Published online Dec 6, 2020. doi: 10.12998/wjcc.v8.i23.6181
Peer-review started: August 7, 2020
First decision: August 22, 2020
Revised: August 29, 2020
Accepted: September 25, 2020
Article in press: September 25, 2020
Published online: December 6, 2020
Processing time: 119 Days and 3.2 Hours
Coronavirus disease 2019 (COVID-19) severity is classified as asymptomatic, mild, moderate, severe, and critical. Mild cases account for a large percentage of cases in the epidemic and typically exhibit a favorable prognosis. However, a 49%-67% mortality is noted in critical cases. No COVID-19-specific drug has been reported to date, and symptomatic and optimal supportive care, including oxygenation, anti-coinfection treatments, and ventilation, represent the mainstay of treatment for this disease, especially in critical patients.
In the above-mentioned context, we share our experience with the treatment of one critical COVID-19 case and review the relevant literature.
Timely tracheal intubation, reasonable mechanical ventilation support, appropriate anti-infection treatment, and early anticoagulation and immunity support are key factors in the successful treatment of this case.
Core Tip: The mortality of severe coronavirus disease 2019 (COVID-19) patients is high, and no effective antiviral drugs are available now. Therefore, it is important to identify a suitable treatment strategy that is associated with improved prognosis of COVID-19, especially in critically ill patients. Here, we share our experience with the treatment of one critical COVID-19 case. We conclude that timely intubation, reasonable mechanical ventilation support, appropriate anti-infection treatment, early anticoagulation and immune support, and other comprehensive measures may help to reduce the course of disease and patient mortality.
- Citation: Pang QL, He WC, Li JX, Huang L. Symptomatic and optimal supportive care of critical COVID-19: A case report and literature review. World J Clin Cases 2020; 8(23): 6181-6189
- URL: https://www.wjgnet.com/2307-8960/full/v8/i23/6181.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i23.6181
In late December 2019, a novel coronavirus pneumonia (COVID-19) caused by a zoonotic coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan, China. The disease is currently spreading worldwide and triggering a great public health concern[1]. To control transmission, the basic reproduction rate (RO) should be less than one. However, the RO of SARS-CoV-2 is thought to be between 1.4-6.49, which is greater than that noted for SARS[2]. As of June 24, 2020, 9247908 confirmed cases and 477536 deaths have been reported worldwide.
According to the virulence-transmission trade-off hypothesis, such highly contagious pathogens are likely less virulent because killing the host too quickly does not benefit pathogen transmission among hosts. Indeed, a large proportion of patients present mild symptom or are asymptomatic. One study based on more than 72000 patients from China reported that 81% of cases exhibited mild presentation[3]. On the Diamond Princess Cruise ship, the estimated asymptomatic proportion was 17.9%[4]. However, it is important to note that the fatality rate is quite high if patients do not receive proper treatment and suitable organ support. In early stages of the outbreak, the mortality rate was 17% in China given the lack of experience of treatment of this disease[5]. In Wuhan, the mortality rate was 25% in the middle of the epidemic[6]. An increased fatality rate was seen in severe and critically ill patients; one large retrospective study from Italy showed that mortality reached 26% among patients admitted to the intensive care unit (ICU)[7]. In some locations, the mortality rate in critically ill patients could be as high as 49%-67%[6,8]. Given that no proven cure exists at this time, it is important to identify a suitable treatment strategy that is associated with improved prognosis of COVID-19, especially in critically ill patients. Here, we share our therapy experience with one critical case of COVID-19 to provide reference for clinical application.
On January 27, 2020, a 64-year-old Chinese woman of Han nationality was admitted to our hospital because of cough for 15 d. She had experienced fever, chest tightness, and shortness of breath for 5 d. She stayed in Wuhan for 12 d before she came back to Shenzhen on January 22.
Her past medical history was unremarkable.
Physical examination results on admission were as follows: Temperature, 37.5 ºC; blood pressure, 124/74 mmHg; SpO2, 91%; pulse, 85 times/min; respiration rate, 22 times/min. The respiratory sounds of both lungs were thick, and no obvious dry or wet rales were heard. Nothing special was identified upon physical examination.
Initial routine blood results were as follows: White blood cells, 5.3 × 109/L; neutrophil percentage, 78%; lymphocytes, 0.9 × 109/L. Blood gas analysis results were as follows: pH, 7.45; PO2, 82 mmHg; PCO2, 37 mmHg; FIO2, 40%. Liver and kidney function and myocardial enzyme values were normal. Inflammation indicators, C reactive protein (CRP, 52 mg/L), and interleukin 6 (IL-6, 153 pg/mL) were increased significantly, but the procalcitonin value was normal.
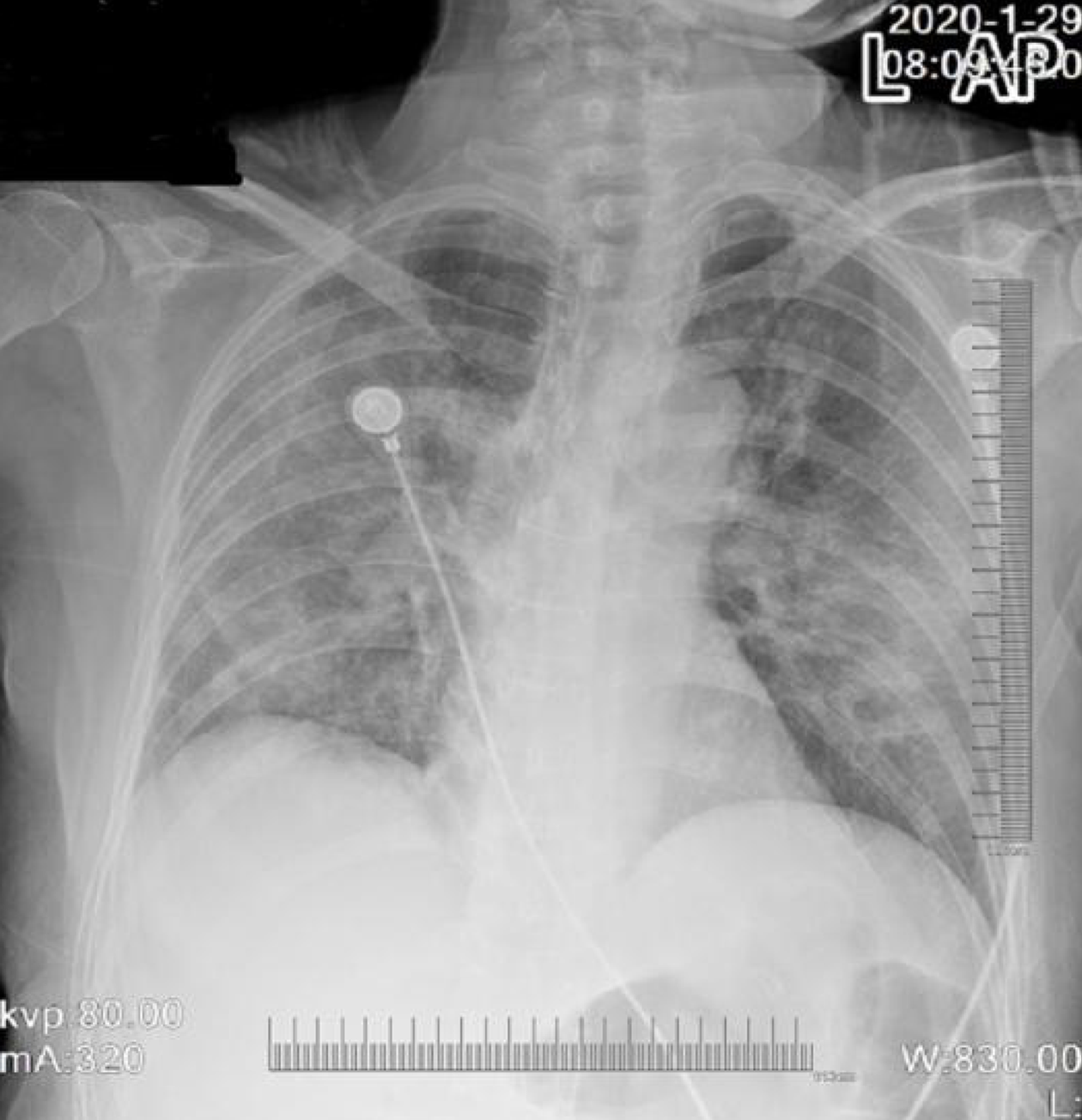
Chest computed tomography (CT) revealed bilateral multi-patchy consolidation and ground-glass opacities (Figure 1).
Pharyngeal swab nucleic acid test for SARS-CoV-2 was positive. The final diagnosis was COVID-19.
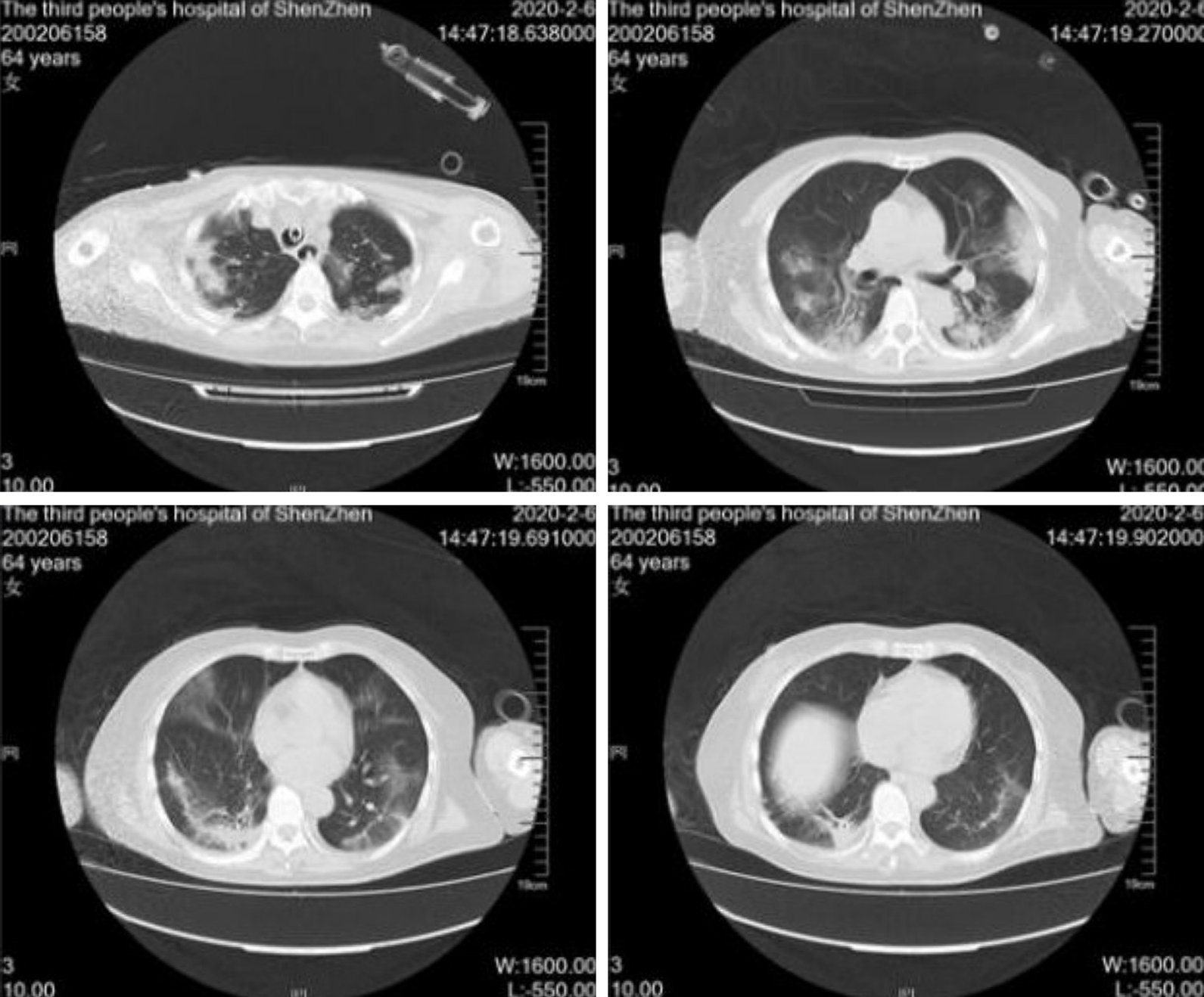
High-flow nasal catheter oxygen therapy was administered to the patient soon after admission. Intermittent noninvasive mechanical ventilation was used, and the oxygenation index was maintained at approximately 200 mmHg. Interferon (60 µg, twice daily) atomization combined with lopinavir/ritonavir tablets (500 mg, oral, twice daily) was administered. Gamma globulin (10 g, intravenous drip, once daily) and thymalfasin (1.6 mg, subcutaneous injection, once every 12 h) were administered to enhance immunity. Naltrexate calcium (4100 µg subcutaneous injection, once daily) was administered to correct coagulation abnormalities. However, the patient's condition deteriorated, and the oxygenation index decreased to 150 mmHg on the 5th day following admission. Invasive mechanical ventilation in the prone position (VCV-A/C mode, 14-16 h/d) was immediately implemented. The oxygenation index quickly increased to 300 mmHg. Antiviral therapy, i.e., ribavirin (0.5, intravenous drip, twice daily), was administered. Ceftazidime (2.0, intravenous drip, once every 8 h) combined with linezolid (600 mg, intravenous drip, once every 12 h) was administered for anti-infection. Immunoglobulin (300 mL daily) and methylprednisolone (60 mg daily) were administered for 3 consecutive days to enhance immunity and anti-inflammatory responses, respectively. On the 7th day following admission, the patient had a large amount of thin yellow sputum. CT assessment revealed increased exudate in the lungs (Figure 2). Inflammation indicators, such as CRP (65 mg/L) and IL-6 (56 pg/mL), increased significantly. Alveolar lavage fluid galactomannan (GM) (4.2 S/CO) and blood GM (0.8 S/CO) increased, and 1,3 β-glucan level increased to 266.8 pg/mL. Secondary pulmonary aspergillosis was suspected; therefore, voriconazole (200 mg once every 12 h) was administered.
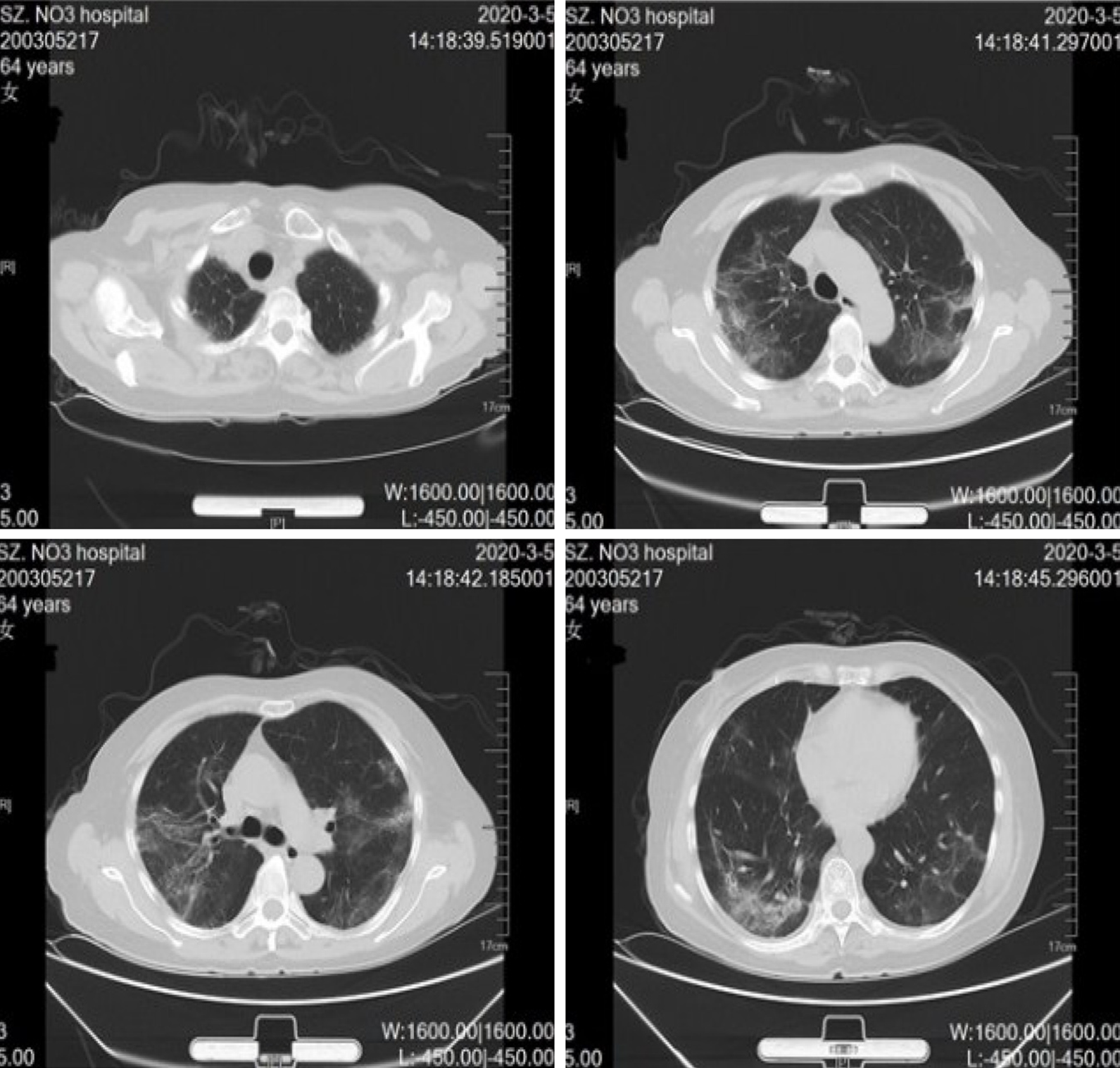
Following these treatments, the whole condition was gradually relieved, and prone position ventilation was stopped on the 9th day of admission. Three days later, tracheal intubation was removed. The nucleic acid test of COVID-19 was negative on the 21st day following admission. After an additional 3 d, the patient was discharged from the ICU. On April 4, 2020, with no complain of any discomfort, the chest CT showed an almost complete resolution of infiltrates (Figure 3), and the patient had completely recovered and was discharged.
SARS-CoV-2 is a single-stranded, positive-sense encapsulated RNA virus that is categorized as a β-coronavirus similar to SARS-CoV and Middle East respiratory syndrome coronavirus. These three viruses are believed to be of zoonotic origin and exhibit cross-species transmission. SARS-CoV is most closely related to SARS-CoV-2, which shares approximately 80% identity at the nucleotide level, and both viruses bind to cells via the same cellular receptor, namely, angiotensin-converting enzyme 2 (ACE2)[9]. The lung is the most vulnerable target for COVID-19, and most fatal cases are attributed to diffuse alveolar damage and progressive respiratory failure[10]. However, ACE2 is not only expressed on the surface of lung alveolar epithelial cells, it is also present in vascular endothelial cells, enterocytes of the small intestine, and arterial smooth muscle cells[11]. In addition, in cases with sepsis or septic shock, the entire body system is affected due to cytokine storm. As a result, critically ill patients can present many complications in addition to acute respiratory distress syndrome (ARDS), such as acute renal injury, cardiovascular complications[12], thromboembolic disease[13], acro-ischemia, and secondary or fungal infections[10,14]. Therefore, complicated clinical manifestations present, and treatment of this disease is tricky.
In this case, the patient had a history of exposure, and the manifestations, such as fever, cough, shortness of breath, and the chest radiograph with typical ground glass opacities, were all suspicious of SARS-CoV-2 infection. The diagnosis of COVID-19 was subsequently confirmed after a positive nucleic acid test for SARS-CoV-2. In total, 60%-80% of COVID-19 cases exhibit mild and moderate presentations with a favorable prognosis[8,15]. However, in critical patients with progressive deterioration after admission, an approximately 49%-67% mortality was noted[6,8]. Among those requiring mechanical ventilation support, mortality rates of 81%-88% are observed[16]. Risk factors associated with critical illness in COVID-19 have been examined[6,14]. Specifically, older age, comorbidities, gender, smoking, the degree of lesions in the lung, and the increase of potential biological markers, such as IL-6, CRP, and D-dimer (DD), all exhibit a potential connection to disease severity.
Although multiple treatment strategies, such as lopinavir/ritonavir, hydr-oxychloroquine (or chloroquine), abidor, interferon, and ribavirin, have been investigated for COVID-19 treatment[17-20], no consistent conclusions were obtained, and many questions have also arisen with regard to the rigorous designs of those studies[21,22]. To date, no definitive cure for COVID-19 has been recommended by the International Campaign to Save Sepsis and the National Institutes of Health[23]. We used a combination of interferon, lopinavir/ritonavir, and ribavirin for antiviral treatment. However, the nucleic acid test results remained positive 21 d after admission, suggesting that these drugs may not be suitable for SARS-CoV-2 clearance. Radcliffe is reported as the most promising drug for COVID-19 treatment, and one observation study based on critical COVID-19 patients showed that Radcliffe improved prognosis in 68% (36/53) of patients. In addition, 57% of cases were successfully weaned from extubation, and the mortality rate was 13%[24]. Nevertheless, limitations of that study include the lack of a random control, the simultaneous use of other antivirus drugs, and the limited number of patients included. Thus, that study was underpowered to produce convincing conclusions, and more evidence is required to clarify the clinical value of Radcliffe in COVID-19 treatment.
Symptomatic and optimal supportive care represents the primary treatment for this disease. Given that approximately 67% of critical COVID-19 cases have ARDS[16], reasonable respiratory support is more important. High-flow oxygen therapy (HFNC) or noninvasive mechanical ventilation (NIV) are priority choices for patients with mild ARDS, cases that do not respond well to HFNC or NIV treatment, or those with moderate or severe ARDS (P/F < 150 mmHg). Invasive mechanical ventilation should be performed as early as possible[23,25], but the treatment should not be excessive given that improper ventilation performance may cause ventilator-related lung injury and increase the risk of nosocomial infection[26,27]. Invasive mechanical ventilation in COVID-19 patients should also follow the ARDS lung protection ventilation strategy[10]. Gattinoni et al[28,29] classified COVID-19 respiratory failure cases into two different types based on severity. One type is characterized by no obvious dyspnea, and lung compliance is approximately normal (> 50 mL/cm water column). In addition, low ventilation/blood flow ratio, small lung weight, and low recoverability are noted, and the underlying mechanism of hypoxemia is attributed to pulmonary vasoconstriction, which results from an imbalance in the ventilation/blood flow ratio. The other types of respiratory failure account for 20%-30% of cases, and severe hypoxemia is accompanied by decreased lung compliance (< 40 mL/cm water column), a large right-to-left partial flow rate and lung weight, and high repeatability and frequently presents with mechanical ventilation-related lung injury. Respiratory support treatment of these two types of respiratory failure should be different. In the first type of patients with high lung compliance and low ventilator-induced lung injury risk, deformation can be tolerated, so the tidal volume can be greater than 6 mL/kg. The positive end-expiratory pressure (PEEP) should be set at a lower level (8-10 cmH2O) given its low recoverability. In contrast, in the second type of patients, the standard strategy for severe ARDS ventilation is generally employed, namely, maintaining a low tidal volume and increased PEEP support (can be cautiously increased to 14-15 cmH2O).
COVID-19 patients typically exhibit good responses to prone position ventilation, which should be implemented as early as possible. Some scholars perform prone position ventilation during the conventional oxygen therapy or high flow oxygen process. This position promotes collapsed alveolar recruitment, increases ventilation/blood flow ratio, and improves respiratory system compliance and right heart function[23,30]. Gattinoni et al[28] believed that prone position ventilation can improve the oxygenation in type one patients given the redistribution of intrapulmonary blood perfusion instead of the re-expansion of collapsed lung tissue, which contributes to improvements in the ventilation/blood flow ratio. In this case, no improvement was observed after HFNC and NIV implementation. Then, invasive mechanical ventilation was immediately performed in the prone position. Thus, the patient’s situation significantly improved, and we believe that this respiratory support strategy was the key to the prognosis.
A hypercoagulable state is very common in COVID-19 patients, particularly in severe and critical cases[31-33]. Increased DD levels are an independent risk factor for ARDS and death[34]. In total, 71% of fatal cases presented with disseminated intravascular coagulation[35]. In addition, venous thromboembolism (VTE) and pulmonary embolism are not rare, and the incidence of cerebral infarction in severe COVID-19 cases was 4.5%[36]. Several guidelines suggest that VTE prevention should be considered in severe and critical COVID-19 patients, and low molecular weight heparin is preferred if no anticoagulation contraindication exists[37-39]. In this case, low molecular weight heparin was administered immediately after admission. Although the DD increased significantly during the course of the disease, no complications of VTE and other thrombotic events occurred.
Antibiotics are not recommended in the early stage of virus infection. However, secondary bacterial or fungal infection may occur in critical patients who required mechanical ventilation (especially after 5-7 d of mechanical ventilation). The incidence of nosocomial-acquired pneumonia is 13.5%-31%[16,25]. In case of sepsis, the possible etiology and drug resistance should be evaluated, and early empirical anti-infection treatment should be considered. Anti-fungal treatment should be given since critical patients are prone to experience secondary fungal infections (especially aspergillus), representing one important reason for immune deficiency in COVID-19[16] given that lymphocytes are the target cell type of SARS-CoV-2. In total, 80%-100% of critical COVID-19 patients exhibit decreased lymphocytes, which is associated with disease severity and mortality[16,32,40]. Therefore, clinicians should be careful when anti-bacterial treatment yielded no improvements, and signs of fungal infection should be monitored (e.g., abnormal radiological findings and positive G test/GM test). In this case, the infection deteriorated on the 10th day after admission (the 5th day after tracheal intubation) although antibiotics were administered. We found that the GM value of bronchoalveolar lavage fluid increased significantly, and pulmonary aspergillus was subsequently considered. This diagnosis was correct because the patient’s condition improved after voriconazole treatment.
The mortality of severe COVID-19 patients is high, and no effective antiviral drugs are available. Timely intubation, reasonable mechanical ventilation support, appropriate anti-infection treatment, early anticoagulation and immune support, and other comprehensive measures may help to reduce the course of disease and patient mortality.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ayukekbong JA S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | WHO statement on the novel coronavirus. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). 2020. Available from: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). |
| 2. | Liu Y, Gayle AA, Wilder-Smith A, Rocklöv J. The reproductive number of COVID-19 is higher compared to SARS coronavirus. J Travel Med. 2020;27:1-4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2041] [Cited by in RCA: 1578] [Article Influence: 315.6] [Reference Citation Analysis (0)] |
| 3. | Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1341] [Reference Citation Analysis (0)] |
| 4. | Mizumoto K, Chowell G. Transmission potential of the novel coronavirus (COVID-19) onboard the diamond Princess Cruises Ship, 2020. Infect Dis Model. 2020;5:264-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 119] [Cited by in RCA: 141] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 5. | WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 2020. Available from: https://www.who.int/publications/i/item/report-of-the-who-china-joint-mission-on-coronavirus-disease-2019-(covid-19). |
| 6. | Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054-1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17476] [Cited by in RCA: 18204] [Article Influence: 3640.8] [Reference Citation Analysis (0)] |
| 7. | Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, Iotti G, Latronico N, Lorini L, Merler S, Natalini G, Piatti A, Ranieri MV, Scandroglio AM, Storti E, Cecconi M, Pesenti A; COVID-19 Lombardy ICU Network. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574-1581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3537] [Cited by in RCA: 3826] [Article Influence: 765.2] [Reference Citation Analysis (0)] |
| 8. | Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11409] [Cited by in RCA: 11508] [Article Influence: 2301.6] [Reference Citation Analysis (0)] |
| 9. | Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15248] [Cited by in RCA: 14133] [Article Influence: 2826.6] [Reference Citation Analysis (1)] |
| 10. | Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, Liu S, Zhao P, Liu H, Zhu L, Tai Y, Bai C, Gao T, Song J, Xia P, Dong J, Zhao J, Wang FS. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420-422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5228] [Cited by in RCA: 5786] [Article Influence: 1157.2] [Reference Citation Analysis (2)] |
| 11. | Fehr AR, Perlman S. Coronaviruses: an overview of their replication and pathogenesis. Methods Mol Biol. 2015;1282:1-23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1889] [Cited by in RCA: 2096] [Article Influence: 209.6] [Reference Citation Analysis (0)] |
| 12. | Atri D, Siddiqi HK, Lang JP, Nauffal V, Morrow DA, Bohula EA. COVID-19 for the Cardiologist: Basic Virology, Epidemiology, Cardiac Manifestations, and Potential Therapeutic Strategies. JACC Basic Transl Sci. 2020;5:518-536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 206] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 13. | Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3488] [Cited by in RCA: 3408] [Article Influence: 681.6] [Reference Citation Analysis (0)] |
| 14. | Released by National Health Commission & National Administration of Traditional Chinese Medicine on March 3 2020. Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7). Chin Med J (Engl). 2020;133:1087-1095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 374] [Cited by in RCA: 531] [Article Influence: 106.2] [Reference Citation Analysis (0)] |
| 15. | Special Expert Group for Control of the Epidemic of Novel Coronavirus Pneumonia of the Chinese Preventive Medicine Association. [An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19)]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 137] [Reference Citation Analysis (0)] |
| 16. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6231] [Cited by in RCA: 6660] [Article Influence: 1332.0] [Reference Citation Analysis (0)] |
| 17. | Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, Ruan L, Song B, Cai Y, Wei M, Li X, Xia J, Chen N, Xiang J, Yu T, Bai T, Xie X, Zhang L, Li C, Yuan Y, Chen H, Li H, Huang H, Tu S, Gong F, Liu Y, Wei Y, Dong C, Zhou F, Gu X, Xu J, Liu Z, Zhang Y, Li H, Shang L, Wang K, Li K, Zhou X, Dong X, Qu Z, Lu S, Hu X, Ruan S, Luo S, Wu J, Peng L, Cheng F, Pan L, Zou J, Jia C, Wang J, Liu X, Wang S, Wu X, Ge Q, He J, Zhan H, Qiu F, Guo L, Huang C, Jaki T, Hayden FG, Horby PW, Zhang D, Wang C. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020;382:1787-1799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3386] [Cited by in RCA: 3627] [Article Influence: 725.4] [Reference Citation Analysis (0)] |
| 18. | Zhang WH, Lu HZ, Gao Y, Hu BJ, Li F, Li X, Li YC, Mao EQ, Qu HP, Shi KH, Wang L, Wang QB, Wang S, Yu KL, Zeng M, Zhang W, Zhu DM, Zhu L. Comprehensive treatment and management of corona virus disease 2019: expert consensus statement from Shanghai. Zhonghua Chuanranbing Zazhi. 2020;38:134-138. |
| 19. | Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Tissot Dupont H, Honoré S, Colson P, Chabrière E, La Scola B, Rolain JM, Brouqui P, Raoult D. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020;56:105949. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3279] [Cited by in RCA: 3272] [Article Influence: 654.4] [Reference Citation Analysis (0)] |
| 20. | Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14113] [Cited by in RCA: 14767] [Article Influence: 2953.4] [Reference Citation Analysis (0)] |
| 21. | Ferner RE, Aronson JK. Chloroquine and hydroxychloroquine in covid-19. BMJ. 2020;369:m1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 241] [Article Influence: 48.2] [Reference Citation Analysis (0)] |
| 22. | Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. JAMA. 2020;323:1824-1836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 978] [Cited by in RCA: 1273] [Article Influence: 254.6] [Reference Citation Analysis (0)] |
| 23. | Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, Oczkowski S, Levy MM, Derde L, Dzierba A, Du B, Aboodi M, Wunsch H, Cecconi M, Koh Y, Chertow DS, Maitland K, Alshamsi F, Belley-Cote E, Greco M, Laundy M, Morgan JS, Kesecioglu J, McGeer A, Mermel L, Mammen MJ, Alexander PE, Arrington A, Centofanti JE, Citerio G, Baw B, Memish ZA, Hammond N, Hayden FG, Evans L, Rhodes A. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Crit Care Med. 2020;48:e440-e469. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 634] [Cited by in RCA: 635] [Article Influence: 127.0] [Reference Citation Analysis (0)] |
| 24. | Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, Castagna A, Feldt T, Green G, Green ML, Lescure FX, Nicastri E, Oda R, Yo K, Quiros-Roldan E, Studemeister A, Redinski J, Ahmed S, Bernett J, Chelliah D, Chen D, Chihara S, Cohen SH, Cunningham J, D'Arminio Monforte A, Ismail S, Kato H, Lapadula G, L'Her E, Maeno T, Majumder S, Massari M, Mora-Rillo M, Mutoh Y, Nguyen D, Verweij E, Zoufaly A, Osinusi AO, DeZure A, Zhao Y, Zhong L, Chokkalingam A, Elboudwarej E, Telep L, Timbs L, Henne I, Sellers S, Cao H, Tan SK, Winterbourne L, Desai P, Mera R, Gaggar A, Myers RP, Brainard DM, Childs R, Flanigan T. Compassionate Use of Remdesivir for Patients with Severe Covid-19. N Engl J Med. 2020;382:2327-2336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1926] [Cited by in RCA: 1885] [Article Influence: 377.0] [Reference Citation Analysis (0)] |
| 25. |
Zheng RQ, Hu M, Li XY, Hu B, Jiang L, Zhong M, Sang L, Zheng X, Pan C, Zhao BL, Zhang W.
Expert recommendations for respiratory treatment of severe COVID-19. |
| 26. | Respiratory care committee of Chinese Thoracic Society. [Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia]. Zhonghua Jie He He Hu Xi Za Zhi. 2020;17:E020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 47] [Reference Citation Analysis (0)] |
| 27. | Wang CY, Jiang W, Xia Y, Weng L, Du B. [Airborne spread of coronavirus in critical coronavirus disease 2019 patients with different oxygen therapies]. Zhonghua Nei Ke Za Zhi. 2020;59:664-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 28. | Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not. Crit Care. 2020;134-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 372] [Cited by in RCA: 433] [Article Influence: 86.6] [Reference Citation Analysis (0)] |
| 29. | Gattinoni L, Chiumello D, Caironi P, Busana M, Romitti F, Brazzi L, Camporota L. COVID-19 pneumonia: different respiratory treatments for different phenotypes. Intensive Care Med. 2020;46:1099-1102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1016] [Cited by in RCA: 1199] [Article Influence: 239.8] [Reference Citation Analysis (0)] |
| 30. | Pan C, Zhang W, Du B, Qiu HB, Huang YZ. [Prone ventilation for coronavirus disease 2019: an urgent salvage therapy]. Zhonghua Nei Ke Za Zhi. 2020;59:670-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 31. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30124] [Article Influence: 6024.8] [Reference Citation Analysis (3)] |
| 32. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12979] [Article Influence: 2595.8] [Reference Citation Analysis (1)] |
| 33. | Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, Psaltopoulou T, Gerotziafas G, Dimopoulos MA. Hematological findings and complications of COVID-19. Am J Hematol. 2020;834-847. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 936] [Cited by in RCA: 1211] [Article Influence: 242.2] [Reference Citation Analysis (0)] |
| 34. | Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4960] [Cited by in RCA: 5518] [Article Influence: 1103.6] [Reference Citation Analysis (1)] |
| 35. | Arachchillage DRJ, Laffan M. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18:1233-1234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 160] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 36. | Mei H, Hu Y. [Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19]. Zhonghua Xue Ye Xue Za Zhi. 2020;41:185-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 37] [Reference Citation Analysis (0)] |
| 37. | Zhai Z, Li C, Chen Y, Gerotziafas G, Zhang Z, Wan J, Liu P, Elalamy I, Wang C; Prevention Treatment of VTE Associated with COVID-19 Infection Consensus Statement Group. Prevention and Treatment of Venous Thromboembolism Associated with Coronavirus Disease 2019 Infection: A Consensus Statement before Guidelines. Thromb Haemost. 2020;937-948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 239] [Cited by in RCA: 257] [Article Influence: 51.4] [Reference Citation Analysis (0)] |
| 38. | Song JC, Wang G, Zhang W, Zhang Y, Li WQ, Zhou Z; People’s Liberation Army Professional Committee of Critical Care Medicine, Chinese Society on Thrombosis and Haemostasis. Chinese expert consensus on diagnosis and treatment of coagulation dysfunction in COVID-19. Mil Med Res. 2020;7:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 39. | Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH; Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:2950-2973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2178] [Cited by in RCA: 2191] [Article Influence: 438.2] [Reference Citation Analysis (0)] |
| 40. | Russell CD, Millar JE, Baillie JK. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395:473-475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1415] [Cited by in RCA: 1444] [Article Influence: 288.8] [Reference Citation Analysis (0)] |