Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.2038
Peer-review started: January 16, 2020
First decision: February 26, 2020
Revised: April 7, 2020
Accepted: April 15, 2020
Article in press: April 15, 2020
Published online: May 26, 2020
Processing time: 129 Days and 22.8 Hours
Cases of cryptococcal pneumonia are frequently observed in patients with various innate or acquired immunodeficiencies, including organ transplant patients, cancer patients undergoing chemotherapy, patients with acquired immune deficiency syndrome, or patients on dialysis. Fluconazole is most often used to treat this condition when it is detected.
In the present report, we describe the case of a 42-year-old human immunodeficiency virus-negative man with normal immune function who had cryptococcal pneumonia that was diagnosed after undergoing computed tomography-guided percutaneous lung puncture. We successfully treated this patient via administration of 200 mg voriconazole twice per day for 9 mo.
This report provides evidence of the successful treatment of pulmonary cryptococcosis using voriconazole.
Core tip: In the present report, we describe the case of a 42-year-old human immunodeficiency virus-negative man with normal immune function who had cryptococcal pneumonia that was diagnosed after undergoing computed tomography-guided percutaneous lung puncture. We successfully treated this patient via administration of 200 mg voriconazole twice per day for 9 mo. This report provides evidence of the successful treatment of pulmonary cryptococcosis using voriconazole.
- Citation: Jiang XQ, Zhang YB. Cryptococcal pneumonia in a human immunodeficiency virus-negative patient: A case report. World J Clin Cases 2020; 8(10): 2038-2043
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/2038.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.2038
Cryptococcosis is a form of opportunistic invasive mycosis that is driven by infection with Cryptococcus neoformans (C. neoformans), which is a relatively common environmental microorganism. Cryptococcal infections are most common in immunocompromised patients, but they can also infect immunocompetent individuals. Pathogenic cryptococci have C. neoformans var neoformans and C. neogormans var gattii, which are the two most common causes of this infection in humans[1,2]. The mechanistic basis for such cryptococcal infections remains to be fully elucidated[3], with C. neoformans infections being most common in HIV-positive patients and Cryptococcus gattii infections being more commonly observed in immunocompetent persons. Inhalational exposure is thought to be the most common mode of infection, although bird droppings are also believed to be a potential source of infection in some cases[4]. While exposure to C. neoformans is relatively common, only patients with dysfunctional cell-mediated immune responses typically suffer from invasive forms of cryptococcal disease[5]. Infections with cryptococci can result in skin lesions, or in more serious conditions including meningitis and pneumonia[6]. Pulmonary cryptococcosis often presents with a series of variable and nonspecific physical symptoms and imaging findings, leading it to often be incorrectly diagnosed as a more typical form of pneumonia, or as another condition such as diffuse lung disease or lung cancer. Herein, we describe the case of an immunocompetent patient who suffered from pulmonary cryptococcosis complicated by fluconazole resistance and voriconazole sensitivity.
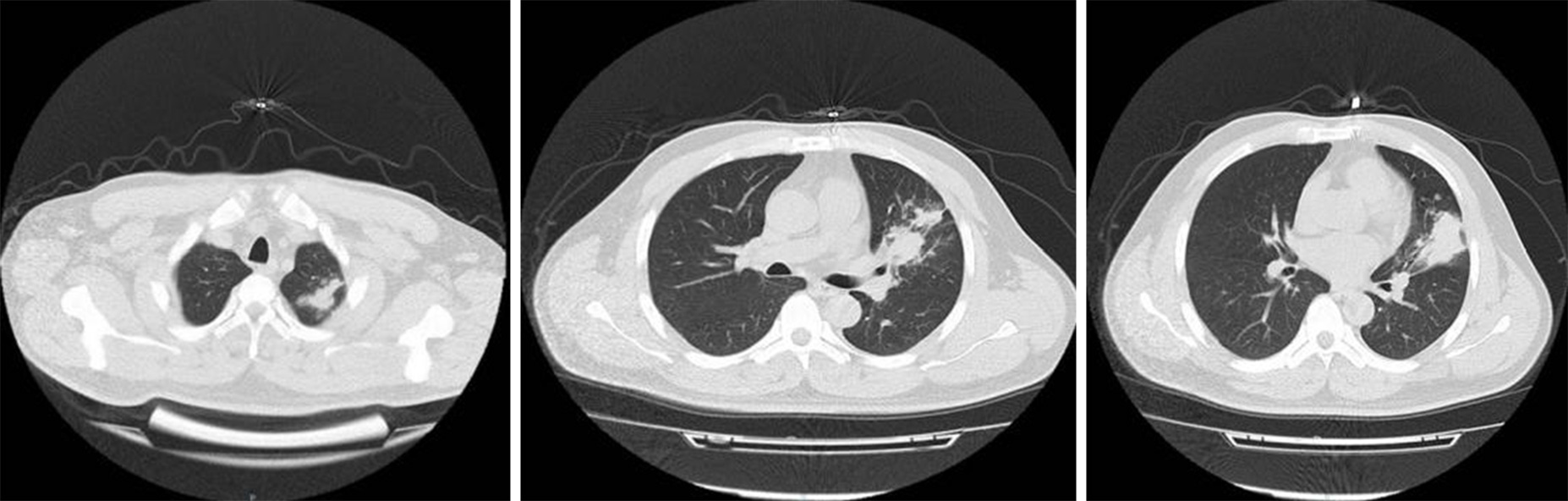
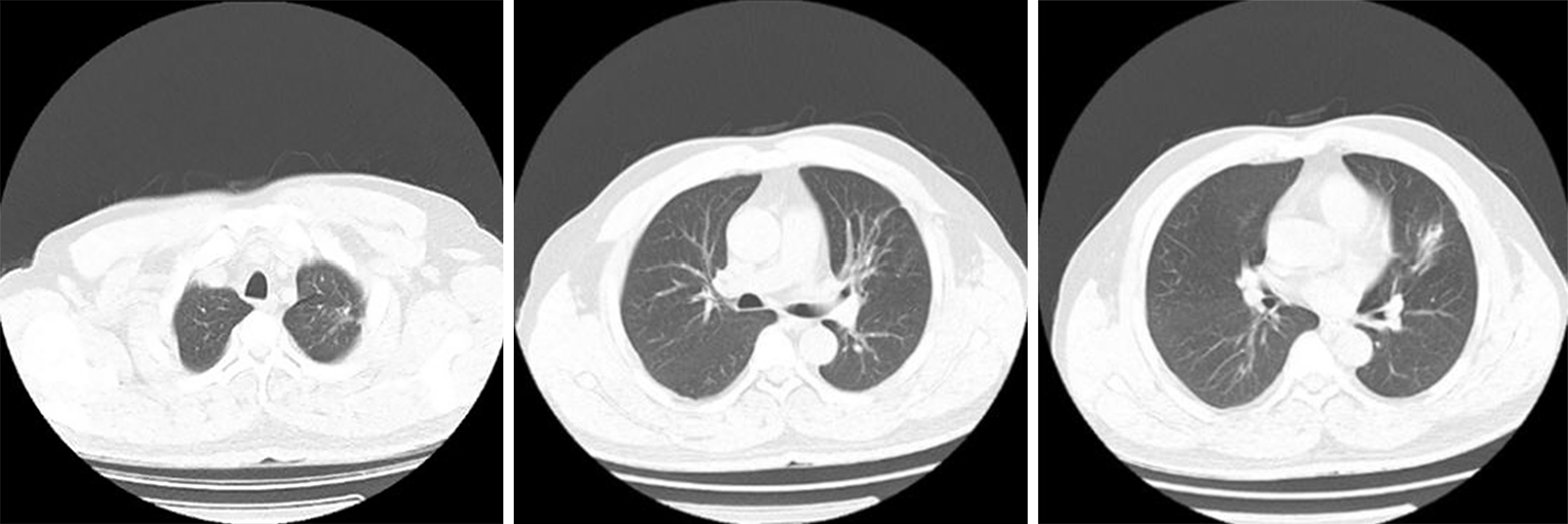
A 42-year-old man was admitted to our hospital suffering from a non-resolving case of pneumonia. The patient had suffered from slight cough for 1 mo, without any associated headache, pleuritic, fever, or sputum production. Two weeks prior to admission, the patient had undergone a routine physical examination, during which a chest computed tomography (CT) scan detected the presence of infiltrative pneumonia in the upper-left lung (Figure 1). The patient had no history of allergies or pulmonary tuberculosis, and he was not a smoker.
The patient had a free previous medical history.
At the time of initial admission, the patient had a heart rate of 84 bpm, respiratory rate of 20 breaths per minute, body temperature of 36.5 °C, and blood pressure of 180/120 mmHg.
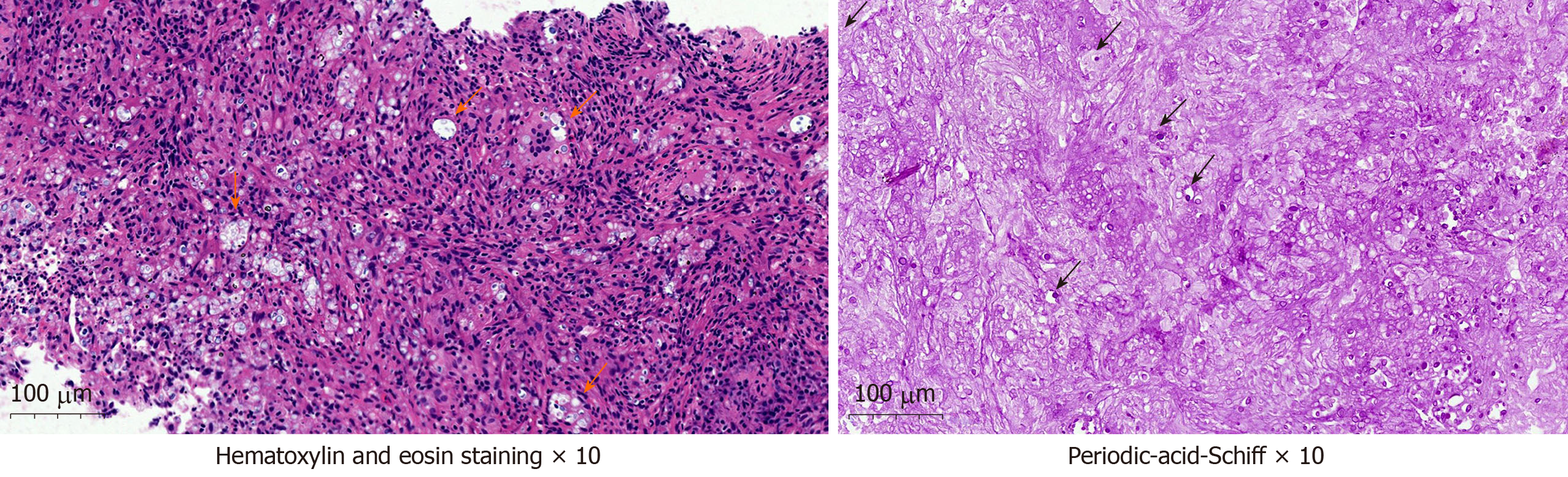
Upon physical examination, the patient exhibited no sighs of wheezing or crackling in the lungs, and no neck lymph nodes were palpable. A complete blood count examination revealed leukocyte numbers to be in the normal range (6.85 × 109/L). Normal liver and renal function and normal electrolyte levels were also detected during routine laboratory testing. The patient was also found to be seronegative for an anti-human immunodeficiency virus antibody. Sputum was first analyzed for acid-fast bacteria, with this examination failing to detect any microorganisms. CT-guided lung puncture was next conducted, and pathological examination of the collected tissue revealed the presence of granulomatous lesions containing both fungal spores and multinucleated giant cells. Hematoxylin and eosin and periodic-acid-Schiff staining of these tissue samples confirmed the presence of yeast-like fungi both in intercellular spaces and within the observed giant multinucleated cells (Figure 2).
The final diagnosis of the present case is cryptococcal pneumonia.
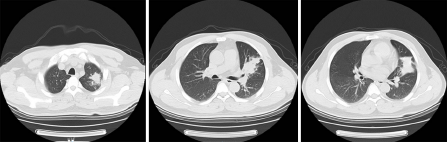
The antibiotic regimen on which the patient had been placed was subsequently replaced with a once-daily injection of fluconazole 400 mg (doubling the first dose) for 1 wk, after which the patient was discharged and prescribed oral fluconazole 400 mg once a day. However, no improvements in respiratory symptoms or radiographic findings were detected after a 6-wk treatment period (Figure 3). The patient was found to have a serum cryptococcal antigen titer > 1:80 after this 6-wk period. The patient was thereafter administered with 200 mg oral voriconazole twice per day for 10 wk.
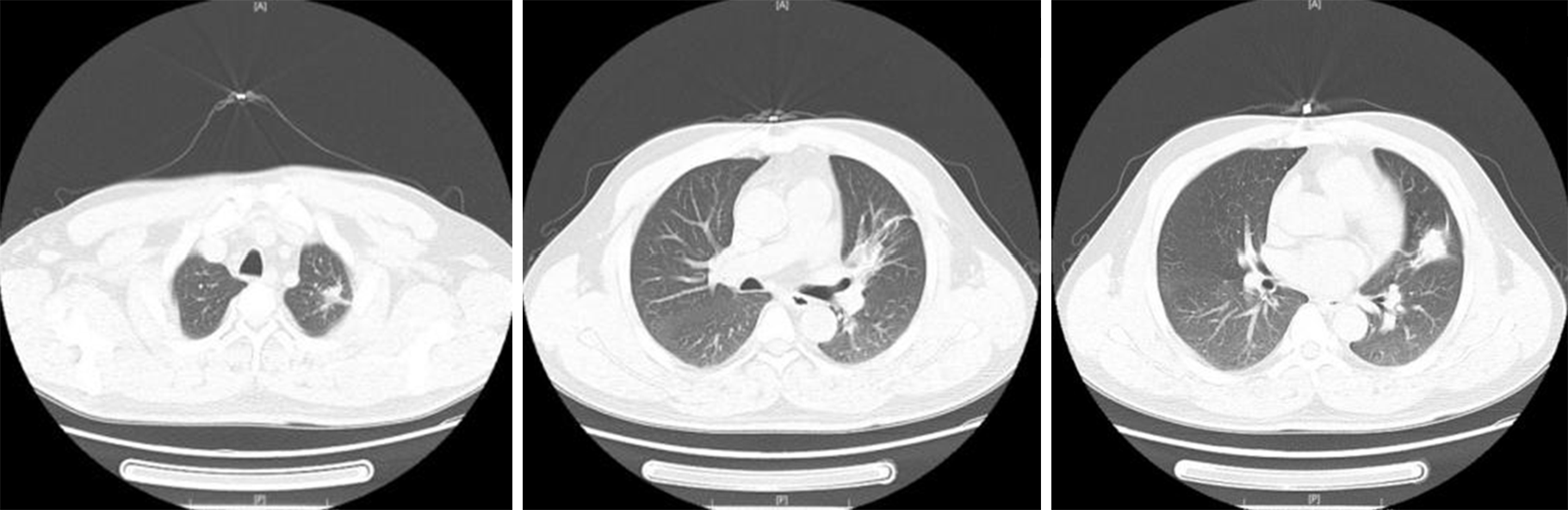
The patient's overall condition improved, with chest X-rays demonstrating a steady decrease in the size of the left lung mass (Figure 4). Following a 9-mo voriconazole course, > 90% lesion absorption was observed (Figure 5).
Cryptococcosis is a form of invasive infectious disease caused by pathogenic cryptococci. Soil contaminated with bird droppings is one of the most common sources of C. neoformans[7-9], with human infections often occurring due to microbial inhalation. However, there are some documented cases of person-to-person or animal-to-person cryptococcal transmission. The patient described in the present case report lived on an apartment block wherein 40 chickens were kept. Innate and T cell-mediated immunities are the primary mediators of host immune responses to C. neoformans[10], resulting in the elevated incidence of cryptococcal infections observed among the immunocompromised.
When symptomatic, pulmonary cryptococcosis can present as a form of pneumonia associated with fever, weight loss, chest pain, coughing, and hemoptysis. However, in up to 30% of patients, these infections are asymptomatic and are only detected incidentally[11]. Typically, C. neoformans infections can be safely and reliably treated via oral administration of fluconazole. Any patients suffering from serious disease-associated symptoms, multiple lung nodules, extensive lung infiltration, and/or positive serum cryptococcal antigen levels represent good candidates for therapeutic intervention. Patients are typically administered with 400 mg of fluconazole per day for 6-12 mo, with an initial 4-wk induction dose of 600-800 mg[12].
In the present study, we observed no significant improvements in patient condition after 6 wk of treatment with fluconazole 400 mg once a day (doubling the first dose). The patient was therefore administered with voriconazole (200 mg, twice daily). After 10 wk, the patient exhibited general improvements and a reduction in mass size, with 90% lesion absorption having been achieved following a 9-mo treatment period. Maybe, the failure of initial treatment with fluconazole may be caused by insufficient initial dosing of fluconazole. Meanwhile, the present case highlights the potential for the successful treatment of pulmonary cryptococcosis using voriconazole. Further patient follow-up is ongoing.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hamed K S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Li X
| 1. | Maziarz EK, Perfect JR. Cryptococcosis. Infect Dis Clin North Am. 2016;30:179-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 462] [Article Influence: 51.3] [Reference Citation Analysis (0)] |
| 2. | Kwon-Chung KJ, Fraser JA, Doering TL, Wang Z, Janbon G, Idnurm A, Bahn YS. Cryptococcus neoformans and Cryptococcus gattii, the etiologic agents of cryptococcosis. Cold Spring Harb Perspect Med. 2014;4:a019760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 350] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 3. | Nakamura S, Miyazaki Y, Higashiyama Y, Yanagihara K, Ohno H, Hirakata Y, Shikuwa M, Mizuta Y, Tashiro T, Kohno S. Community acquired pneumonia (CAP) caused by Cryptococcus neoformans in a healthy individual. Scand J Infect Dis. 2005;37:932-935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Levitz SM. The ecology of Cryptococcus neoformans and the epidemiology of cryptococcosis. Rev Infect Dis. 1991;13:1163-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 280] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 5. | Davis J, Zheng WY, Glatman-Freedman A, Ng JA, Pagcatipunan MR, Lessin H, Casadevall A, Goldman DL. Serologic evidence for regional differences in pediatric cryptococcal infection. Pediatr Infect Dis J. 2007;26:549-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Dromer F, Mathoulin S, Dupont B, Laporte A. Epidemiology of cryptococcosis in France: a 9-year survey (1985-1993). French Cryptococcosis Study Group. Clin Infect Dis. 1996;23:82-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 154] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Johannson KA, Huston SM, Mody CH, Davidson W. Cryptococcus gattii pneumonia. CMAJ. 2012;184:1387-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, Harrison TS, Larsen RA, Lortholary O, Nguyen MH, Pappas PG, Powderly WG, Singh N, Sobel JD, Sorrell TC. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50:291-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1988] [Cited by in RCA: 1797] [Article Influence: 119.8] [Reference Citation Analysis (0)] |
| 9. | Wysham NG, Sullivan DR, Allada G. An opportunistic infection associated with ruxolitinib, a novel janus kinase 1,2 inhibitor. Chest. 2013;143:1478-1479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 10. | Gupta RK, Khan ZU, Nampoory MRN, Mikhail MM, Johny KV. Cutaneous cryptococcosis in a diabetic renal transplant recipient. J Med Microbiol. 2004;53:445-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Guy JP, Raza S, Bondi E, Rosen Y, Kim DS, Berger BJ. Cryptococcus pneumonia presenting in an immunocompetent host with pulmonary asbestosis: a case report. J Med Case Rep. 2012;6:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Choi KH, Park SJ, Min KH, Kim SR, Lee MH, Chung CR, Han HJ, Lee YC. Treatment of asymptomatic pulmonary cryptococcosis in immunocompetent hosts with oral fluconazole. Scand J Infect Dis. 2011;43:380-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |