Published online Dec 16, 2023. doi: 10.12998/wjcc.v11.i35.8310
Peer-review started: November 10, 2023
First decision: November 22, 2023
Revised: December 1, 2023
Accepted: December 6, 2023
Article in press: December 6, 2023
Published online: December 16, 2023
Processing time: 34 Days and 2.1 Hours
There are many available treatment options for keloid; however, single treatments are usually less effective. Therefore, more scientifically rational and effective com
To explore the efficacy and safety of surgical resection and ultra-reduced tension suture combined with superficial radiation as keloid treatment.
Fifteen keloid patients admitted to Qingdao Eighth People's Hospital from June 2020 to January 2022 were enrolled in this retrospective analysis. All patients underwent a comprehensive treatment approach comprising surgical resection, ultra-reduced tension suture incision, and superficial radiation therapy within 24 h postoperatively. The modified Vancouver Scar Scale (mVSS) and Patient and Observer Scar Assessment Scale (POSAS) were used to evaluate the treatment effect, whereas the efficacy, adverse effects, and recurrence rate were observed according to the 12-mo follow-up after treatment.
The mVSS and POSAS scores at 1 and 6 mo after combination treatment decreased compared to before treatment (P < 0.001), and the overall response rate was 93.3%. Only one case recurred, yielding a 6.7% recurrence rate. The incidence of local chromour sedimentation rate in 1–3 mo after radiotherapy was 33.3% (5 patients), all subsiding after 6–9 mo, without complications, such as delayed wound healing or dermatitis.
Surgical resection, super subtraction sutures, and superficial radiotherapy are treatment methods with short courses, low recurrence rates, and good safety profiles.
Core Tip: This study utilizes the most advanced ultra-reduced tension suture technology combined with superficial radiation therapy, known as "superficial radiation therapy," to reduce the recurrence rate of keloids. Only a few reports on this combination therapy method have been reported in China. Based on the pre-and post-treatment follow-up observations, comparison of photographs, and analysis of quantitative indicators in the scar evaluation table, this combination therapy can achieve a short treatment course, low recurrence rate, and good safety profile.
- Citation: Hu XY, Yang Q, Guan XY, Li JY, Wang LL, Li K, Zhang XT. Efficacy of surgical resection and ultra-reduced tension suture combined with superficial radiation in keloid treatment. World J Clin Cases 2023; 11(35): 8310-8319
- URL: https://www.wjgnet.com/2307-8960/full/v11/i35/8310.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i35.8310
Keloid is a special type of pathological scarring that regularly occurs in some body parts of normal people, such as the earlobe and auricle, double mandible, anterior chest, deltoid area of the upper arm, shoulder, upper back, pubic hair, and around the limb joints, in addition to other areas of patients predisposed to scarring. Although the etiology of this condition is complex, with various available treatments, including freezing, laser, injection, surgery, and radiotherapy, use of only a single treatment is associated with a higher recurrence rate[1]. Therefore, more scientific and effective com
In total, 15 patients with keloid who were admitted to Qingdao Eighth People's Hospital from June 2020 to January 2022 were included in this retrospective analysis. The inclusion criteria were as follows: (1) Patients fulfilling the diagnostic criteria for keloids[2]; (2) Less than 3 scars; (3) Scar width (vertical to the skin tension line) < 3 cm; (4) Disease course of < 5 years; (5) Secondary lesions; (6) Normal mental state; and (7) Examination and treatment and follow-up. The exclusion criteria were: (1) Age < 16 years; (2) Pregnant or lactating women; (3) History of severe heart, brain, and kidney systemic diseases; (4) Abnormal coagulation function; (5) History of treatment within 6 mo; (6) History of cutaneous malignancy; and (7) History of malnutrition and villainous disease.
Of the 15 patients aged 16–80 years, 3 were male and 12 female, respectively, with a mean age of 38.3 ± 21.7 years. The disease duration ranged from 1 to 40 years. Among seven cases of ear keloids (six and one cases were caused by ear perforation and perineural surgery, respectively), two were bilateral lesions. In two cases of facial keloids, one was acne-induced bilateral lesions, and the other was nevus-cutting surgery-induced. Additionally, in two cases of anterior thoracic keloid, one was acne-induced (frequent lesions), and the other was surgically induced (single lesion). Keloid scarring of limbs caused by local vaccination or surgery occurred in 4 cases. Furthermore, the keloid sizes were 0.6 cm × 0.6 cm × 0.4–9 cm × 4 cm × 3 cm, and scars had a tough texture, obvious bulge, and clear boundary, accompanied by different degrees of pain, itching, and other discomfort symptoms.
Surgery was performed under local infiltration anesthesia. In brief, the surgical area was disinfected three times with 0.5% iodophor, and a 1:200000 adrenaline lidocaine solution was locally injected around the keloid. After satisfactory anesthesia, the incision design and suture method were decided based on the keloid’s location and base condition.
Regarding extensive keloid base or a small amount of surrounding tissue, which cannot be directly stitched or affect symmetry after resection, the core, and most scar bumps were stripped from the skin and the edge was maintained at a width of 3–10 mm and the scar tissue flap at a thickness of 2 mm. Next, the most suitable type of slow absorption suture (5-0 to 6-0) was selected according to the scar’s location to perform subcutaneous tension suture 2 mm away from the skin margin, and the incision margin was slightly raised to ensure no tension. The skin was intermittently closed using a 6-0 monofiloral nylon thread, and the drainage strips were placed, as appropriate. Finally, erythromycin eye ointment is externally applied, followed by bandaging.
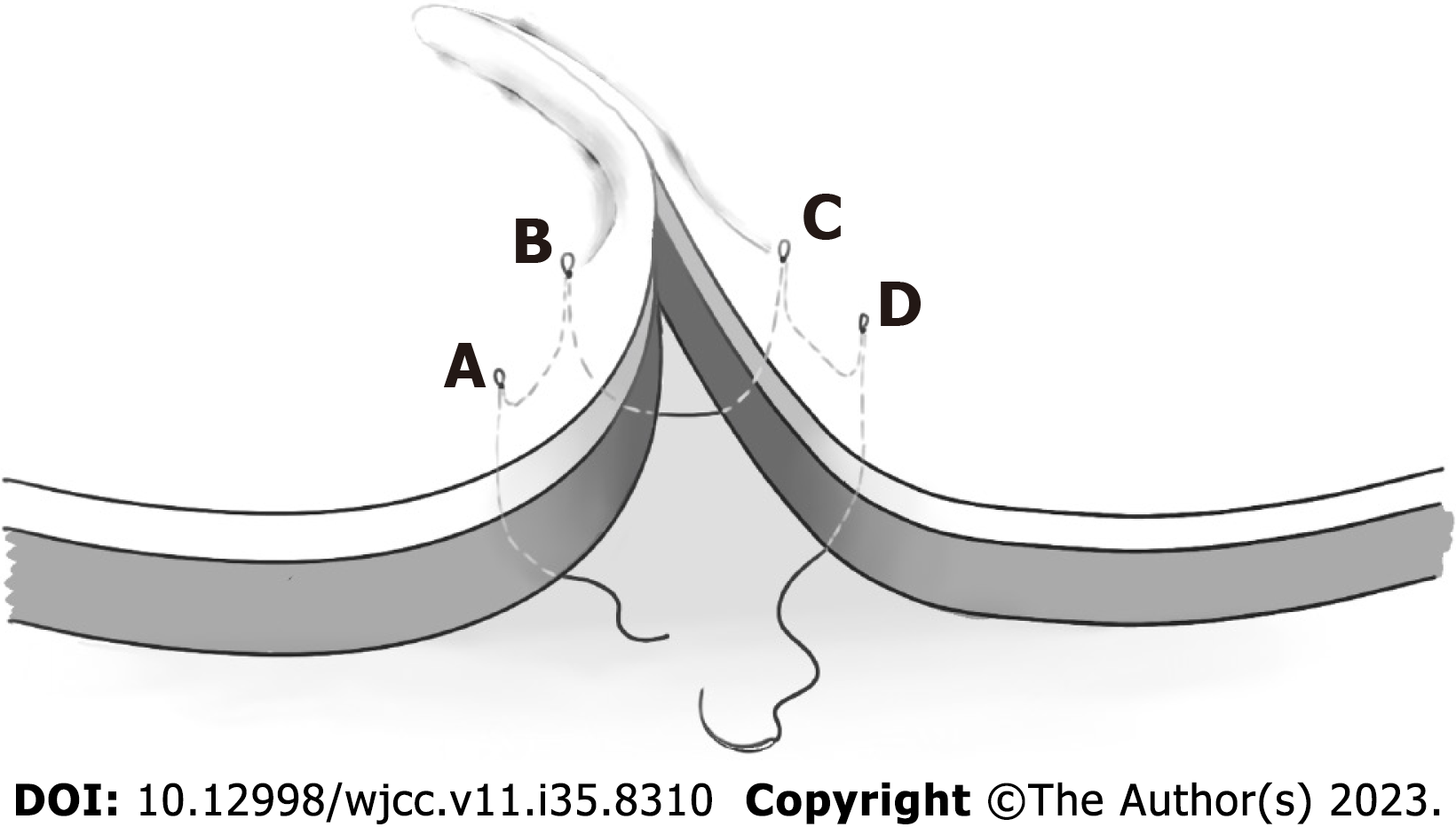
In contrast, for cases with a narrow keloid base or a large amount of surrounding tissue, direct stitching could be performed after evaluation, and the keloid edge could be completely removed. After the edge of the wound is fully detached, the ultra-reduced tension suture can be performed. Due to the large amount of surrounding tissue, the bulge of the incision margin becomes more obvious than that of the scar flap. The suture details included multiple symmetrical super-tension suture skin points designed at 1 cm from both sides of the incision, with a 1 cm ipsilateral spacing, and the outer skin points 0.5 cm above the horizontal edge of the wound. The adjacent puncture points on both sides of the incision were in one group, while the two adjacent groups were pairs. Subsequently, the appropriate type of slow absorption sutures (4-0 to 5-0) was selected according to the scar’s location, penetrating from one end to point A, passing through the epidermis, dermis, and subcutaneous tissue to the adjacent point B; the suture entered from point B, advanced through point C from the subcutaneous tissue to adjacent point D, and finally enters from point D to the incision site (Figure 1). When tying with the tail line, the skin tissue on both sides should be appropriately pushed to the middle, and the skin surface should be depressed at the puncture point. Additionally, the skin around the depression bulged, enabling the incision to be closely aligned, while the line knot becomes buried under the skin. The suture proceeded successively from one end of the incision to the other end. Subsequently, an intermittent subcutaneous suture was continually applied on the skin margin to smooth the wound. Finally, the skin was closed intermittently with a 6-0 single femoral nylon thread, and the drainage strips were placed as appropriate. External erythromycin eye ointment sterile dressings were applied on both sides of the wound to protect the raised incision, followed by bandaging.
The patient received the first superficial placement treatment within 24 h of surgery. The dressing was opened during treatment, and the wound was disinfected. Subsequent treatment depended on the drainage situation; those with drainage strips were pulled out or retained until the second postoperative day. Mold shielding protection was required outside the radiation area, and postoperative continuous radiotherapy was performed five times. The opening times were 5–7, 8–10, and 12–14 d for the face and ear, trunk, and limbs, respectively.
Daily care measures for scars in the surgical area, such as sun protection, avoiding spicy food, and no drinking, were implemented after the wound removal for 3–6 mo. Other anti-scar treatments, including silicone preparation and pressure, were not used.
Observational indicators
The observational indicators included the following: Scar score: Scars were evaluated preoperatively, 1 mo postoperatively, and 6 mo postoperatively using the following: (1) Modified Vancouver Assessment Scale (mVSS): This was achieved by palpating patients’ scar and assessing the severity of the scar using six color aspects, scar thickness, vascular distribution, softness, pain, and itching. The highest and lowest scores were 18 and 0, respectively. Higher and lower scores indicate heavier and lighter scars, respectively; and (2) The Patient and Observer Scar Assessment Scale was measured through self-assessment by the patient or their family members and observation by the attending physician. The Patient Scale (PSAS) (including pain level, pruritus, color, hardness, thickness, and irregularity) and Observer Scale (OSAS) (such as vascular distribution, color, thickness, roughness, softness, and surface area) were assigned separately, and an overall evaluation was determined. The maximum and lowest scores were 10 and 1 point, respectively; higher and lower scores indicated heavier and lighter scars, respectively.
Efficacy assessment: Based on contemporary scarring and following Liu Wenge’s standard for efficacy, this assessment was categorized according to the degree of improvement of symptoms and signs into cure, effective, and ineffective. (1) Cure: This assessment comprises disappeared itching pain and other symptoms; scar softening, not higher than the skin; continuous observation; and no recurrence after 6–12 mo; (2) Effective: This is characterized by significant improvement in itching pain and other symptoms, smaller size, or the severity changed to moderate, moderate to mild, and no reversal achieved 6–12 mo after treatment; (3) Ineffective: Slight or no improvement in itching pain and other symptoms, in
Adverse reactions and recurrence rate: Data were collected at follow-up visits in 1, 3, 6, and 12 mo after the combi
All data analyses were performed using the IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, NY, United States). Measuring data with mean ± SD, t-test; statistical significance was considered at P < 0.05.
Comparison of before combination therapy and 1 and 6 mo after the combination treatment (P < 0.001); Comparison of 1 and 6 mo after combination therapy (P < 0.001) (Table 1).
| Score | Example number | Before combination therapy | 1 mo after the combination treatment | 6 mo after the combination treatment | t value | P value |
| mVSS | 19 | 13.21 ± 2.20 | 4.68±2.41 | / | 15.12 | < 0.001 |
| mVSS | 19 | 13.21 ± 2.20 | / | 0.89 ± 2.11 | 24.27 | < 0.001 |
| mVSS | 19 | / | 4.68 ± 2.41 | 0.89 ± 2.11 | 7.69 | < 0.001 |
All 15 patients had significantly lower OSAS scores after the combination therapy than pre-treatment (P < 0.001) (Tables 2 and 3). The difference in scores was statistically significant (P < 0.01) (Table 4).
| Item | Before combination therapy | 1 mo after the combination treatment | t value | P value |
| Vascularity | 8.20 ± 1.15 | 2.67 ± 1.05 | 16.46 | < 0.001 |
| Color and luster | 7.87 ± 1.13 | 2.87 ± 1.60 | 10.92 | < 0.001 |
| Thickness | 7.73 ± 1.28 | 1.93 ± 0.88 | 19.59 | < 0.001 |
| Roughness | 7.13 ± 1.60 | 1.73 ± 0.80 | 13.92 | < 0.001 |
| Compliance | 7.87 ± 1.30 | 2.80 ± 1.08 | 13.65 | < 0.001 |
| Superficial area | 7.33 ± 1.50 | 2.20 ± 1.01 | 14.66 | < 0.001 |
| Overall evaluation | 7.53 ± 1.36 | 2.47 ± 0.83 | 17.84 | < 0.001 |
| Item | Before combination therapy | 6 mo after the combination treatment | t value | P value |
| Vascularity | 8.20 ± 1.15 | 1.27 ± 1.03 | 17 | < 0.001 |
| Color and luster | 7.87 ± 1.13 | 1.40 ± 1.06 | 18.47 | < 0.001 |
| Thickness | 7.73 ± 1.28 | 1.47 ± 1.30 | 20.87 | < 0.001 |
| Roughness | 7.13 ± 1.60 | 1.40 ± 1.06 | 13.67 | < 0.001 |
| Compliance | 7.87 ± 1.30 | 1.47 ± 1.30 | 19.09 | < 0.001 |
| Superficial area | 7.33 ± 1.50 | 1.27 ± 1.03 | 17.61 | < 0.001 |
| Overall evaluation | 7.53 ± 1.36 | 1.40 ± 1.06 | 22.41 | < 0.001 |
| Item | 1 mo after the combination treatment | 6 mo after the combination treatment | t value | P value |
| Vascularity | 2.67 ± 1.05 | 1.27 ± 1.03 | 10.69 | < 0.001 |
| Color and luster | 2.87 ± 1.60 | 1.40 ± 1.06 | 5.05 | < 0.001 |
| Thickness | 1.93 ± 0.88 | 1.47 ± 1.30 | 1.97 | 0.068 |
| Roughness | 1.73 ± 0.80 | 1.40 ± 1.06 | 1.58 | 0.136 |
| Compliance | 2.80 ± 1.08 | 1.47 ± 1.30 | 4.39 | 0.001 |
| Superficial area | 2.20 ± 1.01 | 1.27 ± 1.03 | 3.5 | 0.004 |
| Overall evaluation | 2.47 ± 0.83 | 1.40 ± 1.06 | 4.68 | < 0.001 |
The PSAS scores of the 15 patients were significantly lower after the combination therapy than before combination treatment (P < 0.05 and P < 0.01, Tables 5 and 6). The hardness and irregularity degree score decreased in 1 and 6 mo after the combination treatment, which were statistically significant (P < 0.05),the other scores were not significant (P > 0.05), but the overall evaluation was significant (P < 0.05), indicating that the effect 6 mo after the combination treatment was superior to that 1 mo post-treatment (Table 7).
| Item | Before combination therapy | 1 mo after the combination treatment | t value | P value |
| Degree of pain | 2.67 ± 2.09 | 1.27 ± 0.59 | 2.82 | 0.014 |
| Degree of itching | 6.27 ± 2.02 | 1.60 ± 0.74 | 9.26 | < 0.001 |
| Pigment | 7.87 ± 1.55 | 2.80 ± 1.66 | 10.95 | < 0.001 |
| Hardness | 8.20 ± 1.08 | 2.40 ± 0.83 | 17.02 | < 0.001 |
| Thickness | 7.73 ± 1.58 | 1.93 ± 1.16 | 12.08 | < 0.001 |
| Irregular degree | 7.33 ± 1.68 | 1.80 ± 1.15 | 14.23 | < 0.001 |
| Overall evaluation | 7.80 ± 1.21 | 2.27 ± 1.10 | 17.2 | < 0.001 |
| Item | Before combination therapy | 6 mo after the combination treatment | t value | P value |
| Degree of pain | 2.67 ± 2.09 | 1.13 ± 0.52 | 2.98 | 0.01 |
| Degree of itching | 6.27 ± 2.02 | 1.33 ± 1.05 | 10.02 | < 0.001 |
| Pigment | 7.87 ± 1.55 | 1.73 ± 1.39 | 15.3 | < 0.001 |
| Hardness | 8.20 ± 1.08 | 1.47 ± 1.06 | 20.38 | < 0.001 |
| Thickness | 7.73 ± 1.58 | 1.47 ± 1.30 | 14.19 | < 0.001 |
| Irregular degree | 7.33 ± 1.68 | 1.20 ± 0.78 | 15.78 | < 0.001 |
| Overall evaluation | 7.80 ± 1.21 | 1.53 ± 1.06 | 19.85 | < 0.001 |
| Item | 1 mo after the combination treatment | 6 mo after the combination treatment | t value | P value |
| Degree of pain | 1.27 ± 0.59 | 1.13 ± 0.52 | 1.47 | 0.164 |
| Degree of itching | 1.60 ± 0.74 | 1.33 ± 1.05 | 1.17 | 0.262 |
| Pigment | 2.80 ± 1.66 | 1.73 ± 1.39 | 2.98 | 0.1 |
| Hardness | 2.40 ± 0.83 | 1.47 ± 1.06 | 2.71 | 0.017 |
| Thickness | 1.93 ± 1.16 | 1.47 ± 1.30 | 1.45 | 0.169 |
| Irregular degree | 1.80 ± 1.15 | 1.20 ± 0.78 | 2.36 | 0.033 |
| Overall evaluation | 2.27 ± 1.10 | 1.53 ± 1.06 | 2.96 | 0.01 |
The surgical incision of 19 keloids in 15 patients healed initially without complications, such as hemorrhage, hematoma, infection, or delayed healing. The uplift area was generally completely flat 25–40 d after surgery. At 1 and 6 mo after treatment, scar vascular distribution, color, thickness, roughness, softness, and surface area all significantly improved according to the clinical observation evaluation; furthermore, the subjective feeling of itching or pain also decreased and the scar area texture became more soft. Further, there was no swelling hyperplasia or linear mature scars, and patients were satisfied with the appearance. The total effective rate was 94.74%.
Overall, 5 of 15 patients experienced hyperpigmentation in the wound area during radiotherapy; however, this hyperpigmentation was resolved 6–9 mo after the end of the radiotherapy. In one case, sagging and pulling caused by the large breast volume surrounding the wound resulted in the recurrence of a new scar postoperatively, which the injection treatment improved. The remaining case had no recurrence.
Case 1 was a female patient aged > 30 years who presented with a keloid on her left earlobe 3 years prior. This left eardrop keloid caused the formation of an ear hole, which gradually increased, with obvious itching that affected the appearance and function. The patient had a keloid before the left earlobe, dark red ellipsoid, 2 cm × 1.5 cm × 1 cm, hard keloid texture, obvious itching, and no local rupture (Figure 2A). The treatment plan included surgical resection, hy
Case 2 was a 70-year-old female patient who underwent total right breast resection and systemic chemotherapy for right breast cancer 7 years prior. Six months postoperatively, scar hyperplasia appeared at the medial half of the incision and gradually widened with pain. The patient sought treatment due to the concern about cancer recurrence in the scar area. During the physical examination, an oblique surgical scar was observed on the right side of the chest wall, approximately 21 cm long; the medial half was approximately 7 cm bulge and dark red; the widest part was approximately 1.4 cm; irregular edge, hard texture; a certain range of motion; obvious pain and itching; and no local rupture was observed (Figure 3A). The established treatment regimen comprising surgical resection plus radiotherapy was planned. The patient underwent scar resection under local anesthesia, and the bilateral tissue extension was legal (Figure 3B and C). Both intraoperative freezing and postoperative pathology suggested scar tissue. β-ray at 6 Mev was initiated 15 h postoperatively, and the target area was expanded 1.5 cm outside the surgical incision (Figure 3D) at a fractionated regimen of 3 Gy for 5 consecutive for a cumulative dose of 15 Gy was administered. The incision healed well 9 d postoperatively, but the color was obvious (Figure 3E). After 40 d, the area was flat, the local color subsidence subsided (Figure 3F), and the color subsidence had completely subsided by 6 mo. The scar was soft and flat without recurrence, with a satisfactory appearance at 12 mo postoperatively (Figure 3G).
Keloid scarring manifests as a colored mass raised above the normal skin surface. Keloid scars extend beyond the original damage range and exhibit persistent growth, with a hard texture and poor elasticity, frequently accompanied by itching or pain. Keloids are characterized by their resistance to therapy and high recurrence rate after treatment. The keloid formation mechanism has been shown to involve capillary angiogenesis[3], fibroblasts, myofibroblasts, various cytokines, and tissue collagen[4]; as such, a single treatment method cannot achieve significant and lasting outcomes. Previous clinical practice has shown that skin regions with higher tension, such as the chest and back of the shoulder are more prone to developing multiple keloids. When these skin regions experience insults, such as skin disease or wound, the greater tension stimulates collagen hyperplasia, and the consequences of collagen decomposition and synthesis eventually cause the formation of a keloid[5]. Keloids are conventionally treated with surgical resection; however, this procedure can impact the skin and cause tissue defects, thereby increasing the incision tension and leading to posto
In addition to meeting the requirements of wound malocclusion and valgus, ensuring a tension reduction effect is crucial. When the incision tension is large, the inner suture can easily cause local poor blood transportation and pig
In this study, the 15 patients had a medical history of > 1 year. When selecting surgical methods, decisions are based on the location and size of the keloid. This study combines the methods of LBD suture, which uses more non-absorbable thread in the internal suture, and Zhang's super-tension suture, which employs more absorbable barbed thread. Additionally, we investigated the influence of a non-absorbable line on keloid recurrence over time; considering the keloid location, the cost of the barbed line, and other factors, the inner suture was replaced with a slow absorption suture. Simultaneously, the personalized adjustment was made according to the characteristics of the keloid area to achieve the tension state of the incision of scar repair surgery. The authors’ experience involves preserving the aesthetics of the original lesion based on maximizing the resection region.
Using a scar valve simplifies the operation, making surgery easier, resulting in minimal alterations to the appearance and easy acceptance of this approach by the patients[12]. However, the keloid recurrence rate can reach as high as 45%–100%[12]. The retention of the scar flap is also one of the reasons for recurrence; therefore, under the condition of maintaining the ear appearance, the tension of the cutting margin should be significantly reduced to avoid the recurrence of keloids caused by large tension. Regarding the trunk, limbs, and other areas with a large amount of surrounding tissue, complete removal of the scar is achievable with direct suture, provided the edge of the wound remains fully free under the skin, enabling the tensioned suture to be performed.
Radiotherapy is an independent treatment modality for keloids and is commonly used as an adjunct to surgical treatment. Radiotherapy is used to eliminate fibroblasts and vascular endothelial cells in keloids, inhibit the production of collagen and the growth of naive fibroblasts, and block vascular regeneration, thereby directly and indirectly inhibiting keloid growth[13]. However, damage to the skin is a common side effect of radiotherapy which produces skin redness, itching, and even short-term pain. In the long term, radiotherapy can also cause excessive keratosis, skin tissue atrophy, abnormal skin pigment metabolism (pigmentation or depigmentation), and telangiectasia. Generally, low-energy electron rays (β-ray, 6–7 MeV) or X-rays (soft X-ray) are used as the radiotherapy modality, and two prophylactic radiotherapies can be performed within 24 h (and no more than 48 h) after keloid surgery, at a dose of 500–700 cGy/fraction.
In this study, radiotherapy was indicated for scars where the thickness of the lesion area was < 5 mm. All areas that underwent surgical treatment were considered eligible for radiotherapy. Additionally, the β-rays used can penetrate the skin surface and reach the deeper layer of the scar to inhibit its growth. Because the highest dose point of the electronic line is 15 mm below the skin, 80% of the depth dose exhibits rapid decay, and only 8.9% remains below the subcutaneous 30 mm, thereby providing good protection for the deep tissues and organs[14]. A special mold is available to protect the surrounding tissues outside the operation area during radiation to prevent damage to tissues outside the operation area. In our study, some of the patients experienced transient pigmentation in the irradiation area, which subsided from 6 to 12 mo postoperatively.
However, this study had some limitations which should be mentioned. First, the sample size was small due to the intention and choice of treatment and the long duration required for observing the treatment efficacy. Second, it was a single-center study. Therefore, in future studies, as this treatment plan evolves, more cases should be included in the observation, and the patients who prefer surgery and other methods, including injection treatment, should be used as control groups to seek a more scientific and effective comprehensive treatment plan for patients with keloid.
This study shows that the effect of surgical resection and ultra-reduced tension sutures combined with superficial radiotherapy is obvious; it has a short course, low recurrence rate, and good safety profile, and is easily accepted and preferred by patients, which is worthy of clinical promotion.
Keloids are a type of pathological scar whose appearance increases the psychological burden to patients; however, in more severe cases, keloids can affect the patient’s body function, disrupting their ability to lead a normal life and even isolating them from society. When treating keloids, a unimodal treatment strategy cannot achieve significant and lasting effects; therefore, the identification of more effective treatment methods is of great significance.
Surgical treatment is the modality that achieves the most visible improvement; however, because of the high posto
To investigate the optimal scheme for adjuvant surgical treatment of keloids and improve clinical efficacy and patient satisfaction.
The suture techniques employed in this investigation are the relatively new LBD suture and Zhang's suture. The ultra-reduced tension suture was placed once the subcutaneous surface of the wound edge was completely free. This study selected several radiotherapy strategies approved in the field to guarantee optimal results; however, all were performed within 24 h of surgery. The Scar Observation Scale of the patient and observer was completed concurrently during the same observation period, considering both patients' subjective experiences and professionals' objective indicators.
This study’s findings demonstrate that maximum resection, super tension suture, and superficial radiotherapy admi
Surgical treatment of keloid is the traditional therapeutic modality. This study uses a more cutting-edge tension suture technique. Surgical resection, super subtraction sutures, and superficial radiotherapy are treatment methods with short courses, low recurrence rates, and good safety profiles.
Future studies should observe more cases as treatment options mature. Simultaneously, patients who select surgery and other methods, such as botulinum toxin, platelet-rich plasma, and nano-fat injections, could be selected as other obser
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dermatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Romandini M, Italy S-Editor: Liu JH L-Editor: A P-Editor: Xu ZH
| 1. | Ekstein SF, Wyles SP, Moran SL, Meves A. Keloids: a review of therapeutic management. Int J Dermatol. 2021;60:661-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 127] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 2. | Gupta S, Sharma VK. Standard guidelines of care: Keloids and hypertrophic scars. Indian J Dermatol Venereol Leprol. 2011;77:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Sarkar A, Dewangan YK, Bain J, Rakshit P, Dhruw K, Basu SK, Saha JK, Majumdar BK. Effect of intense pulsed light on immature burn scars: A clinical study. Indian J Plast Surg. 2014;47:381-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Atiyeh BS. Nonsurgical management of hypertrophic scars: evidence-based therapies, standard practices, and emerging methods. Aesthetic Plast Surg. 2007;31:468-92; discussion 493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 170] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 5. | Ogawa R. Keloid and hypertrophic scarring may result from a mechanoreceptor or mechanosensitive nociceptor disorder. Med Hypotheses. 2008;71:493-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Ogawa R, Akaishi S, Huang C, Dohi T, Aoki M, Omori Y, Koike S, Kobe K, Akimoto M, Hyakusoku H. Clinical applications of basic research that shows reducing skin tension could prevent and treat abnormal scarring: the importance of fascial/subcutaneous tensile reduction sutures and flap surgery for keloid and hypertrophic scar reconstruction. J Nippon Med Sch. 2011;78:68-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 117] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Zhang X, Diao JS, Guo SZ, Han Y, Ai YF, Zeng XH, Li LW, Shu MG. Wedge-shaped excision and modified vertical mattress suture fully buried in a multilayered and tensioned wound closure. Aesthetic Plast Surg. 2009;33:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Wang AS, Kleinerman R, Armstrong AW, Fitzmaurice S, Pascucci A, Awasthi S, Ratnarathorn M, Sivamani R, King TH, Eisen DB. Set-back versus buried vertical mattress suturing: results of a randomized blinded trial. J Am Acad Dermatol. 2015;72:674-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Yang J, Kim KH, Song YJ, Kim SC, Sung N, Kim H, Lee DH. Cosmetic outcomes of cesarean section scar; subcuticular suture versus intradermal buried suture. Obstet Gynecol Sci. 2018;61:79-87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Zhang J, Liu X, Zheng M, Yin J, Xing W. Case Report: Dermoscopic, High-Frequency Ultrasound, Contrast-Enhanced Ultrasound Appearances and Special Treatment of a Patient With Syringoid Eccrine Carcinoma on the Chest. Front Oncol. 2021;11:717581. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Chen J, Zhang YX. [Clinical effect of Zhang's super tension-relieving suture for high-tension wound closure]. Zhonghua Shao Shang Za Zhi. 2020;36:339-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Ogawa R, Huang C, Akaishi S, Dohi T, Sugimoto A, Kuribayashi S, Miyashita T, Hyakusoku H. Analysis of surgical treatments for earlobe keloids: analysis of 174 lesions in 145 patients. Plast Reconstr Surg. 2013;132:818e-825e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Bijlard E, Verduijn GM, Harmeling JX, Dehnad H, Niessen FB, Meijer OWM, Mureau MAM. Optimal High-Dose-Rate Brachytherapy Fractionation Scheme After Keloid Excision: A Retrospective Multicenter Comparison of Recurrence Rates and Complications. Int J Radiat Oncol Biol Phys. 2018;100:679-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Bijlard E, Timman R, Verduijn GM, Niessen FB, Hovius SER, Mureau MAM. Intralesional cryotherapy versus excision with corticosteroid injections or brachytherapy for keloid treatment: Randomised controlled trials. J Plast Reconstr Aesthet Surg. 2018;71:847-856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |