Published online Aug 6, 2021. doi: 10.12998/wjcc.v9.i22.6544
Peer-review started: April 20, 2021
First decision: May 11, 2021
Revised: May 18, 2021
Accepted: May 26, 2021
Article in press: May 26, 2021
Published online: August 6, 2021
Processing time: 107 Days and 12 Hours
Intracranial hypotension (IH) is a disorder involving cerebrospinal fluid (CSF) hypovolemia due to spontaneous or traumatic spinal CSF leakage and is easily being misdiagnosed or missed, especially in these patients without the prototypical manifestation of an orthostatic headache. At present, the management of IH with both cranial nerve VI palsy and bilateral subdural hematomas (SDHs) is still unclear.
A 67-year-old male Chinese patient complained of diplopia on the left side for one and a half mo. Computed tomography revealed bilateral SDHs and a midline shift. However, neurotrophic drugs were not effective, and 3 d after admission, he developed a non-orthostatic headache and neck stiffness. Enhanced magnetic resonance imaging revealed dural enhancement as an additional feature, and IH was suspected. Magnetic resonance myelography was then adopted and showed CSF leakage at multiple sites in the spine, confirming the diagnosis of having IH. The patient fully recovered following multiple targeted epidural blood patch (EBP) procedures.
IH is a rare disease, and to the best of our knowledge, IH with diplopia as its initial and primary symptom has never been reported. In this study, we also elucidated that it could be safe and effective to treat IH patients with associated cranial nerve VI palsy and bilateral SDHs using repeated EBP therapy.
Core Tip: Intracranial hypotension (IH) is an uncommon disorder of cerebrospinal fluid (CSF) hypovolemia due to spontaneous or iatrogenic spinal CSF leakage, and is easily being misdiagnosed or missed as it can be associated with a large diversity of clinical signs. To the best of our knowledge, this is the first case in the literature describing a patient of having IH with diplopia as his initial and primary complaint, and demons
- Citation: Wei TT, Huang H, Chen G, He FF. Management of an intracranial hypotension patient with diplopia as the primary symptom: A case report . World J Clin Cases 2021; 9(22): 6544-6551
- URL: https://www.wjgnet.com/2307-8960/full/v9/i22/6544.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i22.6544
Intracranial hypotension (IH) is a disease being recognized with increasing frequency and is caused by decreased intracranial pressure (ICP), usually due to cerebral spinal fluid (CSF) leakage[1]. This case report describes the case of a 67-year-old male with diplopia as his primary symptom; the diagnosis of IH was missed until CSF leakage in the spine was found on magnetic resonance myelography (MRM), and the patient was successfully managed by multiple epidural blood patch (EBP) procedures. This is the first case to describe a patient with IH with diplopia as his initial and chief complaint and discuss the efficacy of using repeated EBP therapy to treat a patient with IH complicated with cranial nerve VI palsy and subdural hematomas (SDHs).
A 67-year-old Asian man complained of diplopia on the left side.
The patient’s symptom started one and a half mo prior to presentation. However, after half a mo of conservative treatment for paralytic strabismus, his symptom did not improve.
The patient had a history of type 2 diabetes for 15 years, with well-controlled glucose. He suffered a stroke 10 years ago without sequelae and took sitagliptin regularly afterwards.
No smoking or drinking history, and no similar family history were noted.
Physical examination revealed left lateral gaze palsy and horizontal diplopia, consisting of left abducens nerve paralysis, as well as weaker strength in the left upper limb (motor strength score of 4) and a positive Babinski sign.
Blood analysis revealed an elevated total cholesterol of 5.57 mmol/L and a very low density lipoprotein of 0.96 mmol/L. The electrocardiogram showed a first-degree atrioventricular block and a conduction block in the left forearm. The microprotein level in CSF obtained from a lumbar puncture performed 2 wk after the third EBP treatment was 950 mg/L. The Pandy test was positive. The ICP was normal.
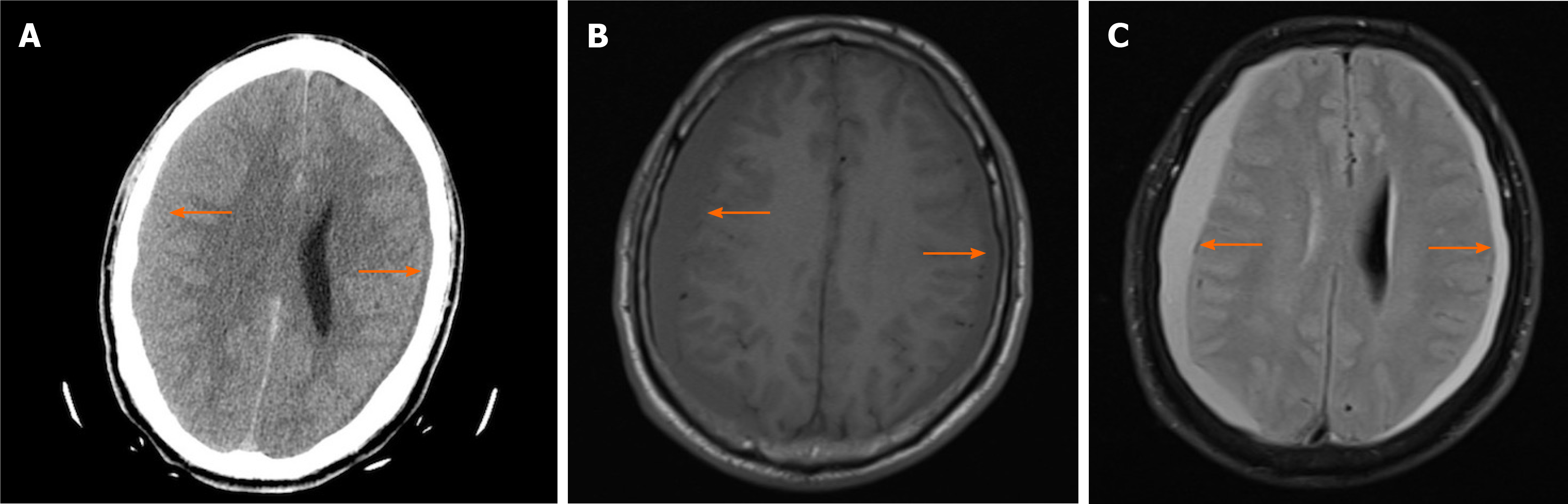
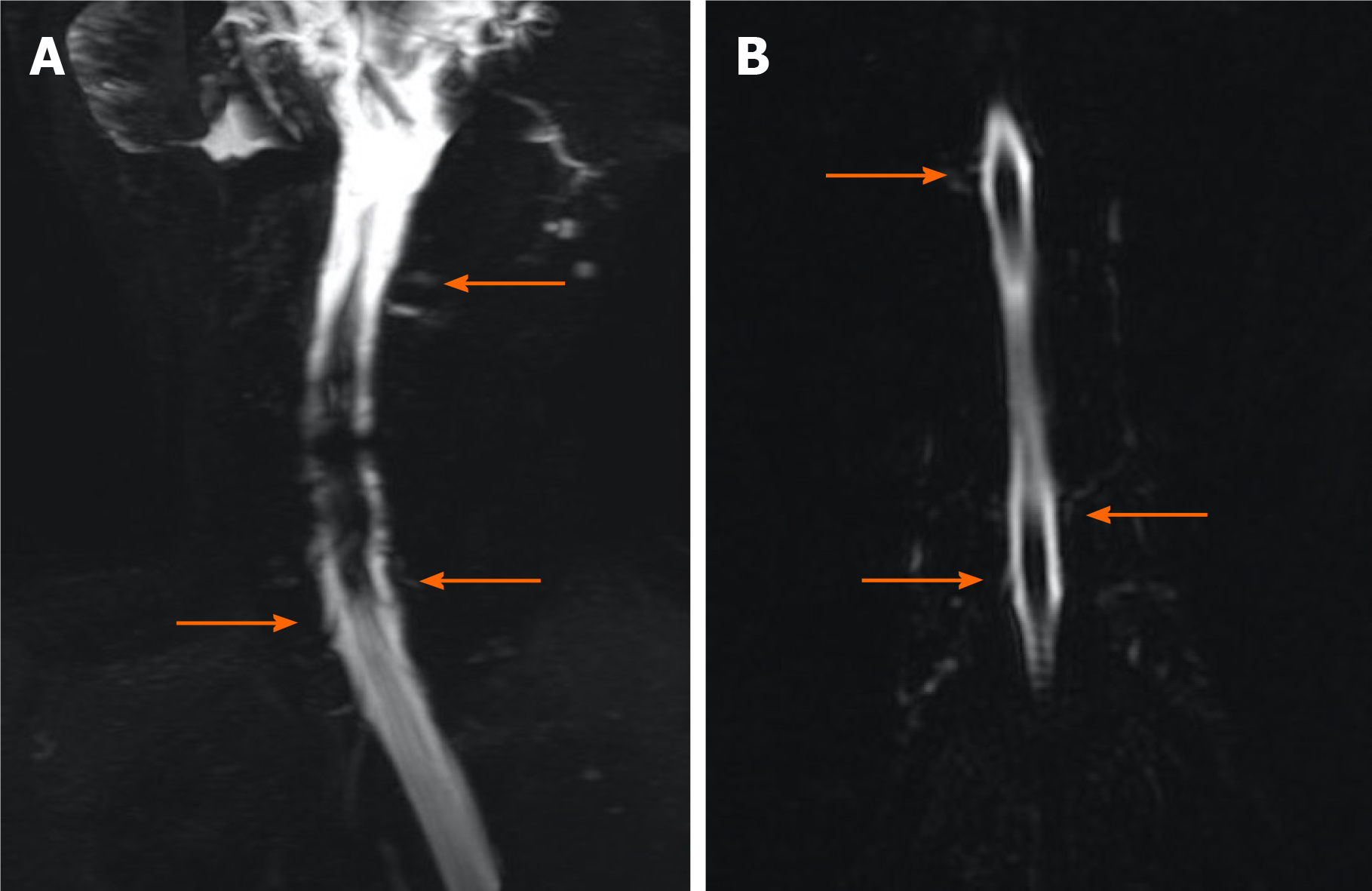
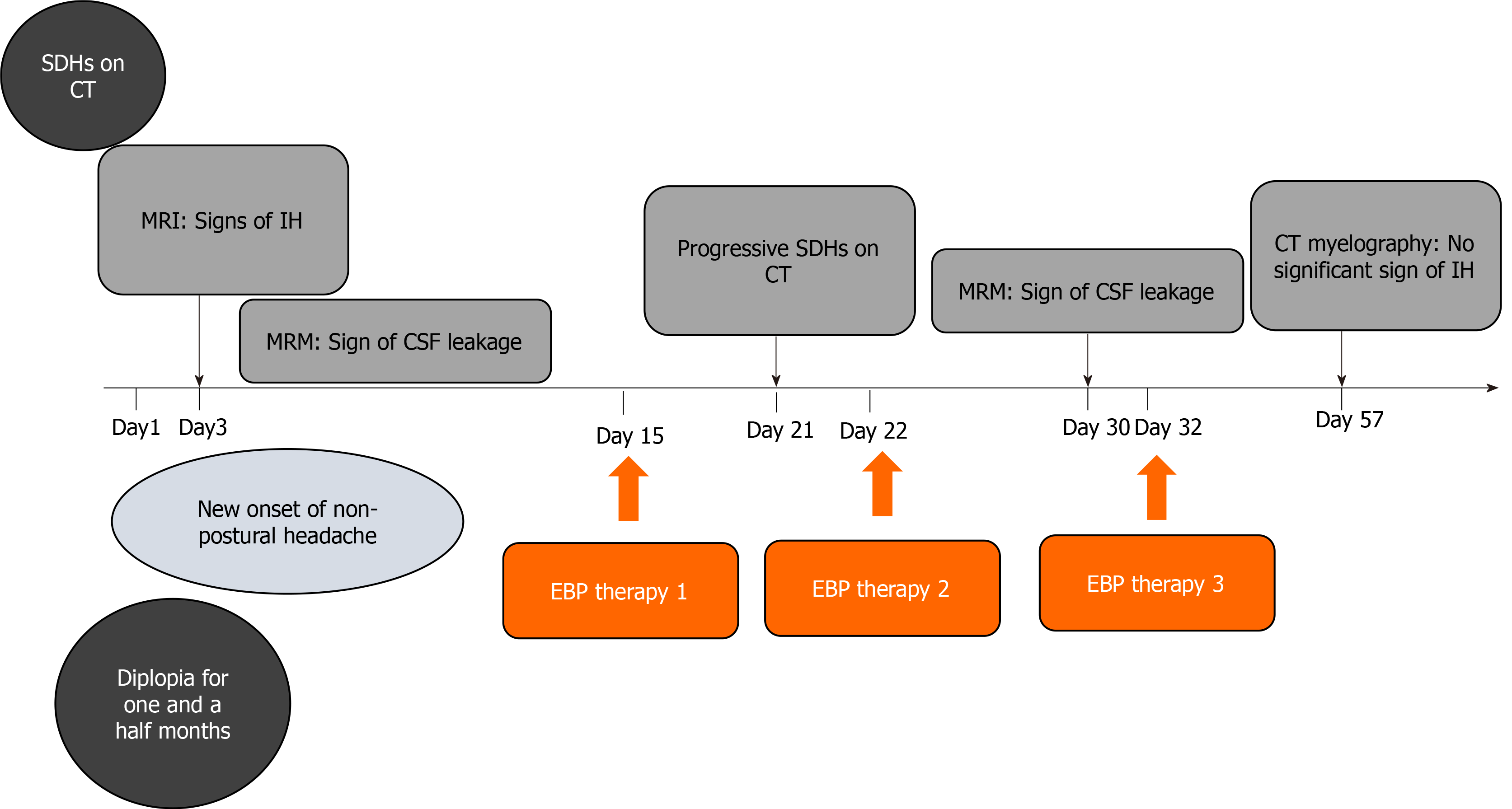
The initial plain computed tomography (CT) scan revealed SDH, which resulted in referral of the patient to the Neurosurgery Department (Figure 1A). The patient suffered a sudden severe non-orthostatic headache with neck stiffness on day 3 after admission. Enhanced magnetic resonance imaging (MRI) of his head revealed dural enhancement as an additional feature (Figure 1B and C). He was then suspected of having IH. MRM was utilized and showed multiple sites of CSF leakage in the spine, confirming the diagnosis of IH (Figure 2).
Fei-Fang He, MD, Professor and Chief, Department of Pain Management, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University. Yi-Rong Wang, MD, PhD, Professor and Chief, Department of Neurosurgery, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University
Since CSF leakage in the spine was confirmed and the patient had a stable condition, EBP therapy could be performed first.
The final diagnosis of this case was IH complicated with cranial nerve VI palsy and SDHs.
He was treated with bed rest, hydration, neurotrophic drugs for treating cranial nerve VI palsy, cholesterol lowering and glycemic control medication after the confirmation of having IH. On day 15 after his admission, the patient underwent the first EBP procedure. An 18-G needle was inserted into his epidural space at the T2/3 level, and 21 mL of autologous peripheral venous blood was infused. The second EBP treatment was performed on day 22 after considering the progression of the SDHs, with 21 mL of blood being infused at the T8/9 level. According to the MRM results on day 30, the third EBP procedure was performed on day 32 using 22 mL of blood at the T5/6 level. He accepted the same drug treatment after each EBP procedure.
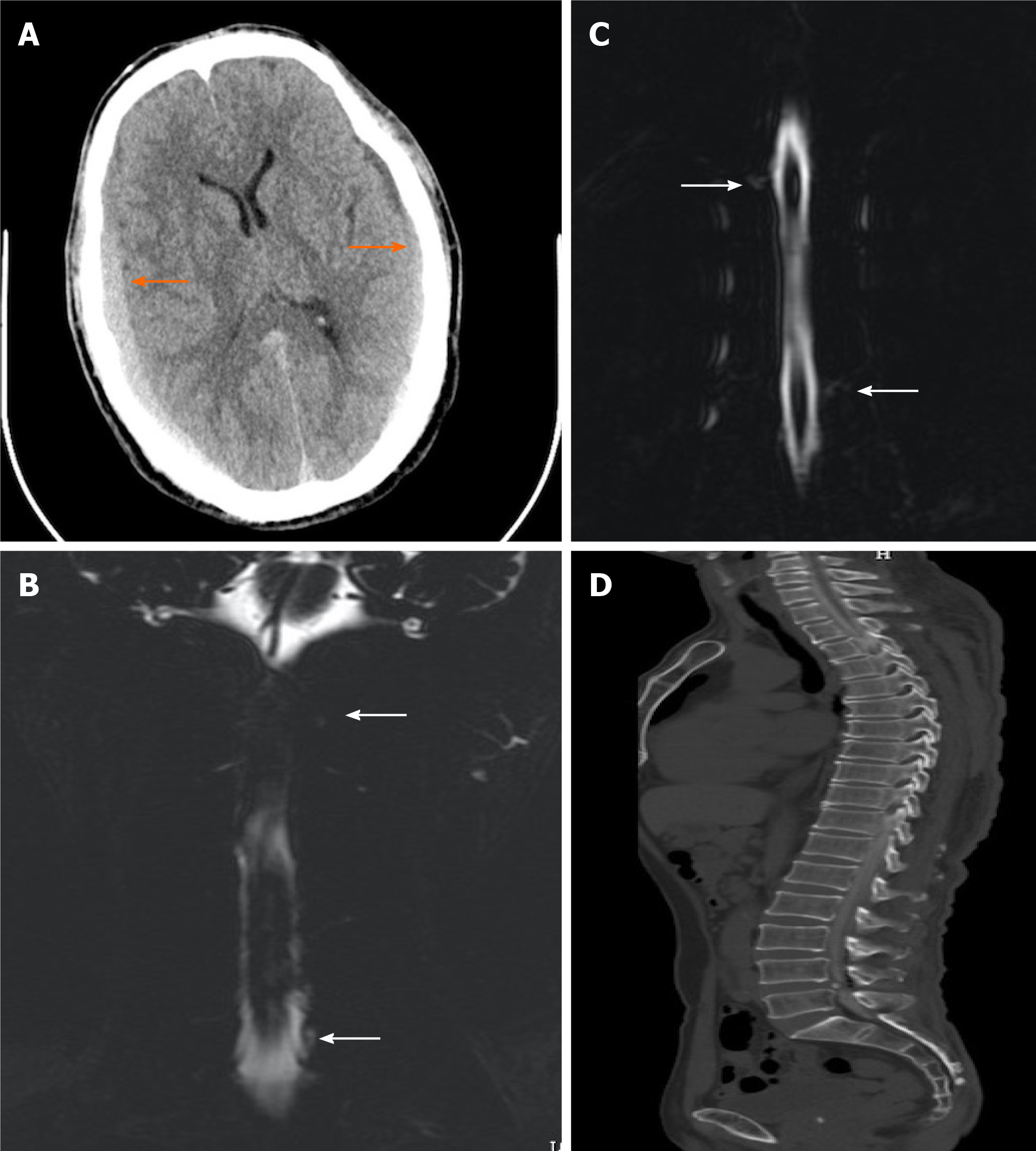
After the first EBP therapy, his headache and neck stiffness were markedly alleviated. On day 21, the follow-up CT revealed bilateral SDHs with greater density volume than the previous SDHs (Figure 3A). However, he had no complaints other than diplopia. This was followed by the second EBP therapy on day 22. The MRM of the spinal column on day 30 revealed a similar scan with no obvious decrease in CSF leakage (Figure 3B and C). Accordingly, the third EBP procedure was performed on day 32. To evaluate the curative efficacy of EBP therapy, CT myelography was employed on day 57 and showed no evident CSF leakage (Figure 3D). His symptom of diplopia was relieved 3 wk after the third EBP therapy. Over a follow-up period of 6 mo, none of the symptoms recurred, suggesting a favorable recovery.
Figure 4 summarizes the key events of this case report chronologically.
IH is a disorder of CSF hypovolemia due to spontaneous or traumatic spinal CSF leakage. The most common symptom of IH is a headache. The characteristic headache is orthostatic, aggravating in the upright posture and alleviating in the supine position[2]. In this patient, diplopia presented as the initial and primary complaint; it should be noted that this is the first reported case with this feature, which delayed making the correct diagnosis and increased the difficulty of proper therapy. In this case, horizontal diplopia, which was worse in one direction of lateral gaze, occurred with an abduction deficit and presented as esodeviation. Possible etiologies of abduction deficits include conditions affecting the pons, cranial nerve VI, neuromuscular junctions, and extraocular muscles[3]. Specifically, this patient’s diplopia was attributed to cranial nerve VI palsy derived from continuous CSF leakage. The sixth cranial nerve is the most frequently injured because of its long intracranial path. MRI has shown that continuous CSF leakage leads to IH with descent of the brain, causing traction of the sixth nerve and subsequent symptoms[4].
The presence of SDH was another characteristic feature in this case. SDH is a severe complication of IH that may lead to neurological deficits and can be life-threatening[5]. SDH associated with IH is considered to be secondary to the collapse of the intrathecal space due to CSF leakage[6]. The reported incidence of SDH among spontaneous IH patients ranges from 16% to 57%, prevailingly in males[7], whereas spontaneous IH without SDH is predominant in females and the average onset age of spontaneous IH with SDH is 44.9 years[8,9].
The association between SDH and abducens nerve palsy is rarely mentioned in the literature. These two complications were related to descent of the brain, causing traction of cranial nerves with a long intracranial course and on intracranial vessels. This traction leads to the avulsion of dural veins and subsequent subdural bleeding[10].
MRI has facilitated the recognition of IH. The typical imaging features of IH on MRI include subdural fluid collections, engorgement of venous structures, pachymeningeal enhancement, pituitary hyperemia and sagging of the brain. Although not as conclusive as MRI, CT can be of significant diagnostic value in detecting SDH, particularly in the emergency department setting[11]. In this case, repeated CT was used to detect SDH and monitor the intracranial lesions, facilitating the diagnosis and treatment of IH. If there is a high clinical suspicion of IH but normal MRI or CT findings, radioisotope cisternography or CT myelography may be the next modality of choice to pinpoint sites of CSF leakage. Furthermore, MRM is a developing cutting-edge technology that was used in our case, serving as an alternative to CT myelogra
The treatment strategy for IH consists of conservative schemes such as bed rest, intravenous hydration, caffeine intake and invasive therapies, including EBP therapy and surgery. However, there is a lack of systematic studies on therapeutic methods and outcomes in IH patients with both cranial nerve VI palsy and SDH. We provide a review of published reports describing IH as an explicit cause of SDH and abducens nerve paralysis (Table 1). As shown in the chart, conservative treatment always fails to yield persistent improvement in such patients, and currently, whether to perform surgical SDH evacuation or EBP therapy as the initial procedure is still controversial[12,13]. Through the review of those reports above and other published reports, we believe that IH patients with both SDH and cranial nerve injury require emergency surgery under the following conditions: Moderate to large hematoma causing brain hernia and neurological deterioration[14], failure to improve after applying the Trendelenburg position in comatose SDH patients with a mass effect and pupil dilation[6], and progressive SDH or rapid cognitive deterioration after EBP therapy[15,16]. Furthermore, surgical repair is indispensable in patients with evidence of cranial or spinal anatomic abnormalities (i.e. osteophytes, arachnoid cyst congenital abnormalities, etc.) to prevent the recurrence of IH[9,17]. In terms of this case, we gave preference to repeated EBP therapy due to these reasons. First, EBP therapy is proven to be effective in relieving symptoms in 90% of cases, and if symptoms can be ameliorated after EBP therapy, even a thick SDH could resolve spontaneously[18,19]. Second, conservative treatment failed in our patient, and although the follow-up CT image showed SDH progression after the first EBP procedure, his symptoms did not worsen. We decided to perform a second EBP procedure in consideration of his stable conditions and multiple sites of CSF leakage. In addition, although we found a case of recovery after surgical evacuation without EBP therapy[20], many authors believe that empirical EBP therapy after surgical evacuation could treat the underlying cause of SDH and therefore minimize the risk of relapse[5,6,21]. Moreover, our literature search yielded a report of mortality after surgery and mentioned the possibility of pneumonia and cerebral infarction as postoperative complications[22]. Loya et al[5] summarized that in most cases, surgical correction is not inevitable and may bring about deteriorated outcomes[5]. Thus, EBP therapy may be a priority since it is much safer, with less adverse reactions. Last, compared with injecting blood into multiple targeted sites of CSF leakage at one time, putting the patient at a risk of deterioration after EBP therapy due to ICP elevation[16], it is safer to perform repeated targeted EBP procedures after some interval of time with careful follow-up.
| Case No. | Ref. | Age in yr/sex | Presenting symptoms | Positive imaging findings | Subdural hematoma eva. and outcome | IH treatment | Outcome | ||
| Postural headache | Diplopia | Consciousness disturbance | |||||||
| 1 | Takahashi et al[6], 2016 | 49/M | √ | √ | √ | BSDH, DME, DOCT, NOC | √ × 2, trans imp | EBP × 2 | Near FR |
| 2 | Veeravagu et al[17], 2013 | 36/M | √ | √ | √ | Spur, DME, DOOC, SOT, Large BSDH, MS | √ + osteophyte repair | EBP, trans imp | Near FR |
| 3 | Fiala et al[12], 2012 | 28 /F | √ | √ | BSDH, thrombosis after EBP1 | EBP × 1 | FR | ||
| 4 | Slowinski et al[20], 2003 | 38 /F | √ | √ | Thick BSDH | √ | FR | ||
| 5 | Whiteley et al[13], 2003 | 62/M | √ | √ | √ | Large BSDH, DME | √ × 2, trans imp | EBP × 1 | FR |
| 6 | Velarde et al[10], 2000 | 58/M | √ | √ | Thin BSDH | EBP × 1 | FR | ||
| 7 | Welch et al[22], 1959 | 69/M | NP H/A | √ | √ | NA | √2 | Dead | |
When a patient presents with diplopia and SDH on CT, the clinician should perform a comprehensive examination to search for even subtle evidence of IH. Once IH is confirmed, EBP therapy may be a priority in such patients, except under emergency conditions necessitating surgical evacuation.
The authors thank Zhong-Feng Niu for assistance with figure preparation.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chrastina J S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li JH
| 1. | Santos JP, Silva AM, Velasco RM, Freitas MJ. Lumbar epidural blood patch for the treatment of spontaneous intracranial hypotension. J Clin Anesth. 2020;60:11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Spears RC. Low-pressure/spinal fluid leak headache. Curr Pain Headache Rep. 2014;18:425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Malloy KA, Chigbu DI. Ocular manifestations uncover chronic subdural hematoma secondary to abuse. Optometry. 2010;81:61-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Pannullo SC, Reich JB, Krol G, Deck MD, Posner JB. MRI changes in intracranial hypotension. Neurology. 1993;43:919-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 220] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Loya JJ, Mindea SA, Yu H, Venkatasubramanian C, Chang SD, Burns TC. Intracranial hypotension producing reversible coma: a systematic review, including three new cases. J Neurosurg. 2012;117:615-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | Takahashi K, Mima T, Akiba Y. Chronic Subdural Hematoma Associated with Spontaneous Intracranial Hypotension: Therapeutic Strategies and Outcomes of 55 Cases. Neurol Med Chir (Tokyo). 2016;56:69-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Hashizume K, Watanabe K, Kawaguchi M, Fujiwara A, Furuya H. Evaluation on a clinical course of subdural hematoma in patients undergoing epidural blood patch for spontaneous cerebrospinal fluid leak. Clin Neurol Neurosurg. 2013;115:1403-1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Chung SJ, Lee JH, Kim SJ, Kwun BD, Lee MC. Subdural hematoma in spontaneous CSF hypovolemia. Neurology. 2006;67:1088-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Yoon SH, Chung YS, Yoon BW, Kim JE, Paek SH, Kim DG. Clinical experiences with spontaneous intracranial hypotension: a proposal of a diagnostic approach and treatment. Clin Neurol Neurosurg. 2011;113:373-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Velarde CA, Zuniga RE, Leon RF, Abram SE. Cranial nerve palsy and intracranial subdural hematoma following implantation of intrathecal drug delivery device. Reg Anesth Pain Med. 2000;25:76-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Schievink WI. Spontaneous spinal cerebrospinal fluid leaks. Cephalalgia. 2008;28:1345-1356. [RCA] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 126] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 12. | Fiala A, Furgler G, Baumgartner E, Paal P. Delayed subdural haematoma complicated by abducens nerve palsy and cortical vein thrombosis after obstetric epidural anaesthesia. Br J Anaesth. 2012;108:705-706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Whiteley W, Al-Shahi R, Myles L, Lueck CJ. Spontaneous intracranial hypotension causing confusion and coma: a headache for the neurologist and the neurosurgeon. Br J Neurosurg. 2003;17:456-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Bullock MR, Chesnut R, Ghajar J, Gordon D, Hartl R, Newell DW, Servadei F, Walters BC, Wilberger JE; Surgical Management of Traumatic Brain Injury Author Group. Surgical management of acute subdural hematomas. Neurosurgery. 2006;58:S16-24; discussion Si. [PubMed] |
| 15. | Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y, Yatsushige H, Sugawara T. Progressive subdural hematomas after epidural blood patch for spontaneous intracranial hypotension. J Anesth. 2010;24:315-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Matsuoka K, Nakai E, Kawanishi Y, Kadota T, Fukuda H, Ueba T. Acute Deterioration in a Patient with Bilateral Chronic Subdural Hematomas Associated with Intracranial Hypotension Treated with an Epidural Blood Patch. World Neurosurg. 2020;141:331-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Veeravagu A, Gupta G, Jiang B, Berta SC, Mindea SA, Chang SD. Spontaneous intracranial hypotension secondary to anterior thoracic osteophyte: Resolution after primary dural repair via posterior approach. Int J Surg Case Rep. 2013;4:26-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Groen RJ, Hoogland PV. Spontaneous intracranial hypotension. J Neurosurg. 2010;113:685-8; author reply 688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286-2296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 667] [Cited by in RCA: 695] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 20. | Slowinski J, Szydlik W, Sanetra A, Kaminska I, Mrowka R. Bilateral chronic subdural hematomas with neurologic symptoms complicating spinal anesthesia. Reg Anesth Pain Med. 2003;28:347-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Wan Y, Xie J, Xie D, Xue Z, Wang Y, Yang S. Clinical characteristics of 15 cases of chronic subdural hematomas due to spontaneous intracranial hypotension with spinal cerebrospinal fluid leak. Acta Neurol Belg. 2016;116:509-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | WELCH K. Subdural hematoma following spinal anesthesia. AMA Arch Surg. 1959;79:49-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |