Published online May 16, 2021. doi: 10.12998/wjcc.v9.i14.3478
Peer-review started: December 30, 2020
First decision: January 24, 2021
Revised: February 2, 2021
Accepted: March 3, 2021
Article in press: March 3, 2021
Published online: May 16, 2021
Processing time: 119 Days and 20 Hours
Paget’s disease of bone (PDB) is a rare metabolic bone disease in China and is characterized by increased bone resorption and disorganized bone formation. The main clinical symptoms of PDB are focal or multiple bone pain and deformity with high disability. The disease has high missed diagnosis and misdiagnosis rates. This report summarizes the clinical manifestations, imaging and pathological features, and treatments of 11 patients with PDB at our hospital from 1993 to 2020 in order to improve the recognition and prognosis of PDB.
There were eight male and three female patients whose average age was 48.7 ± 11.0 years with a PDB course of 1-16 years. Nine patients had bone pain and bone deformities in different parts of the body, the majority of which involved the long bones. Laboratory examinations revealed elevated serum alkaline phosphatase (ALP) in all patients with an average of 618 ± 460 IU/L (normal range 0-130 IU/L), and serum calcium and phosphorus levels were in the normal range. Imageology showed that osteolysis was usually combined with osteosclerosis and/or bone deformities in single or multiple bones. 99mTc-methylene dipho
Early diagnosis of the rare disease PDB can be made through elevated ALP levels and typical presentations on bone X-ray and from bone tissue biopsy.
Core Tip: Paget’s disease of bone (PDB) is a rare metabolic bone disease in China that has high missed diagnosis and misdiagnosis rates. We retrospectively summarize the clinical data of 11 patients with a diagnosis of PDB to provide additional clinical evidence for the disease. We found that PDB presented with a predisposition toward the older male population, and the main clinical symptoms were bone pain, deformity, and a high risk of disability. Early identification of PDB can be made through elevated alkaline phosphatase levels and typical presentations on bone X-ray and from bone tissue biopsy. Bisphosphonates are the first choice to improve the symptoms and prognosis.
- Citation: Miao XY, Wang XL, Lyu ZH, Ba JM, Pei Y, Dou JT, Gu WJ, Du J, Guo QH, Chen K, Mu YM. Paget’s disease of bone: Report of 11 cases. World J Clin Cases 2021; 9(14): 3478-3486
- URL: https://www.wjgnet.com/2307-8960/full/v9/i14/3478.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i14.3478
Paget’s disease of bone (PDB), also known as osteitis deformans, was first discovered by the British surgeon James Paget in 1876[1]. PDB is a metabolic bone disease that presents with hyperactive bone remodeling and high-speed trabecular osteolysis leading to decreased bone quality and mechanical strength[2]. The chronic bone damage caused by PDB can be monostotic or polyostotic, and almost any bone can be affected, but the pelvis, spine, femur, tibia, skull, humerus, and scapula are involved more frequently. The common clinical manifestations are an abnormal bone structure, such as localized bone hypertrophy, and osteoporosis, leading to bone pain, bone deformity, and fracture. Significant regional and ethnic differences are observed in PDB patients. The prevalence of PDB is lower in Asian countries than in Western countries[3]. Due to its diverse clinical presentations and rarity in China, patients with PDB are often admitted to different departments and are prone to missed diagnosis or misdiagnosis; therefore, we retrospectively summarize the clinical data of 11 patients with a diagnosis of PDB from 1993 to 2020 at our hospital to provide more clinical evidence for the disease.
Eleven patients (eight males and three females) with a diagnosis of PDB were enrolled. The average age was 48.7 ± 11.0 years, and the disease duration was 1-16 years. The chief complaints of the patients are shown in Table 1. Nine of the eleven patients had bone pain, and seven of the eleven had bone deformities. Two patients were admitted to the hospital because of a painless bony mass in the jaw.
| Sex | Age (yr) | Chief complaints | X-ray findings | Bone scintigraphy findings | Surgery | Pathology findings | ALP (IU/L) | |
| 1 | Male | 34 | Painless mass on right mandible | An area of high-density bone sclerosis was seen on the right mandible measuring 2.5 cm × 2.5 cm × 2 cm | NA | Mandibular mass resection | Abnormal bone hyperplasia accompanied by fibrous hyperplasia | 400 |
| 2 | Male | 46 | Right hip joint pain and outward deformity of the right lower limb | Low density in the right femoral head was observed, with sparse patchy cystic areas. The articular surface was fuzzy with a narrowed joint space | NA | Lesion removal from the right hip joint | Mosaic appearance in bone trabeculae resulting from irregular cement lines | 505 |
| 3 | Male | 60 | Systematic bone pain with right humerus fracture | The diploic structure of the cranial bones was unclear. Bilateral femoral shafts were enlarged and deformed, with periosteal hyperplasia and ossification; the marrow cavity was irregular, and patchy, low-density areas were observed in cortical bone | Symmetrical, increased radionuclide uptake in the skull, bilateral ribs, clavicles, humeri, tibiae and femurs | NA | NA | 1671 |
| 4 | Male | 65 | Bone pain and deformity of the left lower limb | The middle part of the left femur was bent, the bone cortex was thickened, and there were patches of low-density areas in the bone marrow cavity | NA | NA | NA | 277 |
| 5 | Female | 48 | Left lower limb pain for 16 yr, with deformity for 14 yr | The cortex of the left femur was thickened, with the marrow cavity narrowed, and a sabre-like deformation was detected in the left femur | NA | NA | NA | 248 |
| 6 | Male | 47 | Constant pain in the right hip | Multiple cystic, low-density areas in the right ilium, ischia, and pubis | Abnormal, increased radionuclide uptake in the skull, spine and pelvis | CT-guided percutaneous biopsy of the right iliac bone | Obvious proliferation of localized matrix fibers in the bone paratrabecular area, with osteoclasts and osteoblasts aggregated | 457 |
| 7 | Female | 66 | Lumbar and lower limb pain with kyphosis | The pelvic bones and bilateral upper femur had multiple radiolucent spaces, with uneven bone density | Systemic osteolytic changes | Percutaneous biopsy of the left upper femur | Irregular trabeculae and hyperplasia of bone fibrous connective tissue | 817 |
| 8 | Male | 42 | Pain, deformity and limited mobility in the left knee | Diffuse bone lesions in the left femur, tibia, and fibula with thickened bone cortex and uneven density in the marrow cavity were observed | Diffuse, increased radionuclide uptake in the skull, left scapula, right fifth anterior rib, and right hemipelvis and limb bones | NA | NA | 1212 |
| 9 | Male | 39 | Pain and deformity of the left calf | The anterior arch of the left tibia was deformed and demonstrated disordered bone | NA | Percutaneous biopsy of the left tibia | Hyperplastic and disordered lamellar bone tissue of the left tibia and irregular broad trabeculae with fibrous vascular tissue | 203 |
| 10 | Male | 37 | Left hip pain for 16 yr, with claudication for 1 yr | Multiple uneven density bone lesions were observed in the middle and upper right humeri, left femur, and pelvis, showing multiple cystic radiolucent spaces, a thickened bone cortex, a narrowed marrow cavity, and a sabre-like deformation of the femur | Increased radionuclide uptake in the 11 thoracic vertebrae, pelvis, right humerus, and left femur | NA | NA | 312 |
| 11 | Female | 52 | Right maxillary mass | Expansion of the sphenoid bone, bilateral maxillae, cheekbones, temporal bones, and occipital bone was observed, and the diploic structure of the cranial bones was unclear | NA | Right maxillary mass resection | Mosaic appearance caused by randomly arranged cement lines and multinuclear osteoclasts | 699 |
The features of bone pain were constant and worsened at rest. Bone deformities included localized bone expansion and bending of the long bones during weight-bearing. Four patients had monostotic bone deformation, and seven patients had polyostotic bone deformation. The long bones (8/11) and hip (5/11) were the most affected bones. One patient (case 3) had a fracture of the right humerus. The 11 patients were admitted to departments of endocrinology, orthopedics, stomatology, and rheumatology separately. Before admission to our hospital, four patients (cases 5, 7, 9, and 10) were misdiagnosed with fibrous dysplasia of bone, bone metastases, bone tumours, and osteoarthritis, respectively. Patients 1 and 11 were admitted to the Department of Stomatology for jawbone lesions.
There was no history of essential hypertension, diabetes mellitus, or relevant cerebrovascular disease. The patients also had no history of confirmed malignant tumours.
Four patients had a smoking history. Family members of the patients did not have metabolic bone diseases or bone deformities.
Body temperature, blood pressure, respiratory rate, and heart rate were all in the normal range on admission. There were no other obvious symptoms except bone deformities (localized bone expansion and bending of long bones) and limited mobility of the hip or knee joints in seven of eleven patients.
Laboratory examinations revealed a significant increase in serum alkaline phosphatase (ALP) level, which was 618 ± 460 IU/L (normal range, 0-130 IU/L), while serum calcium 2.37 ± 0.16 mmol/L (2.09-2.54 mmol/L) and phosphorus 1.17 ± 0.21 mmol/L (0.89-1.60 mmol/L) were in the normal range.
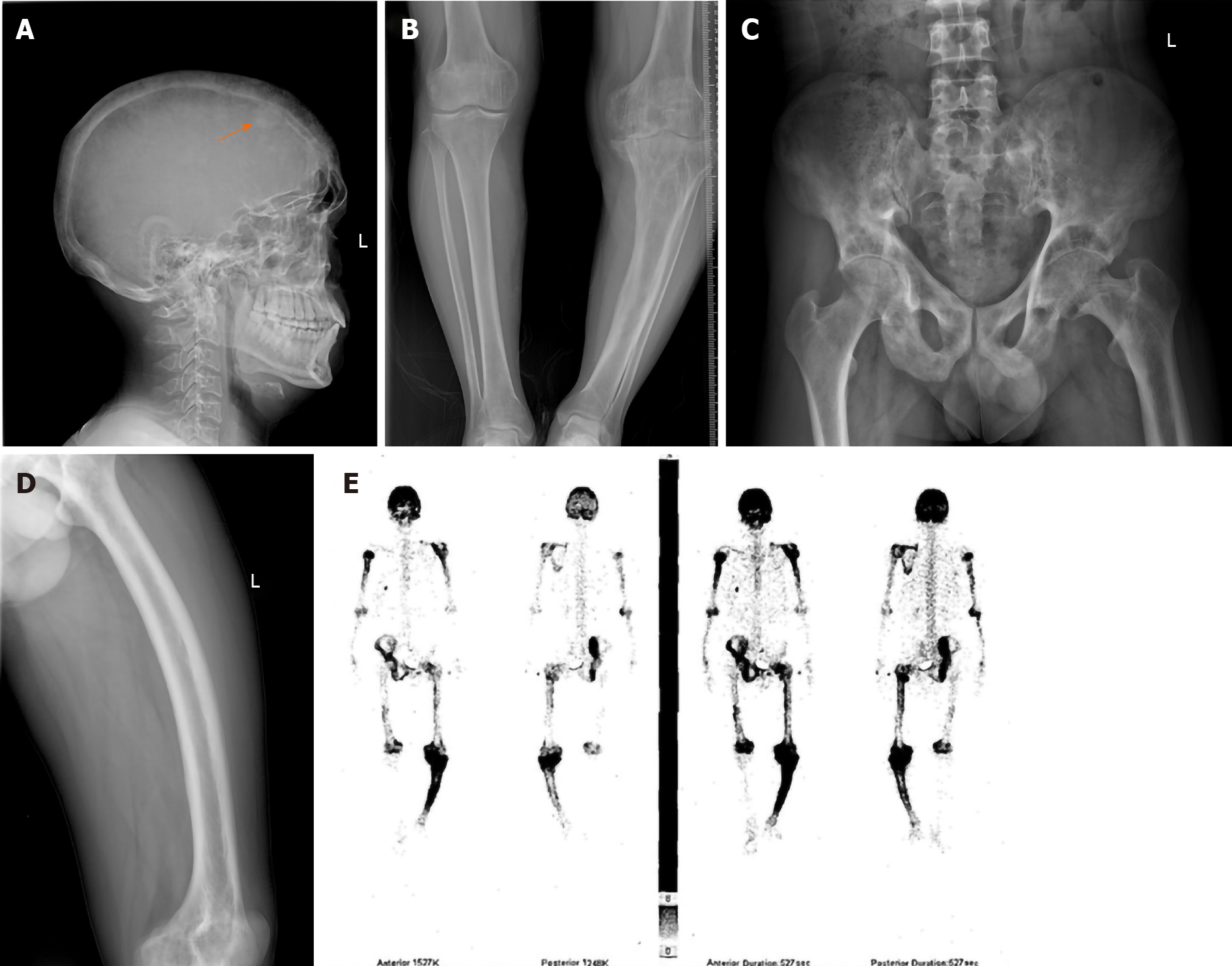
The X-ray examination showed bone resorption, destruction, and sclerosis at different levels and ranges, characterized by an uneven bone density, cystic, light-transmitting areas and bone expansion and deformities (Figure 1A-D); 99mTc-methylene dipho
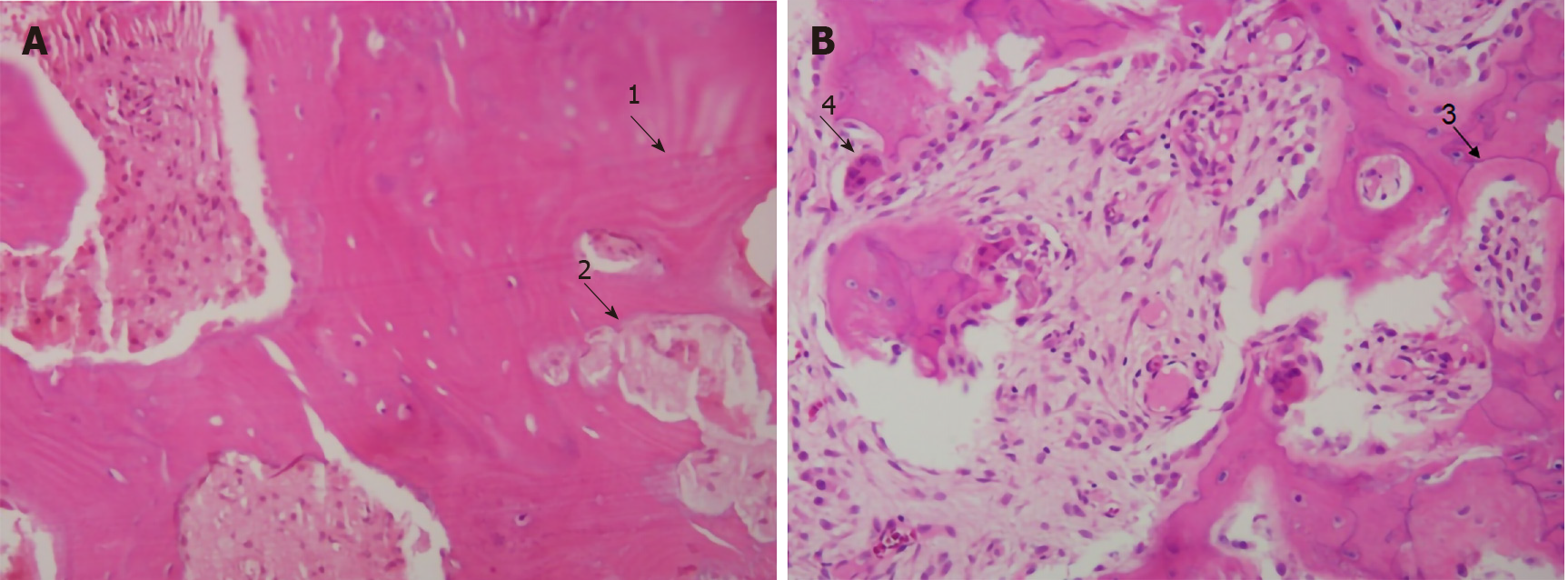
The diagnosis of PDB was based on the findings from bone biopsy or postoperative pathology. Pathological changes included the formation of irregular, broad bone trabeculae and fibrous vascular tissue, a mosaic structure of the bone trabeculae with irregular cement lines and multinuclear osteoclasts (Figure 2).
In the absence of pathology, the diagnosis depended on clinical manifestations, including bone pain, bone deformity and/or pathological fractures, X-rays (localized or multiple-bone osteolysis and sclerosis accompanied by bone deformity or fracture), 99mTc-MDP bone scan imaging (multiple abnormal radionuclide concentrations), and a significantly elevated serum ALP level[4].
Two patients were treated with three cycles of 200 mg etidronate sodium twice a day orally for 2 wk and withdrawal for 11 wk; two patients were treated with 10 mg alendronate once a day orally for 7 mo; three patients were treated with an intravenous injection of 15 mg pamidronate bisphosphonate every week for 7 wk; and three patients were treated with an intravenous injection of 5 mg zoledronate per year for 2 or 3 years (Table 2). Calcium (600 mg elemental calcium) and vitamin D (vitamin D 1000 IU/d or calcitriol 0.25 μg/d) were administered simultaneously. Cases 1, 2, and 11 underwent bone lesion surgery.
| Medical treatment | Follow-up | Symptoms | ALP (posttreatment IU/L) | |
| 1 | NA | 1 yr | No symptom | NA |
| 2 | Three cycles of etidronate sodium 200 mg administered twice a day orally for 2 wk and withdrawn for 11 wk | 10 yr | Bone pain relieved; mobility of the affected limb improved after surgery | 311 |
| 3 | Pamidronate bisphosphonate 15 mg/week intravenous injection for 7 wk | 3 mo | Bone pain relieved | 1398 |
| 4 | Three cycles of etidronate sodium 200 mg administered twice a day orally for 2 wk and withdrawn for 11 wk | 19 yr | Bone pain relieved | 212 |
| 5 | Alendronate 10 mg once a day orally for 7 mo | 15 yr | Bone pain relieved | 158 |
| 6 | Pamidronate bisphosphonate 15 mg/week intravenous injection for 7 wk | 3 yr | Bone pain relieved | 245 |
| 7 | Alendronate 10 mg once a day orally for 7 mo | 3 yr | Bone pain relieved | 752 |
| 8 | Zoledronate 5 mg per year intravenous injection for 3 yr | 5 yr | Bone pain relieved | 977 |
| 9 | Zoledronate 5 mg per year intravenous injection for 3 yr | 3 yr | Bone pain relieved | 60 |
| 10 | Zoledronate 5 mg per year intravenous injection for 2 yr | 2 yr | Bone pain relieved | 52 |
| 11 | Pamidronate bisphosphonate 15 mg/week intravenous injection for 7 wk | 1 yr | No symptom | 405 |
Bone pain was relieved after bisphosphonate treatment with good tolerance. The mobility of the affected limb for case 2 improved after surgery. Mean serum ALP level decreased significantly to 457 ± 445 IU/L (bP < 0.01). Serum calcium and phosphorus levels did not change significantly compared to the levels before treatment.
PDB is a chronic metabolic bone disease with a predisposition for older people, and more men than women tend to develop the disease. The disease is prone to missed diagnosis or misdiagnosis due to its diverse clinical manifestations and is usually asymptomatic during the early phase[5]. PDB is rare in China, and few reports have described it in individuals of Chinese ancestry. Clinicians should work to improve their recognition of PDB to reduce the disease course and disability. In this report, only 11 patients were diagnosed with PDB over 27 years at our hospital, including eight males and three females, with an average age of 48.7 ± 11.0 years. We summarize the clinical and pathological features of the cases to provide more evidence for the disease.
The etiology of PDB remains unclear, but some studies suggest that several genes involved in the differentiation or function of osteoclasts[6-9] and environmental factors, such as viral infection, particularly measles, animal contact, pesticides, and tobacco smoke, together play important roles in its pathogenesis[10]. Furthermore, rapidly increased bone resorption accompanied by abnormal new bone formation is a substantial PDB pathological characteristic. The number of enlarged and multinu
The clinical manifestations of PDB are nonspecific, and bone pain, the most common symptom, is constant and tends to worsen at night and upon weight bearing[12]. Other presentations include fractures, osteoarthritis, bone deformities, spinal canal stenosis, and paraplegia. The skull can be affected, which can lead to an enlarged head, and compression of nerves and brain tissues may cause headache and hearing loss[13]. The majority of patients in this report had bone pain and deformities, but none had headache or hearing loss. The bone lesions mainly involved the pelvis (5/11) and femur (7/11), followed by the spine, tibia, humerus, skull, ribs, clavicle, and scapula. Jawbones were affected in two cases.
The diagnosis of PDB is usually made by X-ray and elevated serum ALP levels, particularly in asymptomatic patients[14,15]. Common X-ray features include localized osteoporosis distributed along the trabecular bone in a wedge shape. A long bone absorption zone, such as in a “V”-shape, is typical during the early stage of the disease. Bone deformities, including bone cortex expansion, thickening, and deformation, are common. The edges of the cortical bone and trabecular bone in the lesion are rough and villi-like, and patchy frosted glass-like high-density foci are observed. Fractures follow this stage. In this study, the X-rays of case 8 revealed localized frosted glass-like high-density lesions in the skull (Figure 1A). The X-rays of case 10 showed multiple cystic translucent areas of the pelvis and deformation of the left femur into a “sabre shape” (Figure 1B and C). After PDB is visualized on X-ray, radionuclide bone scintigraphy is used to determine any additional lesions. The characteristic features on radionuclide bone scintigraphy are osteolysis during the initial stage, followed by osteogenesis and osteosclerosis. Marked increased radionuclide uptake can be seen during the osteolysis and osteogenesis stages of the disease, and low uptake is seen in sclerotic (“burned out”) lesions[16]. The bone scintigraphy of case 8 in this report showed increased radionuclide uptake in the skull, scapula, ribs, pelvis, and limbs (Figure 1D).
PDB is prone to misdiagnosis because of it various nonspecific clinical manifestations and rarity in China. Four patients in this report were misdiagnosed with fibrous dysplasia of bone, bone metastases, bone tumours, or osteoarthritis separately, and one was misdiagnosed with hyperparathyroidism on admission. PDB can be easily confused with bone tumours, bone metastases, fibrous dysplasia of bone, and hyperparathyroidism in clinical practice. Bone tumours (giant cell tumours, bone hemangiomas, or osteosarcomas) or bone metastases are similar to PDB[17,18], in which the most common symptom is bone pain. X-rays show osteolytic destruction, and bone scintigraphy shows increased radionuclide uptake with an elevated serum ALP level. However, the most common sites of involvement in patients with PDB are the pelvis and femur, which are characterized by broad trabeculae and thickened cortical bone on X-rays, whereas patients with bone tumours or bone metastases are often accompanied by systemic symptoms of consumption, such as fatigue and weight loss. Moreover, their blood ALP levels do not match those of patients with bone lesions. The osteolytic changes in PDB are prone to be confused with fibrous dysplasia of bone. The characteristic X-ray features of patients with fibrous dysplasia of bone are frosted glass-like, loofah-like, and cystic swelling changes and bone cortex thinning at lesion sites[19], with serum ALP levels in the normal range or slightly elevated but lower than those of patients with PDB. Histology of the affected bone is helpful in the diagnosis. Identifying PDB with hyperparathyroidism depends on medical history, calcium, phosphorus, and parathyroid hormone examinations as well as ultrasound of the parathyroid and bone X-rays[20].
The treatment for PDB is aimed at suppressing osteoclast activity and reducing bone turnover from a pathophysiological standpoint. Bisphosphonates suppress increased bone resorption and decrease serum ALP and are an ideal choice for treating PDB[21]. Multiple bisphosphonates have been approved by the United States Food and Drug Administration to treat PDB, among which zoledronic acid is most likely to relieve bone pain[4]. Studies have demonstrated that zoledronic acid is superior to other bisphosphonates for normalizing ALP levels and suppressing bone turnover markers[22]. In this report, all patients treated with a bisphosphonate responded, and their ALP levels decreased after short-term therapy. In addition, the clinical guidelines[23] suggest that total hip or knee replacement is recommended for PDB patients accompanied by osteoarthritis for whom medical treatment is refractory. The patient in case 2 underwent hip debridement surgery, and his limb activity improved.
Approximately 10% of patients with PDB develop malignant degeneration, primarily older men. Osteosarcoma is the most common malignant change, followed by fibrosarcoma and lymphosarcoma[24]. The main clinical symptoms of malignant PDB are an aggravation of constant pain, soft tissue swelling, and the occurrence of new lumps. Malignant degeneration is indicated by extended lesions, worm-eaten cortical bone destruction, and periosteal reactions. In this study, no malignant changes were detected, but long-term follow-up should be performed.
PDB is rare in China, but it is necessary to improve recognition of the disease with early diagnosis and treatment due to its high rate of disability. We report 11 PDB patients and summarize their clinical manifestations, laboratory and imaging examinations, pathological bone lesion characteristics, and main treatment methods, which may provide more evidence for the early identification of PDB.
We thank Li B at the Department of Pathology, The First Medical Center, Chinese PLA General Hospital for pathological data collection.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ma L S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Ralston SH. Clinical practice. Paget's disease of bone. N Engl J Med. 2013;368:644-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 103] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Hsu E. Paget's disease of bone: updates for clinicians. Curr Opin Endocrinol Diabetes Obes. 2019;26:329-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Griz L, Fontan D, Mesquita P, Lazaretti-Castro M, Borba VZ, Borges JL, Fontenele T, Maia J, Bandeira F; Brazilian Society of Endocrinology and Metabolism. Diagnosis and management of Paget's disease of bone. Arq Bras Endocrinol Metabol. 2014;58:587-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Ralston SH, Corral-Gudino L, Cooper C, Francis RM, Fraser WD, Gennari L, Guañabens N, Javaid MK, Layfield R, O'Neill TW, Russell RGG, Stone MD, Simpson K, Wilkinson D, Wills R, Zillikens MC, Tuck SP. Diagnosis and Management of Paget's Disease of Bone in Adults: A Clinical Guideline. J Bone Miner Res. 2019;34:579-604. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 102] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 5. | Malik AR, Lone NA, Rather HA, Jan VM, Malik JA, Khan KA, Jalal S. Asymptomatic Paget's disease of bone presenting with complete atrioventricular block. Chin Med J (Engl). 2008;121:2357-2359. [PubMed] |
| 6. | Gu JM, Zhang ZL, Zhang H, Hu WW, Wang C, Yue H, Ke YH, He JW, Hu YQ, Li M, Liu YJ, Fu WZ. Thirteen Chinese patients with sporadic Paget's disease of bone: clinical features, SQSTM1 mutation identification, and functional analysis. J Bone Miner Metab. 2012;30:525-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Goode A, Long JE, Shaw B, Ralston SH, Visconti MR, Gianfrancesco F, Esposito T, Gennari L, Merlotti D, Rendina D, Rea SL, Sultana M, Searle MS, Layfield R. Paget disease of bone-associated UBA domain mutations of SQSTM1 exert distinct effects on protein structure and function. Biochim Biophys Acta. 2014;1842:992-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Qi X, Pang Q, Wang J, Zhao Z, Wang O, Xu L, Mao J, Jiang Y, Li M, Xing X, Yu W, Asan, Xia W. Familial Early-Onset Paget's Disease of Bone Associated with a Novel hnRNPA2B1 Mutation. Calcif Tissue Int. 2017;101:159-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Guay-Bélanger S, Picard S, Gagnon E, Morissette J, Siris ES, Orcel P, Brown JP, Michou L. Detection of SQSTM1/P392L post-zygotic mutations in Paget's disease of bone. Hum Genet. 2015;134:53-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Numan MS, Jean S, Dessay M, Gagnon E, Amiable N, Brown JP, Michou L. Gene-environment interactions in Paget's disease of bone. Joint Bone Spine. 2019;86:373-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Zimmermann EA, Köhne T, Bale HA, Panganiban B, Gludovatz B, Zustin J, Hahn M, Amling M, Ritchie RO, Busse B. Modifications to nano- and microstructural quality and the effects on mechanical integrity in Paget's disease of bone. J Bone Miner Res. 2015;30:264-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 12. | Bolland MJ, Cundy T. Paget's disease of bone: clinical review and update. J Clin Pathol. 2013;66:924-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Wang QY, Fu SJ, Ding N, Liu SY, Chen R, Wen ZX, Fu S, Sheng ZF, Ou YN. Clinical features, diagnosis and treatment of Paget's disease of bone in mainland China: A systematic review. Rev Endocr Metab Disord. 2020;21:645-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Singer FR, Bone HG 3rd, Hosking DJ, Lyles KW, Murad MH, Reid IR, Siris ES; Endocrine Society. Paget's disease of bone: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2014;99:4408-4422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 15. | Bao CH, Zhang ZL. Diagnosis and treatment for 8 cases with Paget disease. Shanghai Yiyao. 2012;35:530-533. |
| 16. | Wang XL, Yang G, Lu JM, Dou JT, Mu YM, Meng JH, Pan CY, Shi HY. Clinical analysis of 7 patients with Paget’s disease of bone. Zhonghua Neifenmi Daixie Zazhi. 2008;24:412-414. |
| 17. | Du HQ, Zheng Y, Zhang M, He XF, Liu LY, Zhang ZL. Paget’s disease of bone misdiagnosed as hemangioma: report of one case. Zhonghua Neifenmi Daixie Zazhi. 2015;31:176-178. [DOI] [Full Text] |
| 18. | Gezer NS, Balcı A, Özdoğan Ö, Özaksoy D. Paget's Disease Mimicking Bone Metastasis in a Patient with Neuroendocrine Tumor on 68Ga-DOTANOC PET/CT. J Belg Soc Radiol. 2016;100:66. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Lu CZ, Xiao WJ, Zhang ZL. The value of bone scintigraphy in diagnosis of fibrous dysplasia of bone. Zhonghua Guzhishusong He Gukuangyanjibing Zazhi. 2011;4:82-86. |
| 20. | Xu B, Yu J, Lu Y, Han B. Primary hyperparathyroidism presenting as a brown tumor in the mandible: a case report. BMC Endocr Disord. 2020;20:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Gennari L, Rendina D, Falchetti A, Merlotti D. Paget's Disease of Bone. Calcif Tissue Int. 2019;104:483-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 22. | Devogelaer JP, Geusens P, Daci E, Gielen E, Denhaerynck K, Macdonald K, Hermans C, Vancayzeele S, Abraham I, Boonen S. Remission over 3 years in patients with Paget disease of bone treated with a single intravenous infusion of 5 mg zoledronic acid. Calcif Tissue Int. 2014;94:311-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Paul Tuck S, Layfield R, Walker J, Mekkayil B, Francis R. Adult Paget's disease of bone: a review. Rheumatology (Oxford). 2017;56:2050-2059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 40] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Rendina D, De Filippo G, Ralston SH, Merlotti D, Gianfrancesco F, Esposito T, Muscariello R, Nuti R, Strazzullo P, Gennari L. Clinical characteristics and evolution of giant cell tumor occurring in Paget's disease of bone. J Bone Miner Res. 2015;30:257-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |