Published online Sep 26, 2023. doi: 10.12998/wjcc.v11.i27.6653
Peer-review started: July 21, 2023
First decision: August 4, 2023
Revised: August 15, 2023
Accepted: August 31, 2023
Article in press: August 31, 2023
Published online: September 26, 2023
Processing time: 61 Days and 7.4 Hours
Neurofibromas are benign tumors of a neurogenic origin. If these tumors occur without any other signs of neurofibromatosis, they are classified as isolated neurofibromas. Neurofibromas in the oral cavity mostly occur within soft tissues, indicating that solitary intraosseous neurofibromas in the mandible are rare. Due to the absence of specific clinical manifestations, early diagnosis and treatment of these tumors are difficult to achieve.
A 37-year-old female patient visited our hospital due to numbness and swelling of the gums in the right lower molar area that had persisted for half a month. The patient’s overall condition and intraoral examination revealed no significant abnormalities. She was initially diagnosed with a cystic lesion in the right man
This case report discusses the key features that are useful for differentiating solitary intraosseous neurofibromas from other cystic lesions.
Core Tip: We present the case of a 37-year-old female with a solitary intraosseous neurofibroma in the right mandible, accompanied by tooth root resorption and local sensory abnormalities. Imaging revealed low-density unicysts with clear borders. The area affected by the inferior alveolar nerve canal was locally dilated, without displacement. A histological evaluation of the mass revealed spindle-shaped fibroblasts and fibroblast-like cell proliferation with a slight increase in nuclear size. Immunohistochemistry results showed positive staining for S100 and CD34 markers. Complete tumor resection and partial removal of the right inferior alveolar nerve were performed.
- Citation: Zhang Z, Hong X, Wang F, Ye X, Yao YD, Yin Y, Yang HY. Solitary intraosseous neurofibroma in the mandible mimicking a cystic lesion: A case report and review of literature. World J Clin Cases 2023; 11(27): 6653-6663
- URL: https://www.wjgnet.com/2307-8960/full/v11/i27/6653.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i27.6653
Neurofibromas are typically benign tumors that originat from the sheath of the peripheral nervous system. They can present as isolated lesions or as a part of neurofibromatosis type 1 (NF1), a systemic syndrome also known as von Recklinghausen disease[1]. NF1 is a common neurocutaneous disorder with an autosomal dominant inheritance pattern; however, solitary neurofibromas do not exhibit this pattern[2]. Neurofibromas occur predominantly in soft tissues and less frequently in bones. It is important to note that approximately 20%-60% of oral neurofibromas are associated with neurofibromatosis. They are commonly found in the tongue, buccal mucosa, and vestibular areas[3]. Solitary intraosseous neurofibromas of the head and neck are rare, with those in the posterior part of the mandible being the most prevalent site. The early diagnosis and treatment of neurofibromas can be challenging due to their lack of specific clinical manifestations. However, with the aid of imaging techniques, such as cone-beam computed tomography (CT) (CBCT), cystic lesions can be easily diagnosed, which can affect treatment plans. Timely local organizational biopsies are crucial for an accurate diagnosis, and confirmation can be obtained through pathological examination. This report describes a rare case of a solitary intraosseous neurofibroma in the right mandible accompanied by tooth root resorption and local sensory abnormalities.
A 37-year-old female patient visited our hospital with numbness and swelling of the gums in the right lower molar area that had persisted for half a month.
Fifteen days prior, the patient had visited a local clinic due to numbness and swelling of the gums in the right lower molar area. Oral panoramic radiography revealed low-density lesions at the root tip in the right mandibular molar area, specifically affecting the lower right second molar. Despite discovering the anomaly, the patient did not report any significant pain, bleeding in the lower right gum or teeth, or unusual odor in the mouth. Additionally, the patient denied experiencing any abnormal sensation in the lower right lip.
There was no significant medical history related to this illness.
The patient had no family history of hereditary diseases or malignant tumors.
The patient’s general health was satisfactory, and no anomalies were detected on the skin of the face or the rest of the body. The patient’s facial features were symmetrical, with no apparent swelling. No significant buccolingual bulge was observed in the right mandible, nor was there any palpable ping-pong-like sensation. The right mandibular molars exhibited second-degree loosening and discomfort upon percussion. Slight redness and swelling were noticed on the buccal side of the right lower posterior tooth’s gingiva, with no sinus, pus discharge, or bleeding. The patient reported symmetrical sensory acuity in both upper and lower lips.
The results of routine blood tests were as follows: Mean platelet volume: 8.7 fL (reference value: 9.0-13.0 fL); platelet distribution width: 8.8 fL (reference value: 9.0-17.0 fL).
CBCT revealed a hypodense image measuring approximately 4.7 cm × 2.3 cm × 1.6 cm in the body of the right mandible. A white bone line surrounding the lesion was observed, along with thinning of the cortical bone. The lesion affected the apex of the lower right second molar with evident root resorption. The apical lesion of the lower right first molar seemed isolated, while the lower right third molar was located outside the mass and buried within the bone. The affected area of the inferior alveolar nerve canal was locally dilated without displacement (Figure 1).
After comprehensive assessment of the clinical presentation, blood test results, imaging findings, and pathological examination, the patient was diagnosed with a solitary intraosseous neurofibroma of the right mandible.
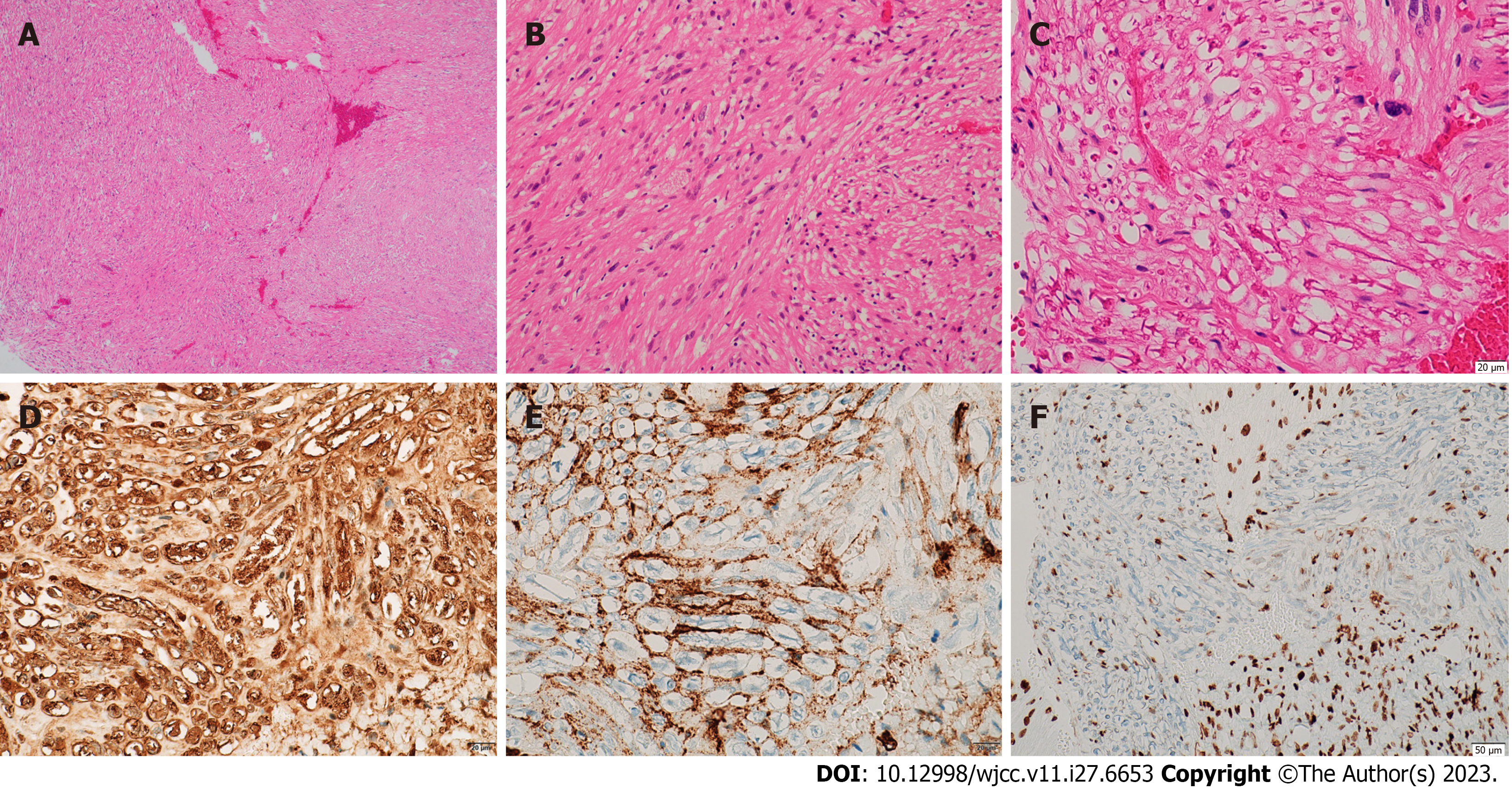
On September 7, 2022, we performed complete tumor resection, along with partial removal of the right inferior alveolar nerve and extraction of the lower right third molar. During surgery, the tumor appeared as a grayish-white solid and the main trunk of the inferior alveolar nerve was not visible. Microscopic examination revealed spindle-shaped fibroblasts and fibroblast-like cell proliferation, with a slight increase in nuclear size. The nuclei were short and spindle-shaped, the cytoplasm showed rich red staining, and axons were locally visible (Figure 2). Immunohistochemistry results showed positive staining for S100, CD34, and H3K27me3 (Figure 2) and negative staining for smooth muscle actin, neurofilaments protein, and epithelial membrane antigen (Supplementary Figure 1).
Nine months after the surgery, there were no signs of tumor recurrence. However, the patient developed numbness in the lower right lip, which had not improved at the time of writing this report.
Solitary neurofibromas are slow-growing benign tumors that are not encapsulated. In cases where patients do not exhibit other manifestations of neurofibromatosis, such as axillary freckling, iris hamartomas, or skeletal dysplasia, they are diagnosed with isolated neurofibromas. Neurofibromas of the oral cavity primarily originate from the mucosa. Bone involvement in neurofibromatosis is typically attributed to subperiosteal neurofibromas, which can cause bone erosion[4]. Solitary intraosseous neurofibromas are rare because the bone marrow space lacks nerve sheaths or myelinated nerves[5]. We have compiled the results from 38 studies on the subject, published since the discovery of solitary intraosseous mandibular neurofibromas (Table 1)[5-35]. The posterior part of the mandible is the most common location, with a higher incidence in females. The average age of presentation is 27.5 years[6]. The length and thickness of the inferior alveolar nerve bundles may contribute to the comparatively high frequency of this illness in the mandible[7].
| Ref. | Age (year)/sex | Site | Clinical features | Radiographic features | Root resorption | Size | Immunohistochemistry features | Surgical approach | Prognosis |
| Present case | 37/F | Body | Numbness and swelling of the gum in the right lower molar area | Unilocular expansile radiolucency involving the inferior alveolar nerve canal | Yes | 4.7 cm × 2.3 cm × 1.6 cm | Positive staining for S100, CD34, and H3K27me3,negative staining for SMA, NF, and EMA | Excision of the tumor and nerve | No recurrence observed nine months post-surgery |
| Kamalakaran et al[5] | 5/M | Body-ramus | Limited mouth opening and enlarged submandibular lymph nodes | Expansile lesion with a mixture of radiolucent and radiopaque components | No | 3.9 cm × 3.8 cm × 3.1 cm | Not reported | Segmental resection of the mandible | No recurrence observed one-year post-surgery |
| Sarkar et al[6] | 2.5/M | Body-ramus | Swelling in the posterior right part of the mandible. Displacement of deciduous teeth | Well-definedexpansile solid-cystic lesion with evidence of cortical erosion | No | 3.7 cm × 3.5 cm × 3.4 cm | S-100 multifocal and moderately positive, strong CD34 positivity EMA, cytokeratin, CD31, SMA, STAT-6, TLE-1, and HMB-45 negative MIB-1 index low | Preservation of the nerve while removing the mass | Not reported |
| Behrad et al[13] | 32/F | Body | Swelling and intermittent dull pain in the left mandible | Unilocular expansile radiolucency involving the inferior alveolar nerve canal | No | 3 cm × 1.5 cm × 2.4 cm | Not reported | Simple excision of the mass | Not reported |
| Iqbal et al[14] | 13/M | Body-angle | Swelling in the posterior area of the right mandible | Ill-defined radiolucency | No | 2.0 cm × 3.0 cm × 2.0 cm | S-100 positive | Simple excision of the mass | No recurrence |
| Inoue et al[15] | 27/M | Ramus to infratemporal fossa | Progressive numbness on the lower right jaw | A nonenhanced mass in the infratemporal region, with an enlarged inferior alveolar nerve canal and foramen ovale | No | Not reported | S-100 positive | Excision of the tumor and nerve | No recurrence |
| Narang et al[16] | 45/F | Left mandibular angle to right mental foramen | Swelling in the posterior area of the left mandible | The radiographic irregularity in the region of the inferior lacrimal canal | Yes | Not reported | S-100 positive, MIB-1 negative | Segmental resection of the mandible | Not reported |
| Fortier[17] | 70/F | Body | Osteolytic lesion of the right posterior mandible | The clear single-eyed translucent area. Involvement of the inferior alveolar nerve canal | No | Not reported | S-100 positive | Preservation of the nerve while removing the mass | No recurrence |
| Gujjar et al[18] | 28/F | Body | Swelling and intermittent dull pain in the left mandible | Uniform radiopacity. Involvement of the inferior alveolar nerve canal | No | 3.0 cm × 4.0 cm | S-100 positive | Segmental resection of the mandible | Not reported |
| Saravani et al[19] | 39/F | Body | Severe pain in the right posterior mandible | Relatively clear single-cyst projection shadow | No | Not reported | S-100 positive | Simple excision of the mass | No recurrence |
| Jangam et al[20] | 62/F | Right body-left body | The lower jaw is significantly swollen. Occasionally, there is severe pain | Radiographically transparent image with clear borders, accompanied by thinning of the lower boundary | Edentulous jaw | Not reported | S-100 positive | Segmental resection of the mandible. Repair using a free fibular graft | No recurrence |
| Deichler et al[21] | 14/M | Ramus | No clinical symptoms, discovered incidentally | Unilocular radiolucency | No | 4.0 cm × 1.5 cm × 0.5 cm | Tumor cells: Vimentin positive, neurospecific enolase (NSE) positive and anti S-100 negative. Residual nerve fibres: S-100 positive; NSE positive | Simple excision of the mass | Not reported |
| Tao et al[22] | 16/F | Ramus | Limited mouth opening, numbness in the lower left lip | Multilocular radiolucency with irregular edges | No | 3.5 cm × 2.0 cm | S-100 positive | Segmental resection of the mandible. Repair using a free iliac bone graft | Not reported |
| Vivek et al[7] | 39/F | Symphysis-parasymphysis | Spontaneous tooth loss, persistent tingling sensation in the lower lip | A relatively well-defined radiolucent area | No | Not reported | S-100 positive | Segmental resection of the mandible | No recurrence observed one-year post-surgery |
| Apostolidis et al8] | 67/F | Body-ramus | Abnormal sensation in the lower left lip | Involvement of the inferior alveolar nerve canal | No | 2.5 cm × 2 cm × 0.7 cm | Not reported | Excision of the tumor and nerve | No recurrence observed three-year post-surgery |
| Alatli et al[23] | 37/F | Body | Abnormal sensation in the lower right lip | No abnormalities detected | No | Diameter of 1.3 centimeters | Not reported | Excision of the tumor and nerve | No recurrence observed two years post-surgery |
| Ueda et al[24] | 37/M | Body | No clinical symptoms, discovered incidentally | Well-defined unilocular radiolucency. Involvement of the inferior alveolar nerve canal | No | Not reported | S-100 positive | Segmental resection of the mandible. Repair using a free scapular flap | No recurrence observed three years post-surgery |
| Papageorge et al[10] | 4.5/M | Ramus-infratemporal fossa | Expansile lesion in the right mandible. Limited mouth opening, chin deviated to the left | Well-defined unilocular radiolucency. Involvement of the inferior alveolar nerve canal | No | Not reported | S-100 protein and vimentin positive | Segmental resection of the mandible. Reconstruction using autologous rib cartilage graft | No recurrence |
| Weaver et al[25] | 22/F | Body | Swelling on the left side of the face | Well-defined unilocular radiolucency | No | 5.0 cm × 3.0 cm | S-100 positive | Excision of the tumor and nerve. | No recurrence observed six months post-surgery |
| Polak et al[26] | 60/M | Body | No clinical symptoms discovered incidentally. When palpated, a crackling sensation can be felt, similar to the sound of breaking eggshells | Unilocular radiolucency involving the mandibular canal | No | Not reported | S-100 and anti-Leu positive | Excision of the tumor and nerve | No recurrence observed six years post-surgery |
| Papadopoulos et al[27] | 15/M | Body | Swelling and mild pain in the left mandible | Unilocular radiolucency near mental foramen | No | 0.5 cm × 0.5 cm × 0.5 cm | Not reported | Excision of the tumor and nerve | No recurrence |
| Larsson et al[11] | 25/F | Body-ramus | No clinical symptoms, discovered incidentally | Well-defined large radiolucency. Involvement of the inferior alveolar nerve canal | No | 10 cm × 2.0 cm | Not reported | Excision of the tumor and nerve, with nerve end-to-end anastomosis | No recurrence observed two years post-surgery |
| Larsson et al[11] | 46/M | Body | Swelling and slow, intermittent pain in the left mandible | Rounded, slightly radiopaque, well-circumscribed radiolucency | No | Diameter of 1 cm | Not reported | Remove all visibly abnormal tissues within the bone | No recurrence observed five months post-surgery |
| Ellis et al[28] | 41/F | Body-ramus | Swelling in the right mandible | Poorly defined multilocular radiolucent lesion | No | Not reported | Not reported | Not reported | Not reported |
| Ellis et al[28] | 4/F | Body | A firm lump on the right mandible | Well demarcated radiolucent lesion. Involvement of the inferior alveolar nerve canal | No | 2.5 cm × 1.6 cm | Not reported | Not reported | No recurrence observed one-year post-surgery |
| Ellis et al[28] | 8/M | Body-angle | Not reported | Well demarcated radiolucent lesion with sclerotic borders | No | 6.0 cm × 4.0 cm | Not reported | Not reported | No recurrence observed one-year post-surgery |
| Ellis et al[28] | 23/F | Body-ramus | Swelling in the posterior area of the right mandible | Radiolucent-radiopaque lesion with indistinct borders | No | Not reported | Not reported | Not reported | Recurrence observed after 3 yr. Partial mandibulectomy performed |
| Ellis et al[28] | 4/M | Body | Swelling in the right mandible | Multilocular radiolucent lesion | No | Not reported | Not reported | Not reported | Not reported |
| Cundy and Matukas[29] | 55/F | Body-angle | Pain and swelling in the left mandible, accompanied by discomfort while chewing | Unilocular radiolucency | No | Not reported | Not reported | Segmental resection of the mandible. Repair using a free iliac bone graft | Not reported |
| Cassalia and Miller[30] | 16/F | Angle | No clinical symptoms, discovered incidentally | Multilocular radiolucency involving mandibular canal | No | Not reported | Not reported | Preservation of the nerve while removing the mass | No recurrence observed six months post-surgery |
| Sharawy and Springer[31] | 22/F | Body-angle | Intermittent numbness in the left mandible, with slight swelling on the cheek side | Multilocular expansile radiolucency | No | Not reported | Not reported | Excision of the tumor and nerve. | No recurrence observed thirteen months post-surgery |
| Gutman et al[32] | 5/F | Body | Painless swelling in the left mandible | Unilocular expansile radiolucency | No | 2 cm × 4 cm | Not reported | Excision of the tumor and nerve | No recurrence observed sixteen months post-surgery |
| Gohel et al[12] | 17/F | Body | A swollen lump on the gums of the lower right mandible | Osteolytic radiolucent lesion | No | 4 cm × 1 cm | Not reported | Not reported | Not reported |
| Johnson et al[9] | 34/F | Body | Abnormal sensation on the left side of the lower lip and tenderness in the lower left jaw during biting | Unilocular radiolucency | No | 2.5 cm × 1.5 cm | Not reported | Not reported | Skin pigmentation observed six months later, followed by local recurrence two years post-surgery |
| CORNELL and VARGAS[33] | 65/F | Body | Oral discomfort | Ill-defined unilocular lesion with unclear borders | Edentulous jaw | Not reported | Not reported | Excision of the tumor and nerve | No recurrence |
| BRUCE[34] | 36/M | Body | A swelling on the alveolar ridge of the edentulous lower left jaw | Well-defined radiolucency involving mandibular canal | No | 3 cm × 2 cm × 2 cm | Not reported | Not reported | Not reported |
| Blackwood and Lucas[35] | 41/M | Body | Swelling in the posterior area of the left mandible | Unilocular radiolucency | Yes | 2 cm × 1.5 cm ×1 cm | Not reported | Simple excision of the mass | Not reported |
In the early stages, solitary intraosseous neurofibromas may not cause any symptoms; however, as the lesions grow, they can lead to expansion of the mandibular cortex. This expansion may occur with or without destruction and can result in pain, anesthesia, or paresthesia[8]. Further invasion of surrounding tissues may lead to abnormalities that alter mouth opening. However, the clinical symptoms lack specificity. This is the third reported case of a solitary intraosseous neurofibroma in the mandible with tooth root resorption. Therefore, the early diagnosis of solitary intraosseous neurofibromas without obvious symptoms is difficult. In contrast to mandibular cystic lesions, which often manifest as local swelling, loose teeth, and discomfort during biting, our patient presented with local numbness of the gums in the posterior mandibular region. Our initial neglect led to a diagnostic bias. Performing pulp vitality tests on the teeth involved in the lesion can also help identify neurofibromas. It should be noted that the clinical manifestations of non-chief complaint diseases in the adjacent teeth may affect judgments regarding the nature of the tumor, highlighting the need for improved accuracy in the clinical judgment of the chief complaint.
The imaging characteristics of solitary intraosseous neurofibromas typically show low-density unicystic or multicystic images with clear or unclear borders that lack specificity. However, these images may be closely related to those of the mandibular nerve canal. We have compiled a list of mandibular diseases that can easily be mistaken for solitary intraosseous neurofibromas (Table 2). The radiological appearance of this patient closely resembled periapical cysts, unicystic ameloblastoma (UA), and odontogenic keratocysts. Periapical cysts are inflammatory odontogenic cysts and are generally the most common type of jaw cysts. They are associated with the apex of non-vital teeth[9]. Radiographically, periapical cysts show well-defined unilocular radiolucency with sclerotic borders in close proximity to the adjacent teeth[36]. UA is a variant of ameloblastoma that presents as a cyst and shares clinical and radiological characteristics with odontogenic cysts. They appear as well-defined unilocular radiolucencies that often surround the crown of an impacted tooth[37]. In the present case, the impacted tooth crown was located outside the lesion. Compared to ameloblastomas, odontogenic keratocysts exhibit less prominent buccolingual expansion and less frequent and severe adjacent tooth root resorption. The presence of pasty fluid in odontogenic keratocysts can lead to areas of attenuation within the cystic cavity, resulting in uneven internal density on CT[38]. Papageorge et al[10] and Larsson et al[11] observed radiographic evidence of calcification in solitary intraosseous neurofibromas and proposed that this might be the result of high collagen content rather than genuine calcification. Odontogenic lesions in the mandible originate above the mandibular canal. Neural and vascular lesions mostly arise within the mandibular canal, whereas lesions centered below the mandibular canal are usually of non-odontogenic origin[12]. Therefore, it is crucial to carefully analyze the correlation between lesions and the inferior alveolar nerve canal. If the lesion involves the inferior alveolar nerve canal, it is essential to consider that the swelling may have a neural origin.
| Disease | Age (year) | Sites | Radiographic Findings |
| Radicular (periapical) cysts | In the 3rd to 5th decades of life | Located at the apices of dead pulp teeth, caused by inflammation of the apical tissue due to caries or trauma | Circular, unilocular low-density images at the apex of the tooth. Massive periapical cysts may cause root resorption, displacement of adjacent structures, and expansion |
| Dentigerous cysts | In adolescents and young adults | The upper canine and lower third molar | Clear radiolucent image around the tooth crown with cortical border causing a significant displacement. Expansion and root resorption may be present. The cortical border is usually preserved |
| Simple bone cysts | In the 2nd decades of life | The posterior part of the mandible | A radiolucency scalloping between the roots of the teeth |
| Odontogenic keratocysts | In the 3rd decades of life | The posterior part of the mandible | Unilocular/multilocular lesions with scalloped margins. May present as radiolucent around the tooth crown. May lead to cortical thinning, tooth displacement, and root resorption |
| Ameloblastoma | In the 3rd to 5th decades of life | The posterior part of the mandible | Well-defined unilocular/multilocular radiolucency. May appear as a pericoronal radiolucency. Extensive root resorption. Has a typical “soap bubble” appearance |
| Aneurysmal bone cyst | In young adults | The posterior part of the mandible | A unilocular or multilocular radiolucency with cortical expansion |
| Central giant cell granuloma | In adolescents and young adults | The anterior part of the mandible | Mandibular border is clearly defined. Radiolucent with granular calcifications. May cause tooth displacement, root absorption, destruction of cortical plates, and invasion into surrounding soft tissues. Early-stage lesions: Small unilocular areas (similar to odontogenic cysts). Progressive stage: Multilocularity with sparse internal septa and bone expansion |
| Schwannomas | Most often in the 4th and 5th decades | The posterior part of the mandible | Radiolucent, unilocular,homogeneous, and well-defined lesions with cortical expansion |
| Neurofibromas | In adolescents and young adults | The posterior part of the mandible | Low-density unicystic or multicystic images with clear or unclear borders. They can expand and penetrate the boundary of the dermis. Tooth root absorption and tooth displacement may also occur. Fusiform enlargement of the mandibular canal |
| Central hemangioma | In the 2nd decades of life | It mainly occurs in the spine. The mandible is a very rare location, with the posterior part of the mandible being slightly more common | Unilocular or multilocular lesion, with large bone marrow spaces and rough trabeculae formation. Accompanied by a typical honeycomb or soap-bubble appearance. When it occurs within the inferior alveolar canal, the canal was wider than normal |
| Arteriovenous malformation | In the 1st decades of life | They are uncommon lesions of the head and neck. The majority of jaw lesions occur in the mandibular ramus and body | May appear cystic due to adjacent bone resorption. May appear multilocular. When located within the inferior alveolar canal, the canal can enlarge throughout the entire course |
| Lymphoma | Most patients aged between 40 and 60 yr | Mandibular body | Radiolucent pattern with non-transmitted radiation particles and reactive bone attachment. May cause “moth-eaten” appearance, lamellar bone formation in periosteum, widening of mandibular canal, irregular increase in periodontal ligament width, and tooth spacing |
Histologically, solitary neurofibromas originate from the nerves and are composed of Schwann cells, perineural cells, endoneural fibroblasts, and intermediate cells[39,40]. They have well-defined boundaries with the surrounding connective tissue, distinguishing them from the multiple neurofibromas observed in cases of neurofibromatosis[3]. It is crucial to perform S-100 and CD34 immunostaining on biopsy samples. In neurofibromas, tumor cells are loosely arranged and fragile, often with wavy or snake-shaped nuclei, and S-100 protein-positive cells are less common than in schwannomas[41]. The final pathological diagnosis should be based on the presence of CD34, which is located in the cell membrane and cytoplasm. CD34 positivity is observed in neurofibromas but not in schwannomas[42].
Surgical resection is currently the primary treatment for solitary intramedullary intraosseous neurofibromas. However, there have been no reports of adjuvant therapy, and the local recurrence rate of neurofibromas is higher than that of schwannomas, possibly because of the lack of an envelope[43]. This makes complete tumor removal more challenging, and the affected nerve is sacrificed during radical resection of neurofibromas[8]. While neurofibromas may progress to neurofibromatosis or undergo malignant transformation as the primary disease[44,45], the likelihood of solitary neurofibromas becoming malignant is quite low compared to that of neurofibromatosis[46]. The possible development of this disease emphasizes the importance of regular monitoring for patients with early neurofibroma symptoms. Our patient showed no signs of recurrence or progression to neurofibromatosis nine months after surgery. In the future, we will continue to monitor these patients.
In this report, we detail the case of a 37-year-old female with tooth root resorption and local sensory abnormalities in the right mandible, indicative of a solitary intraosseous neurofibroma. While pathological examination remains the primary diagnostic method for intraosseous neurofibroma, clinicians must carefully examine the patient’s symptoms and observe the relationship between the lesion and inferior alveolar nerve canal. An accurate distinction between cystic lesions and neurogenic tumors in the mandible is crucial for early diagnosis and appropriate treatment. Following surgical inter
We are very grateful to the patient for providing informed consent for publication after being informed.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Park HK, South Korea; Yarmahmoodi F, Iran S-Editor: Qu XL L-Editor: A P-Editor: Xu ZH
| 1. | Depprich R, Singh DD, Reinecke P, Kübler NR, Handschel J. Solitary submucous neurofibroma of the mandible: review of the literature and report of a rare case. Head Face Med. 2009;5:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Ferner RE, Huson SM, Thomas N, Moss C, Willshaw H, Evans DG, Upadhyaya M, Towers R, Gleeson M, Steiger C, Kirby A. Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. J Med Genet. 2007;44:81-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 655] [Cited by in RCA: 597] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 3. | Wright BA, Jackson D. Neural tumors of the oral cavity. A review of the spectrum of benign and malignant oral tumors of the oral cavity and jaws. Oral Surg Oral Med Oral Pathol. 1980;49:509-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 110] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Mori H, Kakuta S, Yamaguchi A, Nagumo M. Solitary intraosseous neurofibroma of the maxilla: report of a case. J Oral Maxillofac Surg. 1993;51:688-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Kamalakaran A, Jayaraman B, Raghavendran S, Thirunavukkarasu R, Ayyappan M, Syed JBAB. Intraosseous Neurofibroma of Mandible in a 5-Year-Old: A Rare Case Report and Review of Literature. J Maxillofac Oral Surg. 2022;21:1336-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 6. | Sarkar DF, Mishra N, Pati D, Samal SK. Solitary Neurofibroma of Mandible in a 2-Year-Old Child: A Rare Case Report and Review of Literature. J Maxillofac Oral Surg. 2022;21:1320-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 7. | Vivek N, Manikandhan R, James PC, Rajeev R. Solitary intraosseous neurofibroma of mandible. Indian J Dent Res. 2006;17:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Apostolidis C, Anterriotis D, Rapidis AD, Angelopoulos AP. Solitary intraosseous neurofibroma of the inferior alveolar nerve: report of a case. J Oral Maxillofac Surg. 2001;59:232-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Johnson NR, Gannon OM, Savage NW, Batstone MD. Frequency of odontogenic cysts and tumors: a systematic review. J Investig Clin Dent. 2014;5:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 10. | Papageorge MB, Doku HC, Lis R. Solitary neurofibroma of the mandible and infratemporal fossa in a young child. Report of a case. Oral Surg Oral Med Oral Pathol. 1992;73:407-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Larsson A, Praetorius F, Hjörting-Hansen E. Intraosseous neurofibroma of the jaws. Int J Oral Surg. 1978;7:494-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Gohel A, Villa A, Sakai O. Benign Jaw Lesions. Dent Clin North Am. 2016;60:125-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Behrad S, Sohanian S, Ghanbarzadegan A. Solitary intraosseous neurofibroma of the mandible: Report of an extremely rare histopathologic feature. Indian J Pathol Microbiol. 2020;63:276-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Iqbal A, Tamgadge S, Tamgadge A, Chande M. Intraosseous neurofibroma in a 13-year-old male patient: A case report with review of literature. J Cancer Res Ther. 2018;14:712-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Inoue T, Elaskary M, Shima A, Hirai H, Suzuki F, Matsuda M. Trigeminal neurofibroma in the infratemporal fossa arising from the inferior alveolar nerve: A case report. Mol Clin Oncol. 2017;7:825-829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Narang BR, Palaskar SJ, Bartake AR, Pawar RB, Rongte S. Intraosseous Neurofibroma of the Mandible: A Case Report and Review of Literature. J Clin Diagn Res. 2017;11:ZD06-ZD08. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Fortier K. Solitary Intraosseous Mandibular Neurofibroma: Clinical Case Study 2020;. [DOI] [Full Text] |
| 18. | Gujjar PK, Hallur JM, Patil ST, Dakshinamurthy SM, Chande M, Pereira T, Zingade J. The Solitary Variant of Mandibular Intraosseous Neurofibroma: Report of a Rare Entity. Case Rep Dent. 2015;2015:520261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Saravani S, Kadeh H, Nosratzehi T. Solitary intraosseous neurofibroma of the mandible. Zahedan J Res Med Sci. 2014;16. |
| 20. | Jangam SS, Ingole SN, Deshpande MD, Ranadive PA. Solitary intraosseous neurofibroma: Report of a unique case. Contemp Clin Dent. 2014;5:561-563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Deichler J, Martínez R, Niklander S, Seguel H, Marshall M, Esguep A. Solitary intraosseous neurofibroma of the mandible. Apropos of a case. Med Oral Patol Oral Cir Bucal. 2011;16:e704-e707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Tao Q, Wang Y, Zheng C. Neurofibroma in the left mandible: a case report. Kaohsiung J Med Sci. 2010;26:217-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Alatli C, Oner B, Unür M, Erseven G. Solitary plexiform neurofibroma of the oral cavity A case report. Int J Oral Maxillofac Surg. 1996;25:379-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Ueda M, Suzuki H, Kaneda T. Solitary intraosseous neurofibroma of the mandible: report of a case. Nagoya J Med Sci. 1993;55:97-101. [PubMed] |
| 25. | Weaver BD, Graves RW, Keyes GG, Lattanzi DA. Central neurofibroma of the mandible: report of a case. J Oral Maxillofac Surg. 1991;49:1243-1246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Polak M, Polak G, Brocheriou C, Vigneul J. Solitary neurofibroma of the mandible: case report and review of the literature. J Oral Maxillofac Surg. 1989;47:65-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Papadopoulos H, Zachariades N, Angelopoulos AP. Neurofibroma of the mandible. Review of the literature and report of a case. Int J Oral Surg. 1981;10:293-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Ellis GL, Abrams AM, Melrose RJ. Intraosseous benign neural sheath neoplasms of the jaws. Report of seven new cases and review of the literature. Oral Surg Oral Med Oral Pathol. 1977;44:731-743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 72] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Cundy RL, Matukas VJ. Solitary intraosseous neurofibroma of the mandible. Arch Otolaryngol. 1972;96:81-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Cassalia PT, Miller AS. Solitary central neurofibroma of the mandible. Br J Oral Surg. 1971;8:270-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 31. | Sharawy A, Springer J. Central neurofibroma occurring in the mandible. Report of a case. Oral Surg Oral Med Oral Pathol. 1968;25:817-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Gutman D, Griffel B, Munk J, Shohat S. Solitary neurofibroma of the mandible. Oral Surg Oral Med Oral Pathol. 1964;17:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Cornell CF, Vargas HA. Intraosseous neurofibroma of the mandible. Oral Surg Oral Med Oral Pathol. 1955;8:34-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 34. | Bruce KW. Solitary neurofibroma (neurilemmoma, schwannoma) of the oral cavity. Oral Surg Oral Med Oral Pathol. 1954;7:1150-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Blackwood HJ, Lucas RB. Neurofibroma of the mandible. Proc R Soc Med. 1951;44:864-865. [PubMed] |
| 36. | Yoshiura K, Weber AL, Runnels S, Scrivani SJ. Cystic lesions of the mandible and maxilla. Neuroimaging Clin N Am. 2003;13:485-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 37. | Bilodeau EA, Collins BM. Odontogenic Cysts and Neoplasms. Surg Pathol Clin. 2017;10:177-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 97] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 38. | Yoshiura K, Higuchi Y, Ariji Y, Shinohara M, Yuasa K, Nakayama E, Ban S, Kanda S. Increased attenuation in odontogenic keratocysts with computed tomography: a new finding. Dentomaxillofac Radiol. 1994;23:138-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Ide F, Shimoyama T, Horie N, Kusama K. Comparative ultrastructural and immunohistochemical study of perineurioma and neurofibroma of the oral mucosa. Oral Oncol. 2004;40:948-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 40. | Gómez-Oliveira G, Fernández-Alba Luengo J, Martín-Sastre R, Patiño-Seijas B, López-Cedrún-Cembranos JL. Plexiform neurofibroma of the cheek mucosa. A case report. Med Oral. 2004;9:263-267. [PubMed] |
| 41. | Taketomi T, Nakamura K, Teratani Y, Matsuo K, Kusukawa J. Solitary Neurofibroma of the Hard Palate: A Case Report and Literature Review. Am J Case Rep. 2021;22:e929674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Chaubal A, Paetau A, Zoltick P, Miettinen M. CD34 immunoreactivity in nervous system tumors. Acta Neuropathol. 1994;88:454-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Gnepp DR, Keyes GG. Central neurofibromas of the mandible: report of two cases. J Oral Surg. 1981;39:125-127. [PubMed] |
| 44. | D'Ambrosio JA, Langlais RP, Young RS. Jaw and skull changes in neurofibromatosis. Oral Surg Oral Med Oral Pathol. 1988;66:391-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 45. | Hustin J, Delire Y. Unusual intramandibular neural tumor. Oral Surg Oral Med Oral Pathol. 1991;71:593-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 46. | Abell MR, Hart WR, Olson JR. Tumors of the peripheral nervous system. Hum Pathol. 1970;1:503-551. [PubMed] |