrence was defined as the need for reoperative surgery.
Clinical characteristics, including age at diagnosis, sex, age at the time of surgery, appendectomy history, preoperative duration, smoking history, perianal disease, indication for surgery, and disease location, were retrospectively collected for each patient by two independent individuals (W.S. and X.H.). We also collected operative records, including resection range and occurrence of postoperative intra-abdominal septic complications (IASCs). Serum albumin, C-reactive protein, and BMI were also collected after patient admission. The deadline for follow-up was February 2017. All patients were followed-up at regular intervals.
Statistical analysis was performed using SPSS version 19.0 (Chicago, IL, United States). Correlations of clinical characteristics between the repeated surgeries were tested for statistical significance using Pearson’s χ2 test. The paired-samples t-test was used to assess differences in recurrence-free survival after the first and second surgeries. For analysis of recurrence-free survival data related to perforating indication, cumulative survival curves were created using the Kaplan–Meier method; the difference between the curves was analyzed by the log-rank test. Univariate and multivariate survival analyses were carried out using the Cox proportional hazards model. Spearman’s correlation coefficient test was used to assess associations of perforating indications for multiple operations. A value of P < 0.05 was considered statistically significant, and all P values were two-sided.
There were 386 hospitalized patients who had undergone at least one surgical resection in our department; 155 of these patients had undergone two surgical resections, and 41 of these 155 patients had undergone at least three surgical resections. A final total of 386 CD patients were included in this study. The clinical features are shown in Table 1. There were no significant differences between surgeries in sex, appendectomy history, smoking history, perianal disease or IASCs (P > 0.05).
| First surgery (n = 386), % | Second surgery (n = 155), % | Third surgery (n = 41), % | P value | |
| Sex | 0.405 | |||
| Man | 290 (76.69) | 124 (80.00) | 33 (80.49) | |
| Female | 96 (23.31) | 31 (20.00) | 8 (19.51) | |
| Age (year) | 0.037 | |||
| A1 (≤ 16) | 5 (1.30) | 2 (1.29) | 0 (00.00) | |
| A2 (17-40) | 264 (68.39) | 92 (59.35) | 20 (48.78) | |
| A3 (> 40) | 117 (30.31) | 61 (39.35) | 21 (51.22) | |
| Appendectomy | 0.152 | |||
| Yes | 76 (19.69) | 37 (23.87) | 13 (31.70) | |
| No | 310 (80.31) | 118 (76.13) | 28 (68.29) | |
| Smoking history | 0.576 | |||
| Never smoker | 320 (82.90) | 128 (82.58) | 37 (90.24) | |
| Past smoker | 49 (12.69) | 23 (14.84) | 3 (7.32) | |
| Active smoker | 17 (4.40) | 4 (2.58) | 1 (2.44) | |
| Preoperative treatment | ||||
| Immunomodulator | 97 (25.13) | 48 (30.97) | 12 (29.27) | 0.362 |
| Enteral Nutrition | 178 (46.11) | 80 (51.61) | 16 (39.02) | 0.288 |
| 5-aminosalicylates | 32 (8.29) | 23 (14.84) | 4 (9.76) | 0.074 |
| Corticosteroids | 49 (12.69) | 30 (19.35) | 7 (17.07) | 0.130 |
| Infliximab | 8 (2.07) | 5 (3.23) | 1 (2.44) | 0.743 |
| Perianal disease | 0.265 | |||
| Yes | 73 (16.77) | 39 (25.16) | 9 (21.95) | |
| No | 313 (83.22) | 116 (74.84) | 32 (78.05) | |
| Indication for surgery | 0.004 | |||
| Free perforation | 65 (16.83) | 9 (5.81) | 2 (4.87) | |
| Fistula or abscess | 107 (27.72) | 78 (50.32) | 25 (60.97) | |
| Obstruction | 162 (41.96) | 57 (36.77) | 10 (24.39) | |
| Medical intractability | 41 (10.62) | 5 (3.23) | 1 (2.44) | |
| Hemorrhage | 11 (2.85) | 6 (3.87) | 3 (7.32) | |
| Location | 0.028 | |||
| L1 (ileal) | 145 (37.56) | 56 (36.13) | 10 (24.39) | |
| L2 (colonic) | 47 (12.18) | 7 (4.52) | 5 (12.20) | |
| L3 (ileocolonic) | 194 (50.26) | 92 (59.35) | 26 (63.41) | |
| IASCs | 0.569 | |||
| Yes | 27 (6.99) | 15 (9.68) | 3 (7.32) | |
| No | 359 (93.01) | 140 (90.32) | 38 (92.68) |
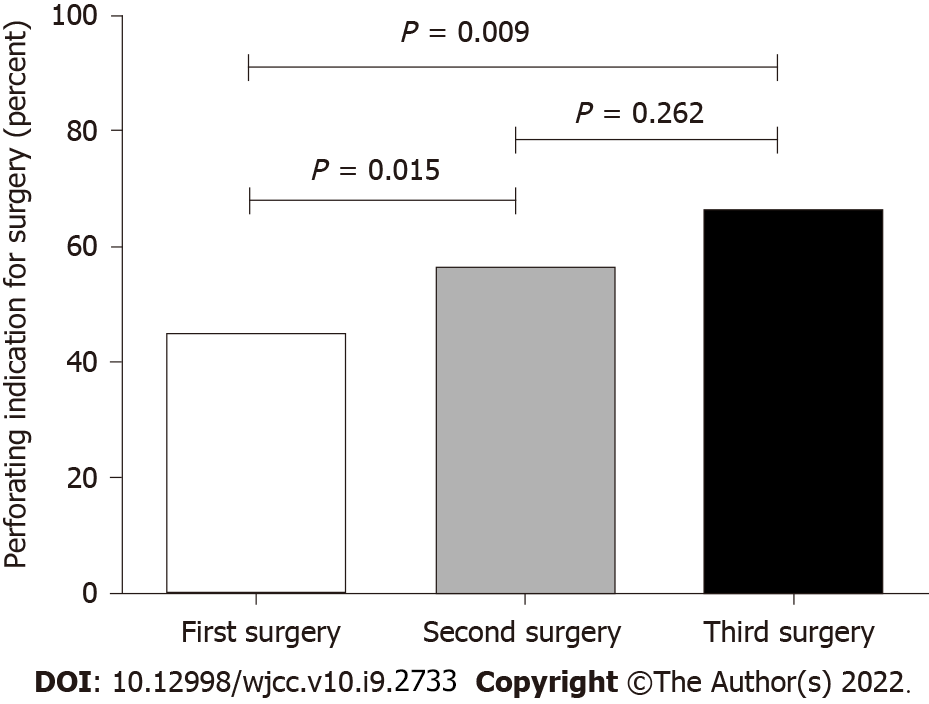
The perforating and nonperforating indications of the initial surgery were correlated with the surgical indication of the second surgery (P = 0.006, r = 0.220), and the surgical indication of the second surgery was also correlated with that of the third surgery (P = 0.033, r = 0.334) (Figure 1). Perforating disease tends to represent as perforating disease and nonperforating as nonperforating. Even with the correlation of surgical indications between repeated operations, the rate of CD perforation behavior as an indication for the second and third surgeries was significantly higher than that for the first surgery (Figure 2). Therefore, although CD can retain disease behavior after surgery, CD is a chronic disease characterized by progressive bowel destruction and will eventually develop a perforation. CD not only has stable characteristics but also progresses chronically.
After the first surgery, perforating indication (HR 1.456, 95%CI 1.051-2.016) and preoperative disease duration (HR 1.003, 95%CI 1.000-1.006) were significantly associated with recurrence-free survival in the univariate analysis. In multivariate analysis, only perforating indication significantly affected the outcome of recurrence and appeared to be an independent prognostic factor (HR 1.425, 95%CI 1.015-2.000) (Table 2).
| Covariates | Univariate | Multivariate | ||||
| HR | 95%CI | P value | HR | 95%CI | P value | |
| Age at diagnosis | 1.000 | 0.987-1.014 | 0.966 | |||
| Preoperative duration | 1.003 | 1.000-1.006 | 0.021 | 1.002 | 0.999-1.005 | 0.112 |
| Age | 1.005 | 0.992-1.018 | 0.496 | 1.004 | 0.991-1.018 | 0.533 |
| Sex | 0.934 | 0.628-1.387 | 0.734 | |||
| Appendectomy | 1.288 | 0.874-1.898 | 0.200 | |||
| Smoking history | 1.026 | 0.676-1.558 | 0.903 | 1.048 | 0.670-1.639 | 0.838 |
| Preoperative treatment | 0.915 | 0.630-1.330 | 0.642 | |||
| Perianal disease | 0.925 | 0.606-1.413 | 0.719 | 0.951 | 0.619-1.461 | 0.819 |
| Location | 1.027 | 0.864-1.222 | 0.761 | 1.040 | 0.871-1.241 | 0.665 |
| Perforating indication | 1.456 | 1.051-2.016 | 0.024 | 1.425 | 1.015-2.000 | 0.041 |
| Resection range | 0.949 | 0.799-1.128 | 0.553 | |||
| IASCs | 0.666 | 0.381-1.164 | 0.154 | |||
Table 3 shows the results of the univariate and multivariate Cox proportional hazard model analyses after the second surgery. In the univariate analysis, only perforating indication (HR 2.036, 95%CI 1.043-3.968) was significantly associated with recurrence-free survival. In the multivariate analysis, none of the factors affected the outcome of recurrence.
| Covariates | Univariate | Multivariate | ||||
| HR | 95%CI | P value | HR | 95%CI | P value | |
| Preoperative duration | 0.998 | 0.990-1.007 | 0.666 | 1.001 | 0.991-1.011 | 0.872 |
| Interval from first to second | 1.001 | 0.992-1.010 | 0.831 | |||
| Age at diagnosis | 1.012 | 0.984-1.041 | 0.406 | |||
| Sex | 0.804 | 0.368-1.755 | 0.583 | |||
| Appendectomy | 0.822 | 0.419-1.610 | 0.567 | |||
| Smoking history | 0.918 | 0.323-2.606 | 0.872 | 1.228 | 0.371-4.065 | 0.737 |
| Preoperative treatment | 1.349 | 0.667-2.752 | 0.405 | |||
| Perianal disease | 1.554 | 0.673-3.592 | 0.302 | 1.448 | 0.593-3.532 | 0.416 |
| Age | 1.008 | 0.980-1.036 | 0.590 | 1.009 | 0.977-1.042 | 0.579 |
| Location | 1.130 | 0.798-1.600 | 0.491 | 1.182 | 0.802-1.742 | 0.397 |
| Perforating indication | 2.036 | 1.043-3.968 | 0.037 | 1.919 | 0.959-3.846 | 0.065 |
| Resection range | 0.955 | 0.682-1.337 | 0.788 | |||
| IASCs | 0.862 | 0.378-1.966 | 0.725 | |||
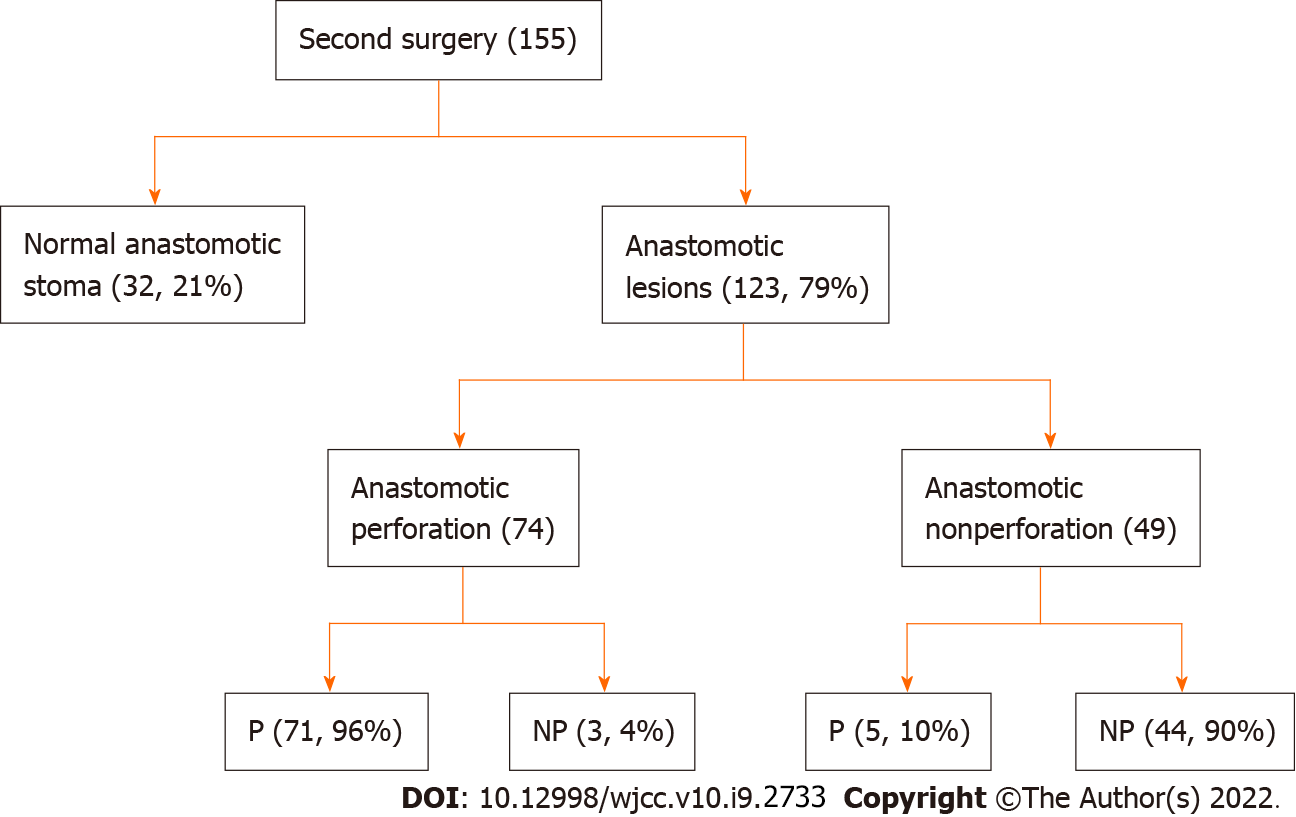
Anastomotic lesions were the most common sites of recurrence after the operation. In the second surgery, 79% of lesions occurred at anastomotic sites. The surgical indication of the second surgery was correlated with the behavior of anastomosis (P = 0.000, r = 0.917) (Figure 3). In the third surgery, 90% of lesions occurred at anastomotic sites. Concordance was found between anastomotic lesion behavior and indication for the third surgery (P = 0.000, r = 0.940) (Figure 4).
Due to the relatively low morbidity and clinical experience in CD in China, there is limited research on CD in our country, especially regarding surgical treatment. In the current study, we analyzed the clinical characteristics of repeated operations in CD, assessed the risk factors for surgical recurrence, and identified the clinical characteristics of perforating indications as common risk factors for postoperative recurrence among CD patients treated with different surgical frequencies. Moreover, our study analyzed correlations and anastomosis characteristics in repeated surgeries for Crohn’s disease.
The evaluation of clinical characteristics included each operation of CD patients. There were no significant differences in sex, appendectomy history, smoking history, perianal disease or IASCs between the primary, second and third surgeries. Our data suggested that the surgical indication of the initial surgery was correlated with the surgical indication of the second surgery. Similarly, the surgical indication of the second surgery was also correlated with that of the third surgery. Perforating CD presents as perforating disease, and nonperforating CD presents as nonperforating disease[12]. Our study confirms this concept. However, the rate of perforating indications for the second and third surgeries was higher than that for the primary surgery. CD is a chronic disease characterized by progressive bowel destruction[13]. The respective rates of inflammation, stricture, and penetrating disease are reportedly 12%, 18%, and 70% after 20 years[14], respectively, and most patients with CD will eventually develop a perforation. With the increase in surgical frequency and longer preoperative disease duration, the disease becomes more severe and more extensive. Our data showed that CD not only has stable characteristics but also progresses chronically, and perforation is a progressive surgical indication for Crohn’s disease.
Postoperative recurrence is a major problem for CD patients[15,16]. Identifying the risk factors associated with postoperative recurrence will markedly benefit patients with CD and will permit doctors to maintain close postoperative surveillance in high-risk cases and optimize CD therapy[17,18]. Although there are conflicting results in the reports according to whether the perforating indication for surgery affects postoperative recurrence[19,20], some studies have indicated that perforating CD is a risk factor for earlier recurrence[21]. Our results showed that the perforating indication was a predictor of surgical recurrence, which confirmed the concept that the perforating indication for surgery was associated with decreased recurrence-free survival. Moreover, we found that a longer preoperative disease duration was significantly associated with a shorter period of postoperative recurrence after the first surgery. As the duration of CD symptoms before surgery may be uncertain, relatively few studies have shown a significant association between preoperative disease duration and earlier recurrence of postoperative CD. Our results agree with that of Lautenbach et al[22], who reported an association between higher recurrence rates and a longer preoperative duration. Antitumor necrosis factor antibodies have been proven to prevent postoperative recurrence[23]. However, infliximab therapy did not significantly affect the outcome of postoperative recurrence in the univariate and multivariate analyses in our study. Moreover, anastomotic lesions were the most common sites of recurrence after the operation. anastomosis might be a new type of disease location for the classification of CD after surgery.
Several limitations of our study need to be considered. As most medical records were collected retrospectively, a potential bias may exist. Additionally, patients may not accurately remember their smoking habits, which may affect the significance of smoking as a risk factor. However, as an IBD center that focuses on surgical treatment in China, most data were accurately collected in our academic database or acquired by interviewing CD patients.
In conclusion, patients can retain their disease behavior after surgery, and the rate of perforating CD increases as the surgical frequency increases. CD not only has stable characteristics but also progresses chronically. Perforation is a progressive surgical indication for Crohn’s disease. Anastomosis might be a new classification of disease location for postoperative CD. These factors may help to stratify patients for preventive treatment.
It was well-known that Crohn’s disease (CD) is a chronic disease characterized by progressive bowel destruction. Despite advances in medical therapy for CD, most patients with CD require repeated resection surgeries.
To delay postoperative recurrence, it is important to analyze the clinical characteristics and predict postoperative recurrence for surgical patients. Patients with risk factors for earlier postoperative recurrence should be considered for postoperative prophylaxis.
The aim of the current study was to analyze the perforating and nonperforating indications of repeated CD operations and identify the anastomosis characteristics for postoperative CD.
Clinical characteristics of each surgery were collected. Univariate and multivariate analyses were performed to determine risk factors for recurrence.
Even if the correlation of surgical indications between repeated operations, the rate of perforating indication for the second and third surgeries was significantly higher than that of the first surgery. Anastomosis might be a new type of disease location for the classification of postoperative CD.
CD not only has stable characteristics but also progresses chronically. Perforation is a progressive surgical indication for Crohn’s disease. For CD after surgery, anastomosis may be a new classification of disease location.
More study analyze the anastomosis characteristics for postoperative CD and develop new typing standardsfor postoperative CD.
We thank all the people who participated in this article and the support of the hospital and department.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Khalili AS, Sassaki LY S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Yang H, Li Y, Wu W, Sun Q, Zhang Y, Zhao W, Lv H, Xia Q, Hu P, Li H, Qian J. The incidence of inflammatory bowel disease in Northern China: a prospective population-based study. PLoS One. 2014;9:e101296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 69] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Dasharathy SS, Limketkai BN, Sauk JS. What's New in the Postoperative Management of Crohn's Disease? Dig Dis Sci. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Papamichael K, Lin S, Moore M, Papaioannou G, Sattler L, Cheifetz AS. Infliximab in inflammatory bowel disease. Ther Adv Chronic Dis. 2019;10:2040622319838443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 4. | Bislenghi G, Sucameli F, Fieuws S, Ferrante M, Sabino J, Wolthuis A, Vermeire S, D'Hoore A. Non-conventional versus conventional strictureplasties for Crohn's disease. A Systematic Review and Meta-analysis of Treatment Outcomes. J Crohns Colitis. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Riss S, Schuster I, Papay P, Mittlböck M, Stift A. Repeat intestinal resections increase the risk of recurrence of Crohn's disease. Dis Colon Rectum. 2013;56:881-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Battat R, Sandborn WJ. Advances in the Comprehensive Management of Postoperative Crohn's Disease. Clin Gastroenterol Hepatol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Fortinsky KJ, Kevans D, Qiang J, Xu W, Bellolio F, Steinhart H, Milgrom R, Greenberg G, Cohen Z, Macrae H, Stempak J, McLeod R, Silverberg MS. Rates and Predictors of Endoscopic and Clinical Recurrence After Primary Ileocolic Resection for Crohn's Disease. Dig Dis Sci. 2017;62:188-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Dal Piaz G, Mendolaro M, Mineccia M, Randazzo C, Massucco P, Cosimato M, Rigazio C, Guiotto C, Morello E, Ercole E, Lavagna A, Rocca R, Ferrero A, Daperno M. Predictivity of early and late assessment for post-surgical recurrence of Crohn's disease: Data from a single-center retrospective series. Dig Liver Dis. 2021;53:987-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Wasmann KATGM, van Amesfoort J, van Montfoort ML, Koens L, Bemelman WA, Buskens CJ. The Predictive Value of Inflammation at Ileocecal Resection Margins for Postoperative Crohn's Recurrence: A Cohort Study. Inflamm Bowel Dis. 2020;26:1691-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Kline BP, Weaver T, Brinton DL Jr, Harris L, Yochum GS, Berg AS, Koltun WA. Clinical and Genetic Factors Impact Time to Surgical Recurrence After Ileocolectomy for Crohn's Disease. Ann Surg. 2021;274:346-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1970] [Cited by in RCA: 2354] [Article Influence: 123.9] [Reference Citation Analysis (2)] |
| 12. | Simillis C, Yamamoto T, Reese GE, Umegae S, Matsumoto K, Darzi AW, Tekkis PP. A meta-analysis comparing incidence of recurrence and indication for reoperation after surgery for perforating versus nonperforating Crohn's disease. Am J Gastroenterol. 2008;103:196-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 146] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 13. | Peyrin-Biroulet L, Loftus EV Jr, Colombel JF, Sandborn WJ. Early Crohn disease: a proposed definition for use in disease-modification trials. Gut. 2010;59:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Pariente B, Cosnes J, Danese S, Sandborn WJ, Lewin M, Fletcher JG, Chowers Y, D'Haens G, Feagan BG, Hibi T, Hommes DW, Irvine EJ, Kamm MA, Loftus EV Jr, Louis E, Michetti P, Munkholm P, Oresland T, Panés J, Peyrin-Biroulet L, Reinisch W, Sands BE, Schoelmerich J, Schreiber S, Tilg H, Travis S, van Assche G, Vecchi M, Mary JY, Colombel JF, Lémann M. Development of the Crohn's disease digestive damage score, the Lémann score. Inflamm Bowel Dis. 2011;17:1415-1422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 412] [Cited by in RCA: 464] [Article Influence: 33.1] [Reference Citation Analysis (1)] |
| 15. | Chen ZX, Chen YL, Huang XM, Lin XT, He XW, Lan P. Risk factors for recurrence after bowel resection for Crohn's disease. World J Gastrointest Pharmacol Ther. 2019;10:67-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Ikeda A, Miyoshi N, Fujino S, Iijima H, Takahashi H, Haraguchi N, Nishimura J, Hata T, Matsuda C, Doki Y, Mori M, Mizushima T. A Novel Predictive Nomogram for Early Endoscopic Recurrence after Intestinal Resection for Crohn's Disease. Digestion. 2019;100:269-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Rottoli M, Vallicelli C, Ghignone F, Tanzanu M, Vitali G, Gionchetti P, Rizzello F, Poggioli G. Predictors of early recurrence after strictureplasty for Crohn's disease of the small bowel during the years of biologics. Dig Liver Dis. 2019;51:663-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Burr NE, Hall B, Hamlin PJ, Selinger CP, Ford AC, O'Connor A. Systematic Review and Network Meta-Analysis of Medical Therapies to Prevent Recurrence of Post-Operative Crohn's Disease. J Crohns Colitis. 2019;13:693-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Aaltonen G, Keränen I, Carpelan-Holmström M, Lepistö A. Risk factors for anastomotic recurrence after primary ileocaecal resection in Crohn's disease. Eur J Gastroenterol Hepatol. 2018;30:1143-1147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Maggiori L, Brouquet A, Zerbib P, Lefevre JH, Denost Q, Germain A, Cotte E, Beyer-Berjot L, Munoz-Bongrand N, Desfourneaux V, Rahili A, Duffas JP, Pautrat K, Denet C, Bridoux V, Meurette G, Faucheron JL, Loriau J, Souche R, Vicaut E, Panis Y, Benoist S; GETAID chirurgie group. Penetrating Crohn Disease Is Not Associated With a Higher Risk of Recurrence After Surgery: A Prospective Nationwide Cohort Conducted by the Getaid Chirurgie Group. Ann Surg. 2019;270:827-834. |
| 21. | Corrigendum to Predicting Risk of Postoperative Disease Recurrence in Crohn's Disease: Patients With Indolent Crohn's Disease Have Distinct Whole Transcriptome Profiles at the Time of First Surgery. Inflamm Bowel Dis. 2019;25:e167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Lautenbach E, Berlin JA, Lichtenstein GR. Risk factors for early postoperative recurrence of Crohn's disease. Gastroenterology. 1998;115:259-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 110] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Liu C, Li N, Zhan S, Tian Z, Wu D, Li T, Zeng Z, Zhuang X. Anti -TNFα agents in preventing the postoperative recurrence of Crohn's disease: Do they still play a role in the biological era? Expert Opin Biol Ther. 2021;21:1509-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |