Published online Apr 26, 2021. doi: 10.12998/wjcc.v9.i12.2703
Peer-review started: November 14, 2020
First decision: December 28, 2020
Revised: January 1, 2021
Accepted: March 11, 2021
Article in press: March 11, 2021
Published online: April 26, 2021
Processing time: 151 Days and 23.8 Hours
A novel coronavirus disease 2019 (COVID-19) is a progressive viral disease that affected people around the world with widespread morbidity and mortality. Patients with COVID-19 infection typically had pulmonary manifestation but can also present with gastrointestinal, cardiac, or neurological system dysfunction. Chest imaging in patients with COVID-19 commonly show bilateral lung involvement with bilateral ground-glass opacity and consolidation. Mediastinal lymphadenopathy can be found due to infectious or non-infectious etiologies. It is commonly found to be associated with malignant diseases, sarcoidosis, and heart failure. Mediastinal lymph node enlargement is not a typical computer tomography of the chest finding of patients with COVID-19 infection. We summarized the literature which suggested or investigated the mediastinal lymph node enlargement in patients with COVID-19 infection. Further studies are needed to better characterize the importance of mediastinal lymphadenopathy in patients with COVID-19 infection.
Core Tip: This reviewed summarized the articles with mediastinal lymphadenopathy evaluation in the patients with a novel coronavirus disease 2019. The content will help understand more regarding current prevalence of mediastinal lymphadenopathy in this population.
- Citation: Taweesedt PT, Surani S. Mediastinal lymphadenopathy in COVID-19: A review of literature. World J Clin Cases 2021; 9(12): 2703-2710
- URL: https://www.wjgnet.com/2307-8960/full/v9/i12/2703.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i12.2703
A novel coronavirus disease 2019 (COVID-19) is a progressive viral disease caused by the severe acute respiratory syndrome coronavirus 2 which initially was reported as a severe flu-like illness related to seafood in wet animal wholesale market in Wuhan, Hubei province, China in December 2019[1]. In January 2020, severe acute respiratory syndrome coronavirus 2 was identified as the causative pathogen and in February 2020 COVID-19 was named by the World Health Organization[2]. Person-to-person transmission is the main route of COVID-19 transmission and it can occur even during the incubation period[3]. COVID-19 rapidly spreads worldwide reaching the pandemic level. COVID-19 has affected people around the world with widespread morbidity and mortality especially in the elderly population with co-morbidities[4]. COVID-19 has a mean incubation period of approximately 5 d[3]. Patients with COVID-19 infection typically had mild symptoms or even asymptomatic[5]. Thus, early diagnosis of COVID-19 infection is very crucial. For symptomatic cases, fever, dry cough, fatigue, and dyspnea are commonly reported. Pulmonary manifestation is frequently found and progresses rapidly but other organ dysfunction such as gastrointestinal, cardiac, or neurological system dysfunction can also present[6]. The high level of inflammatory markers, cytokines, and chemokines in the serum of patients with COVID-19 was reported. The reverse transcription-polymerase chain reaction is considered the gold standard of diagnosis for COVID-19 infection[7].
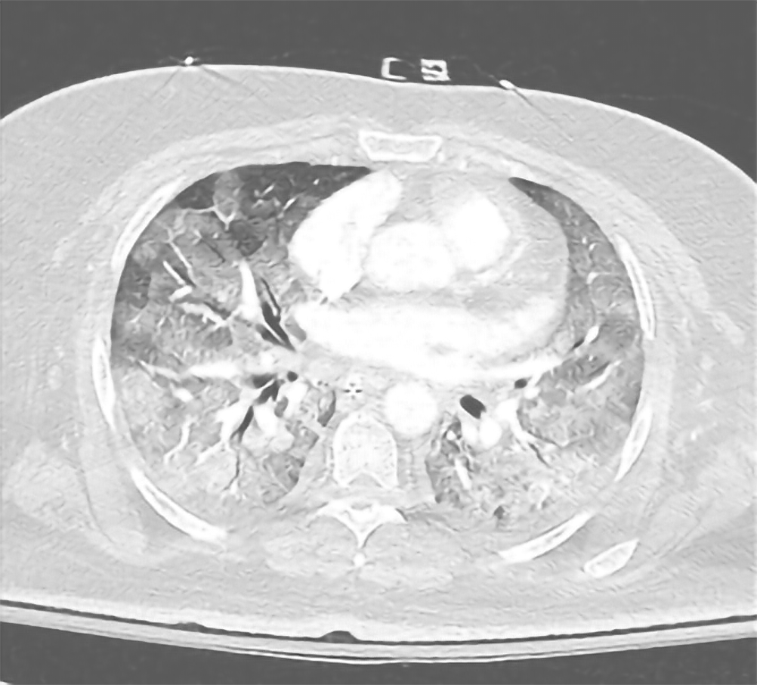
Imaging of the chest is an important diagnostic and follow-up tool for the pulmonary manifestation of COVID-19. Chest X-ray (CXR) is commonly used as it provides faster information than reverse transcription-polymerase chain reaction. However, the CXR finding can be normal in the early stage of COVID-19 infection[8-10]. CXR generally reveals pure ground glass, mixed ground-glass opacities-consolidation in bilateral peripheral and lower lungs zones[11]. Specificity and sensitivity of CXR for COVID-19 infection increased with time (sensitivity of 55% at ≤ 2 d increased to 79% at > 11 d) while specificity decreased with time (specificity of 83% decreased to 70%)[9]. The increase false negative of COVID-19 infection on CXR was found in young age and African-American ethnicity[9]. When compare to CXR, computer tomography (CT) of the chest in patients with COVID-19 showed higher sensitivity in detecting lung abnormality (CT chest 86.2% vs CXR 49.1%)[8] (Figure 1).
CT chest frequently showed bilateral lung involvement with bilateral multi-lobar ground-glass opacity (GGO) with peripheral or posterior distribution especially lower lobes and less commonly in the right middle lobe (Figure 2)[12]. Consolidation may be found on the presentation or superimposed on GGO, mainly in older age cases[3,4]. Less common findings were septal thickening, bronchiectasis, and pleural involvement[12]. Rare findings include lymphadenopathy, pleural effusion, cavitary lesion, and pneumothorax were reported.
The point-of-care ultrasonography performing bedside can also use to evaluate pulmonary pathology at the bedside without the necessity of transporting the patients. In a retrospective single-center study of a total of 22 patients with COVID-19 infection, diffuse B line patterns were found by ultrasonography in all cases[13]. Ultrasonography can also be used to monitor the disease response to prono-supination maneuvers in patients with COVID-19. However, it requires a longer operator-patient contact time than other imaging studies which may prevent it from being the imaging of choice. High definition transthoracic ultrasonography was used to evaluate mediastinal lymphadenopathy in sarcoidosis patients with sensitivity and specificity of 89% and 76%, respectively[14]. In COVID-19 cases, ultrasonography has not yet reported the finding of mediastinal lymphadenopathy.
Mediastinal lymph nodes are seen in the anterior, middle, and posterior mediastinal compartments of the thorax. Mediastinal lymph nodes receive its drainage from the thoracic viscera. Mediastinal lymphadenopathy was defined as mediastinal lymph nodes enlargement with a ≥ 10 mm in short axis[15]. The incidence of mediastinal lymphadenopathy was noted to be 1%-6%[16]. Mediastinal lymphadenopathy can be found due to due to malignant or benign etiologies such as inflammation or infection. Evison et al[17] reported that the size of hilar or mediastinal lymph node was the strongest predictor of etiology, with the size of 15 mm or less always reactive and the size of larger than 25 mm predict pathologic etiology. It is commonly found to be associated with malignant diseases, sarcoidosis, and heart failure[18]. Lymphoma is the most common cause of mediastinal lymphadenopathy. Unlike other lympha-denopathies, mediastinal lymphadenopathy is uncommonly caused by infection. Histoplasmosis, coccidioidomycosis, and tuberculosis were reported to cause mediastinal lymphadenopathy. Exposure history, endemic location along with patients’ symptoms and physical examination are helpful with the diagnosis. Mediastinal lymphadenopathy is commonly asymptomatic. However, it may contribute to pain, cough, wheezing, dysphagia, airway erosion leading to hemoptysis, obstruction of the airway leading to atelectasis, and the obstruction of the great vessels leading to superior vena cava syndrome. Mediastinal lymphadenopathy can be detected from chest X-ray, but a CT scan of the chest is usually performed as the next step to evaluate the lymph nodes as CT chest gives better delineation and characteristics of the lymph nodes such as calcification and necrosis.
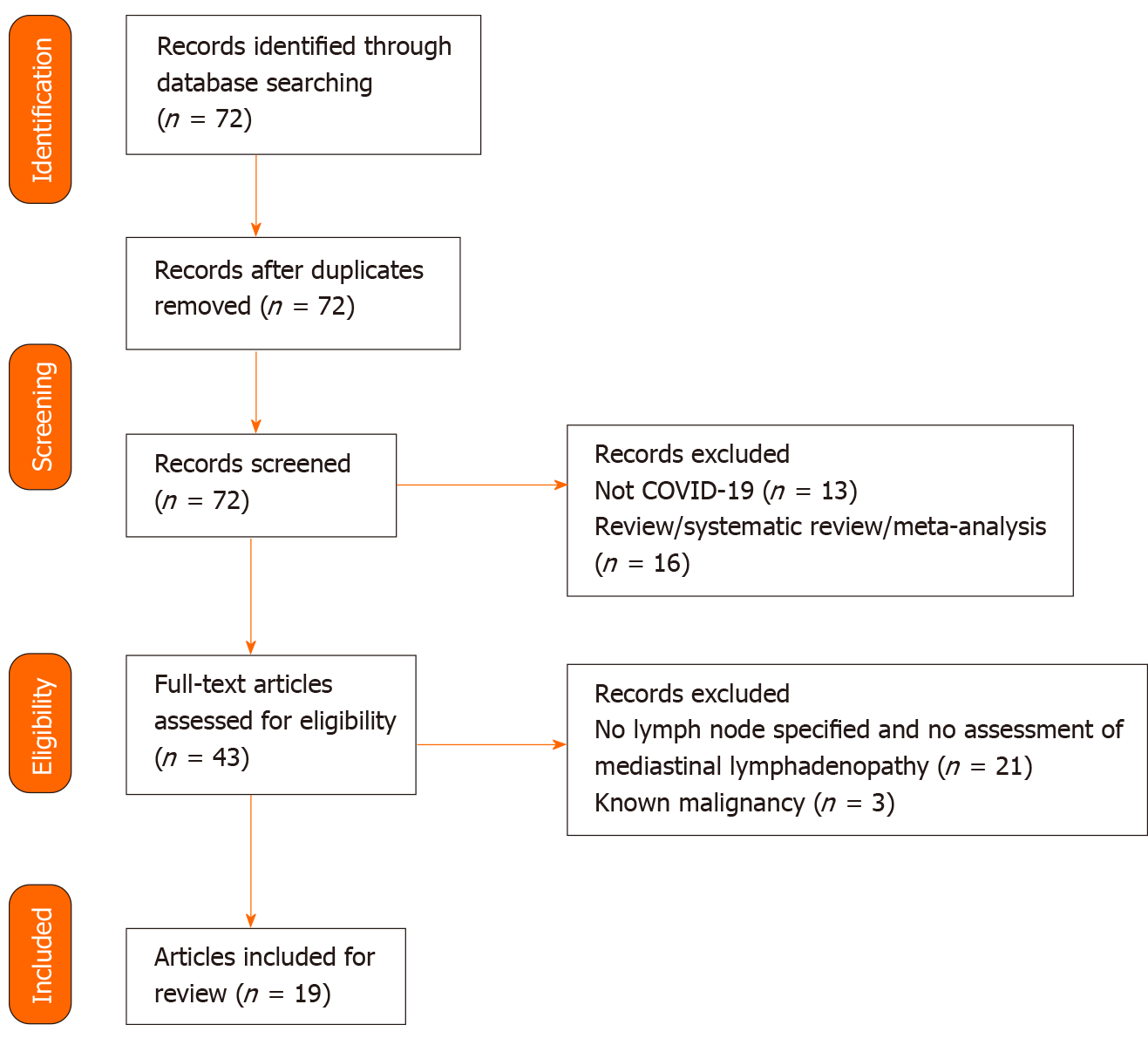
Mediastinal lymph node enlargement was not considered a typical CT chest finding of patients with COVID-19 infection. We summarized the literature which investigated mediastinal lymph node enlargement in patients with COVID-19 infection. Further studies are needed to better investigate the importance of mediastinal lympha-denopathy in patients with COVID-19 infection. We conducted a literature review of mediastinal lymphadenopathy evaluation in patients with COVID-19 infection from inception to November 2020 in PubMed (Figure 3). Keywords of "mediastinal lymphadenopathy" or "mediastinal lymph node” or "lymphadenopathy" and "COVID" or "coronavirus" were used. A total of 19 articles with a total of 1155 patients were included (Table 1).
| Ref. | Country | Type of article | n | Age (yr) | Male (%) | Findings | n (%) of ML |
| Valette et al[29] | France | R | 9 | NA | NA | GGO, reticulation, or consolidation (100%) | 6 (66) |
| Peng et al[20] | China | R | 201 | Median (range); 6 (3 h-15 yr) | 118 (58.7) | GGO (69.7%), consolidation (37%) | 0 (0) |
| Bayramoglu et al[21] | Turkey | R | 37 | Median (IQR); M 12.5 (8-15.5); F 15 (10-16) | 18 (48.6) | GGO with/without consolidation (45.9%) | 3 (8.1) |
| Grassi et al[24] | Italy | R | 134 | Mean (range); 69.3 (29-93) | 89 (71) | GGO and consolidation (71%), crazy-paving pattern (75%) | 69 (54.8) |
| Pakdemirli et al[30] | United Kingdom | R | 18 | mean (SD); 53.3 (NA) | 9 (50) | GGO (44%), pleural thickening (50%), focal vascular engorgement (83%), B/L lesion (100%) | 3 (17) |
| Li et al[31] | China | R | 19 | Mean (range); 63 (25-80) | 11 (57.9) | GGO (100%), consolidation (73.7%), interlobular septal thickening (63.2%) | 0 |
| Gong et al[22] | China | R | 10 | Mean (range); 30 (26-40) | 0 (0) | GGO (100%), B/L lesion (80%) | 0 |
| Sardanelli et al[25] | Italy | R | 410 | Median (IQR); 68 (57-78) | 288 (70) | NA | 76 (19) |
| Luo et al[32] | China | R | 70 | NA | NA | GGO (39%), GGO and consolidation (59%), B/L lesion (84%) | 2 (2.8) |
| Huang et al[33] | China | C | 7 | Median (range); 56 (49-64) | 3 (42.9) | GGO (100%) | 0 (0) |
| Guan et al[34] | China | R | 54 | mean (SD); 44.8 (16.7) | 25 (46) | GGO (100%), crazy-paving pattern (90%), B/L lesion (82%) | 0 (0) |
| Doroudinia et al[35] | Iran | C | 1 | 56 | 0 (0) | GGO both lungs | 0 (0) |
| Lu et al[36] | China | C | 9 | mean (SD); 7.8 (5.3) | 5 (55.6) | GGO (44.4%) | 0 (0) |
| Lei et al[37] | China | R | 14 | mean (SD); 47 (19) | 8 (57.1) | GGO (90%), irregular linear (90%), consolidation (90%) | 0 (0) |
| Himoto et al[38] | Japan | R | 6 | Median (range); 58.5 (45-81) | 5 (83.3) | B/L lesion (100%), GGO without consolidation (66.7%) | 0 (0) |
| Guan et al[39] | China | R | 53 | Mean (range); 42 (1-86) | 25 (47) | GGO (100%), crazy-paving pattern (89%), B/L lesion (79%) | 0 (0) |
| Zhao et al[23] | China | R | 80 | mean (SD); 44 (11.7) | 43 (54) | GGO (71%), B/L lesions (95%), subpleural lesion (90%) | 1 (1.3) |
| Albarello et al[19] | China | C | 2 | 66 and 67 | 1 (50%) | GGO and ML were found in both cases | NA |
| Chung et al[40] | China | R | 21 | mean (SD); 51(14) | 13 (62) | GGO (57%), multi-lobar lesion (71%), B/L lesion (76%) | 0 (0) |
Mediastinal lymphadenopathy was found in 0%-66% of the cases with COVID-19 infection. Subjects from a total of 8 articles (7 retrospective reviews and 1 case report) were noted to have mediastinal lymphadenopathy. In 4 case reports and 8 retrospective reviews with assessment of lymphadenopathy among patients with COVID-19, no mediastinal lymphadenopathy was found. In the case report of 2 cases by of elderly female and male 1/6/10R and 2R/4R/4L respectively on the both their first CT chest and their repeat CT chest after 6 d[19]. In a retrospective review of CT chest in pediatric patients with COVID-19, mediastinal lymphadenopathy was found in 0%-8.1% of the cases[20,21]. Mediastinal lymphadenopathy was not reported in pregnancy patients with COVID-19[22]. The mediastinal lymphadenopathy detected on high-resolution CT chest was 1.3% in a review of 80 patients with COVID-19[23]. In Italy, a review of 418 patients and a recent retrospective study of 134 patients with COVID-19 revealed a prevalence of mediastinal lymphadenopathy of 18.2% and 54.8% respectively[24,25]. No significant difference between patients with and without lymphadenopathy in terms of gender, age, cancer history, non-invasive ventilation, intensive care unit admission, length of hospital stay, laboratory results[25]. Lymphadenopathy was seen more in inpatient with a crazy-paving pattern on CT than those without and in those who died during hospitalization[25]. In China, 3 retrospective reviews of 154, 192, and 499 patients with COVID-19 revealed a prevalence of hilar/mediastinal lymphadenopathy of 43.5%, 41.7%, and 19.8% respectively[26-28]. Valette et al[29] reported that apart from a typical GGO, reticulation, or consolidation features found in all 9 patients with severe COVID-19 who were under invasive mechanical ventilation in intensive care unit in France, 6 patients were found to have mediastinal lymphadenopathy giving this finding the highest percentage of (66%) of mediastinal lymphadenopathy prevalence[29]. The onset of symptoms and CT findings had the median number of days of 7 (interquartile range 6-8). The subcarinal location of lymphadenopathy was noted in several patients up to 30 mm in the short axis.
The strength of this review is this is the first up-to-date review focusing on mediastinal lymphadenopathy in COVID-19. We used PubMed which is a reliable database. This review has limitations in that we used only published articles that are indexed in the PubMed database. Additionally, we have not reviewed the articles with COVID-19 imaging that may have the data of mediastinal lymph node without having our keywords.
Albeit rare in initial reports, mediastinal lymphadenopathy can be found in A novel COVID-19 infection especially in critically ill patients with COVID-19. Evaluating overall clinical condition is important to help with diagnosis, treatment, and prevention in this COVID-19 pandemic era.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: American College of Chest Physician.
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rahman MM S-Editor: Zhang L L-Editor: A P-Editor: Ma YJ
| 1. | Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Pneumonia of unknown aetiology in Wuhan, China: potential for international spread via commercial air travel. J Travel Med. 2020;27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 457] [Cited by in RCA: 421] [Article Influence: 84.2] [Reference Citation Analysis (0)] |
| 2. | World Health Organization. Director-General’s opening remarks at the media briefing on COVID-19. 11 March 2020. [cited November 1, 2020]. Available from: http://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. |
| 3. | Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11224] [Cited by in RCA: 9309] [Article Influence: 1861.8] [Reference Citation Analysis (0)] |
| 4. | Rossen LM, Branum AM, Ahmad FB, Sutton P, Anderson RN. Excess Deaths Associated with COVID-19, by Age and Race and Ethnicity - United States, January 26-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1522-1527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 273] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 5. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11409] [Cited by in RCA: 11490] [Article Influence: 2298.0] [Reference Citation Analysis (0)] |
| 6. | Behzad S, Aghaghazvini L, Radmard AR, Gholamrezanezhad A. Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clin Imaging. 2020;66:35-41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 178] [Article Influence: 35.6] [Reference Citation Analysis (0)] |
| 7. | Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470-473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4848] [Cited by in RCA: 4383] [Article Influence: 876.6] [Reference Citation Analysis (1)] |
| 8. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18848] [Article Influence: 3769.6] [Reference Citation Analysis (7)] |
| 9. | Stephanie S, Shum T, Cleveland H, Challa SR, Herring A, Jacobson FL, Hatabu H, Byrne SC, Shashi K, Araki T, Hernandez JA, White CS, Hossain R, Hunsaker AR, Hammer MM. Determinants of Chest X-Ray Sensitivity for COVID- 19: A Multi-Institutional Study in the United States. Radiol Cardiothorac Imag. 2020;2:e200337. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 10. | Fatima S, Ratnani I, Husain M, Surani S. Radiological Findings in Patients with COVID-19. Cureus. 2020;12:e7651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvarà S, Lucarini S, Busoni S, Mazzoni LN, Miele V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome. Radiol Med. 2020;125:730-737. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 155] [Cited by in RCA: 181] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 12. | Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients. AJR Am J Roentgenol. 2020;215:87-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 769] [Cited by in RCA: 858] [Article Influence: 171.6] [Reference Citation Analysis (0)] |
| 13. | Lomoro P, Verde F, Zerboni F, Simonetti I, Borghi C, Fachinetti C, Natalizi A, Martegani A. COVID-19 pneumonia manifestations at the admission on chest ultrasound, radiographs, and CT: single-center study and comprehensive radiologic literature review. Eur J Radiol Open. 2020;7:100231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 186] [Cited by in RCA: 179] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 14. | Hirche TO, Hirche H, Cui X-W, Wagner TO, Dietrich CF. Ultrasound evaluation of mediastinal lymphadenopathy in patients with sarcoidosis. Med Ultrason. 2014;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Munden RF, Carter BW, Chiles C, MacMahon H, Black WC, Ko JP, McAdams HP, Rossi SE, Leung AN, Boiselle PM, Kent MS, Brown K, Dyer DS, Hartman TE, Goodman EM, Naidich DP, Kazerooni EA, Berland LL, Pandharipande PV. Managing Incidental Findings on Thoracic CT: Mediastinal and Cardiovascular Findings. A White Paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2018;15:1087-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 16. | Jacobs PC, Mali WP, Grobbee DE, van der Graaf Y. Prevalence of incidental findings in computed tomographic screening of the chest: a systematic review. J Comput Assist Tomogr. 2008;32:214-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Evison M, Crosbie PA, Morris J, Martin J, Barber PV, Booton R. A study of patients with isolated mediastinal and hilar lymphadenopathy undergoing EBUS-TBNA. BMJ Open Respir Res. 2014;1:e000040. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Dabrowska M, Faber K, Tandejko-Burdyna M, Korczynski P, Krenke R. Etiology of mediastinal lymph node enlargement in patients who underwent EBUS-TBNA. Eur Respir J. 2019;54:PA3095. [DOI] [Full Text] |
| 19. | Albarello F, Pianura E, Di Stefano F, Cristofaro M, Petrone A, Marchioni L, Palazzolo C, Schininà V, Nicastri E, Petrosillo N, Campioni P, Eskild P, Zumla A, Ippolito G; COVID 19 INMI Study Group. 2019-novel Coronavirus severe adult respiratory distress syndrome in two cases in Italy: An uncommon radiological presentation. Int J Infect Dis. 2020;93:192-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 114] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 20. | Peng X, Guo Y, Xiao H, Xia W, Zhai A, Zhu B, Zhang W, Shao J. Overview of chest involvement at computed tomography in children with coronavirus disease 2019 (COVID-19). Pediatr Radiol. 2021;51:222-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Bayramoglu Z, Canıpek E, Comert RG, Gasimli N, Kaba O, Sarı Yanartaş M, Hançerli Torun S, Somer A, Erturk SM. Imaging Features of Pediatric COVID-19 on Chest Radiography and Chest CT: A Retrospective, Single-Center Study. Acad Radiol. 2021;28:18-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 22. | Gong X, Song L, Li H, Li L, Jin W, Yu K, Zhang X, Ke H, Lu Z. CT characteristics and diagnostic value of COVID-19 in pregnancy. PLoS One. 2020;15:e0235134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Zhao X, Liu B, Yu Y, Wang X, Du Y, Gu J, Wu X. The characteristics and clinical value of chest CT images of novel coronavirus pneumonia. Clin Radiol. 2020;75:335-340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 24. | Grassi R, Fusco R, Belfiore MP, Montanelli A, Patelli G, Urraro F, Petrillo A, Granata V, Sacco P, Mazzei MA, Feragalli B, Reginelli A, Cappabianca S. Coronavirus disease 2019 (COVID-19) in Italy: features on chest computed tomography using a structured report system. Sci Rep. 2020;10:17236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 25. | Sardanelli F, Cozzi A, Monfardini L, Bnà C, Foà RA, Spinazzola A, Tresoldi S, Cariati M, Secchi F, Schiaffino S. Association of mediastinal lymphadenopathy with COVID-19 prognosis. Lancet Infect Dis. 2020;20:1230-1231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Fang X, Li X, Bian Y, Ji X, Lu J. Relationship between clinical types and radiological subgroups defined by latent class analysis in 2019 novel coronavirus pneumonia caused by SARS-CoV-2. Eur Radiol. 2020;30:6139-6150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Fang X, Li X, Bian Y, Ji X, Lu J. Radiomics nomogram for the prediction of 2019 novel coronavirus pneumonia caused by SARS-CoV-2. Eur Radiol. 2020;30:6888-6901. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 28. | Li X, Fang X, Bian Y, Lu J. Comparison of chest CT findings between COVID-19 pneumonia and other types of viral pneumonia: a two-center retrospective study. Eur Radiol. 2020;30:5470-5478. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 29. | Valette X, du Cheyron D, Goursaud S. Mediastinal lymphadenopathy in patients with severe COVID-19. Lancet Infect Dis. 2020;20:1230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 30. | Pakdemirli E, Mandalia U, Monib S. Characteristics of Chest CT Images in Patients With COVID-19 Pneumonia in London, UK. Cureus. 2020;12:e10289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Li SK, Ng FH, Ma KF, Luk WH, Lee YC, Yung KS. Patterns of COVID-19 on computed tomography imaging. Hong Kong Med J. 2020;26:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Luo N, Zhang H, Zhou Y, Kong Z, Sun W, Huang N, Zhang A. Utility of chest CT in diagnosis of COVID-19 pneumonia. Diagn Interv Radiol. 2020;26:437-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 33. | Huang J, Ding J. Coronavirus Disease 2019: Initial High Resolution Computed Tomography Imaging Feature Analysis: Report of 7 Cases. Jpn J Infect Dis. 2020;73:459-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Guan CS, Wei LG, Xie RM, Lv ZB, Yan S, Zhang ZX, Chen BD. CT findings of COVID-19 in follow-up: comparison between progression and recovery. Diagn Interv Radiol. 2020;26:301-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Doroudinia A, Tavakoli M. A Case of Coronavirus Infection Incidentally Found on FDG PET/CT Scan. Clin Nucl Med. 2020;45:e303-e304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 36. | Lu Y, Wen H, Rong D, Zhou Z, Liu H. Clinical characteristics and radiological features of children infected with the 2019 novel coronavirus. Clin Radiol. 2020;75:520-525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 37. | Lei P, Huang Z, Liu G, Wang P, Song W, Mao J, Shen G, Zhou S, Qian W, Jiao J. Clinical and computed tomographic (CT) images characteristics in the patients with COVID-19 infection: What should radiologists need to know? J Xray Sci Technol. 2020;28:369-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 38. | Himoto Y, Sakata A, Kirita M, Hiroi T, Kobayashi KI, Kubo K, Kim H, Nishimoto A, Maeda C, Kawamura A, Komiya N, Umeoka S. Diagnostic performance of chest CT to differentiate COVID-19 pneumonia in non-high-epidemic area in Japan. Jpn J Radiol. 2020;38:400-406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 39. | Guan CS, Lv ZB, Yan S, Du YN, Chen H, Wei LG, Xie RM, Chen BD. Imaging Features of Coronavirus disease 2019 (COVID-19): Evaluation on Thin-Section CT. Acad Radiol. 2020;27:609-613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 121] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 40. | Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, Cui J, Xu W, Yang Y, Fayad ZA, Jacobi A, Li K, Li S, Shan H. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295:202-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1827] [Cited by in RCA: 1693] [Article Influence: 338.6] [Reference Citation Analysis (0)] |