Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10134
Peer-review started: July 15, 2021
First decision: August 19, 2021
Revised: August 29, 2021
Accepted: September 16, 2021
Article in press: September 16, 2021
Published online: November 26, 2021
Processing time: 130 Days and 3.1 Hours
In robot-assisted (RA) spine surgery, the relationship between the surgical outcome and the learning curve remains to be evaluated.
To analyze the learning curve of RA pedicle screw fixation (PSF) through fitting the operation time curve based on the cumulative summation method.
RA PSFs that were initially completed by two surgeons at the Beijing Jishuitan Hospital from July 2016 to March 2019 were analyzed retrospectively. Based on the cumulative sum of the operation time, the learning curves of the two surgeons were drawn and fit to polynomial curves. The learning curve was divided into the early and late stages according to the shape of the fitted curve. The operation time and screw accuracy were compared between the stages.
The turning point of the learning curves from Surgeons A and B appeared in the 18th and 17th cases, respectively. The operation time [150 (128, 188) min vs 120 (105, 150) min, P = 0.002] and the screw accuracy (87.50% vs 96.30%, P = 0.026) of RA surgeries performed by Surgeon A were significantly improved after he completed 18 cases. In the case of Surgeon B, the operation time (177.35 ± 28.18 min vs 150.00 ± 34.64 min, P = 0.024) was significantly reduced, and the screw accuracy (91.18% vs 96.15%, P = 0.475) was slightly improved after the surgeon completed 17 RA surgeries.
After completing 17 to 18 cases of RA PSFs, surgeons can pass the learning phase of RA technology. The operation time is reduced afterward, and the screw accuracy shows a trend of improvement.
Core Tip: After completing 17 to 18 cases of robot-assisted pedicle screw fixations, surgeons can pass the learning phase of robot-assisted technology. The operation time is reduced afterward, and the screw accuracy shows a trend of improvement.
- Citation: Yu J, Zhang Q, Fan MX, Han XG, Liu B, Tian W. Learning curves of robot-assisted pedicle screw fixations based on the cumulative sum test. World J Clin Cases 2021; 9(33): 10134-10142
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10134.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10134
Because spine surgeons cannot see deep tissues, they cannot directly apply preo
Surgical robots have been successfully used in many surgeries[5-7], and robotic systems have been developed to improve the accuracy of screw placement in spine surgery[8-12]. The advantage of surgical robots is that they allow doctors to see deep tissues through three-dimensional real-time navigation, and direct positioning after intraoperative planning.
Every new surgical technique has a unique learning curve[13]. The relationship between the learning curve and the outcome is an important indicator for evaluating a new surgical technique. It takes a certain process for the surgeon to be familiar with and master surgical robot technology. In robot-assisted (RA) spine surgery, the relationship between the surgical outcome and the learning curve remains to be evaluated.
In this study, the cumulative summation method was used to analyze the learning curve of RA PSF through fitting the operation’s time curve.
This study is a retrospective case control study of clinical data. The data come from the medical record management and imaging system of the Beijing Jishuitan Hospital. The learning curve of RA lumbar PSF was analyzed by measuring the operation time and screw accuracy of two of the hospital’s surgeons.
Patient inclusion criteria were: (1) over 18 years old; (2) diagnosed as having lumbar spinal stenosis or lumbar spondylolisthesis; and (3) having undergone RA single-segment minimally invasive pedicle screw surgery. Patient exclusion criteria were: (1) having undergone multi-segment surgery; (2) severe preoperative comorbidities; (3) abnormal coagulation function; and (4) requiring revision surgery.
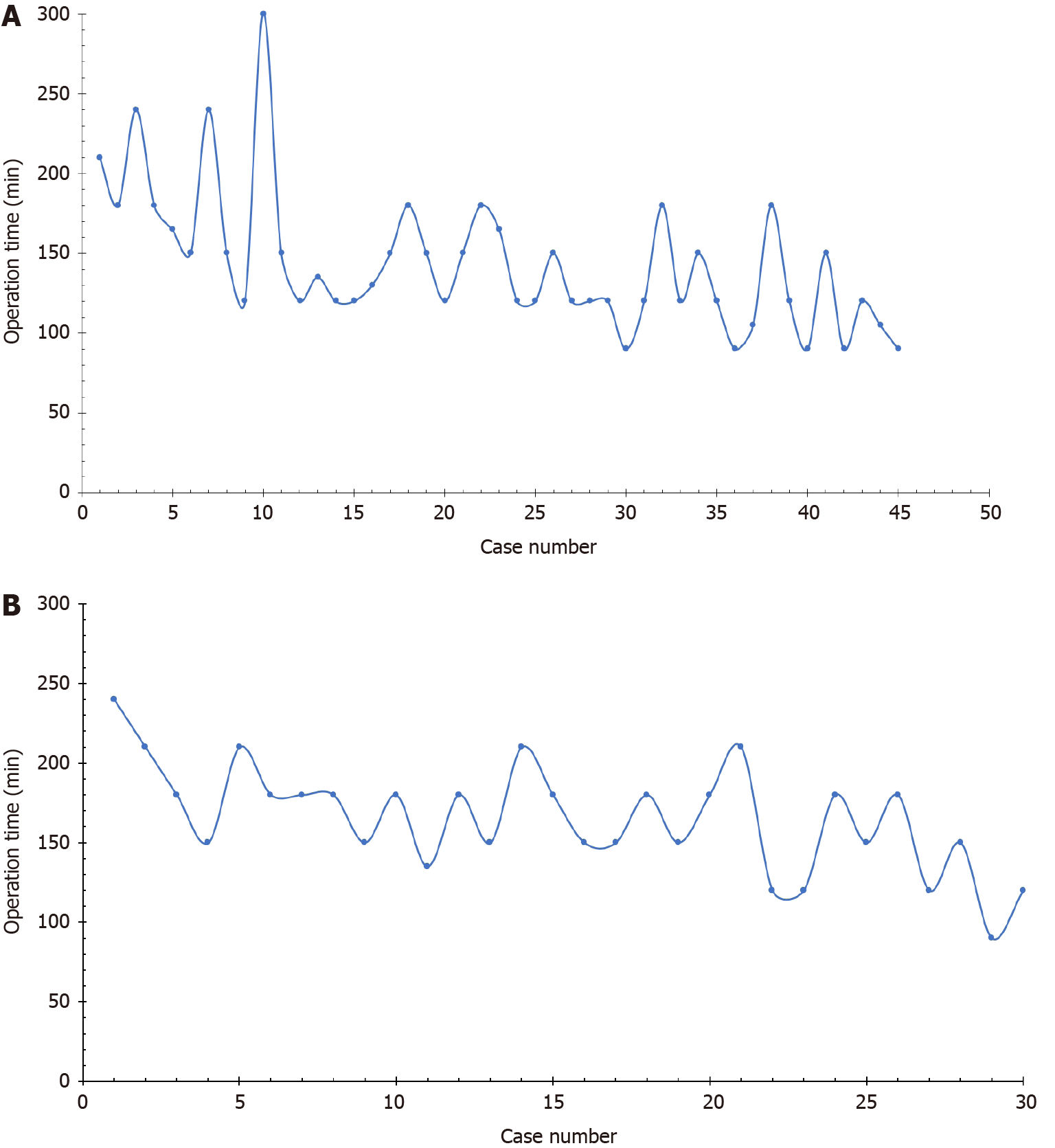
This study retrospectively analyzed the first 45 cases for Surgeon A and the first 30 cases for Surgeon B of RA single-segment minimally invasive PSF at the Department of Spine Surgery of Beijing Jishuitan Hospital from July 2016 to March 2019. Prior to the first RA operation, these two surgeons had independently completed more than 200 freehand pedicle screw internal fixations. Both surgeons had accepted formal training before starting the operation. This study was approved by the ethics review committee of Beijing Jishuitan Hospital. RA procedures were performed according to the guideline for thoracolumbar pedicle screw placement assisted by the TiRobot Orthopedic Robotic System[14] (Beijing TINAVI Medical Technology Co. Ltd.).
The estimate of sample size is based on the operation time in the early and late stages of the learning curve. The formula for calculating the sample size is n = 2 [σ × (z1-α/2 + z1-β)/(μA - μB)]2.
According to previous research, μA (pre-operation time) was assumed to be 180 min, μB (post-operation time) was assumed to be 150 min, σ was 25, α was 0.05, and β was 0.20. Based on these calculations, each group required at least 12 cases; that is, each surgeon needed to include at least 24 cases.
A postoperative computed tomography (CT) scan was performed to evaluate the accuracy of the pedicle screws. One surgeon and one radiologist who were blind to this study independently assessed the accuracy of the pedicle screws through the lumbar CT multiplanar reconstruction images. If the ratings of the two were inconsistent, the evaluation was then conducted by a senior surgeon. The pedicle screw position was graded according to the Gertzbein and Robbins grading scale[15] (screw accuracy = number of grade A screws/total number of screws × 100%).
The operation time was recorded as the time from the installation of the patient tracer to completion of the suture. According to the intraoperative use of gauze and suction, the surgeon, anesthesiologist, and nurse calculated the amount of blood loss. Surgery-related complications included postoperative infection, cerebrospinal fluid leakage, vessel damage, and nerve damage.
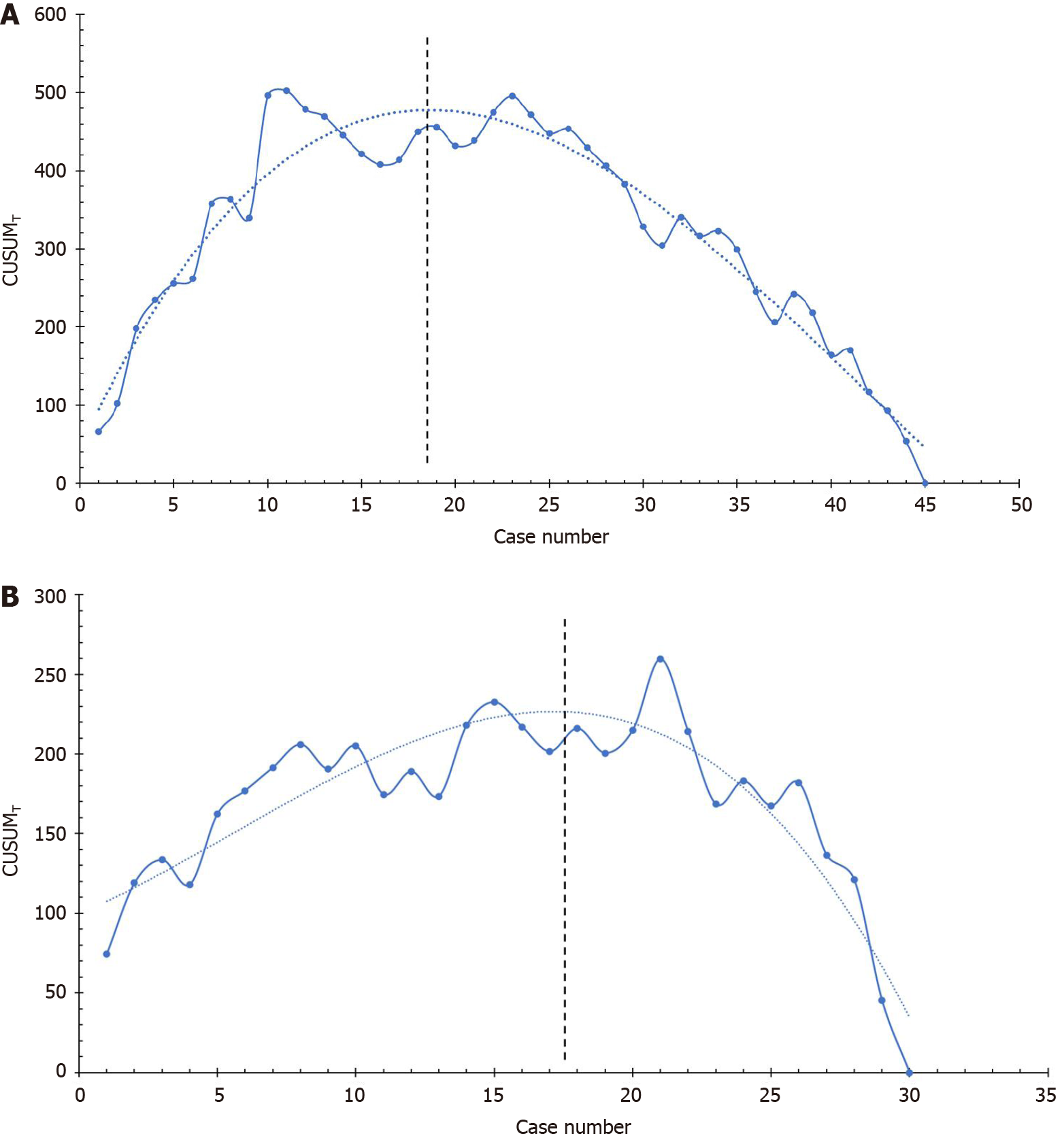
According to the method proposed by Bokhari et al[16] and Song et al[17], the cumulative sum (CUSUM) method was used to determine the learning curve based on the operation time.
The CUSUMT value of the first case was the operation time (T1) minus the mean operation time (MT); the CUSUMT value of the second case was the operation time of the second case (T2) minus the MT, then plus the CUSUMT value of the first case. A recursive process continued until the last case, and the CUSUMT value was zero at the end. Polynomial curve fitting was performed on CUSUMT to calculate the model’s fit.
According to the shape of the fitted curve, when the curve changes from rising to falling, it indicated that the learning curve had been successfully crossed. We chose this time point to divide the surgeries of one surgeon into early stage and late stage. We then compared the results of screw accuracy, operation time, blood loss, and complications in the early and late stages.
Statistical analysis was performed using IBM SPSS v 24.0 software). The categorical variables were expressed by frequencies (percentage), and the χ2 test or Fisher’s exact test was used for comparison between groups. The Shapiro-Wilk test was used to test the normalcy of continuous variables. Normally distributed continuous variables were represented by the mean ± SD, and non-normally distributed continuous variables were represented by the median (25% quantile, 75% quantile). The Student’s t-test was used to compare between groups of normally distributed data, and the Mann-Whitney U test was used to compare between groups of non-normally distributed data. A P value < 0.05 was considered statistically significant.
Surgeon A completed 45 RA PSFs. Patients included 24 males and 21 females, with an average age of 60.38 years. Surgeon A placed a total of 180 pedicle screws. Posto
The fitting model formula of Surgeon A’s learning curve was CUSUMT = 0.014X3 − 1.769X2 + 51.305X + 45.437 (X represents the case order). The goodness of fit was R² = 0.935. According to the shape of the learning curve for Surgeon A, the learning curve for RA surgery can be divided into two stages (Figure 2A). The first 18 cases were in the early stage (CUSUMT fitting curve continued to rise, representing the learning of surgical technique), and the 19th to 45th cases in the late stage (CUSUMT fitting curve continued to decline, representing the mastery of surgical technique).
The comparison of screw accuracy, operation time, and intraoperative blood loss in the two stages of Surgeon A’s learning curve is shown in Table 1. The operation time in the late stage was shorter than that in the early stage [150 (128, 188) min vs 120 (105, 150) min, P = 0.002]. The screw accuracy in the late stage was higher than that in the early stage (87.50% vs 96.30%, P = 0.026). There was no statistically significant difference in intraoperative blood loss between the two stages [100 (88, 200) mL vs 100 (80, 100) mL, P = 0.186].
| Variables | Early stage | Late stage | P value |
| Number of surgeries | 18 | 27 | |
| Number of screws | 72 | 108 | |
| Screw accuracy | 87.50% | 96.30% | 0.026 |
| Operation time (min) | 150 (128, 188) | 120 (105, 150) | 0.002 |
| Blood loss (mL) | 100 (88, 200) | 100 (80, 100) | 0.186 |
Surgeon B completed 30 RA PSFs. Patients included 14 males and 16 females, with an average age of 57.57 years. Surgeon B placed a total of 120 pedicle screws. Postoperative CT showed that the accuracy of pedicle screws was 93.33%. The operation time was 165.50 ± 33.54 min (Figure 1B). The intraoperative blood loss was 200 (100, 200) mL. There were no perioperative complications related to the use of the robot.
The fitting model formula of Surgeon B’s learning curve was CUSUMT = −0.024X3 + 0.405X2 + 7.642X + 99.455 (X represents the case order). The goodness of fit was R² = 0.835. According to the shape of the learning curve of Surgeon B, the learning curve of RA surgery can be divided into two stages (Figure 2B). The first 17 cases were in the early stage (CUSUMT fitting curve continued to rise, representing learning of the surgical technique), and the 18th to 30th cases in the late stage (CUSUMT fitting curve continued to decline, representing mastery of the surgical technique).
The comparison of the screw accuracy, operation time, and intraoperative blood loss in the two stages of Surgeon B’s learning curve is shown in Table 2. The operation time during the late stage was shorter than that during the early stage (177.35 ± 28.18 min vs 150.00 ± 34.64 min, P = 0.024). The screw accuracy in the late stage (96.15%) was slightly higher than that in the early stage (91.18%), but the difference was not statistically significant (P = 0.475). There was no statistically significant difference in intraoperative blood loss between the two stages [200 (100, 200) mL vs 100 (100, 200) mL, P = 0.095].
| Variables | Early stage | Late stage | P value |
| Number of surgeries | 17 | 13 | |
| Number of screws | 68 | 52 | |
| Screw accuracy | 91.18% | 96.15% | 0.475 |
| Operation time (min) | 177.35 ± 28.18 | 150.00 ± 34.64 | 0.024 |
| Blood loss (mL) | 200 (100, 200) | 100 (100, 200) | 0.095 |
Spine surgery requires surgeons to have sufficient professional knowledge, good planning ability, and meticulous surgical techniques. The training process for spine surgeons is usually long and arduous. Only after years of professional learning and clinical practice can spine surgeons accurately and efficiently complete preoperative planning, exposure, nerve decompression, internal fixation, and fusion[18]. Therefore, any techniques that can improve the safety, accuracy, and efficiency and shorten the learning curve of spine surgery will be welcome.
The use of surgical robots aims to make up for the surgeon’s physiological shortcomings in vision and operation. Their emergence has brought about significant improvements in spinal fixation. With the development of image navigation technology, a variety of surgical robot systems have been developed to deal with the problems encountered in spine surgery, especially for the accurate placement of internal fixation[8,12]. The positioning of surgical robots is accurate and stable, which can improve the accuracy and safety of PSF in minimally invasive spine surgery[9]. Studies have shown that the accuracy of pedicle screw placement in RA lumbar spine surgery can reach about 95%, which is much higher than the accuracy of freehand pedicle screw placement[19,20]. However, we still do not have enough knowledge on the learning curve of RA PSF.
Looking at RA surgery of other disciplines, we see that the learning curve of RA urological surgery is significantly shorter than that of freehand surgery[21]. Surgeons can master surgical techniques after completing 50 RA gynecological surgeries. Surgeons can also master surgical techniques after completing 16 to 32 cases of RA cholecystectomy. The learning stage of RA gastric bypass surgery can be passed after completing 14 cases[22,23].
As an emerging technology, RA spine surgery has a specific learning curve, which is mainly reflected in the operation time and screw accuracy[18,24-26]. This study included RA single-segment minimally invasive lumbar spine surgeries performed separately by two surgeons, and evaluated the learning curve of RA PSF. The turning points of the learning curve of surgeons A and B were in the 18th and 17th cases, respectively. The screw accuracy and operation time in the late stage of the learning curve were improved compared with the early stage, indicating that the surgeon can master the surgical technique of RA lumbar spine surgery after completing 17 to 18 cases. Therefore, problems such as long operation time and insufficient screw accuracy in the initial application of RA lumbar spine surgery would be gradually solved after surgeons completed a certain number of surgeries.
Hu et al[25] studied the learning curve for Mazor Robotics’ Renaissance RA pedicle screw placement. They analyzed the results of the first 150 RA pedicle screw placements performed by one surgeon. They divided 150 surgeries into five groups of 30. The success rate of RA surgery in groups 1 to 5 were 82%, 93%, 91%, 95%, and 93%, respectively. The inaccurate rate of screws in groups 1 to 5 were 0.8%, 0.3%, 1.4%, 0.8%, and 0%, respectively. Therefore, they defined the first 30 cases as the learning curve of RA spine surgery[25]. Siddiqui et al[24] analyzed the learning curve of the ExcelsiusGPS® RA spine surgery. After a clear learning curve of 30 screws being placed, the screw accuracy improved. The study of Kam et al[27] showed that the learning curve of RA pedicle screw placement is very short. The study of Urakov et al[18] showed that the operation time of RA surgery decreased with the increase in the number of cases. In addition, RA pedicle screw placement can reduce the technical training required for successful screw placement[18]. Schatlo et al[26] found that the inaccurate rate of screws was higher in the 10th to 20th cases in the SpineAssist RA spine surgery. Hyun et al[28] found that the average insertion time per screw was reduced from 5.5 min in the first 15 cases to 4.0 min in the subsequent 15 cases and that the average fluoroscopy time per screw was reduced from 4.1 s to 2.9 s. The study of Kim et al[29] showed that the screw insertion time was reduced from 14.9 min in the first eight cases to 9.3 min in the subsequent 29 cases and that the fluoroscopy time was reduced by 30% after the eighth case.
The CUSUM method was originally used for quality control in the industrial field, and was subsequently introduced into the medical field to analyze a surgery’s learning curve[30]. CUSUM analysis is currently widely used to evaluate the learning curve of new surgeries, such as RA rectal resection[31], laparoscopic hepatectomy[32], and laparoscopic pancreaticoduodenectomy[33]. Kim et al[20] believe that the CUSUM method can be effective in studying the results of spine surgery. CUSUM analysis converts the original data into continuous cumulative data that deviate from the average value, which can display data trends that cannot be discerned by other methods. In this study, the turning point of the learning curve cannot be derived from the original data of the operation time. However, the CUSUM fitting curve of the operation time can be used to divide the learning process of RA surgery into two stages, according to the apex of the curve. The CUSUMT in the early stage of the curve showed an upward trend, which represents the learning of the surgical technique. The CUSUMT in the late stage of the curve showed a downward trend, which represents the mastery of the surgical technique. Through CUSUM analysis, it was found that the learning stages of Surgeons A and B were the first 18 cases and the first 17 cases, respectively.
This study has several limitations. First, the sample size of this study was limited to 75 surgeries performed by two surgeons. Secondly, these two surgeons came from the leading orthopedic hospital in China. Whether other surgeons with less experience can obtain the same learning curve remains to be seen.
This paper retrospectively studied the RA minimally invasive single-segment PSF performed by two surgeons, and analyzed the learning curve of RA PSF using the CUSUM method. After completing 17 to 18 cases of RA lumbar PSF, surgeons can pass the learning phase of RA technology. Operation time is reduced, and screw accuracy shows a trend of improvement.
Every new surgical technique has a unique learning curve. The relationship between the learning curve and the outcome is an important indicator for evaluating a new surgical technique. It takes a certain process for the surgeon to be familiar with and master surgical robot technology.
In robot-assisted (RA) spine surgery, the relationship between the surgical outcome and the learning curve remains to be evaluated.
This study aimed to analyze the learning curve of RA pedicle screw fixation (PSF) through fitting the operation’s time curve.
Based on the cumulative sum of the operation time, the learning curves of the two surgeons were drawn and fit to polynomial curves. The learning curve was divided into the early and late stages according to the shape of the fitted curve. The operation time and screw accuracy were compared between the stages.
The turning point of the learning curves from Surgeons A and B appeared in the 18th and 17th cases, respectively.
After completing 17 to 18 cases of RA PSFs, surgeons can pass the learning phase of RA technology. The operation time is reduced afterward, and the screw accuracy shows a trend of improvement.
These two surgeons came from the leading orthopedic hospital in China. Whether other surgeons with less experience can obtain the same learning curve remains to be seen.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Archer KR S-Editor: Wang JL L-Editor: A P-Editor: Liu JH
| 1. | Tian W, Liu Y, Fan M, Zhao J, Jin P, Zeng C. CAMISS Concept and Its Clinical Application. Adv Exp Med Biol. 2018;1093:31-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S. Accuracy of pedicle screw placement in lumbar vertebrae. Spine (Phila Pa 1976). 1996;21:1320-1324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 330] [Cited by in RCA: 323] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 3. | Gelalis ID, Paschos NK, Pakos EE, Politis AN, Arnaoutoglou CM, Karageorgos AC, Ploumis A, Xenakis TA. Accuracy of pedicle screw placement: a systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012;21:247-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 505] [Cited by in RCA: 450] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 4. | Jutte PC, Castelein RM. Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J. 2002;11:594-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 194] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 5. | Leal Ghezzi T, Campos Corleta O. 30 Years of Robotic Surgery. World J Surg. 2016;40:2550-2557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 250] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 6. | Yaxley JW, Coughlin GD, Chambers SK, Occhipinti S, Samaratunga H, Zajdlewicz L, Dunglison N, Carter R, Williams S, Payton DJ, Perry-Keene J, Lavin MF, Gardiner RA. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet. 2016;388:1057-1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 478] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 7. | Dogangil G, Davies BL, Rodriguez y Baena F. A review of medical robotics for minimally invasive soft tissue surgery. Proc Inst Mech Eng H. 2010;224:653-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 8. | Chen AF, Kazarian GS, Jessop GW, Makhdom A. Robotic Technology in Orthopaedic Surgery. J Bone Joint Surg Am. 2018;100:1984-1992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 9. | Ghasem A, Sharma A, Greif DN, Alam M, Maaieh MA. The Arrival of Robotics in Spine Surgery: A Review of the Literature. Spine (Phila Pa 1976). 2018;43:1670-1677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 138] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 10. | Rasouli JJ, Shao J, Neifert S, Gibbs WN, Habboub G, Steinmetz MP, Benzel E, Mroz TE. Artificial Intelligence and Robotics in Spine Surgery. Global Spine J. 2021;11:556-564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 11. | Siccoli A, Klukowska AM, Schröder ML, Staartjes VE. A Systematic Review and Meta-Analysis of Perioperative Parameters in Robot-Guided, Navigated, and Freehand Thoracolumbar Pedicle Screw Instrumentation. World Neurosurg. 2019;127:576-587.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Zhang Q, Han XG, Xu YF, Fan MX, Zhao JW, Liu YJ, He D, Tian W. Robotic navigation during spine surgery. Expert Rev Med Devices. 2020;17:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Roser F, Tatagiba M, Maier G. Spinal robotics: current applications and future perspectives. Neurosurgery. 2013;72 Suppl 1:12-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 193] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 14. | Tian W, Liu YJ, Liu B, He D, Wu JY, Han XG, Zhao JW, Fan MX; Technical Committee on Medical Robot Engineering of Chinese Society of Biomedical Engineering; Technical Consulting Committee of National Robotic Orthopaedic Surgery Application Center. Guideline for Thoracolumbar Pedicle Screw Placement Assisted by Orthopaedic Surgical Robot. Orthop Surg. 2019;11:153-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 15. | Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15:11-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 825] [Cited by in RCA: 934] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 16. | Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc. 2011;25:855-860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 294] [Cited by in RCA: 314] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 17. | Song G, Sun X, Miao S, Li S, Zhao Y, Xuan Y, Qiu T, Niu Z, Song J, Jiao W. Learning curve for robot-assisted lobectomy of lung cancer. J Thorac Dis. 2019;11:2431-2437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Urakov TM, Chang KH, Burks SS, Wang MY. Initial academic experience and learning curve with robotic spine instrumentation. Neurosurg Focus. 2017;42:E4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 19. | Han X, Tian W, Liu Y, Liu B, He D, Sun Y, Han X, Fan M, Zhao J, Xu Y, Zhang Q. Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. 2019;1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 138] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 20. | Kim HJ, Lee SH, Chang BS, Lee CK, Lim TO, Hoo LP, Yi JM, Yeom JS. Monitoring the quality of robot-assisted pedicle screw fixation in the lumbar spine by using a cumulative summation test. Spine (Phila Pa 1976). 2015;40:87-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 73] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Yohannes P, Rotariu P, Pinto P, Smith AD, Lee BR. Comparison of robotic versus laparoscopic skills: is there a difference in the learning curve? Urology. 2002;60:39-45; discussion 45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 233] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 22. | Lenihan JP Jr, Kovanda C, Seshadri-Kreaden U. What is the learning curve for robotic assisted gynecologic surgery? J Minim Invasive Gynecol. 2008;15:589-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 171] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 23. | Vidovszky TJ, Smith W, Ghosh J, Ali MR. Robotic cholecystectomy: learning curve, advantages, and limitations. J Surg Res. 2006;136:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 24. | Siddiqui MI, Wallace DJ, Salazar LM, Vardiman AB. Robot-Assisted Pedicle Screw Placement: Learning Curve Experience. World Neurosurg. 2019;130:e417-e422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 25. | Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res. 2014;472:1839-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 123] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 26. | Schatlo B, Martinez R, Alaid A, von Eckardstein K, Akhavan-Sigari R, Hahn A, Stockhammer F, Rohde V. Unskilled unawareness and the learning curve in robotic spine surgery. Acta Neurochir (Wien). 2015;157:1819-1823; discussion 1823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 27. | Kam JKT, Gan C, Dimou S, Awad M, Kavar B, Nair G, Morokoff A. Learning Curve for Robot-Assisted Percutaneous Pedicle Screw Placement in Thoracolumbar Surgery. Asian Spine J. 2019;920-927. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 28. | Hyun SJ, Kim KJ, Jahng TA, Kim HJ. Minimally Invasive Robotic Versus Open Fluoroscopic-guided Spinal Instrumented Fusions: A Randomized Controlled Trial. Spine (Phila Pa 1976). 2017;42:353-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 200] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 29. | Kim HJ, Jung WI, Chang BS, Lee CK, Kang KT, Yeom JS. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot. 2017;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 149] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 30. | Wohl H. The cusum plot: its utility in the analysis of clinical data. N Engl J Med. 1977;296:1044-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 186] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Morelli L, Guadagni S, Lorenzoni V, Di Franco G, Cobuccio L, Palmeri M, Caprili G, D'Isidoro C, Moglia A, Ferrari V, Di Candio G, Mosca F, Turchetti G. Robot-assisted versus laparoscopic rectal resection for cancer in a single surgeon's experience: a cost analysis covering the initial 50 robotic cases with the da Vinci Si. Int J Colorectal Dis. 2016;31:1639-1648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 32. | Lin CW, Tsai TJ, Cheng TY, Wei HK, Hung CF, Chen YY, Chen CM. The learning curve of laparoscopic liver resection after the Louisville statement 2008: Will it be more effective and smooth? Surg Endosc. 2016;30:2895-2903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 33. | Wang M, Meng L, Cai Y, Li Y, Wang X, Zhang Z, Peng B. Learning Curve for Laparoscopic Pancreaticoduodenectomy: a CUSUM Analysis. J Gastrointest Surg. 2016;20:924-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 111] [Article Influence: 12.3] [Reference Citation Analysis (0)] |