Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5191
Peer-review started: December 13, 2020
First decision: March 27, 2021
Revised: April 6, 2021
Accepted: May 8, 2021
Article in press: May 8, 2021
Published online: July 6, 2021
Processing time: 188 Days and 21.3 Hours
Myelodysplastic syndromes (MDSs) are a group of hematological diseases caused by expansion of an abnormal clone of hematopoietic stem cells. Primary MDS is a potentially premalignant clonal disorder that may progress to overt acute leukemia in 25%-50% of cases. However, most of these cases evolve into acute myeloid leukemia and rarely progress to acute lymphoblastic leukemia (ALL). Thus, transformation of MDS into B-cell ALL is rare.
A 58-year-old man was admitted to the hospital for reduced blood cell counts. Based on all the test results and the World Health Organization diagnosis and classification, the patient was finally diagnosed with ring-shaped sideroblastic MDS with refractory hemocytopenia due to multilineage dysplasia. We used red blood cell transfusions and other symptomatic support treatments. After 4 years, the patient felt dizziness, fatigue, and night sweats. We improved bone marrow and peripheral blood and other related auxiliary examinations. He was eventually diagnosed with B-lineage acute lymphocytic leukemia (MDS transformation).
The number of peripheral blood cells, type of MDS, proportion of primitive cells in bone marrow, and number and quality of karyotypes are all closely related to the conversion of MDS to ALL.
Core Tip: We present a case of ring-shaped sideroblastic myelodysplastic syndrome, with refractory hemocytopenia due to multi-lineage dysplasia, that was transformed into B-cell acute lymphoblastic leukemia. Even though the lymphoid progression in myelodysplastic syndrome has been reported previously, most displayed myeloid-lymphoid hybrid, B cell acute lymphoblastic leukemia is rarely reported, and the specific mechanism is still unclear. We report a rare lymphoid transformation in order to provide information for the study of specific mechanism, and help doctors to provide appropriate treatment to patients.
- Citation: Zhu YJ, Ma XY, Hao YL, Guan Y. Myelodysplastic syndrome transformed into B-lineage acute lymphoblastic leukemia: A case report. World J Clin Cases 2021; 9(19): 5191-5196
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5191.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5191
Myelodysplastic syndromes (MDSs) are a group of hematological diseases caused by the expansion of an abnormal clone of hematopoietic stem cells, progressively replacing their normal counterparts in the bone marrow (BM). The expansion of the abnormal clone causes various degrees of peripheral cytopenia and abnormal function of hematological cells. The French-American-British cooperative group proposed five subgroups of MDS primarily based on the percentage of blasts in the BM and peripheral blood: Refractory anaemia, refractory anaemia with ringed sideroblasts, refractory anaemia with excess blasts, refractory anaemia with excess blasts in transformation, and chronic myelomonocytic leukemia. Soon afterwards, the World Health Organization (WHO) proposed a new classification for MDS on this basis, but its biological and clinical relevance has been questioned. MDS blasts often coexpress stem cell antigens and late-stage myeloid antigens asynchronously but rarely express T- or B-lymphoid cell-specific antigens[1].
Acute lymphoblastic leukemia (ALL) is characterized by clonal expansion of lymphoid blasts in BM, blood, and other tissues and can be divided into the T lineage and B lineage. B-cell ALL (B-ALL) is an aggressive malignant neoplasm of the BM and blood, and its cells proliferate uncontrollably. ALL is characterized by immature B-cell progenitors (i.e., lymphoid or lymphoblastic cells) that cannot mature properly into lymphocytic B cells[2]. B-ALL is the most common type of ALL.
Primary MDSs are potentially premalignant clonal disorders, and in 25%-50% of cases they may progress to overt acute leukemia. However, most of these cases evolve into acute myeloid leukemia, and some studies have shown that MDS may occasionally progress to pure acute lymphoblastic or hybrid (myeloid–lymphoid) leukemia[3-5]. Here, we report a unique patient who presented with MDS and soon developed precursor B-ALL.
The patient was diagnosed with MDS for > 4 years and fatigue aggravation for 10 d.
A 58-year-old man of Han nationality was admitted to the hospital due to a reduction in blood cells: White blood cell count (WBC) of 2.3 × 109/L, neutrophil count of 1.76 × 109/L, erythrocyte count of 1.76 × 1012/L, haemoglobin (Hb) of 56 g/L, and platelet count of 127 × 109/L. A BM smear revealed abnormal hematopoiesis in the granulocytes, erythrocytes, and megakaryocytes; however, BM cells exhibited active proliferation. At this point, we suspected MDS-refractory cytopenia with multilineage dysplasia and ringed sideroblasts (MDS-RCMD-RS). The BM biopsy aspirate was sent for immunohistochemistry to exclude MDS. Immunotyping of the cells showed that the proportion of lymphocytes and immature cells among nucleated cells was not high; monocytes were abnormal and expressed CD56; and the relationship between CD16/CD13 and granulocytes was abnormal. The anti-human globulin test (Coombs test) was negative, and negative CD55 and CD59 expression was also noted. Therefore, combining all the test results and the WHO diagnosis and classification standard, we concluded that the diagnosis was MDS with ring sideroblasts combined with RCMD. The patient underwent red blood cell transfusion to correct the anaemia, and erythropoietin (1 U qod), cyclosporin A (50 mg tid), stanozolol (2 mg tid), and reconstituted blood platelets (1.75 g tid) were administered. The patient’s hemogram recovered, and his symptoms improved. He was discharged from the hospital and continued oral medication. After three courses of treatment, his BM smear indicated that all three blood lines exhibited active proliferation: Granulocytes proliferated with 0.5% myeloblasts, erythrocytes proliferated with partial megaloblastic change, the lymphocyte ratio was decreased, and megakaryocytes were easily observed in the whole film. We continued to provide symptomatic supportive therapy, such as cyclosporin A (150 mg q12 h), stanozolol (2 mg tid), and thalidomide (25 mg qn). After > 1 year of oral medication, the blood cells recovered to normal, and he stopped the medication. Unfortunately, the patient was lost to follow-up. Four years later, the patient came to the hospital again and complained of dizziness, fatigue, and night sweats.
The patient had a previous history of hypothyroidism.
The patient denied any other specific personal or family history of other diseases.
The patient presented with the following vital signs: Body temperature, 36.8 °C; blood pressure, 103/68 mmHg; pulse rate, 86 beats/min; and respiratory rate, 22 breaths/min. The patient’s conjunctiva and skin were pale, and the sclera was not yellow. He had clear breathing sounds in both lungs. His heart rate was 86 bpm with a normal rhythm, and no other abnormalities were noted.
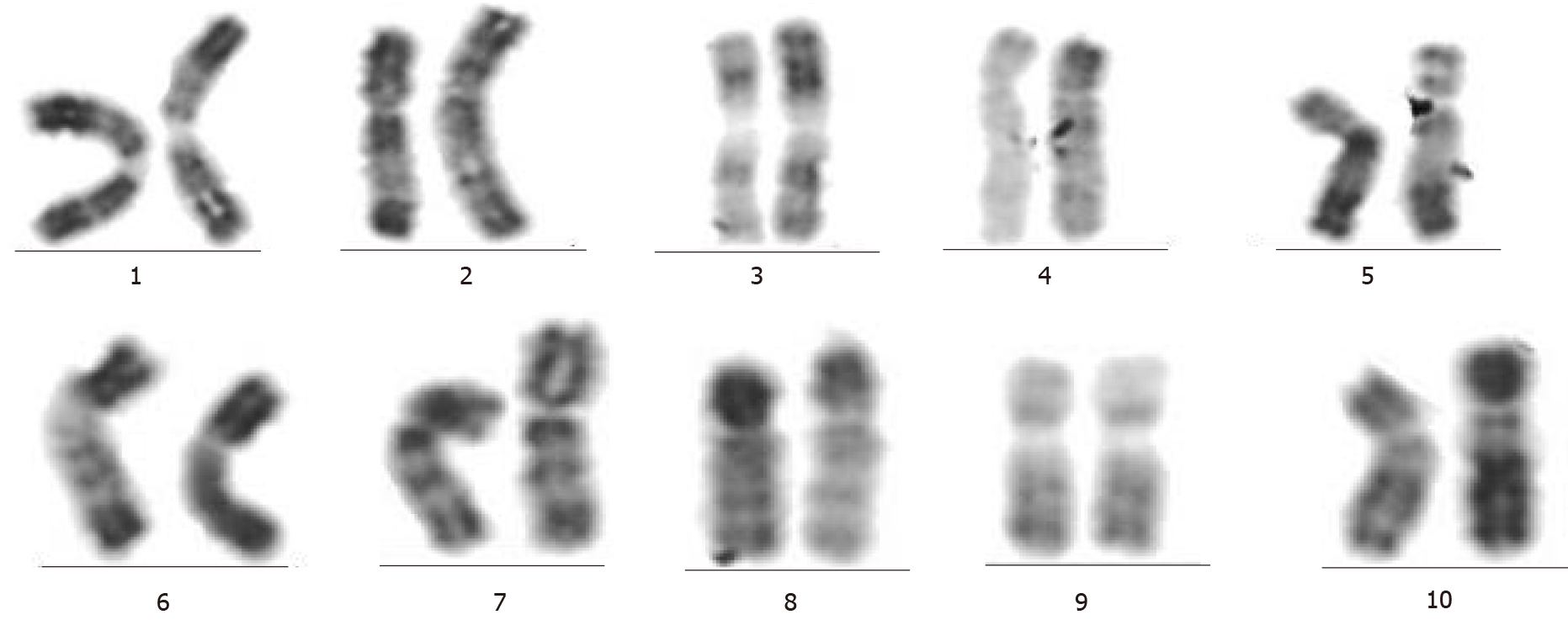
His blood count showed a WBC of 7.54 × 109/L, neutrophil count of 1.02 × 109/L, Hb of 53 g/L, and platelet count of 36 × 109/L. The BM smear revealed that all three blood cell lines exhibited active hyperplasia and included 52% primary cells. Four days later, his blood test showed Hb of 71 g/L, WBC of 10.29 × 10/L, neutrophil count of 1.72× 109/L, and platelet count of 32 × 109/L. The BM biopsy showed that myelosis was extremely active (approximately 90%). The number of immature cells increased significantly, and partial mature stage granulocytes were scattered or clustered. Numerous megakaryocytes and reticular fibre staining (MF-1) (MF: reticular fibre) was noted. To distinguish the nature and origin of the tumour, the degree of BM fibrosis was evaluated. The reticular fibres in tissues were clearly displayed by silver immersion staining; thus, we considered B-ALL as the diagnosis. Flow cytometry of the BM aspirate showed that 58.37% of cells were abnormal. In addition, these cells were positive for expression of CD38, CD34, CD123, TDT, CD9, CD13, and HLA-DR. Partial expression of CD117 and CD33 and weak signals for CD19, CD22, and cCD79a were detected (Table 1). Primitive B lymphocytes were also visible. These results confirmed the B-ALL phenotype. The paroxysmal nocturnal hemoglobinuria test showed no abnormal clones. No fusion gene was detected. The BM chromosome showed 47, XY, +21 (Figure 1), and the clonal abnormality was +21.
| Immunophenotype of B-ALL | |
| Positive markers | CD34, CD38, HLA-DR, CD123, CD9, TDT, CD13, CD117 (partial), CD33 (partial), CD22 (dim), CD19 (dim), cCD79a (dim) |
| Negative markers | CD7, CD15, CD64, CD11b, CD5, CD20, CD2, CD10, CD36, CD4, CD14, MPO, cCD3, mCD3, CD56 |
The patient was eventually diagnosed with B-ALL (MDS transformation). He also had hypothyroidism and lung infection.
Based on the patient’s blood and BM results on admission and considering that he had AML, we temporarily administered azacytidine (100 mg d 2-6) and CAG [epirubicin (20 mg d 1-4), cytarabine (20 mg q12 h d 11-14), and granulocyte colony-stimulating factor (300 mg d 1-14) after excluding any contraindications. When all the test results were obtained, he was eventually diagnosed with B-ALL (MDS transformation). We adjusted the treatment scheme to VDCP (vindesine sulfate 4 mg d 4, 11, 18 and 25; epirubicin 20 mg d 4; cyclophosphamide 1.4 g d 4; and prednisolone 80 mg d 4-5; 60 mg qd gradually reduced) after excluding any contraindications.
After one course of treatment, BM morphological analysis showed that the patient was in complete remission. After chemotherapy was completed and his condition improved, he was discharged from the hospital. His blood condition must be regularly reviewed, and he is regularly admitted to the hospital for chemotherapy.
MDSs are a group of hematological diseases caused by expansion of an abnormal clone of hematopoietic stem cells and are characterized by cytopenia, BM hypercellularity, and abnormal blood cell differentiation (ineffective hematopoiesis)[6]. MDS is a malignant disorder of hematopoietic progenitors in which the BM is composed of clonal hematopoietic cells showing various degrees of differentiation in each case. The abnormal hematopoietic clone in MDS can give rise to mature blood cells, and these cells are functionally and morphologically abnormal. We generally believe that MDS has the potential for myeloid and lymphoid differentiation[7]. Based on flow cytometric immunophenotyping, approximately 85% of blast cells in the leukemic transformation from MDS display a myeloid phenotype, whereas 15% of blast cells display a hybrid (myeloid-lymphoid) phenotype. It is rare for only the lymphoid phenotype to be displayed[8,9].
Here, we describe the conversion of MDS to B-ALL. This case clinically supported the nature of MDS as a pluripotent hematopoietic stem cell disorder. MDS is thought to be a preleukaemic state and a recognizable intermediate stage in the multistage pathogenesis of acute leukemia. MDS can be transformed into acute leukemia, usually of a myeloid phenotype. The transformation of MDS into ALL is rare, and the underlying mechanism of lymphoid transformation is unknown.
Therefore, we collected relevant data on the conversion of MDS to AL and analyzed and summarized similar case reports. We found that some studies have repeatedly mentioned three explanations for the rarity of transformation to acute leukemia from MDS. First, MDS is a multipotent hematopoietic stem cell disorder. It may have myelopoietic potential as well as lymphopoietic potential, but there may be specific impairment of lymphopoiesis by intrinsic or extrinsic factors. Thus, acute leukemia secondary to MDS is generally believed to be of myeloid origin. Recent studies have suggested that on rare occasions, clonal expansion leading to MDS might occur beyond the committed myeloid phenotype but at the uncommitted stem cell level. Under this condition, all the progenies harbour genetic instability. Thus, there is a possibility that the promotion needed for the conversion of MDS into acute leukemia occurs at the committed lymphoid stem cell level[10,11]. We believe that our case is not excluded from this possibility. Second, as a consequence of MDS-specific defects in lymphopoiesis, ALL target cells may be absent or scarce[12]. Third, we think that the influence of the tumour microenvironment on its transformation cannot be excluded. The tumour microenvironment is essential for tumour cell proliferation, angiogenesis, invasion, and metastasis by providing survival signals and a sanctuary site for tumour cells. The tumour marrow microenvironment provides a sanctuary site for MDS and leukemia and likely contributes to residual disease and reoccurrence[13]. Relevant studies have shown that the tumour microenvironment of MDS patients has undergone significant changes with a reduced count of CD4+ T cells and a more frequent presence of markers related to T cell exhaustion. This finding indicates that T cell damage is the main factor in the microenvironment of MDS. Once the progression of MDS exhibits a trend of acute lymphocyte transformation, if the surface markers of T cells are further attacked and the T cell markers are reduced, the surface markers of B cells are dominant[14]. All of these factors may promote the conversion of MDS to B-ALL. Recent studies on chromosomal genetic abnormalities have also gradually emerged. Related reports indicate that MDS can progress to acute leukemia by acquiring multiple genetic abnormalities. A variety of cytogenetic abnormalities are noted in MDS patients, including nonequilibrium chromosome deletion changes, and the transformation rate of ALL with abnormal karyotypes is obviously greater than that of normal karyotypes. The more common karyotypes are +8, -7/7q-, and +11, and rare karyotypes include -5/5q-, -Y, and 20q-. However, there are no reports of chromosome 21 abnormalities[15,16]. In the reported chromosomal test results of this patient, we reported a +21 clonal abnormality, which may be one of the reasons for his final convergence to ALL. With the increasing number of chromosome abnormal karyotypes, the conversion rate of ALL is also increasing.
In addition, in the summary of reports of similar cases, we found that MDS with three-line reduction and most active myelodysplasia exhibits a greater risk of developing acute leukemia. Even if it is converted to acute leukemia, the patient still has morphological residual traces of morbid hematopoiesis of MDS. The BM morphology of MDS/ALL often exhibits abnormal hyperplasia of the granulocyte, erythroid, and megakaryocytic lines[17]. The early stage of the patient was MDS-RCMD, and the proportion of erythroid, granulocyte, or megakaryocytic lines may also be related to the type of leukemia transformed. The early manifestation of the current patient was MDS-RCMD-RS, and the three lines had abnormal hyperplasia and abnormal proportions, which may promote conversion to ALL. However, these notions still require verification.
The number of peripheral blood cells in patients with MDS, the type of MDS, the proportion of primitive cells in BM, and the number and quality of karyotypes are all closely related to the conversion of MDS to ALL. In our case, the number of peripheral blood cells was significantly reduced. In addition, abnormal hyperplasia of his three blood cell lines in the BM was noted, and there were abnormalities in the karyotype +21. These may be related factors that promote the transformation of MDS into ALL, but the specific mechanism of conversion to B-ALL should be further explored.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nwabo Kamdje AH S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Ogata K, Nakamura K, Yokose N, Tamura H, Tachibana M, Taniguchi O, Iwakiri R, Hayashi T, Sakamaki H, Murai Y, Tohyama K, Tomoyasu S, Nonaka Y, Mori M, Dan K, Yoshida Y. Clinical significance of phenotypic features of blasts in patients with myelodysplastic syndrome. Blood. 2002;100:3887-3896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 135] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Managò S, Valente C, Mirabelli P, Circolo D, Basile F, Corda D, De Luca AC. A reliable Raman-spectroscopy-based approach for diagnosis, classification and follow-up of B-cell acute lymphoblastic leukemia. Sci Rep. 2016;6:24821. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Tricot G, Vlietinck R, Boogaerts MA, Hendrickx B, De Wolf-Peeters C, Van den Berghe H, Verwilghen RL. Prognostic factors in the myelodysplastic syndromes: importance of initial data on peripheral blood counts, bone marrow cytology, trephine biopsy and chromosomal analysis. Br J Haematol. 1985;60:19-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 148] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Berneman ZN, Van Bockstaele D, De Meyer P, Van der Planken M, Vertessen F, De Bock R, Peetermans ME. A myelodysplastic syndrome preceding acute lymphoblastic leukaemia. Br J Haematol. 1985;60:353-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Nagler A, Brenner B, Tatarsky I. Secondary refractory anemia with excess of blasts in transformation terminating as acute lymphoblastic leukemia. Acta Haematol. 1986;76:164-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Sabattini E, Bacci F, Sagramoso C, Pileri SA. WHO classification of tumours of haematopoietic and lymphoid tissues in 2008: an overview. Pathologica. 2010;102:83-87. [PubMed] |
| 7. | Janssen JW, Buschle M, Layton M, Drexler HG, Lyons J, van den Berghe H, Heimpel H, Kubanek B, Kleihauer E, Mufti GJ. Clonal analysis of myelodysplastic syndromes: evidence of multipotent stem cell origin. Blood. 1989;73:248-254. [PubMed] |
| 8. | San Miguel JF, Hernández JM, González-Sarmiento R, González M, Sánchez I, Orfao A, Cañizo MC, López Borrasca A. Acute leukemia after a primary myelodysplastic syndrome: immunophenotypic, genotypic, and clinical characteristics. Blood. 1991;78:768-774. [PubMed] |
| 9. | Orfao A, Ortuño F, de Santiago M, Lopez A, San Miguel J. Immunophenotyping of acute leukemias and myelodysplastic syndromes. Cytometry A. 2004;58:62-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Pajor L, Matolcsy A, Vass JA, Méhes G, Marton E, Szabó F, Iványi JL. Phenotypic and genotypic analyses of blastic cell population suggest that pure B-lymphoblastic leukemia may arise from myelodysplastic syndrome. Leuk Res. 1998;22:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Koh YR, Cho EH, Park SS, Park MY, Lee SM, Kim IS, Lee EY. A rare case of transformation of childhood myelodysplastic syndrome to acute lymphoblastic leukemia. Ann Lab Med. 2013;33:130-135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Disperati P, Ichim CV, Tkachuk D, Chun K, Schuh AC, Wells RA. Progression of myelodysplasia to acute lymphoblastic leukaemia: implications for disease biology. Leuk Res. 2006;30:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 62] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Zhou J, Mauerer K, Farina L, Gribben JG. The role of the tumor microenvironment in hematological malignancies and implication for therapy. Front Biosci. 2005;10:1581-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Montes P, Bernal M, Campo LN, González-Ramírez AR, Jiménez P, Garrido P, Jurado M, Garrido F, Ruiz-Cabello F, Hernández F. Tumor genetic alterations and features of the immune microenvironment drive myelodysplastic syndrome escape and progression. Cancer Immunol Immunother. 2019;68:2015-2027. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 15. | Bain BJ. The relationship between the myelodysplastic syndromes and the myeloproliferative disorders. Leuk Lymphoma. 1999;34:443-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Hasle H, Baumann I, Bergsträsser E, Fenu S, Fischer A, Kardos G, Kerndrup G, Locatelli F, Rogge T, Schultz KR, Starý J, Trebo M, van den Heuvel-Eibrink MM, Harbott J, Nöllke P, Niemeyer CM; European Working Group on childhood MDS. The International Prognostic Scoring System (IPSS) for childhood myelodysplastic syndrome (MDS) and juvenile myelomonocytic leukemia (JMML). Leukemia. 2004;18:2008-2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 55] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Haferlach T. The Molecular Pathology of Myelodysplastic Syndrome. Pathobiology. 2019;86:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |