Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1049
Peer-review started: November 26, 2022
First decision: December 26, 2022
Revised: January 6, 2023
Accepted: January 19, 2023
Article in press: January 19, 2023
Published online: February 16, 2023
Processing time: 79 Days and 23.2 Hours
Hepatic colon carcinoma invading the duodenum is not common in clinical pra
To discuss the efficacy and safety of duodenum-jejunum Roux-en-Y anastomosis for the treatment of hepatic colon carcinoma invading the duodenum.
From 2016 to 2020, 11 patients from Panzhihua Central Hospital diagnosed with hepatic colon carcinoma were enrolled in this study. Clinical and therapeutic effects and prognostic indicators were retrospectively analyzed to determine the efficacy and safety of our surgical procedures. All patients underwent radical resection of right colon cancer combined with duodenum-jejunum Roux-en-Y anastomosis.
The median tumor size was 65 mm (r50-90). Major complications (Clavien-DindoI-II) occurred in 3 patients (27.3%); the average length of hospital stay was 18.09 ± 4.21 d; and only 1 patient (9.1%) was readmitted during the 1st mo after the surgery. The 30-d mortality rate was 0%. After a median follow-up of 41 m (r7-58), the disease-free survival at 1, 2, and 3 years was 90.9%, 90.9% and 75.8%, respectively; the overall survival at 1, 2, and 3 years was 90.9%.
In selected patients, radical resection of right colon cancer combined with duodenum-jejunum Roux-en-Y anastomosis is clinically effective, and the complications are manageable. The surgical procedure also has an acceptable morbidity rate and mid-term survival.
Core Tip: In summary, radical right hemicolectomy and duodenum-jejunum Roux-en-Y anastomosis are feasible and safe in selected patients with colorectal carcinoma complicated with duodenal invasion, with a low incidence of postoperative complications and a good prognosis for tumor treatment. We still need larger prospective studies with longer follow-up to confirm these preliminary findings.
- Citation: Liu PG, Feng PF, Chen XF. Right hemicolectomy combined with duodenum-jejunum Roux-en-Y anastomosis for hepatic colon carcinoma invading the duodenum: A single-center case series. World J Clin Cases 2023; 11(5): 1049-1057
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1049.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1049
Colorectal cancer (CRC) is one of the most common cancers worldwide and is the fifth leading cause of cancer incidence and mortality[1,2]. The prevalence of CRC is increasing globally[3], and the mortality rate of patients with advanced CRC is high[4,5]. CRC survival is significantly affected by the location, stage, and size of the cancer. Adjacent organ invasion is found in 5%-24% of CRC patients[6,7].
CRC, especially tumors near the hepatic flexure of the colon, frequently infiltrates the lower section of the descending duodenum and horizontal duodenum[8]. Hepatic colon carcinoma invading the duodenum is not common in clinical practice, and it is difficult to treat surgically. The main reason is the relatively high risk of surgery and the obviously high probability of complications, including severe complications (e.g., duodenal leakage). Due to the complexity and difficulty of surgical treatment, some surgeons tend to believe that there is no chance of cure. In this case, they give up the treatment of duodenal lesions and perform palliative right-side colon resection, which affects these patients’ 3- and 5-year survival rates[9]. According to different degrees of hepatic colon carcinoma invading the duodenum, active and reasonable surgical method formulas and correct treatment of duodenal defects will be used to help improve the condition or reduce postoperative complications.
Eleven patients with cancers of the hepatic flexure of the colon invading the duodenum were treated with duodenum-jejunum Roux-en-Y anastomosis in our hospital. In this retrospective study, our aim was to evaluate the effect of duodenal-jejunal Roux-en-Y anastomosis on the invasion of the duodenum by hepatic colon carcinoma and to provide a reference for the clinical promotion of this technique.
According to the PROCESS guidelines[10], a retrospective analysis was performed based on a single-center prospective case series. From May 2016 to June 2020, 11 patients were preoperatively diagnosed with colonic hepatic curl carcinoma with duodenal invasion at Panzhihua Central Hospital (Panzhihua, China). Before the operation, the hospital's gastrointestinal surgery specialists, internal medicine specialists, pathologists, radiologists, and imaging experts participated in the evaluation of the patient. The patients had undergone right semicolon carcinoma radical resection and duodenal-jejunal Roux-EN-Y anastomosis in the General Surgery Department of our hospital. None of them received neoadjuvant chemotherapy intervention prior to surgery. Surgeon Pei-Gen Liu, deputy chief physician, has completed laparotomy and minimally invasive laparoscopic surgery for more than 500 cases of CRC. He has rich experience in combined viscerectomy for locally advanced CRC and a profound understanding of membrane anatomy. He is quite accomplished in protecting patients’ sexual function and urination function when performing rectal cancer surgery. The surgeries were performed with the full advice and assistance of a multidisciplinary team. This study was approved by the ethics committee of Panzhihua Central Hospital (No. 20160001).
The following information of the patients was collected in detail: demographic aspects of the patients, American Society of Anesthesiologists (ASA) scores, duration of surgery, intraoperative blood loss, perioperative complications, pathological staging, and calculated overall survival and disease-free survival (DFS). Surgical risk was classified according to the ASA classification. Complications were classified according to the Clavien-Dindo classification[11]. The histopathological staging was recorded according to the tumor, nodes, metastases classification (American Joint Committee on Cancer 8th Edition for Cancer Staging).
Postoperatively, all patients were reevaluated by an oncologist to determine whether adjuvant therapy would be used. Five patients were in fair condition and underwent adjuvant chemotherapy (CAPOX, 12 wk), another two patients were not eligible for chemotherapy due to their cachexia, and four elderly patients in their 70 s gave up chemotherapy due to their elderly family members.
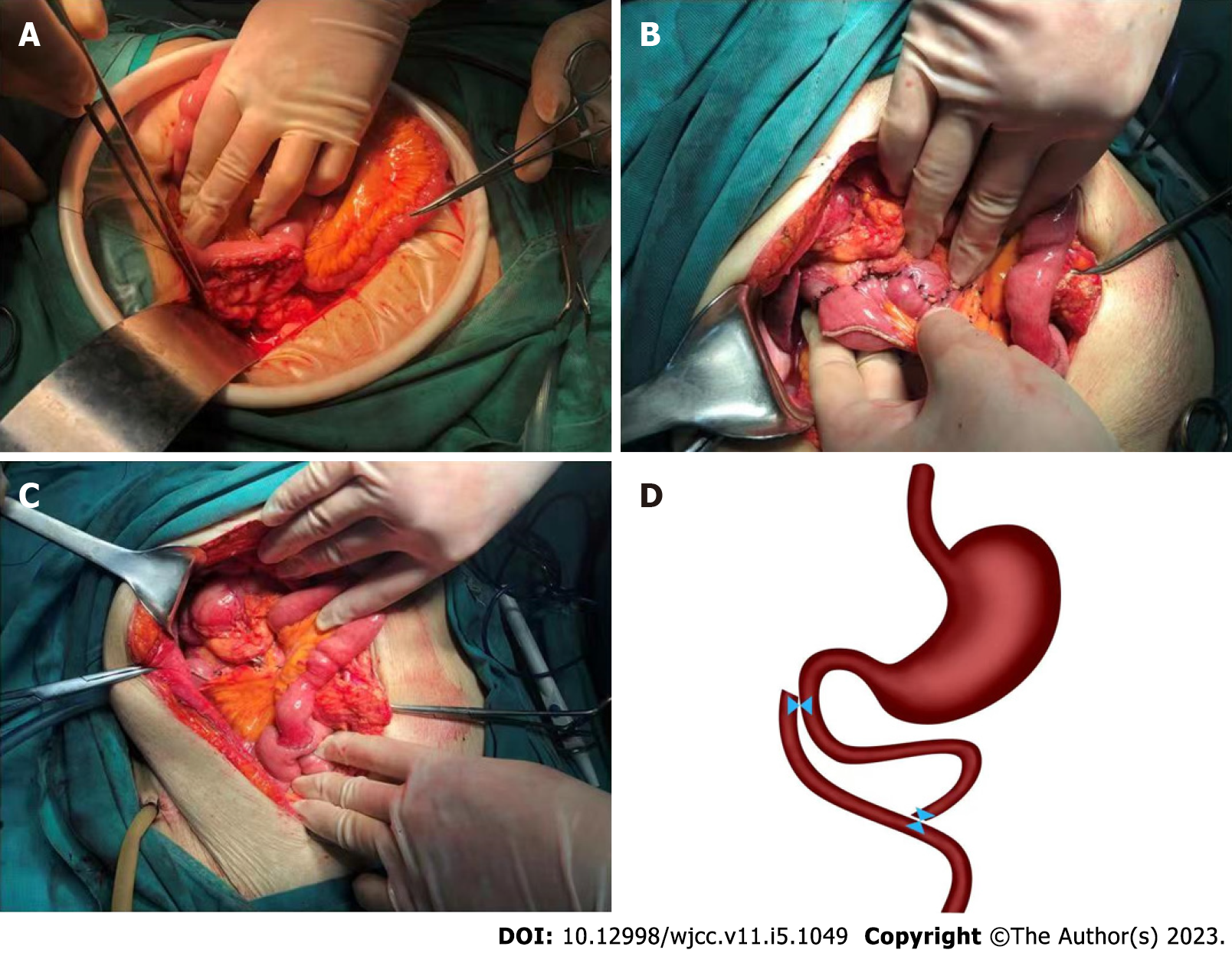
Once anesthetized, the patient was placed in the supine position. The operation was performed from a midline incision in the abdomen. First, whether the tumor had spread throughout the abdominal cavity was carefully determined. When the tumor had metastasized, we either abandoned radical surgery or continued the surgery. On the premise of no tumor metastasis, it was very important to explore the relationship between the tumor and its surroundings. Since the tumor only invaded part of the intestinal wall of the duodenum, it could be indicated that the tumor might be radically removed. In this case, we performed complete radical surgery. Radical surgery for right colon cancer was carried out according to the D3 standardization. The tumor and the surrounding 1 cm normal intestinal wall were resected at the site of duodenal invasion. In the upper part of the jejunum (20 cm from the ligament of flexion), a linear cutting stapling device was used to close the severed jejunum and the opening of the distal jejunum sidewall (the size of the opening was equivalent to the wound surface after duodenal wall tumor resection). A 3-0 absorbable suture was used to suture the duodenal wound and the jejunum opening (side-to-side anastomosis), and an interrupted suture technique was used for the plasma muscle layer to strengthen the anastomosis. The opening of the sidewall of the small intestine measuring approximately 40 cm at the distal end of the duodenal-jejunal anastomosis was used to complete the anastomosis with the proximal jejunum. The surgical technique is shown in Figure 1.
Quantitative variables were described with percentages. The median and range or the mean and standard deviation were used to calculate some of the quantitative variables. The Kaplan–Meier method was used to estimate patient survival. DFS was defined as the time from the date of surgical intervention to the date of recurrence. Statistical analyses were performed with SPSS20.0.
Eleven patients with hepatic colon carcinoma invading the duodenum underwent duodenum-jejunum Roux-en-Y anastomosis from May 2016 to June 2020. The demographics and general characteristics of the patients are shown in Table 1. The median age of the patients was 68 years (range: 34-74 years), and 5 (45.5%) patients were male. The median body mass index was 18 kg/m2 (range: 14.3-23). Two patients were considered to be ASA I (18.2%), and 9 were considered ASA II (81.8%). The performance status of 8 patients was assessed as electrocorticography 1 (72.7%). Ten (90.9%) patients had carcinoembryonic antigen > 5 ng/mL. The median tumor size was 65 mm (range: 50-90 mm). Three (27.3%) patients had T4bN1 disease, and two (18.2%) had T4bN2 disease.
The perioperative and postoperative results are shown in Table 2. The operative time was 241.36 ± 31.23 min, and the operative blood loss was 190.91 ± 59.07 mL. Three patients (27.3%) presented with complications. Incisional infection (Clavien-Dindo classification I) was found in 2 (18.2%) patients, and lymphatic leak (Clavien-Dindo classification II) was found in 1 (9.1%) patient. The times to the first bowel movement and resumption of a regular diet were 3.45 ± 1.04 and 7.55 ± 1.21 d, respectively. The postoperative hospital stay was 18.09 ± 4.21 d. None of the patients died during the first 30 postoperative days. Only 1 (9.1%) patient was hospitalized again within 30 d after surgery.
| Parameter | Value |
| Operative timea in min | 241.36 ± 31.23 |
| Blood lossa in mL | 190.91 ± 59.07 |
| Perioperative complications by Clavien-Dindo classification | 3 (27.3) |
| I | 2 (18.2) incision infection |
| II | 1 (9.1) lymphatic leak |
| III | 0 |
| IV | 0 |
| V | 0 |
| Time to first bowel movementa | 3.45 ± 1.04 |
| Time to resumption of regular dieta | 7.55 ± 1.21 |
| Hospital staya | 18.09 ± 4.21 |
| 30-d mortality | 0 |
| 30-d readmission | 1 (9.1) |
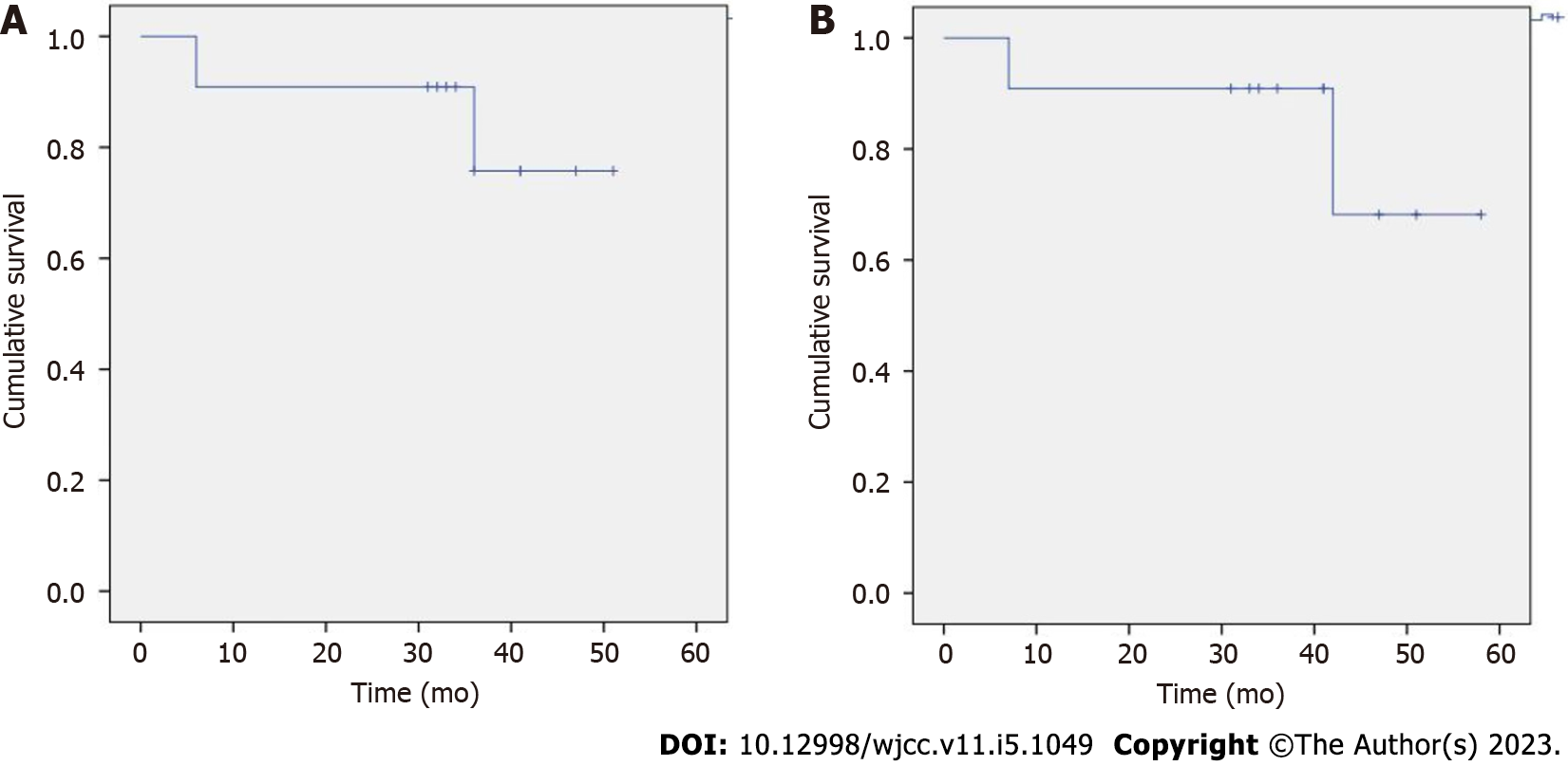
The patients were followed up, and the short- and medium-term outcomes are shown in Table 3. The median follow-up was 41 mo (range: 7-58). Five (45.5%) patients received chemotherapy after surgery, four (36.4%) received a complete course of chemotherapy, and treatment was discontinued in one patient due to intolerance. Progression was observed in 3 (27.3%) patients, with a median time to recurrence of 32 mo (r6-36). The recurrence sites included the lymph nodes (1 patient), liver (1 patient) and peritoneum (1 patient). During the follow-up period, 2 (18.2%) patients died from abdominal or liver metastases. The 1-, 2- and 3-year DFS rates were 90.9%, 90.9% and 75.8%, respectively. In addition, the 1-, 2- and 3-year overall survival rates were all 90.9%.
| Parameter | Value |
| Follow-upa in mo | 41 (r7-58) |
| Adjuvant chemotherapy | 5 (45.5) |
| Completed chemotherapy | 4 (36.4) |
| Recurrence | 3 (27.3) |
| Time to recurrencea in mo | 32 (r6-36) |
| Recurrence sites | |
| Lymph node | 1 (9.1) |
| Liver | 1 (9.1) |
| Peritoneum | 1 (9.1) |
| Disease-free survival | |
| 1-yr | 90.9% |
| 2-yr | 90.9% |
| 3-yr | 75.8% |
| Overall survival | |
| 1-yr | 90.9% |
| 2-yr | 90.9% |
| 3-yr | 90.9% |
| Deaths | 2 (18.2) |
The DFS rates at 1, 2 and 3 years were 90.9%, 90.9% and 75.8%, respectively (Figure 2A). Patients with recurrent tumors cannot be treated surgically. Two deaths occurred during follow-up, both of which were due to recurrent tumors. The overall survival rates at 1, 2 and 3 years were all 90.9% (Figure 2B).
CRC, a common malignant tumor of the digestive tract, is a serious threat to human health worldwide. According to China's cancer statistics in 2015, the incidence and mortality of CRC ranked fifth among all malignant tumors. Data show that the number of new cases of CRC in China that involved male patients was 376300, while 160600 involved female patients. Additionally, 191000 patients died of CRC, including 111000 males and 80000 females[12]. The incidence of CRC in developed countries such as the United States has shown a significant decline, but it has shown an upward trend in China[13]. Epidemiological results show that compared with left colon cancer, right colon cancer has a lower 5-year survival rate and a shorter average survival time[14]. The main reason is that radical resection of the right colon is generally believed to be more complicated than that of the left colon, radical resection is more difficult to achieve, and the recurrence and metastasis rates after radical resection are relatively high.
Hepatic colon carcinoma is considered right colon cancer, with an incidence rate of 1.4% to 6.0% among the colon cancer cases[15]. The incidence of colon cancer invading adjacent organs is approximately 23%. Once colon cancer invades the serosal membrane, it can directly infiltrate and metastasize to the surrounding organs, and this occurs especially with hepatic colon carcinoma. Due to the specificity of the anatomical position, the colonic liver curve and the duodenum are located in the retroperitoneal space at the same time, and the adjacent relationship is close. No barrier exists between the two. The first organ invaded is the duodenum. Severe cases can lead to duodenal fistula, which can cause difficulties during surgical treatment. Hepatic colon carcinoma does not commonly invade the duodenum in clinical practice. Originally, when hepatic colon carcinoma invaded the duodenum, the opportunity for radical treatment was believed to be lost, and palliative treatment was then given. Currently, surgery is the first choice for the treatment of hepatic colon carcinoma invading the duodenum. The choice of surgical method has a decisive influence on patient prognosis.
Certain controversy exists regarding the choice of surgical procedures for hepatic colon carcinoma invading the duodenum. Some researchers believe that to ensure radical cure of the tumor, right hemicolectomy and pancreaticoduodenectomy should be performed at the same time once colon cancer invades the duodenum, regardless of the degree of invasion. However, this operation is likely to cause greater trauma, increase blood loss, and produce a large number of anastomoses. The operation is difficult, and most patients cannot tolerate the procedure[16], resulting in certain limitations to its promotion. Based on extensive research, as long as the tumor does not invade the pancreas and is more than 2 cm away from the duodenal papilla, pancreaticoduodenectomy is believed to be unnecessary. Radical treatment of tumors can also be achieved by resection of the right colon and duodenal lesions[17]. The blood supply of the duodenum is poor. In addition, a large amount of digestive juice passes through the duodenum, resulting in a high probability of duodenal leakage after surgery. To prevent the occurrence of anastomotic leakage, low tension on the anastomosis must be maximally ensured while avoiding stenosis. In addition, the occurrence of intestinal stenosis should be avoided. After resection of hepatic colon carcinoma invading the duodenum, conventional treatment of the duodenal defect entails a lateral intermittent suture for closure or fungus-like tube placement at the end of surgery for duodenal fistulas and according to the size of the defect[18]. However, these treatments do not solve the problems of local tension and effective diversion of digestive juice, and the risk of postoperative leakage is still high.
To solve the above problems, we performed duodenal-jejunal Roux-en-Y anastomosis after radical resection of right colon cancer and achieved good clinical results. Roux-en-Y duodenum-jejunum anastomosis can reduce the amount of digestive juice and chyme flowing through the duodenum and reduce the occurrence of duodenal leakage.
In general, this operation had the following advantages. First, there is no intestinal stenosis. This operation employs the duodenal defect surface for anastomosis with the jejunum to avoid local suturing, which can cause intestinal stenosis. Gastric juice, bile and pancreatic juice can move along the intestinal tract to the distal small intestine through the duodenal-jejunal anastomosis and jejunal-jejunal anastomosis. Second, there was no tension: the duodenum and jejunum were anastomosed, and the mesentery was free. After anastomosis, the local anastomosis can be completely tension-free. Third, regarding early food intake, any duodenal leakage caused by eating is not a concern. The 11 patients in this article started eating normally approximately 7 d after the operation, and no significant increase in abdominal drainage after eating was observed. In addition, because a duodenal fistula was not created, the patients’ pain was markedly reduced, and their quality of life was improved. Fourth, the difficulty of the operation remains unchanged, and the patient's prognosis is unaffected. Duodenal-jejunal Roux-en-Y anastomosis is simpler than repair of the pedicled terminal ileum patch, and the surgical effect is accurate. At the same time, the occurrence of perioperative complications is reduced. Only 2 patients had a mild incisional infection, 1 patient had lymphatic leakage, and all recovered spontaneously. The 3-year follow-up survival rate was 90.9%, and the 3-year DFS rate was 75.8%. The long-term efficacy requires further observation.
The comprehensive treatment model of radical surgery and adjuvant chemotherapy has increased the 5-year survival rate of stage Ⅱ-Ⅲ colon cancer by 15%-20%[19,20]. The current CAPOX regimen (capecitabine + oxaliplatin) is an internationally recognized standard postoperative chemotherapy regimen for stage III CRC. In recent years, oxaliplatin-based adjuvant chemotherapy has been demonstrated to effectively improve the survival rate of patients, but its peripheral toxicity cannot be ignored[21]. Of the 11 patients in this manuscript, 5 received postoperative chemotherapy according to the CAPOX regimen, and the remaining patients did not undergo chemotherapy due to intolerance. One patient discontinued treatment after two courses of chemotherapy due to a severe chemotherapy reaction, and the remaining 4 patients were able to tolerate it. To date, none of the patients who received postoperative chemotherapy have had tumor recurrence or metastasis. This study showed that the 3-year DFS rate of patients was 75.8%, suggesting that postoperative chemotherapy may effectively improve the DFS rate of patients. Postoperative chemotherapy is recommended when the patient's physical condition permits.
This study had some limitations. First, our study was retrospective, and the number of patients was limited. Second, our research did not have a comparative group. Third, once anastomotic fistula occurs, drainage must be maintained, and the healing time for patients is usually long, which complicates resolution of the enteral nutrition problem. In addition, the median follow-up was only 41 mo, which did not allow us to report long-term outcomes.
In summary, radical right hemicolectomy and duodenum-jejunum Roux-en-Y anastomosis are feasible and safe in selected patients with CRC complicated with duodenal invasion, and this technique has a low incidence of postoperative complications and a good prognosis for tumor treatment. We still need larger prospective studies with longer follow-up to confirm these preliminary findings.
Hepatic colon carcinoma invading the duodenum is not common in clinical practice. Surgical treatment of colonic hepatic cancer that invades the duodenum is difficult, and the surgical risk is high.
Surgical treatment of colonic hepatic cancer that invades the duodenum is difficult, and the surgical risk is high.
The aim of the study was to discuss the efficacy and safety of duodenum-jejunum Roux-en-Y anastomosis in the treatment of hepatic colon carcinoma invading the duodenum.
From 2016 to 2020, 11 patients from Panzhihua Central Hospital diagnosed with hepatic colon carcinoma were enrolled in this study. Clinical and therapeutic effects and prognostic indicators were retrospectively analyzed to determine the efficacy and safety of our surgical procedures. All patients underwent radical resection of right colon cancer combined with duodenum-jejunum Roux-en-Y anastomosis.
The median tumor size was 65 mm (r50-90). Major complications (Clavien-DindoI-II) occurred in 3 patients (27.3%); the average length of hospital stay was 18.09 ± 4.21 d; and only 1 patient (9.1%) was readmitted during the 1st mo after the surgery. The 30-d mortality rate was 0%.After a median follow-up of 41 m (r7-58), the disease-free survival at 1, 2, and 3 years was 90.9%,90.9% and 75.8%, respectively; the overall survival at 1, 2, and 3 years was 90.9%.
In selected patients, radical resection of right colon cancer combined with duodenum-jejunum Roux-en-Y anastomosis is clinically effective, and the complications are manageable. The surgical procedure also has an acceptable morbidity rate and mid-term survival.
Radical right hemicolectomy and duodenum-jejunum Roux-en-Y anastomosis are feasible and safe in selected patients with colorectal carcinoma complicated with duodenal invasion, and this technique has a low incidence of postoperative complications and a good prognosis for tumor treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Nur NM, Somalia; Yamashina T, Japan S-Editor: Liu JH L-Editor: Filipodia P-Editor: Liu JH
| 1. | Chen W, Zheng R, Zeng H, Zhang S, He J. Annual report on status of cancer in China, 2011. Chin J Cancer Res. 2015;27:2-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 374] [Reference Citation Analysis (0)] |
| 2. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55666] [Article Influence: 7952.3] [Reference Citation Analysis (132)] |
| 3. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13300] [Cited by in RCA: 15450] [Article Influence: 2575.0] [Reference Citation Analysis (2)] |
| 4. | Iguchi K, Mushiake H, Aoyama T, Suwa H, Yukawa N, Ota M, Rino Y, Kunisaki C, Endo I, Masuda M. Additional Surgical Resection After Endoscopic Resection for Patients With High-risk T1 Colorectal Cancer. In Vivo. 2019;33:1243-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Baran B, Mert Ozupek N, Yerli Tetik N, Acar E, Bekcioglu O, Baskin Y. Difference Between Left-Sided and Right-Sided Colorectal Cancer: A Focused Review of Literature. Gastroenterology Res. 2018;11:264-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 336] [Article Influence: 48.0] [Reference Citation Analysis (1)] |
| 6. | Zhang J, Leng JH, Qian HG, Qiu H, Wu JH, Liu BN, Li CP, Hao CY. En bloc pancreaticoduodenectomy and right colectomy in the treatment of locally advanced colon cancer. Dis Colon Rectum. 2013;56:874-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Kapoor S, Das B, Pal S, Sahni P, Chattopadhyay TK. En bloc resection of right-sided colonic adenocarcinoma with adjacent organ invasion. Int J Colorectal Dis. 2006;21:265-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Chen JB, Luo SC, Chen CC, Wu CC, Yen Y, Chang CH, Chen YA, P'eng FK. Colo-pancreaticoduodenectomy for locally advanced colon carcinoma-feasibility in patients presenting with acute abdomen. World J Emerg Surg. 2021;16:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Yang WL, Yan CQ, Zhang HG, Wang FJ, Ma YL. [Surgical treatment and prognosis of cancer of hepatic flexure of colon invading the duodenum in 65 patients]. Zhonghua Zhong Liu Za Zhi. 2009;31:873-876. [PubMed] |
| 10. | Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler AJ, Orgill DP; PROCESS Group. The PROCESS 2018 statement: Updating Consensus Preferred Reporting Of CasE Series in Surgery (PROCESS) guidelines. Int J Surg. 2018;60:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 411] [Article Influence: 58.7] [Reference Citation Analysis (0)] |
| 11. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24675] [Article Influence: 1175.0] [Reference Citation Analysis (0)] |
| 12. | Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11444] [Cited by in RCA: 13192] [Article Influence: 1465.8] [Reference Citation Analysis (3)] |
| 13. | Wang XS. Epidemiological characteristics and prevention and control strategies of colorectal cancer in China and American. Chin J Colorec Dis (Electronic Edition). 2019;8:1-5.. [DOI] [Full Text] |
| 14. | Murcia O, Juárez M, Hernández-Illán E, Egoavil C, Giner-Calabuig M, Rodríguez-Soler M, Jover R. Serrated colorectal cancer: Molecular classification, prognosis, and response to chemotherapy. World J Gastroenterol. 2016;22:3516-3530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Zeng ZY, Luo YF, Gui SY. Liver Colon Cancer Lymph Node Metastasis in Clinical Analysis. Med Inform. 2012;25:176-177. [RCA] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 16. | Cirocchi R, Partelli S, Castellani E, Renzi C, Parisi A, Noya G, Falconi M. Right hemicolectomy plus pancreaticoduodenectomy vs partial duodenectomy in treatment of locally advanced right colon cancer invading pancreas and/or only duodenum. Surg Oncol. 2014;23:92-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Saiura A, Yamamoto J, Ueno M, Koga R, Seki M, Kokudo N. Long-term survival in patients with locally advanced colon cancer after en bloc pancreaticoduodenectomy and colectomy. Dis Colon Rectum. 2008;51:1548-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Harris JW, Martin JT, Maynard EC, McGrath PC, Tzeng CW. Increased morbidity and mortality of a concomitant colectomy during a pancreaticoduodenectomy: an NSQIP propensity-score matched analysis. HPB (Oxford). 2015;17:846-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | André T, Boni C, Navarro M, Tabernero J, Hickish T, Topham C, Bonetti A, Clingan P, Bridgewater J, Rivera F, de Gramont A. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol. 2009;27:3109-3116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1502] [Cited by in RCA: 1638] [Article Influence: 102.4] [Reference Citation Analysis (0)] |
| 20. | Adjuvant chemotherapy with oxaliplatin, in combination with fluorouracil plus leucovorin prolongs disease-free survival, but causes more adverse events in people with stage II or III colon cancer Abstracted from: Andre T, Boni C, Mounedji-Boudiaf L, et al. Multicenter international study of oxaliplatin/5-fluorouracil/leucovorin in the adjuvant treatment of colon cancer (MOSAIC) investigators. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med 2004; 350:2343-51. Cancer Treat Rev. 2004;30:711-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Allegra CJ, Yothers G, O'Connell MJ, Beart RW, Wozniak TF, Pitot HC, Shields AF, Landry JC, Ryan DP, Arora A, Evans LS, Bahary N, Soori G, Eakle JF, Robertson JM, Moore DF Jr, Mullane MR, Marchello BT, Ward PJ, Sharif S, Roh MS, Wolmark N. Neoadjuvant 5-FU or Capecitabine Plus Radiation With or Without Oxaliplatin in Rectal Cancer Patients: A Phase III Randomized Clinical Trial. J Natl Cancer Inst. 2015;107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 221] [Article Influence: 22.1] [Reference Citation Analysis (0)] |