Published online Apr 26, 2020. doi: 10.12998/wjcc.v8.i8.1538
Peer-review started: January 8, 2020
First decision: March 18, 2020
Revised: March 26, 2020
Accepted: April 10, 2020
Article in press: April 10, 2020
Published online: April 26, 2020
Processing time: 107 Days and 2.9 Hours
Congenital radioulnar synostosis (CRUS) is a rare deformity of the upper extremity. It is characterized by loss of rotation of the involved forearm and functional limitations in daily activities. No studies on CRUS with osteoporosis have been reported to date, and osteoporosis is usually recognized as an important dimension of genetic disorder in children. We discuss the possible relationship among this disorder, osteoporosis and fracture nonunion, investigate the strict surgical indications and recommended treatments.
A 14-year-old male patient with bilateral CRUS with osteoporosis, fragility fracture and nonunion of fractures in ulna and radius presented our institution for further treatment, complaining of limitation in rotation. The bone mineral density of the hip and lumbar spine was 0.687 g/cm2 and 0.705 g/cm2, respectively, and the Z-score for both was -2.1, which revealed osteoporosis and a high risk of fracture. Tow serum bone turnover markers indicated an imbalance of bone metabolism. Reoperation for ulna fracture with autogenous bone grafting and a postoperative physiotherapy program were adopted rather than the separation of pathological synostosis. Radiological examination, observational posture assessment and limb function scale were evaluated before and 1 year after surgery. At 1 year, the fracture nonunion had almost recovered, forearm movement function on the fracture side was restored, and function on the healthy side was significantly improved compared with that before rehabilitation.
Surgical indications for CRUS vary from person to person. Surgery should not be the first choice of treatment, and physiotherapy is not inferior to surgical treatment.
Core tip: Congenital radioulnar synostosis is a rare deformity of the upper extremity, which is characterized by loss of rotation and a variety of functional limitations. We present a rare case of bilateral congenital proximal radioulnar synostosis with osteoporosis, fragility fracture and nonunion. This case suggests that internal fixation plus bone grafting or stimulus of osteogenesis may result in a much better outcome than expected. In addition, this case highlights that surgery should not be the first choice except for those with severe daily activity limitations, and physiotherapy is not inferior to surgical treatment.
- Citation: Yang ZY, Ni JD, Long Z, Kuang LT, Tao SB. Unusual presentation of congenital radioulnar synostosis with osteoporosis, fragility fracture and nonunion: A case report and review of literature. World J Clin Cases 2020; 8(8): 1538-1546
- URL: https://www.wjgnet.com/2307-8960/full/v8/i8/1538.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i8.1538
Congenital radioulnar synostosis (CRUS), which is caused by fusion between the proximal end of the radius and ulna with the forearm fixed in some degrees of pronation, is a rare deformity of the upper extremity. It is common, however, in congenital elbow anomalies, and approximately 60%-80% of cases are bilateral[1-3]. It is characterized by loss of rotation of the involved forearm and a variety of functional limitations in daily activities in severe cases, presumably as a result of an insult in utero at the time when the proximal ends of the radius and ulna were connected by a common perichondrium[4,5]. The etiology has been reported to be genetic and multifactorial[1]. Pain or restriction of elbow flexion-extension movements is absent in most patients with CRUS; their forearm is usually fixed in the pronation, and the function of supination is lost to varying degrees[1,6]. In most cases, the evaluation of the malformation is based on the classification by Cleary and Omer[7,8]. It is classified into four radiographic types, as shown in Table 1[9].
| Type (proportion) | Description |
| I (19%) | Fibrous synostosis with a reduced normal-appearing radial head |
| II (8%) | Visible bony synostosis with a reduced radial head |
| III (56%) | Visible bony synostosis with a hypoplastic and posteriorly dislocated radial head |
| IV (17%) | Short bony synostosis with an anteriorly dislocated mushroom-shaped radial head |
No studies on CRUS with osteoporosis have been reported to date, but osteoporosis is usually recognized as an important dimension of genetic disorder in children. Childhood osteoporosis is typically divided into primary and secondary causes, with osteogenesis imperfecta (OI) representing the prototypical primary osteoporosis of childhood, predisposing to bone fragility and fracture[10-13]. Low-trauma non-vertebral fractures in children with osteoporosis are observed most frequently at the femur, tibia, forearm, humerus, feet and ankles[14-16].
We here report a 14-year-old male patient with bilateral CRUS with osteoporosis, fragility fracture and nonunion of fracture in ulna and radius. Informed consent was obtained from the patient and his guardians for using the data of this case to be submitted for publication.
A 14-year-old right-handed boy with CRUS of the bilateral forearm and a fragility fracture of both bones of the forearm in a fall presented to the Department of Orthopedics of our hospital.
In another hospital, open reduction and internal fixation were performed, while the ulna was fixed with a Kirschner wire, maintaining neutral forearm position in a plaster cast for 8 wk before rehabilitation was initiated. At 3 mo after surgery, since the location of the reduced ulna was lost and the fracture was nonunion, the patient came to our hospital and asked for further treatment.
The boy had two previous fractures, including one distal radius fracture and one tibiofibular fracture.
There was a possible hereditary history in his family, where his mother and younger brother had a similar elbow deformity.
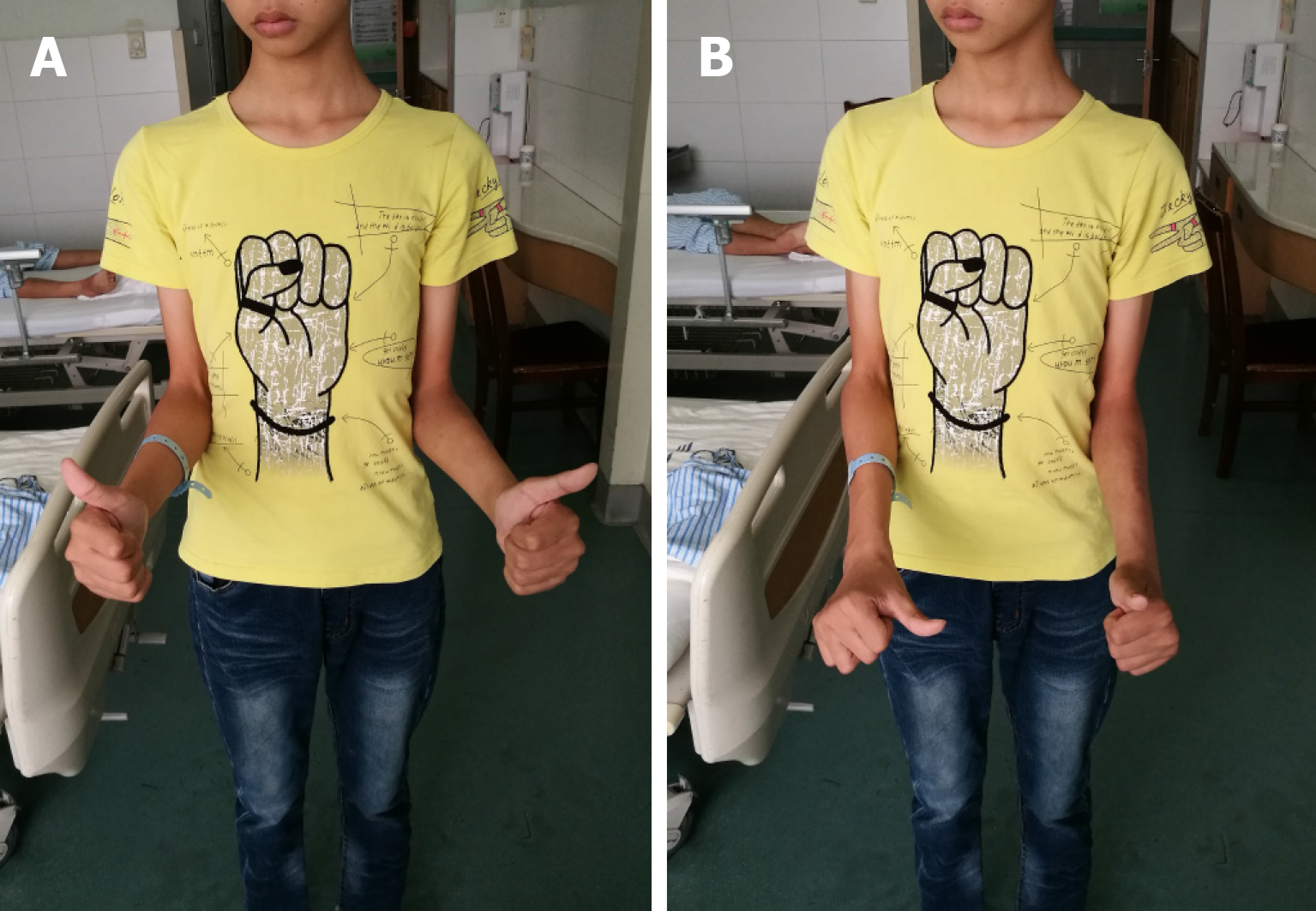
On physical examination, a hard but painless lump was found in the posterolateral region of the bilateral elbow, and it could not be reduced in flexion-extension or in pronation-supination. A deficiency in active motion was present at the left forearm (Figure 1). Right forearm function was slightly limited for the compensation of the ipsilateral shoulder, and the patient had no flexion and extension dysfunction on both sides of the forearm.
Bone mineral density (BMD) was measured by Dual Energy X-ray Absorptiometry. BMD of the hip and lumbar spine was 0.687 g/cm2 and 0.705 g/cm2, respectively, and the Z-score for both was -2.1. The 2013 International Society for Clinical Densitometry recommended a BMD Z-score threshold (−2.0 or worse) in children to denote childhood osteoporosis, provided such children also have a clinically significant fracture history, defined as ≥ 2 long bone fractures by age 10 and ≥ 3 long bone fractures by age 18[17]. According to the recommendation, the patient was identified as childhood osteoporosis with an increased fracture risk. Serum collagen type I cross-linked C-telopeptide (a marker of bone resorption) and serum procollagen I N-terminal propeptide (a marker of bone formation) of the patient were 1832 ng/mL and 347 ng/mL, respectively. These two bone turnover markers are recommended by the International Osteoporosis Foundation and the International Federation of Clinical Chemistry and Laboratory Medicine for the assessment of bone health[18].
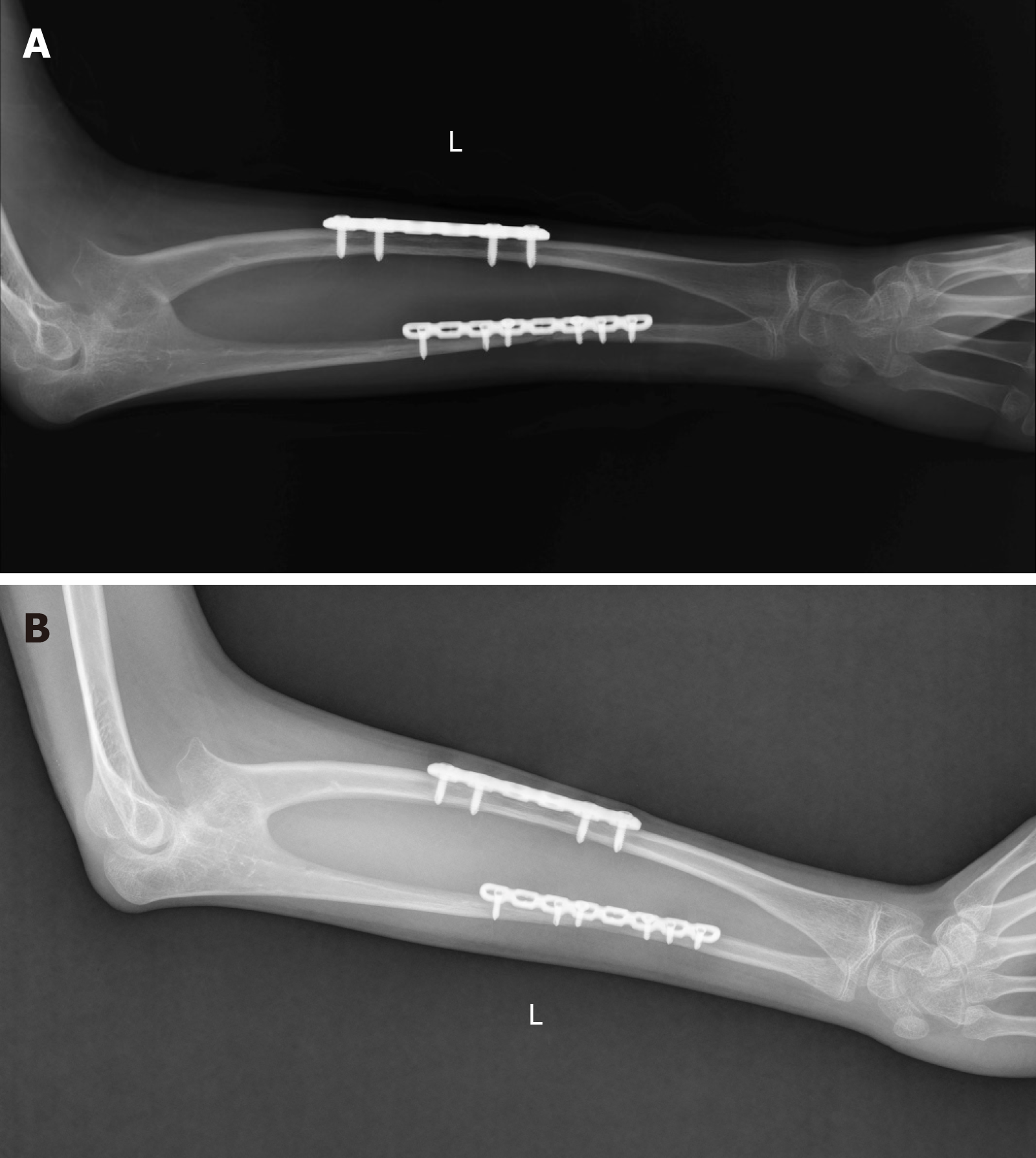
Plain radiography showed a fracture of both bones of the left forearm and pathologic fusions between the proximal diaphysis of radius and ulna, with a small bone diameter (Figure 2).
Bilateral CRUS with osteoporosis, fragility fracture and nonunion of fractures in ulna and radius.
Bilateral synostoses of this case were both classified as type II according to Cleary and Omer. Considering that the child’s forearm function of the dominant side was not significantly affected with the compensation of the ipsilateral limb and could ensure necessary living requirements, reoperation for ulna fracture with autogenous bone grafting and a postoperative physiotherapy program were adopted rather than the separation of pathological synostosis. Physiotherapy was performed by a professional rehabilitation physician, and all exercises were practiced bilaterally. These exercises consisted of actively stretching the muscle to the point of limitation of supination, followed by a passive supination movement, and then practicing compensatory movement of adjacent joints.
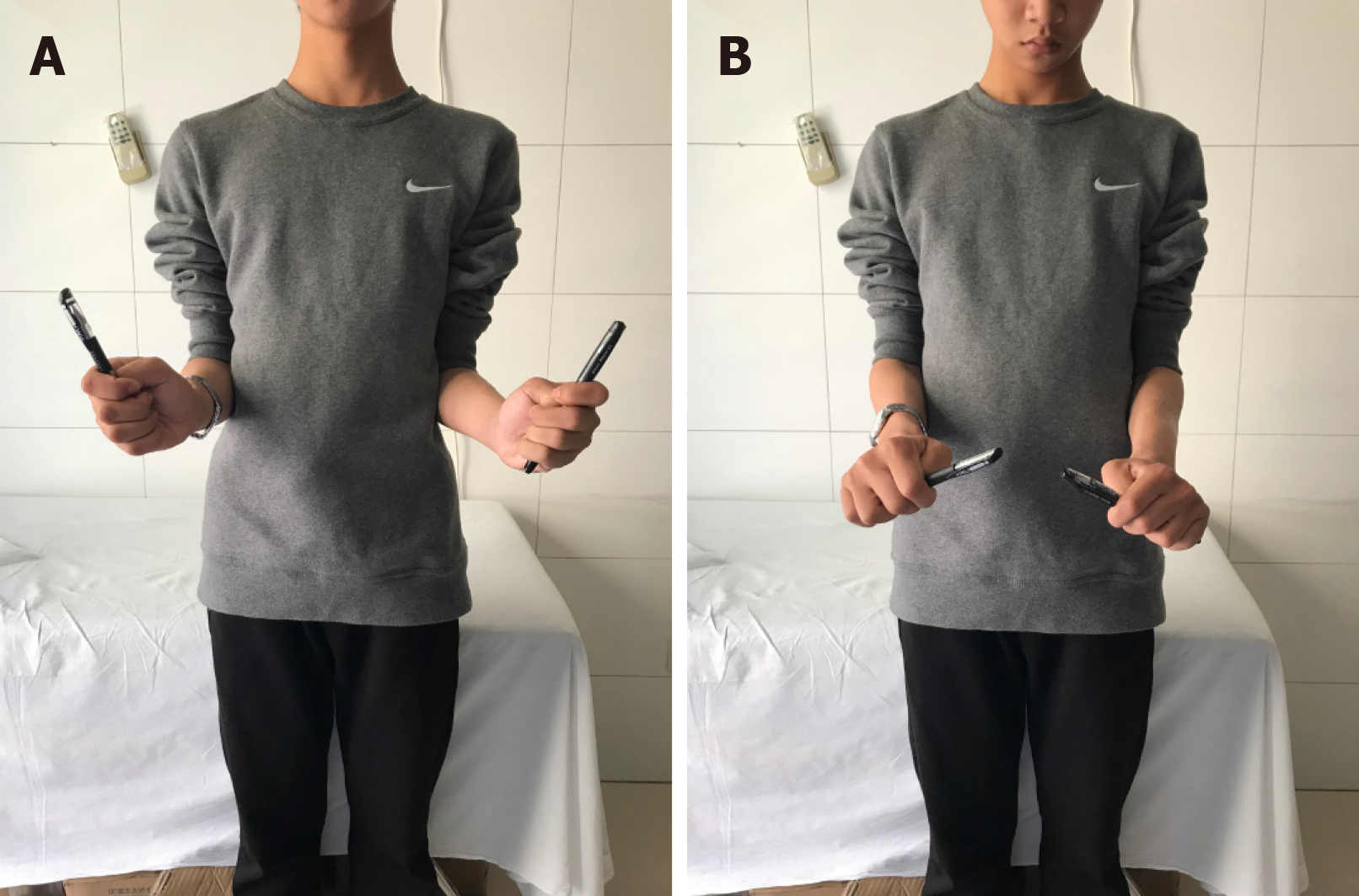
The patient was evaluated before and 1 year after surgery with radiological examination, observational posture assessment, the Activities of Daily Living Scale, the Liverpool Elbow Score, the Disabilities of the Arm, Shoulder, and Hand score and the Failla classification system. The Activities of Daily Living Scale was used to evaluate subjectively the degree of improvement in activities of daily living, including 11 that related to hygiene and self-care, eight that related to feeding, and seven that assessed environmental interaction on a 5-point scale. The Liverpool Elbow Score was first introduced in 2004 as an elbow-specific outcome score to be completed by both the clinicians and patients, combining a nine-item patient-answered questionnaire and a six-item clinical assessment score[19]. The Disabilities of the Arm, Shoulder, and Hand score is a 30-item questionnaire that quantifies physical function and symptoms in persons with any or multiple musculoskeletal disorders of the upper limb[20]. The Failla classification system is a grading system used by Failla et al[21] to evaluate the functional ranges of rotation of the forearm. The evaluation results are given in Table 2. One year later, the fracture had almost recovered (Figure 3), and the range of motion was significantly improved (Figure 4).
| Outcome assessment | Before surgery | At 1 yr after surgery | ||
| Nondominant, fractured side | Dominant, non-fractured side | Nondominant, fractured side | Dominant, non-fractured side | |
| ROM of elbow E/F (°) | 0/140 | 0/140 | 0/140 | 0/140 |
| ROM of forearm P/S (°) | 0/5 | -30/0 | -45/45 | -45/30 |
| ADL1 | ||||
| Hygiene and self-care items | 3.5 | 4.0 | 4.2 | 4.5 |
| Feeding-related items | 3.3 | 4.6 | 4.5 | 4.9 |
| Environmental interaction | 3.3 | 4.3 | 4.3 | 4.7 |
| Average | 3.4 | 4.3 | 4.3 | 4.7 |
| LES2 | ||||
| Clinical assessment | 12 | 15 | 17 | 17 |
| Patient-answered questions | 11 | 30 | 31 | 34 |
| Final scores | 4.4 | 8.2 | 8.7 | 9.2 |
| DASH3 | ||||
| Function | 48 | 32 | ||
| Symptoms | 14 | 7 | ||
| DASH value | 26.7 | 7.5 | ||
| Failla classification system | Fair | Good | Good | Excellent |
The forearm complex functions to rotate the hand in space and allow for a redistribution of forces during functional tasks. Disruptions of any one of the components can potentially lead to limitations in forearm rotation and function[22]. CRUS as a rare malformation is thought to be an anomaly of longitudinal segmentation that develops in the early fetal life. The elbow begins to appear at day 34-35 of fetal life, while the humerus, radial bone and ulna appear at day 37[7]. The humerus, radius and ulna are continuous with each other and are joined by a common perichondrium within the first 60 d of embryologic development. The cartilaginous anlage between these bones is separated by condensation, while the forearm is in a neutral position. Deformity of the radial head may be closely related to complete proximal union caused by early interference with joint formation[23] or unequal growth of the radius head caused by limited distal epiphyseal fusion[24].
CRUS is usually bilateral and subject to autosomal dominant inheritance[25]. Moreover, CRUS is one of many components of malformation syndromes in children with chromosomal aberrations[8,26]. A number of authors have claimed that there is a genetic basis for radioulnar synostosis. Evidence for this etiology, like in this case, includes familial occurrence and the close relation with other congenital syndromes such as acrocephalosyndactyly, microcephaly, Apert's syndrome, Carpenter's syndrome, arthrogryposis, Klinefelter syndrome, multiple exostoses, Holt-Oram syndrome, fetal alcohol syndrome, Ayme-Gripp syndrome, Saethre-Chotzen syndrome, mandibulofacial dysostosis with microcephaly and William's syndrome[2,27-30].
Because children can easily compensate for rotational limitations caused by joint deformities, the disease is usually not diagnosed early[31]. Although the pronation and supination movements of forearm are limited, elbow flexion and extension exercises are generally unaffected. Most patients with CRUS can manage daily activities through the overuse and compensation of shoulder and wrist[6,32]. Shoulder abduction compensates for inadequate pronation, and shoulder adduction compensates for inadequate supination[33].
Our patient had type II bilateral synostoses, according to the Cleary and Omer classification, and had an accessory bone in the proximal part of his bilateral forearm wedged between the radius and ulna. In addition, there was a fracture with slender long bones and thin cortex after a low-energy injury. Laboratory examination also revealed the presence of osteoporosis as compared with peers. The only available method to determine the pathogenesis with certainty is to measure directly bone formation and resorption on trabecular surfaces via transiliac bone biopsy. However, the patient refused this procedure because of the potential risks. We hypothesize that patients with CRUS may have OI or calcification disorder due to genetic defects. Therefore, for such patients with fractures, in addition to strong internal fixation, bone grafting or stimulation of osteogenesis may have more benefits than expected.
Many studies have examined different surgical methods for CRUS, such as derotational osteotomy of radial shaft, radial head excision and graft applications (see Table 3 for details). As CRUS is rare, it is difficult to conduct randomized-controlled trials, and there are generally only case reports or case series in the literature. Surgical techniques for treating radioulnar synostosis can be categorized into two groups: (1) Operations that improve pro-supination through synostosis resection, with or without interposition of biological or synthetic materials; and (2) Operations that improve the forearm’s fixed position[34]. Surgery is performed with the intention of restoring normal anatomical alignment, thus preserving normal forearm biomechanics. However, some studies have shown a high incidence of postoperative complications[35-37]. It is almost impossible to restore the complete rotation of the affected forearm, and although the initial results might be satisfactory, the range of motion would return to the preoperative status over time[37,38]. Satisfactory results were usually achieved in patients with very severe preoperative disability[31,39-42].
| Ref. | Post-op follow-up in mo | Surgical methods | Preoperative fixed forearm position (°)1 | Final forearm position (°)4 | Complications |
| Simcock et al[31], 2015 | 46 (range, 6-148) | Derotational osteotomy | 85 (range, 60-100) | -8 (range, -30-0) | 12% |
| VanHeest et al[35], 2013 | 33 (range, 24-42)2 | Radial head excision3 | 27.5 (range, 0-60) | Mainly improve elbow extension movement | 25% (one with transient radial nerve neuropraxia) |
| Shingade et al[46], 2014 | 54 (range, 36-84) | Radial osteotomy | 56.3 (range, 30-86) | 27.2 (range, 20-30) | Not available |
| Hung et al[39], 2008 | 64 (range, 30-129) | Derotational osteotomy | 78 (range, 65-85) | 8 (range, 0-30) | 0% |
| Bishay et al[40], 2016 | 30.4 (range, 24-36) | single-session double-level rotational osteotomy | 70.7 (range, 60-85) | -15.5 (range, -30-20) | 0% |
| Garg et al[36], 2015 | 32.1 (range, 16-65) | Radial head excision with a tensor fascia lata graft | 51.6 (range, 30-70) | 15 (range, 5-32) | 50% (superficial infection, posterior interosseous nerve palsy and a persistent extension lag) |
| Horii et al[41], 2014 | 60 (range, 12-156) | Derotational osteotomy | 72 (range, 40-100) | 0 | 0% |
| Pei et al[42], 2019 | 55.19 (range, 24-123) | Derotational osteotomy | 62.92 (55-80) | 7.94 (range, -10-20) | 9.7% (transient nerve palsies and compartment syndrome) |
| Satake et al[47], 2018 | 163.2 (range, 120-228) | Derotational osteotomy | 51.3 (range, 30-90) | 4 (range, -20-30) | 0% |
| Hwang et al[38], 2015 | 33 (range, 12-72) | Derotational osteotomy | 47 (range, 30-65) | 27 (range, 25-30) | 0% |
| Kanaya et al[37], 2016 | 120 (range, 96-144) | Radial osteotomy with a free vascularized adipofascial graft | 14.2 (range, 0-25) | 6.7 (range, 0-25) | 66.7% (flap congestion, transient radial nerve palsy, synovial fold and posterior or anterior radial head dislocation) |
Although an indication for operation in a patient with more than 60 degrees of fixed pronation was proposed, it must be individualized in patients with pronation between 15 and 60 degrees[43]. The patients with > 60 degrees of pronation usually have restrictions in daily activities[44]. Generally, the surgical protocol is dependent more on functional deficits than absolute forearm position. Studies have shown that physiotherapy is effective in the functional recovery of the upper extremities in patients with CRUS[45].
In the present case, forearm rotation function was compensated well through the adjusted movements of the adjacent joints, wrists and shoulders, and there was no obvious limitation in daily life. Therefore, we suggest that the choice of procedure should be individualized as not all the patients are eligible for surgery.
In summary, based on a review of all similar reported cases, we believe that patients with CRUS complicated with osteoporosis and fracture, due to the suspicious gene-induced OI or calcification disorder, may benefit not only from indispensable firm internal fixation but also bone grafting or stimulus of osteogenesis. In addition, surgical indications in such patients vary from person to person. Surgery should not be the first choice except for those with severe limitations in daily activities, and physiotherapy may be a new method of functional rehabilitation. However, these are just conjectures obtained from a common case, and more research is needed to confirm these predictions in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gheita T, Ünver B S-Editor: Dou Y L-Editor: Filipodia E-Editor: Wu YXJ
| 1. | Siemianowicz A, Wawrzynek W, Besler K. Congenital radioulnar synostosis - case report. Pol J Radiol. 2010;75:51-54. [PubMed] |
| 2. | Wurapa R. Radioulnar Synostosis. 2009. Available from: https://emedicine.medscape.com/article/1240467-overview-a6.html. |
| 3. | Lescault E, Mulligan J, Williams G. Congenital radioulnar synostosis in an active duty soldier: case report and literature review. Mil Med. 2000;165:425-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Shoham Y, Gurfinkel R, Sagi A. Idiopathic distal radioulnar synostosis. J Plast Surg Hand Surg. 2014;48:89-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Kasten P, Rettig O, Loew M, Wolf S, Raiss P. Three-dimensional motion analysis of compensatory movements in patients with radioulnar synostosis performing activities of daily living. J Orthop Sci. 2009;14:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Elliott AM, Kibria L, Reed MH. The developmental spectrum of proximal radioulnar synostosis. Skeletal Radiol. 2010;39:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Cho YG, Kim DS, Lee HS, Cho SC, Choi SI. A case of 49,XXXXX in which the extra X chromosomes were maternal in origin. J Clin Pathol. 2004;57:1004-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Cleary JE, Omer GE. Congenital proximal radio-ulnar synostosis. Natural history and functional assessment. J Bone Joint Surg Am. 1985;67:539-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 101] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Bachrach LK. Diagnosis and treatment of pediatric osteoporosis. Curr Opin Endocrinol Diabetes Obes. 2014;21:454-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Mäkitie O. Causes, mechanisms and management of paediatric osteoporosis. Nat Rev Rheumatol. 2013;9:465-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Saraff V, Schneider J, Colleselli V, Ruepp M, Rauchenzauner M, Neururer S, Geiger R, Högler W. Sex-, age-, and height-specific reference curves for the 6-min walk test in healthy children and adolescents. Eur J Pediatr. 2015;174:837-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Bianchi ML, Leonard MB, Bechtold S, Högler W, Mughal MZ, Schönau E, Sylvester FA, Vogiatzi M, van den Heuvel-Eibrink MM, Ward L; International Society for Clinical Densitometry. Bone health in children and adolescents with chronic diseases that may affect the skeleton: the 2013 ISCD Pediatric Official Positions. J Clin Densitom. 2014;17:281-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 14. | King WM, Ruttencutter R, Nagaraja HN, Matkovic V, Landoll J, Hoyle C, Mendell JR, Kissel JT. Orthopedic outcomes of long-term daily corticosteroid treatment in Duchenne muscular dystrophy. Neurology. 2007;68:1607-1613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 179] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 15. | Högler W, Wehl G, van Staa T, Meister B, Klein-Franke A, Kropshofer G. Incidence of skeletal complications during treatment of childhood acute lymphoblastic leukemia: comparison of fracture risk with the General Practice Research Database. Pediatr Blood Cancer. 2007;48:21-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | van Staa TP, Cooper C, Leufkens HG, Bishop N. Children and the risk of fractures caused by oral corticosteroids. J Bone Miner Res. 2003;18:913-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 151] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Bishop N, Arundel P, Clark E, Dimitri P, Farr J, Jones G, Makitie O, Munns CF, Shaw N; International Society of Clinical Densitometry. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2013 Pediatric Official Positions. J Clin Densitom. 2014;17:275-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 198] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 18. | Vasikaran S, Cooper C, Eastell R, Griesmacher A, Morris HA, Trenti T, Kanis JA. International Osteoporosis Foundation and International Federation of Clinical Chemistry and Laboratory Medicine position on bone marker standards in osteoporosis. Clin Chem Lab Med. 2011;49:1271-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 253] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 19. | Sathyamoorthy P, Kemp GJ, Rawal A, Rayner V, Frostick SP. Development and validation of an elbow score. Rheumatology (Oxford). 2004;43:1434-1440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 56] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 46] [Reference Citation Analysis (0)] |
| 21. | Failla JM, Amadio PC, Morrey BF. Post-traumatic proximal radio-ulnar synostosis. Results of surgical treatment. J Bone Joint Surg Am. 1989;71:1208-1213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 84] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 22. | LaStayo PC, Lee MJ. The forearm complex: anatomy, biomechanics and clinical considerations. J Hand Ther. 2006;19:137-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | García-Mata S, Hidalgo-Ovejero AM. Developmental anterior dislocation of the radial head resulting from a congenital solitary osteochondroma of the proximal ulna in an infant. Bull NYU Hosp Jt Dis. 2010;68:38-42. [PubMed] |
| 24. | Mital MA. Congenital radioulnar synostosis and congenital dislocation of the radial head. Orthop Clin North Am. 1976;7:375-383. [PubMed] |
| 25. | Rizzo R, Pavone V, Corsello G, Sorge G, Neri G, Opitz JM. Autosomal dominant and sporadic radio-ulnar synostosis. Am J Med Genet. 1997;68:127-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Burgemeister AL, Daumiller E, du Bois G, Graul-Neumann LM, Köhler B, Knecht S, Burgemeister S, Gronwald S, Maurer MH, Zirn B. Clinical report of 8 patients with 49,XXXXY syndrome: Delineation of the facial gestalt and depiction of the clinical spectrum. Eur J Med Genet. 2019;62:210-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Amudhavalli SM, Hanson R, Angle B, Bontempo K, Gripp KW. Further delineation of Aymé-Gripp syndrome and use of automated facial analysis tool. Am J Med Genet A. 2018;176:1648-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 28. | Gandomi SK, Parra M, Reeves D, Yap V, Gau CL. Array-CGH is an effective first-tier diagnostic test for EFTUD2-associated congenital mandibulofacial dysostosis with microcephaly. Clin Genet. 2015;87:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 29. | Germeshausen M, Ancliff P, Estrada J, Metzler M, Ponstingl E, Rütschle H, Schwabe D, Scott RH, Unal S, Wawer A, Zeller B, Ballmaier M. MECOM-associated syndrome: a heterogeneous inherited bone marrow failure syndrome with amegakaryocytic thrombocytopenia. Blood Adv. 2018;2:586-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 30. | Lord SV, Jimenez JE, Kroeger ZA, Patrick CS, Sanchez-Pena I, Ziga E, Bademci G, Tekin M. A MECOM variant in an African American child with radioulnar synostosis and thrombocytopenia. Clin Dysmorphol. 2018;27:9-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 31. | Simcock X, Shah AS, Waters PM, Bae DS. Safety and Efficacy of Derotational Osteotomy for Congenital Radioulnar Synostosis. J Pediatr Orthop. 2015;35:838-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 32. | Tuli S, Kelly M, Ryan K, Tuli S, Giordano BP. A 4-year-old child who could not supinate her forearm. J Pediatr Health Care. 2014;28:357-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Kozin SH. Congenital differences about the elbow. Hand Clin. 2009;25:277-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 34. | Barrera-Ochoa S, Campillo-Recio D, Mir-Bullo X. Treating bilateral congenital radioulnar synostosis using the reverse Sauvé-Kapandji procedure. J Hand Surg Eur Vol. 2019;44:430-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 35. | VanHeest AE, Lin TE, Bohn D. Treatment of blocked elbow flexion in congenital radioulnar synostosis with radial head excision: a case series. J Pediatr Orthop. 2013;33:540-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Garg G, Gupta SP. Surgical outcome of delayed presentation of congenital proximal radioulnar synostosis. SICOT J. 2015;1:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Kanaya K, Iba K, Yamashita T. Long-term results after a free vascularized adipofascial graft for congenital proximal radioulnar synostosis with an average follow-up of 10 years: a series of four cases. J Shoulder Elbow Surg. 2016;25:1258-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Hwang JH, Kim HW, Lee DH, Chung JH, Park H. One-stage rotational osteotomy for congenital radioulnar synostosis. J Hand Surg Eur Vol. 2015;40:855-861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Hung NN. Derotational osteotomy of the proximal radius and the distal ulna for congenital radioulnar synostosis. J Child Orthop. 2008;2:481-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 40. | Bishay SN. Minimally invasive single-session double-level rotational osteotomy of the forearm bones to correct fixed pronation deformity in congenital proximal radioulnar synostosis. J Child Orthop. 2016;10:295-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 41. | Horii E, Koh S, Hattori T, Otsuka J. Single osteotomy at the radial diaphysis for congenital radioulnar synostosis. J Hand Surg Am. 2014;39:1553-1557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 42. | Pei X, Han J. Efficacy and feasibility of proximal radioulnar derotational osteotomy and internal fixation for the treatment of congenital radioulnar synostosis. J Orthop Surg Res. 2019;14:81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 43. | Simmons BP, Southmayd WW, Riseborough EJ. Congenital radioulnar synostosis. J Hand Surg Am. 1983;8:829-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 75] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 44. | Ogino T, Hikino K. Congenital radio-ulnar synostosis: compensatory rotation around the wrist and rotation osteotomy. J Hand Surg Br. 1987;12:173-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 45. | Kepenek-Varol B, Hoşbay Z. Is short-term hand therapy effective in a child with congenital radioulnar synostosis? A case report. J Hand Ther. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 46. | Shingade VU, Shingade RV, Ughade SN. Results of single-staged rotational osteotomy in a child with congenital proximal radioulnar synostosis: subjective and objective evaluation. J Pediatr Orthop. 2014;34:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 47. | Satake H, Kanauchi Y, Kashiwa H, Ishigaki D, Takahara M, Takagi M. Long-term results after simple rotational osteotomy of the radius shaft for congenital radioulnar synostosis. J Shoulder Elbow Surg. 2018;27:1373-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |