Published online Jul 6, 2021. doi: 10.12998/wjcc.v9.i19.5028
Peer-review started: March 2, 2021
First decision: April 4, 2021
Revised: April 10, 2021
Accepted: April 20, 2021
Article in press: April 20, 2021
Published online: July 6, 2021
Processing time: 113 Days and 22.5 Hours
In both national and international studies, the safety and effectiveness of treatment with the Solitaire stent in patients with ischemic stroke caused by acute large vessel occlusion were good, and the disability rate was significantly reduced. However, there are currently only a few reports on the differences in endovascular treatment for different etiological classifications, especially in the anterior cranial circulation, aorta atherosclerotic stenosis, and acute thrombosis.
To investigate the efficacy of Solitaire AB stent-release angioplasty in patients with acute middle cerebral artery atherosclerosis obliterative cerebral infarction.
Twenty-five patients with acute middle cerebral atherosclerosis obliterative cerebral infarction were retrospectively enrolled in this study from January 2017 to December 2019. The Solitaire AB stent was used to improve anterior blood flow to maintain modified cerebral infarction thrombolysis [modified thrombolysis in cerebral infarction (mTICI)] at the 2b/3 level or above, the stent was then unfolded and released.
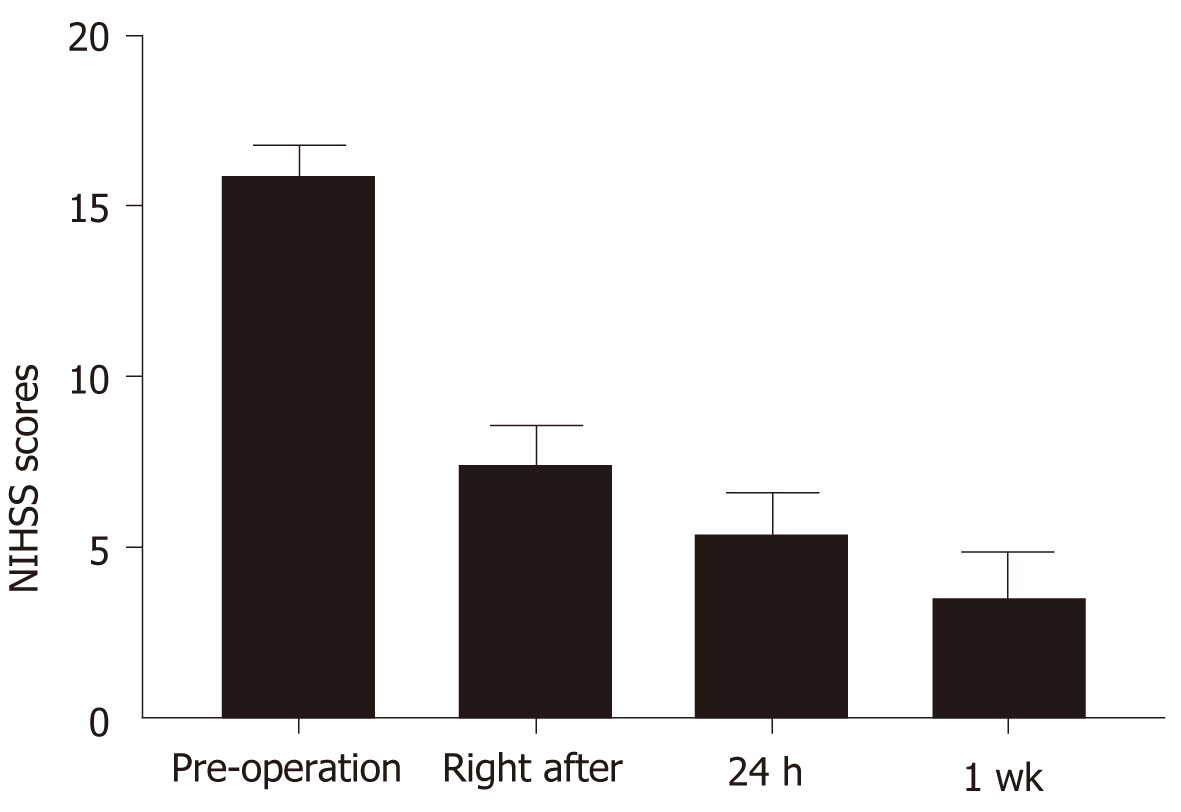
All 25 patients underwent successful surgery, with an average recanalization time of 23 min. One patient died of cerebral hemorrhage and cerebral herniation after the operation. The National Institutes of Health Stroke Scale (NIHSS) scores immediately after surgery (7.5 ± 5.6), at 24 h (5.5 ± 5.6) and at 1 wk (3.6 ± 6.7) compared with the preoperative NIHSS score (15.9 ± 4.4), were significantly different (P < 0.01). One case of restenosis was observed 3 mo after surgery (the stenosis rate was 50% without clinical symptoms), the modified Rankin scale scores were 0 points in 14 cases (56%), 1 point in 4 cases (16%), 2 points in 2 cases (8%), 3 points in 3 cases (12%), 4 points in 1 case (4%), and 6 points in 1 case (4%).
In acute middle cerebral artery atherosclerosis obliterative cerebral infarction, when the Solitaire AB stent is unfolded and the forward blood flow is maintained at mTICI level 2b/3 or higher, stent release may be a safe and effective treatment method; however, long-term observation and a larger sample size are required to verify these findings.
Core Tip: There are currently only a few reports on the differences in endovascular treatment for different etiological classifications, especially in the anterior cranial circulation, aorta atherosclerotic stenosis, and acute thrombosis. There are no relevant reports on the use of Solitaire stent mechanical thrombectomy or stent release angioplasty when used above level 2b/3 (modified thrombolysis in cerebral infarction).
- Citation: Wang XF, Wang M, Li G, Xu XY, Shen W, Liu J, Xiao SS, Zhou JH. Efficacy of Solitaire AB stent-release angioplasty in acute middle cerebral artery atherosclerosis obliterative cerebral infarction. World J Clin Cases 2021; 9(19): 5028-5036
- URL: https://www.wjgnet.com/2307-8960/full/v9/i19/5028.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i19.5028
In both national and international studies, the safety and effectiveness of treatment with the Solitaire stent in patients with ischemic stroke caused by acute large vessel occlusion were good, and the disability rate was significantly reduced[1,2]. However, there are currently only a few reports on the differences in endovascular treatment for different etiological classifications[3], especially in the anterior cranial circulation, aorta atherosclerotic stenosis, and acute thrombosis. There are no relevant reports on the use of Solitaire stent mechanical thrombectomy or stent release angioplasty when used above level 2b/3 [modified thrombolysis in cerebral infarction (mTICI)]. This study reports the outcome of 25 cases with acute middle cerebral artery atherosclerosis occlusive cerebral infarction using Solitaire AB stent-release angioplasty during endovascular treatment.
Twenty-five patients (14 males and 11 females, aged 44-80 years, with an average age of 64.6 ± 5.3 years) with acute middle cerebral artery atherosclerosis obliterative cerebral infarction were retrospectively included in this study from January 2017 to December 2019. The onset time was 1.5-7 h, and the average onset time was 4.5 h. Twenty-one cases (84%) had hypertension, 15 cases (60%) had diabetes, 22 cases (88%) had hyperlipidemia, 5 cases (20%) had peripheral atherosclerosis, 9 cases (36%) had coronary atherosclerotic heart disease, 18 cases (72%) had previous stroke or transient ischemic attack, 13 cases (52%) were smokers (continuous or cumulative smoking for 6 mo or more in their lifetime), and 9 cases (36%) consumed alcohol. Nineteen cases (76%) underwent intravenous thrombolysis combined with endovascular treatment, 6 cases (24%) underwent direct endovascular treatment (lesions may appear hyperintense on fluid-attenuated inversion recovery with increased diffusion-weighted imaging and decreased apparent diffusion coefficient values[4], all had magnetic resonance imaging diffusion weighted imaging-fluid attenuation inversion recovery mismatch), and had a femoral artery puncture time of 77 ± 8.2 min, the average recanalization time was 23 min, and the average operation time was 57 min.
Inclusion criteria: After the patients had undergone cranial computed tomography (CT) to exclude cerebral hemorrhage, the preoperative early CT scores of the Alberta Stroke Project were ≥ 6 points, which was confirmed by CT angiography (CTA), magnetic resonance angiography, or digital subtraction angiography (DSA) as intracranial brain middle artery occlusion; 18 years ≥ age ≤ 80 years; time from onset to femoral artery puncture < 8 h; National Institutes of Health Stroke Scale (NIHSS) scores ≥ 6 points.
Exclusion criteria: A past history of cerebral hemorrhage, history of intracranial aneurysm or bleeding tendency; preoperative modified Rankin scale (mRS) score ≥ 2 points; history of atrial fibrillation or cardiogenic embolism caused by atrial fibrillation; other endovascular treatments using non-stent-like embolization devices; combined with insufficiency or failure of important organs; life expectancy less than 6 mo; uncontrolled severe hypertension. This study was reviewed and approved by the Ethics Committee of Puai Hospital Affiliated to Tongji Medical College of Huazhong University of Science and Technology. All patients or their families signed an informed consent.
Preoperative management: Preoperative cranial CT excluded bleeding, and blood pressure was controlled below 180/105 mmHg after intensive blood pressure reduction, and patients within the intravenous thrombolysis time window were given recombinant tissue-type plasminogen activator (rt-PA). Intravenous thrombolytic therapy (0.9 mg/kg, 10% of the dose by intravenous bolus in 1 min, the remainder was given over 60 min to complete the infusion), patients who exceeded the intravenous thrombolytic time window were given clopidogrel 300 mg, and aspirin 100 mg orally or nasogastrically.
Surgical technique: The patient was placed in the supine position, 1% lidocaine local anesthetic and dexmedetomidine for sedation were administered via femoral artery puncture, an 8F arterial sheath was introduced, an 8F guiding catheter was selected, and a 0.014 inch micro-ribbon micro-catheter was passed through. After occlusion of the blood vessel, the micro-catheter was gradually withdrawn following withdrawal of the micro-guide wire, and the distal end of the occlusion site was determined by segmental radiography. The top of the Rebar 18 micro-catheter was placed at least 5 mm away from the occlusion, and the Solitaire AB stent (4 mm × 20 mm, Medtronic) at the distal end was inserted to the top of the micro-catheter. The micro-catheter was then slowly withdrawn and the stent was unfolded. Five minutes after the stent was unfolded, DSA was performed to observe blood perfusion and the stent shape. If the distal forward blood flow was above 2b, observation was continued for 15 min, and then tirofiban was injected intravenously (8 μg/kg, within 3 min) before the stent was released, and 0.15 μg/kg/min was administered for 24 h after the operation[5]. Immediately after surgery, CT was performed to identify intracranial hemorrhage, and normal heparin saline was injected intravenously throughout the operation.
Postoperative management: Close postoperative monitoring in the intensive care unit included vital signs, strict control of blood pressure, and systolic blood pressure was maintained below 140 mmHg; low molecular weight heparin was injected subcutaneously as needed; postoperative dynamic review of head CT was performed to determine the presence of intracranial hemorrhage and new-onset infarction. The patients were treated with overlapping dual antiplatelet drugs (aspirin 100 mg/d and clopidogrel 75 mg/d) 4 h before stopping tirofiban, and were given long-term single antiplatelet drugs for 3 consecutive mo.
Efficacy and safety: Postoperative re-examination of head CT and CTA to determine the presence of intracranial hemorrhage, new infarction, and patency of cerebral blood vessels was performed. NIHSS scores were used to determine the patient's immediate recovery, at 24 h, and 1 wk after surgery. The mRS score was used to evaluate the prognosis of patients at 3 mo.
SPSS 22.0 was used for analysis; measurement data are expressed as mean ± SD using the t test; and counting data are expressed as frequency or percentage. P < 0.05 was considered statistically significant.
All 25 patients underwent successful surgery, with an average recanalization time of 23 min (the recanalization time refers to the time from femoral artery puncture to blood flow recanalization). The NIHSS score immediately after surgery was (7.5 ± 5.6), at 24 h (5.5 ± 5.6), and at 1 wk (3.6 ± 6.7). Compared with the preoperative NIHSS score (15.9 ± 4.4), the scores after surgery were significantly different (P < 0.01) (Figure 1). One patient died due to cerebral hemorrhage and herniation after the operation. One patient had restenosis 3 mo after surgery (the stenosis rate was 50% without clinical symptoms), the mRS score was 0 points in 14 cases (56%), 1 point in 4 cases (16%), 2 points in 2 cases (8%), 3 points in 3 cases (12%), 4 points in 1 case (4%), and 6 points in 1 case (4%).
Mechanical thrombectomy has become the standard and preferred treatment for acute large vessel occlusion[6-8]. The Solitaire AB stent is composed of a self-expanding nickel-titanium alloy. It is a laser engraved open-loop stent with a diameter of 4-6 mm and a length of 15-30 mm. It is installed on a 0.016 inch push guide-wire. It can be electrolytically removed and an NDS-2 release device is used to release the stent. The Solitaire AB stent has the best radial force to reduce residual stenosis[9], is a representative third-generation intravascular mechanical thrombectomy device and its strong thrombectomy ability has been demonstrated in clinical trials[10-13].
In the treatment of acute ischemic large vessel occlusion, the Solitaire AB stent is mainly used for mechanical thrombus removal alone or in combination with an intermediate catheter, and there are few clinical studies on direct release. The results of a Chinese study on intracranial arterial stenosis and occlusion showed that the incidence of intracranial atherosclerosis in patients with ischemic stroke or transient ischemic attack in China was 46.6%, and the symptoms in patients with intracranial atherosclerotic stenosis were more severe in those with acute anterior circulation large vessel occlusion caused by large atherosclerotic stenosis, and mechanical thrombus removal with a retrievable stent alone was often difficult to achieve blood vessel recanalization, and hospital stay was longer[14]. The risk of re-occlusion caused by thrombosis was very high. Often used as a remedy after other therapeutic measures have failed[15-17], mechanical thrombus removal alone cannot relieve stenosis of the target vessel before stent implantation[18]. There are also rare reports of Solitaire stent retention in situ after thrombectomy[19].
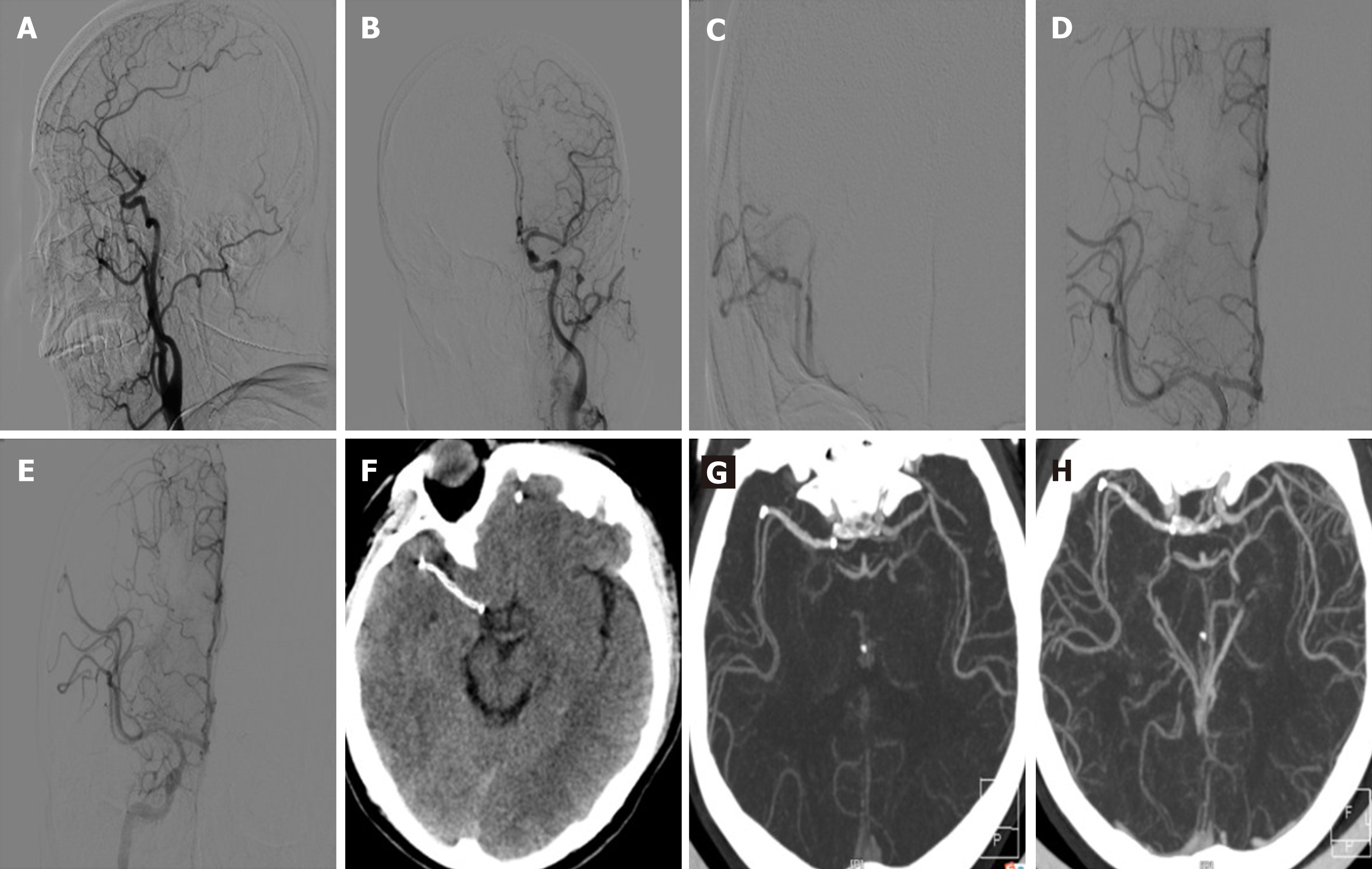
Researchers at home and abroad agree that the purpose of mechanical thrombus removal is to obtain blood flow reperfusion, and not only to achieve recanalization of blood vessels. Reperfusion is the key to improving prognosis. In all current endovascular treatment trials, whether stent thrombectomy or aspiration studies, the modified cerebral infarction thrombolytic classification mTICI 2b/3 is often used as the standard for evaluating effective reperfusion[20-22]. In clinical work, for patients with acute occlusion of intracranial middle cerebral artery atherosclerotic stenosis, if the anterior blood flow was maintained above mTICI 2b/3 after the Solitaire AB stent was unfolded, repeated thrombus removal may easily lead to re-occlusion of the blood vessels, thereby affecting patient prognosis. Possible reasons for this are mechanical thrombectomy injury caused by blood platelet aggregation, lipid core exposure leading to platelet activation and aggregation, in situ stenosis not relieved, blood flow was slowed, and embolus clearance decreased, which can cause re-occlusion[1]. Repeated operations also caused surgery-related complications; thus, the number of mechanical thrombectomies was generally ≤ 3 times[23]. A total of 25 patients were investigated in this study. According to their previous medical history and clinical characteristics, the "micro-catheter first pass effect" proposed by Yi et al[24], preliminarily determined that the responsible vascular disease was acute occlusion based on atherosclerotic stenosis. After opening the Solitaire AB stent, the forward flow was maintained at mTICI level 2b/3 or above, and the operation was successful in all 25 patients. The average recanalization time was 23 min. The operation time was short, the operation relatively simple, and the complications related to the operation were significantly reduced. There were significant differences in NIHSS scores immediately (7.5 ± 5.6), at 24 h (5.5 ± 5.6) and at 1 wk (3.6 ± 6.7) after surgery compared with the preoperative NIHSS score (15.9 ± 4.4) (P < 0.01), and one patient died of cerebral hemorrhage and cerebral hernia after surgery. The patients were followed up for 3 mo after the operation and restenosis occurred in 1 case (stenosis rate 50% without clinical symptoms). The mRS score was 0 points in 14 cases (56%), 1 point in 4 cases (16%), 2 points in 2 cases (8%), 3 points in 3 cases (12%), 4 points in 1 case (4%), and 6 points in 1 case (4%). Figure 2 and 3 both show DSA of the patients undergoing surgery and CTA images of reexamination 3 d and 3 mo after surgery. The stents were in good shape and the distal vessels were unobstructed. Duan et al[25] reported that 44 cases of complicated intracranial atherosclerotic stenosis were treated by balloon angioplasty and Solitaire AB stent implantation in the non-acute stage. The technical success rate was 100%, and the residual stenosis rate after stent implantation was 0%-40% (average 15% ± 12.94%), the incidence of 30-d surgery-related complications was 9.09%, the average follow-up was 25.5 mo, and the recurrence rate of ischemic events at related sites was 4.55%. Therefore, it is believed that balloon angioplasty and implantation of Solitaire AB stents for the treatment of complex intracranial artery atherosclerotic stenosis is safe, effective, and has a high technical success rate, relatively few perioperative complications, and good follow-up prognosis[25]. The Solitaire AB stent has been permanently implanted to restore distal flow after failure of mechanical thrombectomy, and a number of studies have shown that the Solitaire AB stent may be a safer device for intracranial stenosis[26-28]. A recent study by Chang et al[29] retrospectively analyzed 591 patients with acute anterior circulation and great vessel occlusion. Among them, 148 patients who failed mechanical thrombus removal and recanalization were grouped and analyzed according to whether or not stents were implanted. The results showed that the stent implantation rate was 64.6%. Patients with failed thrombus removal were recanalized, and the clinical prognosis after recanalization was similar to that of mechanical thrombectomy, suggesting that rescue stent placement was safe and effective after thrombectomy failure. Stent implantation as the preferred treatment for acute ischemic stroke with large vessel occlusion remains controversial[30]. The major problem facing intravascular opening is how to achieve recanalization in the shortest time and avoid iatrogenic injury[31].
For patients with acute anterior circulation large vessel occlusion caused by intracranial aortic atherosclerosis stenosis, the Solitaire AB stent was unfolded and the anterior blood flow was maintained at mTICI level 2b/3 to release the stent, which can avoid repeated mechanical thrombus removal causing pulling back damage to the vascular intima[32] and repeated mechanical pulling back leads to re-occlusion of the blood vessel. Also, the time for salvage stent placement is shortened. The operation was relatively simple, the operation time was short, and the damage to the blood vessel was small. The operation cost was relatively low, creating favorable conditions for obtaining a good prognosis, and it was a clinically beneficial technique. Due to the relatively small number of cases, a larger sample size is still needed to confirm these findings, and the restenosis and long-term effects after stent release require further investigation.
In conclusion, Solitaire AB stent-release angioplasty may be safe and effective in the treatment of acute middle cerebral artery atherosclerotic occlusive cerebral infarction.
In recent years, the application of various intravascular thrombectomy devices has led to the rapid development of intravascular therapy, the Solitaire AB is a recyclable stent and its efficacy has been confirmed in several large clinical trials. Stent thrombectomy in the treatment of aortic occlusion was rapidly recommended as the standard treatment for acute great artery occlusion by domestic and international guidelines. However, the etiology of acute aortic occlusive cerebral infarction is complex, and at present, there is relatively little research on different treatment strategies for different etiologies and pathogenesis.
Aimed at the characteristics of intracranial atherosclerotic occlusion as the main pathogenesis of acute cerebral infarction in domestic patients, targeted treatment is required.
To analyze the safety and efficacy of Solitaire AB stent-release angioplasty in patients with acute middle cerebral artery atherosclerosis obliterative cerebral infarction.
To observe the effect of Solitaire AB stent release in 25 patients with acute middle cerebral artery atherosclerotic cerebral infarction enrolled in a retrospective study.
The operation was successful in all 25 patients, the mean recanalization time was 23 min, the National Institutes of Health Stroke Scale scores decreased significantly at different time points after surgery, and the proportion of patients with a 3 mo modified Rankin scale score ≤ 2 was 80%.
For patients with acute anterior circulation occlusion caused by intracranial aortic artery atherosclerosis, after Solitaire AB stent opening if the forward flow can maintain the level of modified thrombolysis in cerebral infarction 2b/3, stent release may be safe and effective.
From the perspective of clinical practice, according to the main causes of acute aortic occlusion in China, targeted treatment methods should be adopted.
Manuscript source: Unsolicited manuscript
Specialty type: Clinical neurology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Haneder S S-Editor: Zhang H L-Editor: Webster JR P-Editor: Zhang YL
| 1. | Huo XC, Gao F. Chinese Guidelines for Endovascular Treatment of Acute Ischemic Stroke 2018. Zhongguo Cuzhong Zazhi. 2018;7:707-725. |
| 2. | Campbell BC, Hill MD, Rubiera M, Menon BK, Demchuk A, Donnan GA, Roy D, Thornton J, Dorado L, Bonafe A, Levy EI, Diener HC, Hernández-Pérez M, Pereira VM, Blasco J, Quesada H, Rempel J, Jahan R, Davis SM, Stouch BC, Mitchell PJ, Jovin TG, Saver JL, Goyal M. Safety and Efficacy of Solitaire Stent Thrombectomy: Individual Patient Data Meta-Analysis of Randomized Trials. Stroke. 2016;47:798-806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 189] [Cited by in RCA: 184] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 3. | Sun B, Shi Z, Pu J, Yang S, Wang H, Yang D, Hao Y, Lin M, Ke W, Liu W, Guo F, Bai Y, Zhang S, Li Z, Li S, Zuo M, Xu G, Zi W, Liu X. Effects of mechanical thrombectomy for acute stroke patients with etiology of large artery atherosclerosis. J Neurol Sci. 2019;396:178-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Sanoussi S, Comet C, Kaefer K, Attou R, De Bels D, Gazagnes MD, Honoré PM, Redant S. Can Magnetic Resonance Imaging make the Differential Diagnosis between Cerebral Ischemia and Epilepsy? J Transl Int Med. 2019;7:123-125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Ma N. Chinese expert consensus on antiplatelet strategies for interventional treatment of ischemic cerebrovascular disease. Zhonghua Yixue Zazhi. 2015;95:803-809. |
| 6. | Ding D. Endovascular Mechanical Thrombectomy for Acute Ischemic Stroke: A New Standard of Care. J Stroke. 2015;17:123-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Mulder MJ, van Oostenbrugge RJ, Dippel DW; MR CLEAN Investigators. Letter by Mulder et al Regarding Article, "2015 AHA/ASA Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association". Stroke. 2015;46:e235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Gao F, Xu AD. Chinese guidelines for endovascular treatment of acute ischemic stroke2015. Zhongguo Cuzhong Zazhi. 2015;10:590-606. |
| 9. | Stampfl S, Hartmann M, Ringleb PA, Haehnel S, Bendszus M, Rohde S. Stent placement for flow restoration in acute ischemic stroke: a single-center experience with the Solitaire stent system. AJNR Am J Neuroradiol. 2011;32:1245-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; ESCAPE Trial Investigators. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4180] [Cited by in RCA: 4542] [Article Influence: 454.2] [Reference Citation Analysis (0)] |
| 11. | Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3948] [Cited by in RCA: 4280] [Article Influence: 428.0] [Reference Citation Analysis (0)] |
| 12. | Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W, Jansen O, Jovin TG, Mattle HP, Nogueira RG, Siddiqui AH, Yavagal DR, Baxter BW, Devlin TG, Lopes DK, Reddy VK, du Mesnil de Rochemont R, Singer OC, Jahan R; SWIFT PRIME Investigators. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372:2285-2295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3555] [Cited by in RCA: 3841] [Article Influence: 384.1] [Reference Citation Analysis (0)] |
| 13. | Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Román L, Serena J, Abilleira S, Ribó M, Millán M, Urra X, Cardona P, López-Cancio E, Tomasello A, Castaño C, Blasco J, Aja L, Dorado L, Quesada H, Rubiera M, Hernandez-Pérez M, Goyal M, Demchuk AM, von Kummer R, Gallofré M, Dávalos A; REVASCAT Trial Investigators. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296-2306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3402] [Cited by in RCA: 3686] [Article Influence: 368.6] [Reference Citation Analysis (0)] |
| 14. | Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, Wang Y, Zou X, Leung TW, Cai Y, Bai Q, Wu Y, Wang C, Pan X, Luo B, Wong KS; CICAS Study Group. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014;45:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 320] [Cited by in RCA: 540] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 15. | Levy EI, Siddiqui AH, Crumlish A, Snyder KV, Hauck EF, Fiorella DJ, Hopkins LN, Mocco J. First Food and Drug Administration-approved prospective trial of primary intracranial stenting for acute stroke: SARIS (stent-assisted recanalization in acute ischemic stroke). Stroke. 2009;40:3552-3556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 148] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 16. | Zaidat OO, Wolfe T, Hussain SI, Lynch JR, Gupta R, Delap J, Torbey MT, Fitzsimmons BF. Interventional acute ischemic stroke therapy with intracranial self-expanding stent. Stroke. 2008;39:2392-2395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 17. | Baek JH, Kim BM, Kim DJ, Heo JH, Nam HS, Yoo J. Stenting as a Rescue Treatment After Failure of Mechanical Thrombectomy for Anterior Circulation Large Artery Occlusion. Stroke. 2016;47:2360-2363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 97] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 18. | Liu H, Zhong HL, Jia JW, Li Y, Sun YQ. Application of Solitaire stent in the treatment of intracranial atherosclerotic stenosis. Zhonghua Jieru Fangshexue Dianzi Zazhi. 2015;3:115-118. |
| 19. | Kinariwala JP, Rajah GB, Luqman AW. Retained Solitaire FR device after mechanical thrombectomy: Case review and management strategies. Brain Circ. 2018;4:185-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Yoo AJ, Simonsen CZ, Prabhakaran S, Chaudhry ZA, Issa MA, Fugate JE, Linfante I, Liebeskind DS, Khatri P, Jovin TG, Kallmes DF, Dabus G, Zaidat OO; Cerebral Angiographic Revascularization Grading Collaborators. Refining angiographic biomarkers of revascularization: improving outcome prediction after intra-arterial therapy. Stroke. 2013;44:2509-2512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 168] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 21. | Marks MP, Lansberg MG, Mlynash M, Kemp S, McTaggart R, Zaharchuk G, Bammer R, Albers GW; DEFUSE 2 Investigators. Correlation of AOL recanalization, TIMI reperfusion and TICI reperfusion with infarct growth and clinical outcome. J Neurointerv Surg. 2014;6:724-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 22. | Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, Saleme S, Costalat V, Bracard S, Desal H, Mazighi M, Consoli A, Piotin M; ASTER Trial Investigators. Effect of Endovascular Contact Aspiration vs Stent Retriever on Revascularization in Patients With Acute Ischemic Stroke and Large Vessel Occlusion: The ASTER Randomized Clinical Trial. JAMA. 2017;318:443-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 553] [Cited by in RCA: 578] [Article Influence: 72.3] [Reference Citation Analysis (0)] |
| 23. | Flottmann F, Leischner H, Broocks G, Nawabi J, Bernhardt M, Faizy TD, Deb-Chatterji M, Thomalla G, Fiehler J, Brekenfeld C. Recanalization Rate per Retrieval Attempt in Mechanical Thrombectomy for Acute Ischemic Stroke. Stroke. 2018;49:2523-2525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 24. | Yi TY, Chen WH, Wu YM, Zhang MF, Zhan AL, Chen YH, Wu ZZ, Shi YC, Chen BL. Microcatheter "First-Pass Effect" Predicts Acute Intracranial Artery Atherosclerotic Disease-Related Occlusion. Neurosurgery. 2019;84:1296-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 25. | Duan G, Feng Z, Zhang L, Zhang P, Chen L, Hong B, Xu Y, Zhao W, Liu J, Huang Q. Solitaire stents for the treatment of complex symptomatic intracranial stenosis after antithrombotic failure: safety and efficacy evaluation. J Neurointerv Surg. 2016;8:680-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Ahmed SU, Mann J, Houde J, Barber E, Kelly ME, Peeling L. Permanent implantation of the Solitaire device as a bailout technique for large vessel intracranial occlusions. J Neurointerv Surg. 2019;11:133-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Li DD, Huang H, Fang JH, Fu FW, Lin J, Bai GH, Xu SY, Sheng HS, Zhou Q, Zhang N, Yin B. Solitaire Stent Permanent Implantation as an Effective Rescue Treatment for Emergency Large Artery Occlusion. World Neurosurg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Nappini S, Limbucci N, Leone G, Rosi A, Renieri L, Consoli A, Laiso A, Valente I, Rosella F, Rosati R, Mangiafico S. Bail-out intracranial stenting with Solitaire AB device after unsuccessful thrombectomy in acute ischemic stroke of anterior circulation. J Neuroradiol. 2019;46:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Chang Y, Kim BM, Bang OY, Baek JH, Heo JH, Nam HS, Kim YD, Yoo J, Kim DJ, Jeon P, Baik SK, Suh SH, Lee KY, Kwak HS, Roh HG, Lee YJ, Kim SH, Ryu CW, Ihn YK, Kim B, Jeon HJ, Kim JW, Byun JS, Suh S, Park JJ, Lee WJ, Roh J, Shin BS, Kim JM. Rescue Stenting for Failed Mechanical Thrombectomy in Acute Ischemic Stroke: A Multicenter Experience. Stroke. 2018;49:958-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 123] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 30. | Wang ZD, Liu XL, Cui QK, Zhang M, Lin K, Hao JC, Liu C, Zhang LY. A case of application in difficult thrombectomy of acute great vessel occlusion Balloon dilation technique before release of the Solitaire FR stent. Zhonghua Jieru Fangshexue Dianzi Zazhi. 2019;7:294-299. |
| 31. | Kim BM. Causes and Solutions of Endovascular Treatment Failure. J Stroke. 2017;19:131-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 32. | Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4460] [Cited by in RCA: 4868] [Article Influence: 486.8] [Reference Citation Analysis (0)] |