Published online Jul 16, 2021. doi: 10.12998/wjcc.v9.i20.5562
Peer-review started: December 14, 2020
First decision: March 27, 2021
Revised: April 6, 2021
Accepted: May 7, 2021
Article in press: May 7, 2021
Published online: July 16, 2021
Processing time: 204 Days and 17.5 Hours
Temporary transvenous pacing through the coronary sinus is a novel approach rarely used in treating unstable bradycardia. This modality could provide cardiac pacing while achieving better ventricular synchrony. We present a case who received cardiac pacing through the coronary sinus and provide a summary of evidence in the current literature.
A 55-year-old woman with a history of advanced heart failure was admitted to the rehabilitation ward after a recent stroke. During hospitalization, she had paroxysmal atrial fibrillation with rapid ventricular response resulting from fluid overload. While atrial fibrillation was spontaneously reversed to sinus rhythm after diuresis, she developed multiple episodes of polymorphic ventricular tachycardia along with sinus bradycardia and prolonged QTc interval. She became hypotensive despite appropriate medical management. Pacing through her implantable cardioverter-defibrillator was attempted but worsened her hypotension. Ventricular dyssynchrony was suspected. Temporary transvenous atrial pacing through the coronary sinus was performed, which stabilized her blood pressure and improved end-organ perfusion. A permanent biventricular pacemaker was later implanted, and she was safely discharged to a nursing home.
Temporary transvenous pacing through the coronary sinus, a novel approach to treat unstable bradycardia, may reduce ventricular dyssynchrony.
Core Tip: We present a case who received cardiac pacing through the coronary sinus and provide a summary of evidence in the current literature. A 55-year-old woman with unstable bradycardia complicating cardiogenic shock achieved cardiac resynchronization with placement of a temporary pacing wire to the coronary sinus. This modality, compared to pacing through the right ventricle apex, may induce a more physiologic ventricular depolarization and decrease ventricular dyssynchrony. This approach was safely applied in patients who had risks of ventricular dyssynchrony or required temporary atrial pacing. Pitfalls such as technical requirements and potential complications should be considered prior to electrode lead placement.
- Citation: Ju TR, Tseng H, Lin HT, Wang AL, Lee CC, Lai YC. Temporary coronary sinus pacing to improve ventricular dyssynchrony with cardiogenic shock: A case report. World J Clin Cases 2021; 9(20): 5562-5567
- URL: https://www.wjgnet.com/2307-8960/full/v9/i20/5562.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i20.5562
Placement of a temporary pacing wire (TPW) to the right ventricle apex (RVA) and implementing single chamber pacing are the most common approaches to treat unstable bradycardia[1]. In the presence of severe left ventricular (LV) dysfunction, this modality may worsen ventricular dyssynchrony and impede hemodynamic profiles[2]. While being a more complex procedure, placement of TPW to the coronary sinus (CS) could make atrial or LV pacing possible which results in better ventricular synchrony. Cardiac pacing through the CS has rarely been reported in different clinical settings[3-8]. We herein present a unique case of applying temporary atrial pacing through the CS in a patient who had unstable bradycardia complicating cardiogenic shock. In addition, we provide a review of literature of this novel approach.
A 55-year-old woman was transferred to our medical ward due to dizziness for 48 h.
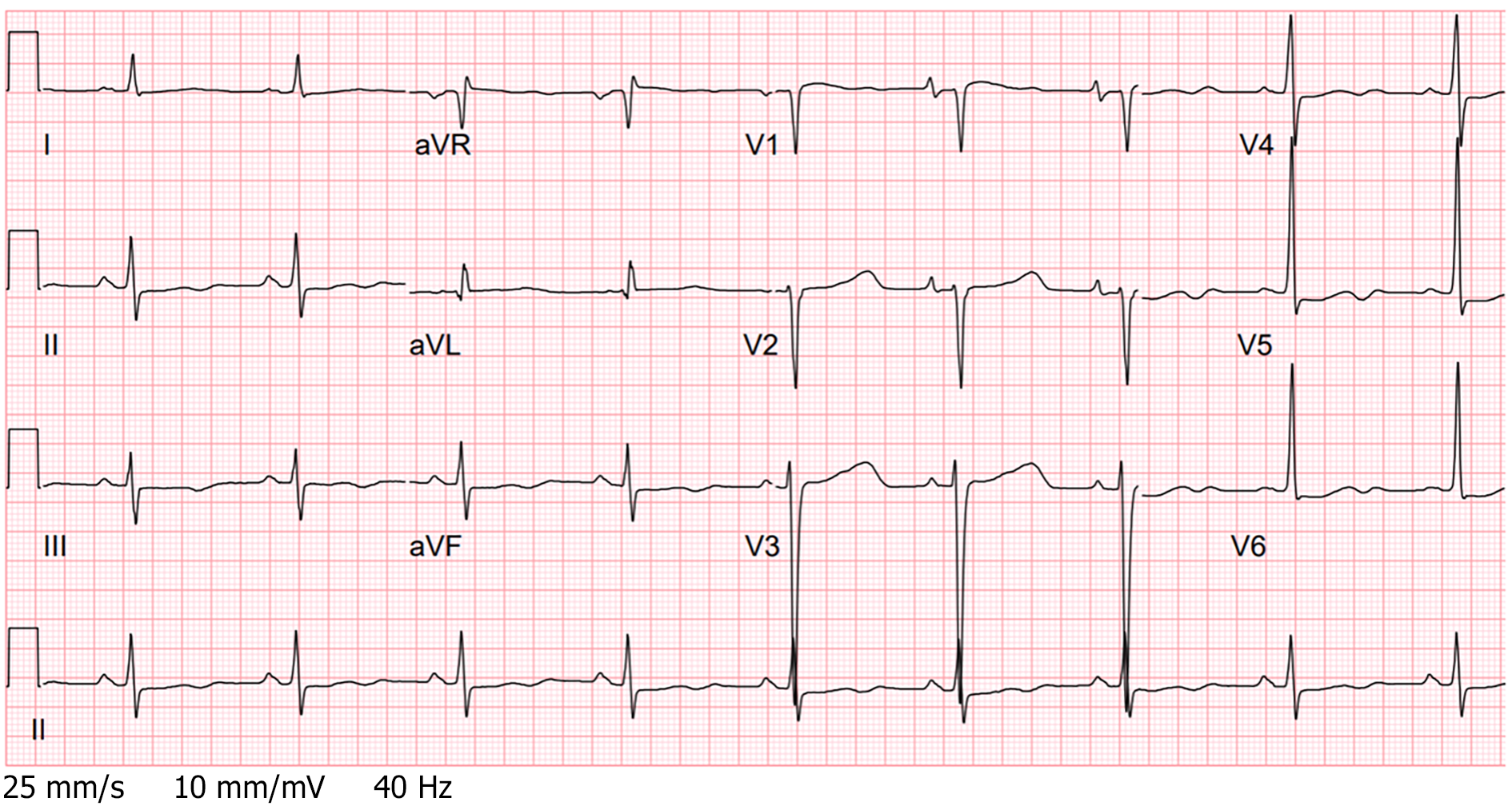
The patient was initially admitted to our rehabilitation ward after a large middle cerebral artery infarction and was transferred to our medical ward due to atrial fibrillation with a rapid ventricular rate due to fluid overload. Diuretics and low-dose beta blockers were administered. Her heart rhythm was spontaneously reversed to sinus rhythm for a short period of time. However, she started to have frequent polymorphic ventricular tachycardia (VT) resulting in cardiogenic shock. Despite receiving high doses of antiarrhythmic agents such as amiodarone, lidocaine, and multiple attempts of defibrillation, she still experienced multiple episodes of VT, along with sinus bradycardia and prolonged QTc interval of 516 milliseconds (Figure 1).
The patient had a history of non-ischemic cardiomyopathy with baseline ejection fraction of 15% with implantable cardioverter-defibrillator (ICD) placement and paroxysmal atrial fibrillation.
The patient's personal and family history were unremarkable.
Physical examination was notable for blood pressure of 87/50 mmHg, heart rate of 52 beats/min, cold extremities, rales over bilateral lung fields on auscultation, and confusion on neurological exam. She was afebrile and had no focal neurologic deficits.
Serial troponin I levels (< 0.03 mg/mL) were within the normal range. Her hemoglobin level was stable at 9.5 g/L. Biochemistry panels were notable for hyponatremia (125 mmol/L) and mild hypokalemia (3.2 mmol/L). Her B-type natriuretic peptide was 18388 pg/mL.
Electrocardiogram (ECG) revealed multiple VT episodes, along with sinus bradycardia and prolonged QTc interval of 516 milliseconds (Figure 1).
The final diagnosis was polymorphic VT and unstable bradycardia complicating cardiogenic shock.
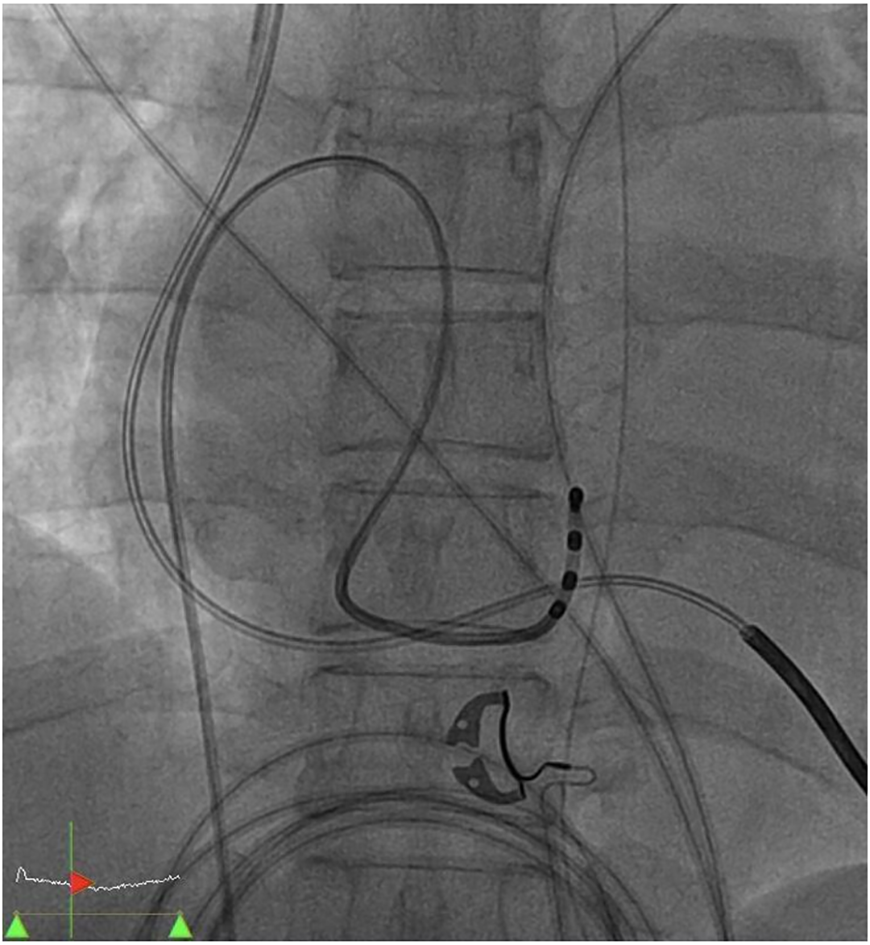
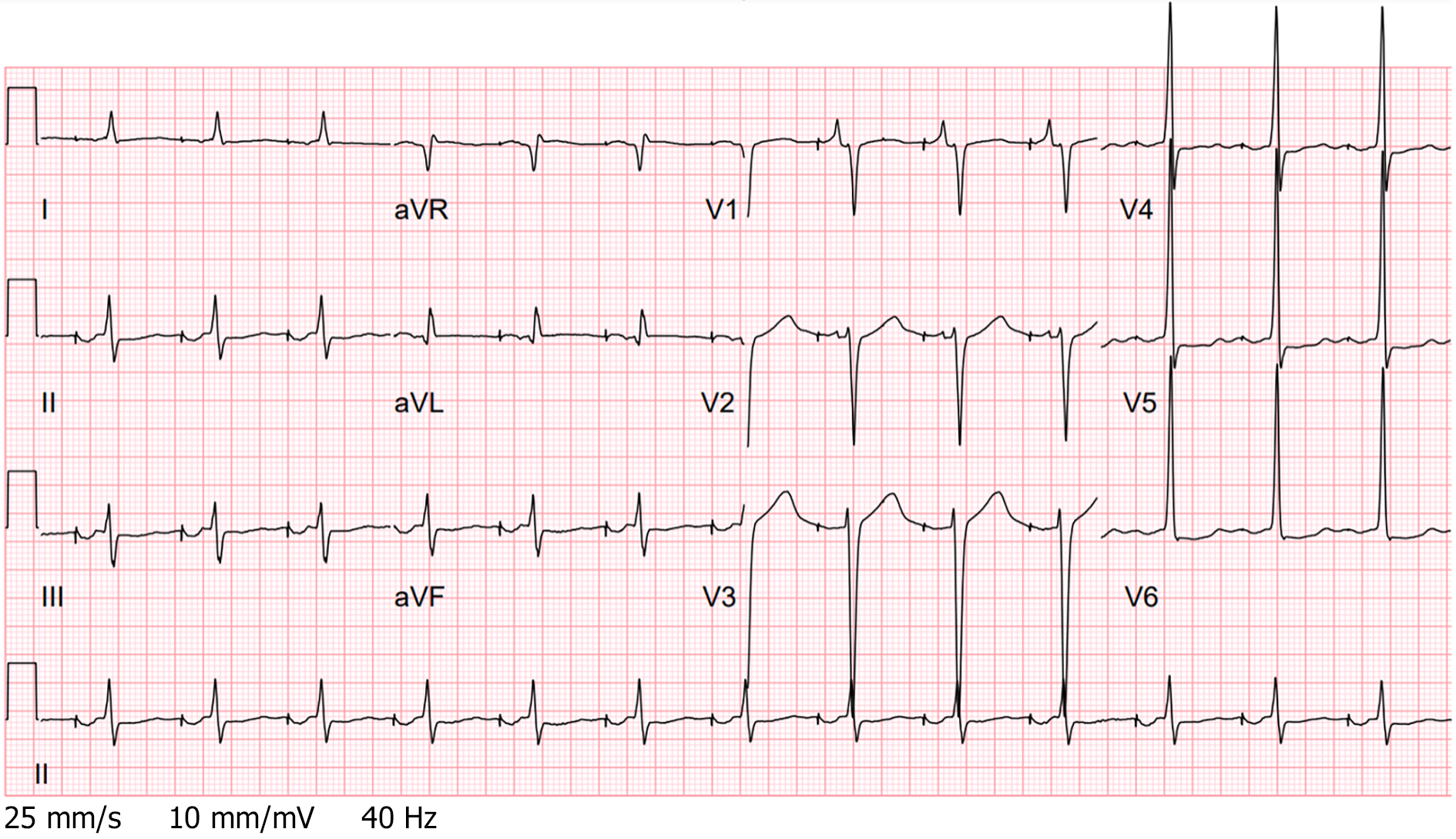
Dobutamine infusions at 7.5 μg/kg/min were started to treat cardiogenic shock. Cardiac catheterization was not conducted because of her unremarkable troponin levels and a normal coronary angiogram performed a month ago. The patient was deemed not a candidate for heart transplant or a left ventricle assisted device due to her poor functionality caused by her recent stroke. With regard to her unstable sinus bradycardia, we applied single chamber pacing through her ICD which adversely aggravated her hypotension. A ventricular dyssynchrony was suspected. To achieve cardiac resynchronization, we placed a TPW to the CS via right femoral vein cannulation under fluoroscopy guidance (Figure 2). The procedure was smooth and without any complications. Atrial pacing at 80 beats/min with an AOO mode was initiated (Figure 3).
The patient’s hemodynamic profiles improved significantly after the procedure. Dobutamine infusions were weaned off within a day following the procedure. She received permanent biventricular pacemaker implantation 3 d later and survived throughout hospitalization.
Temporary transvenous pacing has become the mainstay of treatment for patients who have unstable bradycardia[1]. In terms of electrode lead placement, the RVA is the preferred site given its easy accessibility and long-term stability of lead position and stimulation threshold[9]. While cardiac pacing through the RVA is generally well-tolerated in the short term, this approach could immediately worsen hemodynamic profiles in patients who are at risk of ventricular dyssynchrony[7]. A growing body of evidence has also shown that pacing through the RVA could lead to dyssynchronous LV electrical activation and remodeling of the myocardium, resulting in higher mortality in the long term[2,10]. Certain conditions may limit the use of cardiac pacing through the RVA. For example, failure to capture on pacemaker can occur in patients who have RV ischemia[9]. Stability of lead position would be challenging in patients who have significant tricuspid valve disease[11].
CS as an alternative temporary pacing site was previously studied as shown in the literature, primarily for the purpose of overdrive atrial pacing to suppress ventricular arrhythmia or LV pacing to reduce ventricular dyssynchrony (Table 1). In 2004, McNulty et al[3] first reported a case series of 10 patients who received temporary LV pacing through the CS while undergoing percutaneous coronary interventions involving the right coronary artery. Procedures were successful in eight cases, while one case had failure to capture on pacemaker and one case had difficulty in CS cannulation. No complications were noted, and the average procedure time was 3.8 min. Gimbel[4] then used the CS as the pacing site to assess the need of cardiac resynchronization therapy prior to biventricular pacemaker placement. In 2008, Osman et al[5] reported accidental placement of TPW at the CS in a heart failure patient with cardiogenic shock and complete AV block. Unexpectedly, the patient’s shock status significantly improved. Eitel et al[7] further evaluated the feasibility of temporary transvenous LV pacing through the CS in 15 patients who had refractory cardiogenic shock and asynchronous LV function. Among them, 10 patients (67%) acutely responded by improvement of hemodynamic parameters and no complications were noted. Two cases[6,8] where the CS was used as the pacing site to achieve overdrive atrial pacing and suppress ventricular arrhythmia were reported. Both cases succeeded without further complication.
| Ref. | Setting | Age, gender | Baseline cardiac rhythm | Indication of pacing | Additional lead /pacing mode | Outcome | ||
| Case report | ||||||||
| Gimbel[4], 2005 | Prior to biventricular pacemaker placement | 41, M | QRS duration > 120 ms | Assess the benefit of CRT | RA and RVA lead/AAI, DDD-RV, and DDD-BiV | ↑ Cardiac output | ||
| Osman et al[5], 2008 | Cardiogenic shock | 77, F | Left bundle branch block and intermittent AV block | Unstable bradycardiaLV pacing | No additional lead/VVI | Shock reversal | ||
| Segreti et al[6], 2013 | Prior to hip surgery | 82, M | Normal AV conduction multiple episodes of VT | Overdrive atrial pacing to suppress VT | No additional lead/Not specified | Resolution of VT | ||
| Vyas and Lokhandwala[8], 2018 | Post-CABG | 45, M | Normal AV conduction frequent PVC | Overdrive atrial pacing to suppress PVC and VF | No additional lead/Not specified | Resolution of PVC | ||
| Our case | Cardiogenic shock | 55, F | Sinus bradycardia prolonged QTc interval; Multiple episodes of VT | Unstable bradycardia; Overdrive atrial pacing to suppress VT | No additional lead/AOO | Shock reversal | ||
| Case series | ||||||||
| McNulty et al[3], 2004 (10 pts) | Percutaneous coronary intervention | N/A | Not documented | Assess the feasibility of pacing through CS | No additional lead/VVI | Eight pts: successful procedures | ||
| Eitel et al[7], 2013 (15 pts) | Cardiogenic shock and signs of LV asynchrony | N/A | LV asynchrony (e.g., QRS > 150 ms and poor LV function) | LV pacing to reduce ventricular dyssynchrony | RA lead/VVI in AFib, DDD in others | 10 pts (67%): ↑ cardiac output | ||
Pitfalls exist when it comes to applying temporary transvenous pacing through the CS. First, while placement of electrode catheters to the RVA can be performed in several ways, such as blind techniques, intracavitary ECGs or echocardiograms[1], placement of electrode catheters to the CS always requires fluoroscopy guidance. This requirement limits its use in patients with hemodynamic instability. Second, CS catheterization is not an innocuous procedure. A retrospective study of 62 patients who had CS catheterization during cardiac surgery showed that 6% of patients had blood in the pericardial space and 4.8% of patients had small bleeding spots in the RV wall following the procedure[12]. Consequently, CS catheterization should be performed by operators who can recognize and troubleshoot those complications. Lastly, difficulty in catheterization due to unsatisfactory CS anatomy occurs at times. Backup plans are needed if temporary pacing through the CS turns out to be unsuccessful.
Temporary transvenous pacing through the CS is a novel approach to treat unstable bradycardia. Compared to pacing through the RVA, pacing through the CS may induce a more physiologic ventricular depolarization and reduce ventricular asynchrony. This modality has been studied in patients who required overdrive atrial pacing or had unstable bradycardia and evidence of ventricular dyssynchrony. Technical requirements, potential complications and backup plans should be addressed prior to the procedure. Further prospective studies are warranted to establish the clinical benefits of this approach.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lang MJ, Ueda H S-Editor: Gao CC L-Editor: Webster JR P-Editor: Li X
| 1. | Tjong FVY, de Ruijter UW, Beurskens NEG, Knops RE. A comprehensive scoping review on transvenous temporary pacing therapy. Neth Heart J. 2019;27:462-473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 2. | Sweeney MO, Hellkamp AS, Ellenbogen KA, Greenspon AJ, Freedman RA, Lee KL, Lamas GA; MOde Selection Trial Investigators. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation. 2003;107:2932-2937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1195] [Cited by in RCA: 1207] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 3. | McNulty PH, Rice KS, Saraiya RB, McCann J, Ettinger SM, Gilchrist IC, Kozak M, Chambers CE. Usefulness of temporary left ventricular pacing through the coronary sinus as an adjunct to transfemoral percutaneous coronary intervention. Am J Cardiol. 2004;94:1055-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Gimbel JR. Method and demonstration of direct confirmation of response to cardiac resynchronization therapy via preimplant temporary biventricular pacing and impedance cardiography. Am J Cardiol. 2005;96:874-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Osman F, Ratib K, Krishnamoorthy S, Nadir A, Creamer J, Morley-Davies A. Temporary pacing wire in the coronary sinus: a novel treatment of acute heart failure? Europace. 2008;10:877-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Segreti L, Coluccia G, Zucchelli G, Soldati E, Di Cori A, Romano SL, Bongiorni MG. Temporary coronary sinus pacing to allow hip surgery in a patient with drug-refractory incessant ventricular tachycardia. Int J Cardiol. 2013;169:e21-e23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Eitel C, Gaspar T, Bode K, Andrea B, Sommer P, Stoepel C, Sarwas T, Grebe E, Thiele H, Hindricks G, Piorkowski C. Temporary left ventricular stimulation in patients with refractory cardiogenic shock and asynchronous left ventricular contraction: a safety and feasibility study. Heart Rhythm. 2013;10:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Vyas A, Lokhandwala Y. Coronary sinus as a site for stable temporary atrial pacing to tide over premature ventricular complex-triggered recurrent ventricular fibrillation in a patient with severe left ventricular dysfunction after coronary bypass surgery. Indian Heart J. 2018;70 Suppl 3:S483-S485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Sanaa I, Franceschi F, Prevot S, Bastard E, Deharo JC. Right ventricular apex pacing: is it obsolete? Arch Cardiovasc Dis. 2009;102:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Wilkoff BL, Cook JR, Epstein AE, Greene HL, Hallstrom AP, Hsia H, Kutalek SP, Sharma A; Dual Chamber and VVI Implantable Defibrillator Trial Investigators. Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual Chamber and VVI Implantable Defibrillator (DAVID) Trial. JAMA. 2002;288:3115-3123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1485] [Cited by in RCA: 1463] [Article Influence: 63.6] [Reference Citation Analysis (0)] |
| 11. | Lee CC, Do K, Patel S, Carlson SK, Konecny T, Chang PM, Doshi RN. Single- and dual-site ventricular pacing entirely through the coronary sinus for patients with prior tricuspid valve surgery. J Interv Card Electrophysiol. 2019;56:79-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Langenberg CJ, Pietersen HG, Geskes G, Wagenmakers AJ, Soeters PB, Durieux M. Coronary sinus catheter placement: assessment of placement criteria and cardiac complications. Chest. 2003;124:1259-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |