Published online Mar 6, 2023. doi: 10.12998/wjcc.v11.i7.1488
Peer-review started: December 13, 2022
First decision: January 3, 2023
Revised: January 4, 2023
Accepted: February 15, 2023
Article in press: February 15, 2023
Published online: March 6, 2023
Processing time: 78 Days and 20 Hours
Basal cell carcinoma (BCC) is a slow-growing malignant tumor characterized by local invasiveness but an exceptionally rare metastatic potential. It ideally affects sun-exposed skin of older patients with more propensity for the facial region.
To evaluate the different clinicopathological characteristics of the facial BCC and the efficacy and safety of diode laser for the treatment of these lesions.
We retrospectively reviewed facial BCC lesions of < 1.5 cm in diameter and subjected them to diode laser ablation during the period from September 2016 to August 2021 at Al-Ramadi Teaching Hospital, Ramadi City, Iraq. Data matching the age, gender, duration, site, and clinical and histological types were registered for every subject. The functional and aesthetic outcomes and complications following diode laser ablation for each patient were also recorded.
Of 67 patients with facial BCC, there was 65.67% from the age group ≥ 60 years and 58.21% males. The mean duration of the lesions was 5.15 ± 1.836 mo. The most involved location was the nose (29.85%). About half of the cases belong to the noduloulcerative type. Solid histological type comprises 40.3% of the cases, while the least was keratotic (13.4%). Moreover, 65.2% of the solid cases were from the age group ≤ 60 years and 38.6% of the adenoid type from the age group > 60 years (P value = 0.007). Excellent aesthetic and functional outcomes were reported in all cases after 6 mo of follow-up. Few complications were reported after diode laser ablation.
Facial BCC was mostly seen in the elderly and men. The mean duration was 5.15 mo. The nose was the commonest involved site. Noduloulcerative lesions were seen in approximately half of the lesions. The age of the patients determined the histological type of the lesion (solid type was mostly seen in the age group ≤ 60 years, while, adenoid in the age group > 60 years). Diode laser ablation showed excellent functional and aesthetic outcomes following a 6-mo follow-up.
Core Tip: Facial basal cell carcinoma was mostly seen in the elderly and men. The nose was the commonest involved site. Noduloulcerative lesions were seen in approximately half of the lesions. The age of the patients determined the histological type of the lesion. Diode laser ablation showed excellent functional and aesthetic outcomes following a 6-mo follow-up.
- Citation: Khalil AA, Enezei HH, Aldelaimi TN, Al-Ani RM. Facial basal cell carcinoma: A retrospective study of 67 cases. World J Clin Cases 2023; 11(7): 1488-1497
- URL: https://www.wjgnet.com/2307-8960/full/v11/i7/1488.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i7.1488
Basal cell carcinoma (BCC) was described firstly by Jacob in 1827 and is considered the most frequent skin tumor with an incidence of 12% to 30%[1,2]. BCC is mostly occurred primarily in adults and exclusively on facial hair-bearing skin. BCC is known as a set of cutaneous malignant tumors identified by basaloid cells arranged in columns, bands, lobules, or cords[3].
Clinical types of BCC include noduloulcerative, pigmented, superficial (multifocal), and fibrosing BCC. While Histologically, there are various types including; keratitis, nodular, superficial, morpheiform, basosquamous, adenoid, and cystic[4].
BCC is a locally invasive tumor that rarely metastases. Deeply invasive tumors have increased morbidity that extended deep to facial bony tissue following nerves and spread through bony channels. Neglected tumors more than 10 cm in diameter have increased morbidity and reach to be giant BCCs that could penetrate the cranial bones[3,4].
Currently, there is a variety of treatment modalities i.e. topical therapies intralesional medication, X-ray, chemotherapy, surgery, and laser. Each one has its benefits as well as risks with diverge curing rate. The ideal treatment for BCC is the target goal of both pathologists and surgeons[5].
Nowadays, there is an urgent demand for a minimally invasive, safe, effective, and aesthetically acceptable method to cure BCC. The application of laser therapy has the potential to achieve and address this goal and demand[6]. Furthermore, there is a paucity of researches using different modalities of lasers (CO2, Nd: YAG, pulsed dye, and diode laser) in the treatment of BCC with various clearance rates. Therefore, it is necessary to perform further studies to evaluate the efficacy and safety of this modality of treatment. Hence, we aimed to assess the various clinicopathological aspects of facial BCC and the efficacy and safety of diode laser in the treatment of these tumors.
This retrospective study was conducted at Al-Ramadi Teaching Hospital, Ramadi City, Iraq. We reviewed the histopathologically confirmed cases of BCC during five years (September 2016-August 2021). This research was approved by the Ethical Approval Committee of the University of Anbar (Reference number 4, on 24-1-2021). Patients with facial BCC of any age, both gender, with a lesion less than 1.5 cm in diameter, and treated with diode laser were enrolled in the study. While non-facial BCC, lesion ≥ 1.5 cm in diameter, bony infiltrated lesion, recurrent cases, those with other associated skin or autoimmune diseases like Xeroderma pigmentosa, and those cases with incomplete data on medical records or cannot contact them for follow-up were excluded from the current study.
All patients were referred from the department of dermatology for laser surgical intervention. The presumed BCC lesions were diagnosed after an incisional or punch biopsy examination[7]. Later on, the patients were prepared for laser intervention returned to the clinic and the treatment protocol was clarified to each patient and informed consent was signed to accept the treatment protocol.
Detailed information from every participant concerning the age, gender, duration of the disease, and involved site was recorded. The nature of clinical growth was also described, namely nodular, pigmented, noduloulcerative, or multifocal superficial type.
The treatment plan included preoperative antisepsis with 70% alcohol for 45-60 s, laser safety goggles were used for all attendants (patients and surgeon), infiltration of local anesthesia was done around, beneath, and intralesional with 1.8 mL cartridge of 2% lidocaine and epinephrine. The lesions ablated completely as one piece with 2-3 mm safe margins and bed by diode laser 940 nm/980 nm applying 2 W, after careful lesion ablation; the laser tip was moved in an inverted U-shaped direction on site of surgery to ensure homeostasis. The wound was left to heal by secondary intention. The specimen was kept in 10% formaldehyde solution and sent for histopathological examination. Specimens of BCC were subjected to recommended procedures of tissue processing, 5 µm thickness slice of paraffin-embedded blocks was placed into a glass slide; stained with hematoxylin and eosin staining preceding the inspection under the light microscope.
The histopathological diagnosis was confirmed by describing the growth pattern and differentiation of the tumor cells that can be divided into adenoid type if it was differentiated toward eccrine gland; solid if it was undifferentiated, and keratotic type if it was differentiated to the hair follicle. Besides, description of whether the margins of the specimens were safe and free from the tumor cells or not. Patients were kept close to follow-up visits for clinical evaluation and assessment for six months after the final treatment. The overall satisfaction throughout the entire follow-up period and any complications were registered too.
The Statistical Package for the Social Sciences (SPSS) version 25 for the window was used to analyze the data. The mean, median, mode, and standard deviation were used to express the continuous variables. While frequencies and percentages were used to express the categorical variables in simple tables or figures. A Chi-square test was applied for the comparison between the categorical variables. A P value of less than 0.05 is considered a statistically significant difference.
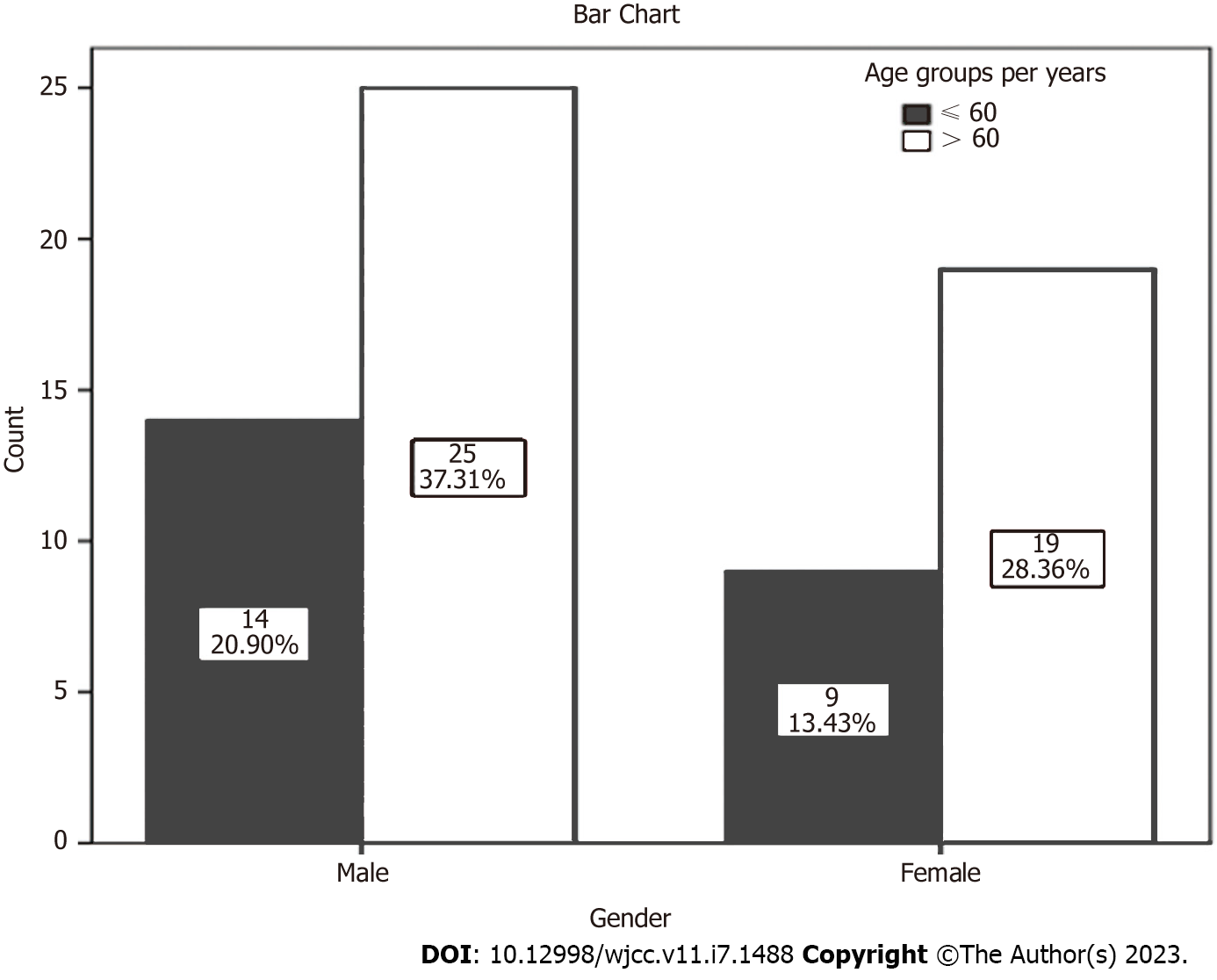
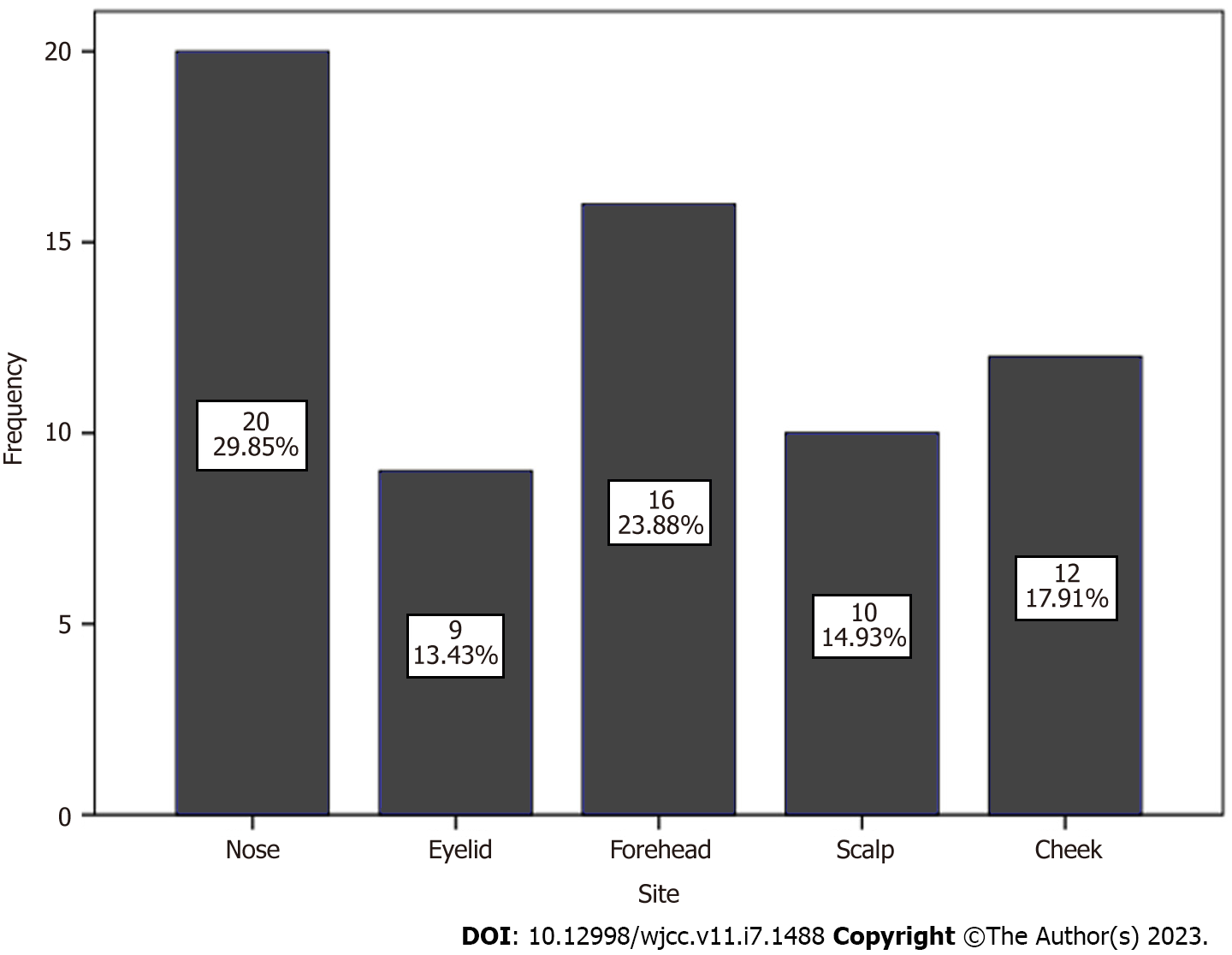
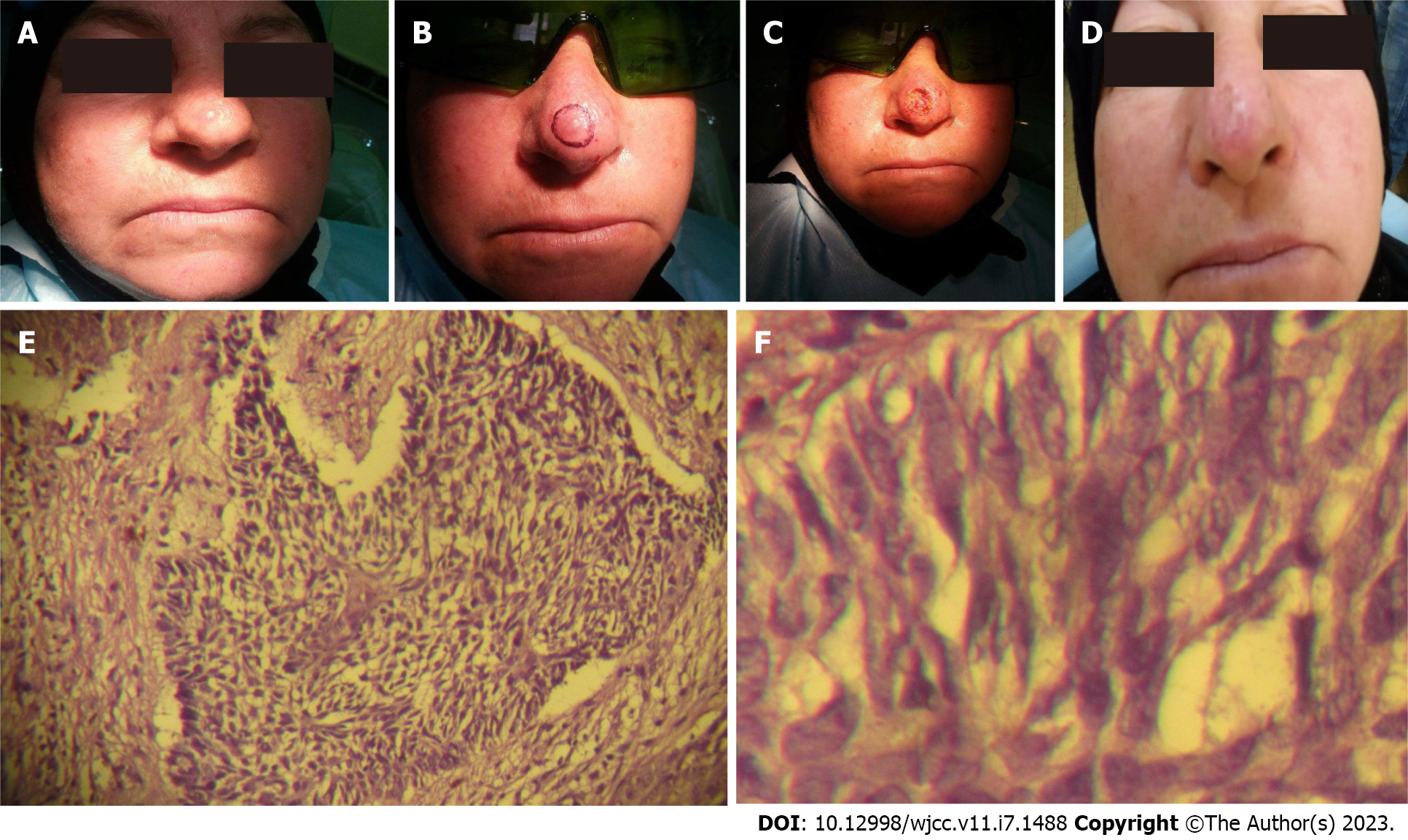
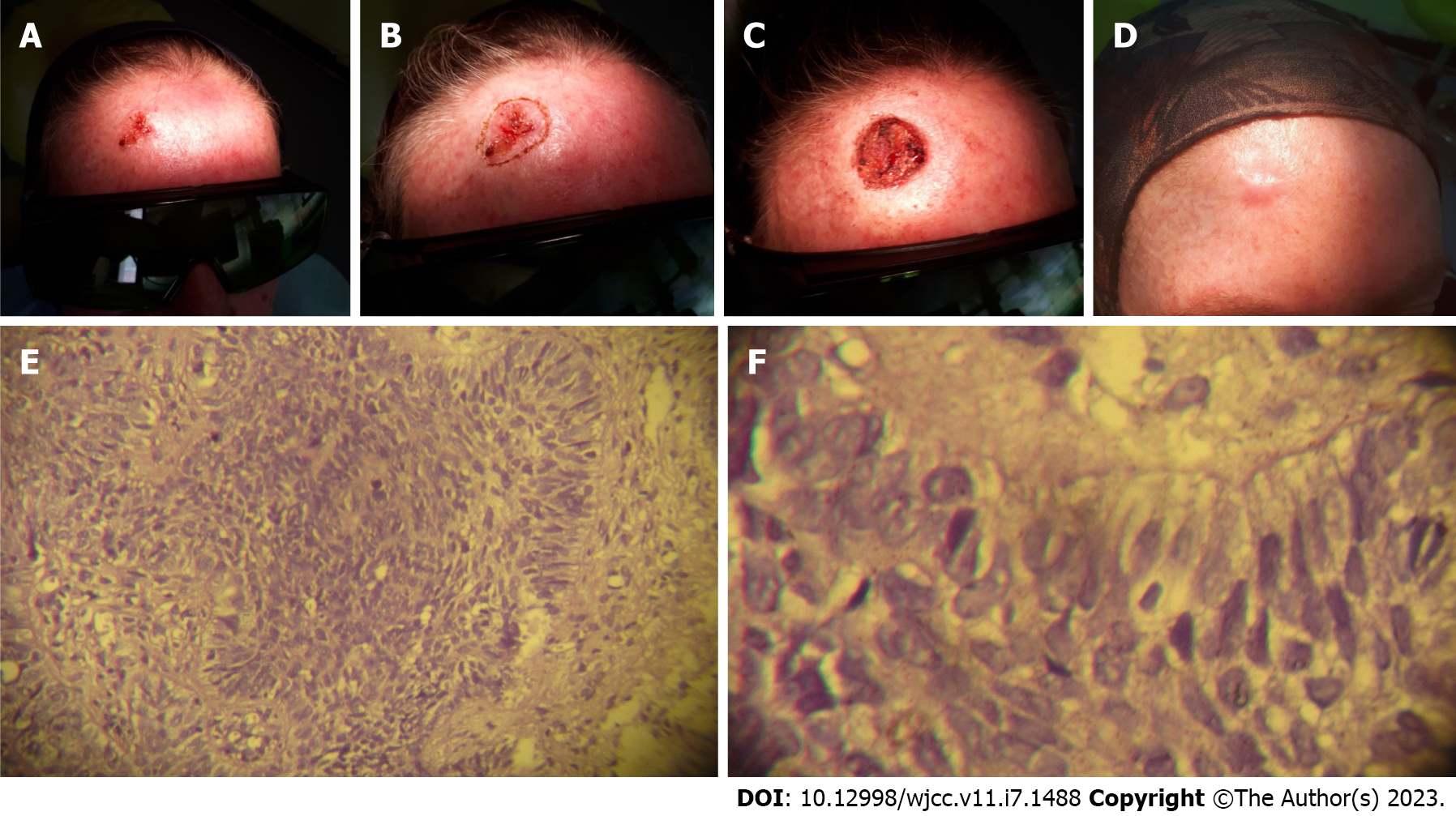
There were 67 patients with facial BCC included in the current investigation. The age was ranged from 36-82 years with a mean age of 61.28 ± 13.424 years. While the median and mode for the age were 62 and 50 years respectively. There were 44 cases (65.67%) from the age group ≥ 60 years. Males (n = 39, 58.21%) outnumber the females (n = 28, 41.79%) patients with a male/female ratio of 1.4/1 (Figure 1, Tables 1 and 2). The duration of the disease was ranged from 3-9 mo with a mean duration of 5.15 ± 1.836 mo. The most common site involved was the nose (n = 20, 29.85%) while the least eyelid (n = 9, 13.43%). However, there was no statistically significant difference (P value > 0.05) among the various sites of the BCC (Figure 2). Most of the cases were presented with less than six months (46/67). Around half of the cases belong to the noduloulcerative type and the least multifocal superficial (n = 10, 14.9%). However, there were no statistically significant differences between the type of the facial BCC and age, gender, duration of the lesions, and the involved sites (P value > 0.05) (Table 1). Solid histological type comprises the highest number (n = 27, 40.3%) of the cases. While the least type was keratotic (n = 9, 13.4%). Moreover, 15 (65.2%) of the solid cases were from the age group ≤ 60 years and 17 (38.6%) of the adenoid type from the age group > 60 years. There was a statistically significant difference between the histological type and age groups (P value = 0.007). While there were no statistically significant differences with other variables (P value > 0.05) (Table 2). All patients showed excellent functional and aesthetic outcome following diode laser ablation of the tumors. Figures 3 and 4 were two examples of our cases that showed excellent healing 6 mo following the diode laser ablation of the facial BCC. Few complications were reported after diode laser ablation (Table 3). Bleeding at the bed lesion were hemostatized by applying simple touches of 3 W diode laser 980 nm for pinpoint bleeding points. While the postoperative pain and edema were treated with prescription of paracetamol tablet 500 mg three times per day, and the redness at the periphery of the ablated area was subsided by ice packs application to the area for a three days postoperatively.
| Variable | Clinical type | P value | ||||||
| Pigmented | Noduloulcerative | Multifocal superficial | Total | |||||
| Age groups per years | 0.278 | |||||||
| ≤ 60 | 11 (47.8) | 10 (43.5) | 2 (8.7) | 23 (100) | ||||
| > 60 | 13 (29.5) | 23 (52.3) | 8 (18.2) | 44 (100) | ||||
| Total | 24 (35.8) | 33 (49.3) | 10 (14.9) | 67 (100) | ||||
| Gender | 0.691 | |||||||
| Male | 13 (33.3) | 19 (48.7) | 7 (18) | 39 (100) | ||||
| Female | 11 (39.3) | 14 (50) | 3 (10.7) | 28 (100) | ||||
| Total | 24 (35.8) | 33 (49.3) | 10 (14.9) | 67 (100) | ||||
| Duration per months | 0.710 | |||||||
| < 6 | 15 (32.6) | 24 (52.2) | 7 (15.2) | 46 (100) | ||||
| ≥ 6 | 9 (42.9) | 9 (42.9) | 3 (14.2) | 21 (100) | ||||
| Total | 24 (35.8) | 33 (49.3) | 10 (14.9) | 67 (100) | ||||
| Site | 0.605 | |||||||
| Nose | 10 (50) | 7 (35) | 3 (15) | 20 (100) | ||||
| Eyelid | 4 (44.4) | 5 (55.6) | 0 | 9 (100) | ||||
| Forehead | 5 (31.3) | 9 (56.2) | 2 (12.5) | 16 (100) | ||||
| Scalp | 3 (30) | 5 (50) | 2 (20) | 10 (100) | ||||
| Cheek | 2 (16.7) | 7 (58.3) | 3 (25) | 12 (100) | ||||
| Total | 24 (35.8) | 33 (49.3) | 10 (14.9) | 67 (100) | ||||
| Variable | Histopathological type | P value | ||||
| Solid | Adenoid | Mixed | Keratotic | Total | ||
| Age groups per years | 0.007 | |||||
| ≤ 60 | 15 (65.2) | 2 (8.7) | 2 (8.7) | 4 (17.4) | 23 (100) | |
| > 60 | 12 (27.3) | 17 (38.6) | 10 (22.7) | 5 (11.4) | 44 (100) | |
| Total | 27 (40.3) | 19 (28.4) | 12 (17.9) | 9 (13.4) | 67 (100) | |
| Gender | 0.952 | |||||
| Male | 15 (38.5) | 11 (28.2) | 7 (17.9) | 6 (15.4) | 39 (100) | |
| Female | 12 (42.9) | 8 (28.6) | 5 (17.9) | 3 (10.7) | 28 (100) | |
| Total | 27 (40.3) | 19 (28.4) | 12 (17.9) | 9 (13.4) | 67 (100) | |
| Duration per months | 0.955 | |||||
| < 6 | 19 (41.3) | 13 (28.3) | 8 (17.4) | 6 (13) | 46 (100) | |
| ≥ 6 | 8 (38.1) | 6 (28.6) | 4 (19) | 3 (14.3) | 21 (100) | |
| Total | 27 (40.3) | 19 (28.4) | 12 (17.9) | 9 (13.4) | 67 (100) | |
| Site | 0.985 | |||||
| Nose | 8 (40) | 5 (25) | 4 (20) | 3 (15) | 20 (100) | |
| Eyelid | 4 (44.4) | 2 (22.2) | 1 (11.2) | 2 (22.2) | 9 (100) | |
| Forehead | 7 (43.8) | 5 (31.3) | 3 (18.8) | 1 (6.3) | 16 (100) | |
| Scalp | 5 (50) | 2 (20) | 2 (20) | 1 (10) | 10 (100) | |
| Cheek | 3 (25) | 5 (41.6) | 2 (16.7) | 2 (16.7) | 12 (100) | |
| Total | 27 (40.3) | 19 (28.4) | 12 (17.9) | 9 (13.4) | 67 (100) | |
| Complication | Frequency | Percentage |
| Bleeding at the bed lesion | 1 | 1.5 |
| Postoperative pain | 10 | 14.9 |
| Redness at the periphery of the ablated area | 2 | 3 |
| Mild edema | 1 | 1.5 |
| Postoperative infection | 0 | 0 |
BCC is a local detrimental skin tumor; although the tumor behavior is not orderly among patients having low or even high-risk types that were based on tumor features, patient clinical history, and histological presentations i.e. demographic data including age and sex, immunosuppression, radiotherapy, organ transplant, tumor location and size, deeper invasion beyond reticular dermis, aggressive histological subtypes, and lymphovascular and/or perineural involvement[6,8,9]. The main outcomes of this study were that facial BCC was more common in the elderly and males, noduloulcerative was the most common clinical type, and solid histological type comprises 40% of the cases. Diode laser ablation revealed excellent outcomes in all cases.
Our study and several studies have shown a higher rate of BCC in men, this being due to prolonged outdoor activities under the action of ultraviolet radiation (farmers, gardeners, fishermen, and builders)[10-13]. But other studies reported female preponderance[8,14,15]. The study by George et al[14] reported a high prevalence of female patients (18/29) with facial BCC[14]. However, they did not give a history of excessive sun exposure. The female preponderance in this study might be due to that the women are subjected to a significant amount of heat and fumes during their cooking in the kitchen.
Facial BCC is more prevalent in the elderly population[12,15]. About 2/3rd of our patients were from the age group ≥ 60 years. Elderly subjects are more to acquire BCC because they have low immunity, decrease the ability of the DNA repair, and the cumulative impact of excessive sun exposure[16].
Facial BCC is usually presented late in the majority of the patients as reported by several studies[8,12,13]. This results in larger tumor size at the time of presentation which might be a risk factor regarding the behavior of the tumor. Owing to the excluded cases of large-sized tumors (≥ 1.5 cm), our cases were presented relatively earlier than the above-mentioned studies.
The nodular type of the BCC is characterized by nodules or papules that associated with telangiectasias, and on rare occasion there are central ulcerations. BCC is characterized by slow extension, local invasiveness, and an exceptionally rare metastatic potential[4,17,18]. Despite this relatively benign appearance, there are aggressive clinical forms that produce significant local tissue destructions. Given the increasing solar activity in recent years and the ozone layer depletion, there are expected to be major increases in global skin carcinoma[19]. Many of these tumors cannot distinguish from the melanocytic origin tumors on clinical background owing to the possibility of their rich content of pigmentation of some of these tumors. The classical features of the BCC are pearly appearance with telangiectasia in a nodular or papular lesion, however, these manifestations may be subtle. Therefore, dermoscopy might be helpful in distinguishing these lesions. Histopathological evaluation of biopsy is a confirmatory test[17,18]. Noduloulcerative type constitutes around 50% of the cases in the current study, but it didn’t show a significant association with the age, gender, duration of the disease, and the site of the tumor (P value > 0.05). Moreover, the present study reported that the nose was the commonest site of BCC which was consistent with other investigations[8,13,20].
Histopathologically, the different types of BCC demonstrate the general characteristic of a loose fibromucinous stroma surrounding basaloid cells (“germinative cells”) which are organized in columns, lobules, bands, and cords with a peripheral palisading. The most common type of this tumor is nodular type based on histopathological evaluation, followed by adenoid form. Further, pigmented BCC is frequently encountered in clinical practice. Several of these lesions contain a large amount of pigmentation, making them difficult to be differentiated from the melanocytic tumors. The current investigation reported various morphological types of BCC in the studied sample that diagnosed on histopathological evaluation to avoid wrong diagnosis[2,19,21,22]. Histologic assessments of BCC reveal a predictive vision in terms of behavior and recurrence risk. Depth of invasion, histologic subtype, and lymphovascular and/or perineural invasion are significant parameters in the accurate and precise treatment planning as well as prediction of metastasis and recurrence[18,23,24].
There are two aims in handling the treatment of facial BCC; functional and aesthetic requirements of the involved sites. For a tumor, less than 2 cm and from the low-risk group, a safety margin of 3 mm is required. While the tumors of larger than 2 cm and of high risk, a 4 to 6 mm safety margin is necessary to achieve optimum results. Furthermore, in recurrent and complex tumors, Mohs micrographic surgical approach is used to overcome the diffuse nature of these tumors. However, this approach is available only in certain centers as well as it requires a lot of experience and training. Therefore, a safety margin of 2 mm with strict regular follow-up is required to preserve the function of the involved tissues and avoid more complex reconstructive surgeries[25]. The laser is becoming a new and rapidly emerging tool that becomes of importance to both surgeons and pathologists in the removal of oral and maxillofacial pathological lesions that acquired expanded knowledge about its clinicopathological applications more effectively, safely, and efficiently[26]. Although the current study was of short-term follow-up (6 mo), we recommend the usage of diode laser ablation for smaller lesions (< 1.5 cm) owing to the excellent outcome regarding the functional and esthetic requirements.
The retrospective nature of the study and we didn’t take the occupation and the duration of sun or heat exposure (major risk factors of the facial BCC) of the participants into account were considered the limitations of the current study.
Facial BCC was mostly affecting the age group > 60 years and in men. The majority of the lesions were presented in less than 6 mo. The nose was the commonest predilection site of the BCC. Noduloulcerative lesions were accounted for approximately 50% of the cases. However, they didn’t show significant association with the age, gender, duration of the lesions, and the involved sites. The solid histological type was mostly seen in the age group ≤ 60 years, while, adenoid variety was commonly seen in the age group > 60 years. There was a statistically significant effect between the histological type and the age, but there was no significant association with other variables. Diode laser ablation with a safety margin of 2-3 mm showed satisfactory results concerning the functional and aesthetic outcomes on the short-term follow-up period.
Basal cell carcinoma (BCC) is considered the most frequent skin tumor. It is mostly affected adults and occurred exclusively on the skin of facial hair-bearing. Surgical excision is the treatment of choice for these lesions. Different lasers were used for the treatment of facial BCC with different cure rates.
With this retrospective study, we aimed to analyze the various features of facial BCC as well as to assess the benefits and risks of diode lasers in the treatment of these lesions.
This retrospective study aimed to evaluate various demographic, clinical, and pathological characteristics of facial BCC and assessment of the diode laser outcome in the treatment of these tumors.
In the current retrospective study, we reviewed the medical records of 67 patients with small facial BCC (< 1.5 cm in diameter) and subjected them to treatment with diode laser ablation. The study covered 5 years. Detailed information regarding the demographic, clinical, and pathological features of the tumor for each subject was recorded. The outcome following treatment regarding the functional and aesthetic results and any complications were registered too.
The majority of the cases (65.67%) belonged to the age group ≥ 60 years. About 60% were men. The mean duration of the tumors was 5.15 mo. The nose was the most commonly affected site. The noduloulcerative form was seen in about 50% of the patients. The solid histological form was seen in 40.3% of the subjects. Besides, 65.2% of the solid lesions were seen in the age group ≤ 60 years and 38.6% of the adenoid form in the age group older than 60 years (P value < 0.05). Following a six months follow-up, excellent outcomes were reported regarding the function and shape of the involved site in all patients. Postoperative pain was the most frequent complication after diode laser ablation.
Facial BCC was seen more in patients older than 60 years and males. The mean duration of the tumors was 5.15 mo. The nose was the most commonest affected site. Noduloulcerative type was seen in approximately 50% of the cases. The age of the patients might determine the histological type of the lesion (solid type was mostly seen in the age group equal to or less than 60 years, while, adenoid type was in the age group more than 60 years). Diode laser ablation is effective and safe in the management of facial BCC.
We believe that future investigations with many patients and longer follow-ups will validate these results. Besides, further studies are necessary for the comparison the diode laser ablation with other modalities in the management of BCC.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Iraq
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kadriyan H, Indonesia; Parekh M, India; Yarso KY Indonesia S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Tas B, Uyar M, Altinay S. An interesting coexistence of a classical-nodular and an adenoid-ulcerous basal cell carcinoma in the same anatomic location. J Case Rep Stud. 2014;2:401. |
| 2. | Abreo F, Sanusi ID. Basal cell carcinoma in North American blacks. Clinical and histopathologic study of 26 patients. J Am Acad Dermatol. 1991;25:1005-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Ikeda S, Kiyohara Y, Mizutani H. Comparative aspects of melanoma and non-melanoma skin cancers in Japan. J Invest Dermatol. 1989;92:204S-209S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | J Metib N, H Aboud A. Histopathologic Study for Skin Basal Cell Carcinoma. Kerbala J Med. 2018;11:3884-3888. |
| 5. | Vantuchova Y, Curik R. Histological types of basal cell carcinoma. Scr Medica. 2006;79:261-270. |
| 6. | Aldelaimi TN, Khalil AA. Clinical Application of Diode Laser (980 nm) in Maxillofacial Surgical Procedures. J Craniofac Surg. 2015;26:1220-1223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Newlands C, Currie R, Memon A, Whitaker S, Woolford T. Non-melanoma skin cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol. 2016;130:S125-S132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 123] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 8. | Kumar S, Mahajan BB, Kaur S, Yadav A, Singh N, Singh A. A study of Basal cell carcinoma in South asians for risk factor and clinicopathological characterization: a hospital based study. J Skin Cancer. 2014;2014:173582. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Donaldson MR, Coldiron BM. No end in sight: the skin cancer epidemic continues. Semin Cutan Med Surg. 2011;30:3-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Yalcin O, Sezer E, Kabukcuoglu F, Kilic AI, Sari AG, Cerman AA, Altunay IK. Presence of ulceration, but not high risk zone location, correlates with unfavorable histopathological subtype in facial basal cell carcinoma. Int J Clin Exp Pathol. 2015;8:15448-15453. [PubMed] |
| 11. | Mahajan S, Kalaivani M, Sethuraman G, Khaitan BK, Verma KK, Gupta S. A retrospective comparative study of outcome with surgical excision and repair versus nonsurgical and ablative treatments for basal cell carcinoma. Indian J Dermatol Venereol Leprol. 2021;87:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Kasumagic-Halilovic E, Hasic M, Ovcina-Kurtovic N. A Clinical Study of Basal Cell Carcinoma. Med Arch. 2019;73:394-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Kavoussi H, Ebrahimi A, Rezaei M, Najafi F, Zarpoosh M, Kavoussi R. Comparison of Demographic and Clinicopathological Characteristics of Basal Cell Carcinoma on the Nose and Other Sites of the Face: A Cross-Sectional Study. Iran J Otorhinolaryngol. 2021;33:257-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | George RM, Nazeer M, Criton S, Abraham UM, Francis A. Clinicopathological analysis of basal cell carcinoma–A retrospective study. J Ski Sex Transm Dis. 2021;3:51-55.. [DOI] [Full Text] |
| 15. | Kim ES, Yang CE, Chung YK. Does reduction of the oncologic safety margin for facial basal cell carcinoma result in higher recurrence rates? Arch Craniofac Surg. 2021;22:135-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Wei Q, Matanoski GM, Farmer ER, Hedayati MA, Grossman L. DNA repair and aging in basal cell carcinoma: a molecular epidemiology study. Proc Natl Acad Sci U S A. 1993;90:1614-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 275] [Cited by in RCA: 255] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 17. | Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166:1069-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1436] [Cited by in RCA: 1265] [Article Influence: 97.3] [Reference Citation Analysis (0)] |
| 18. | Sarma DP, Olson D, Olivella J, Harbert T, Wang B, Ortman S. Clear cell Basal cell carcinoma. Patholog Res Int. 2011;2011:386921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Warner CL, Cockerell CJ. The new seventh edition American Joint Committee on Cancer staging of cutaneous non-melanoma skin cancer: a critical review. Am J Clin Dermatol. 2011;12:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Ammasaigoundan V, Shariff VNSA, Ramesh A. Basal cell carcinoma-a prospective clinico epidemiological and pathological study. Int J Res Med Sci. 2017;5:2712-2717.. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Bath-Hextall F, Leonardi-Bee J, Smith C, Meal A, Hubbard R. Trends in incidence of skin basal cell carcinoma. Additional evidence from a UK primary care database study. Int J Cancer. 2007;121:2105-2108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 150] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 22. | Fellner C. Vismodegib (erivedge) for advanced Basal cell carcinoma. P T. 2012;37:670-682. [PubMed] |
| 23. | Rieger KE, Linos E, Egbert BM, Swetter SM. Recurrence rates associated with incompletely excised low-risk nonmelanoma skin cancer. J Cutan Pathol. 2010;37:59-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Khan L, Breen D, Zhang L, Balogh J, Czarnota G, Lee J, Tsao MN, Barnes EA. Predictors of recurrence after radiotherapy for non-melanoma skin cancer. Curr Oncol. 2014;21:e326-e329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Quazi SJ, Aslam N, Saleem H, Rahman J, Khan S. Surgical Margin of Excision in Basal Cell Carcinoma: A Systematic Review of Literature. Cureus. 2020;12:e9211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 26. | McKenzie CA, Chen AC, Choy B, Fernández-Peñas P, Damian DL, Scolyer RA. Classification of high risk basal cell carcinoma subtypes: experience of the ONTRAC study with proposed definitions and guidelines for pathological reporting. Pathology. 2016;48:395-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |