Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3195
Peer-review started: November 20, 2022
First decision: February 14, 2023
Revised: March 5, 2023
Accepted: April 4, 2023
Article in press: April 4, 2023
Published online: May 16, 2023
Processing time: 176 Days and 22.5 Hours
Many studies have focused on the femoral tunnel technique and fixation method, but few studies have involved the tibial tunnel technique and fixation method. The all-inside technique is one of the new techniques that has been described in recent years. All-inside anterior cruciate ligament (ACL) reconstruction is based on a tibial socket instead of a full tunnel. This method has many potential advantages.
To compare clinical outcomes of knee ACL autograft reconstruction using all-inside quadrupled semitendinosus (AIST) and traditional hamstring tendon (TBT) techniques.
From January 2017 to October 2019, the clinical data of 80 patients with ACL reconstruction were retrospectively analyzed, including 67 males and 13 females. The patients had an average age of 24.3 ± 3.1 years (age range: 18-33 years). The AIST technique was used in 42 patients and the TBT technique was used in 38 patients. The time between operation and injury, operative duration, post
Eighty patients were followed for 24-36 mo, with an average follow-up duration of 27.5 ± 1.8 mo. There were no significant differences in the time between surgery and injury, operative duration, IKDC and Lysholm scores of the affected knee at the last follow-up evaluation between the two groups. There were significant differences in VAS scores 1 d, 3 d, 7 d, 2 wk and 1 mo after surgery (P < 0.05). There was no significant difference in VAS score at 3 mo, 6 mo and 1 year after operation.
The efficacy of the AIST ACL reconstruction technique was comparable to the TBT technique, but the postoperative pain was less with the AIST technique. Thus, the AIST technique is an ideal treatment choice for ACL reconstruction.
Core Tip: This study retrospectively analyzed 80 patients with anterior cruciate ligament (ACL) injuries who underwent all-inside quadrupled semitendinosus (AIST) or traditional hamstring tendon (TBT). We demonstrated that there were no significant differences in the time between surgery and injury, operative duration, International Knee Documentation Committee and Lysholm scores of the affected knee. However, there were significant differences in visual analogue scale scores 1 d, 3 d, 7 d, 2 wk and 1 mo after surgery (P < 0.05). These results indicated the efficacy of the AIST ACL reconstruction technique was comparable to the TBT technique, but the postoperative pain was less with the AIST technique. Thus, the AIST technique is a better choice for ACL reconstruction.
- Citation: An BJ, Wang YT, Zhao Z, Wang MX, Xing GY. Comparative study of the clinical efficacy of all-inside and traditional techniques in anterior cruciate ligament reconstruction. World J Clin Cases 2023; 11(14): 3195-3203
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3195.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3195
Anterior cruciate ligament (ACL) injuries are common sports injuries that often lead to knee instability and secondary traumatic osteoarthritis, meniscus injuries, and contralateral ACL injuries[1,2]. Arthroscopic reconstruction of the ACL is the main method of repair. The optimal ACL reconstruction technique has not been determined, with reported graft retear rates ranging from 10%-25%[3-5]. This is a significant clinical problem due to the increasing frequency of ACL injuries occurring in this group[6-9] and to the high rate of secondary injuries following ACL reconstruction in this particular cohort[10-15]. Many studies have focused on the femoral tunnel technique and fixation method, but few studies have involved the tibial tunnel technique and fixation method. The all-inside technique is one of the new techniques that has been descried in recent years. All-inside ACL reconstruction is based on a tibial socket instead of a full tunnel[16]. This method has many potential advantages. Specifically, Lubowitz et al[17] reported less pain with all-inside allograft ACL reconstruction compared with a full tibial tunnel in a randomized controlled trial. Therefore, this all-inside approach improved graft integration and stability of a hamstring construct[18], in contrast to other described hamstring reconstruction techniques that have been compared with a bone-patellar-tendon-bone graft, along with the added benefit of less anterior knee pain. The purpose of this investigation was to compare knee ACL autograft reconstruction using all-inside quadrupled semitendinosus (AIST) and traditional hamstring tendon (TBT) techniques. In this study 80 patients with ACL injuries admitted to our hospital from January 2017 to October 2019 were retrospectively analyzed.
This study retrospectively analyzed the data of 80 patients with ACL injuries admitted to the Department of Orthopedics at the Third Medical Center of PLA General Hospital from January 2017 to October 2019. There were 67 males and 13 females, 18-33 years of age, with an average age of 24.3 ± 3.1 years. There were 42 patients in the AIST group and 38 patients in the TBT group. There were no significant differences in sex, age, injured side, and time between operation and injury between the two groups (P > 0.05). This study was conducted with the informed consent of the patients and according to the guidelines of the Declaration of Helsinki.
Eligibility for the study was assessed before consent and conducted by a research coordinator at the study site. The inclusion criteria were patients with an ACL-deficient knee who agreed to ACL reconstructive surgery using autograft tissue. Patients with associated meniscal and chondral pathologic changes (except those meeting exclusion criteria) were included in the study; the pathologic changes treated at the time of ACL reconstruction were at the discretion of the study surgeon. All pathologic changes and treatments were recorded. Patients who had previous ACL reconstructive surgery or underwent multi-ligament, medial collateral ligament, posterior cruciate ligament, lateral collateral ligament, posteromedial corner, or posterolateral corner repair or reconstruction surgery were excluded.
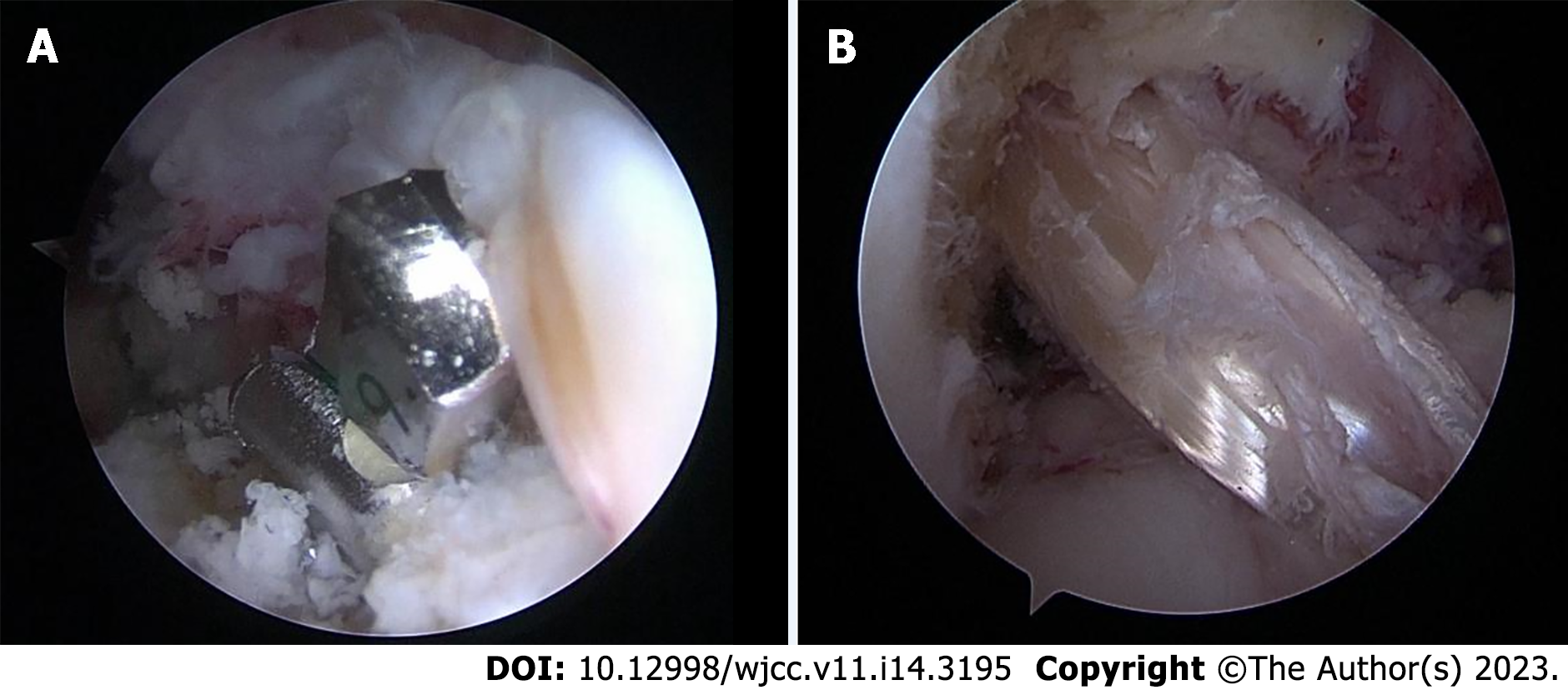
AIST technique group: The ipsilateral semitendinosus muscle was passed through the respective TightRope loops, quadrupled, and the two free ends on the tibial side were sutured together with #0 FiberLoop (Arthrex, ) in a SpeedWhip-type pattern leaving the suture ends intact (Figure 1). Using the remaining native ACL fibers as a reference and the over-the-top position with a guide (Arthrex), a pin was placed and the lateral femur was drilled out. In this way, the femoral socket was created as close as possible to the anatomic ACL center via anteromedial portal drilling using a low-profile reamer (Arthrex) matching the graft diameter. The minimal graft in socket depth was 25 mm. The pin was used to place a #2 FiberWire (Arthrex) shuttle suture. The intra-articular ACL graft distance was measured with an intra-articular ruler (Arthrex), and this distance was added to the length of the graft in the femoral socket to determine the depth of graft in the tibial socket based on the total graft length. The tibial socket was created at the anatomic tibial site indexing off the anterior horn of the lateral meniscus using a FlipCutter aiming guide (Arthrex). A straight FlipCutter pin matching the graft diameter was then drilled into the joint and “unflipped” to become a reamer to retro-cut the tibial socket, which was also reamed 5 mm deeper than needed to allow for optimal graft tensioning with the all-inside technique. The FlipCutter pin was drilled back into the joint, “unflipped,” removed, and a #2 TigerStick suture (Arthrex) was passed through this FlipCutter pin hole up into the joint and retrieved as a tibial shuttle suture. The #2 FiberWire shuttle suture from the femoral socket was used to pull the graft through the anteromedial portal across the joint up into the femur, flipping the suspensory TightRope RT button on the lateral femoral cortex. The graft was then hoisted up into the socket to the appropriate depth with the TightRope shortening strands (Figure 2).
TBT technique group: A #2 FiberWire was used to suture 2 cm at each end of the ipsilateral semitendinosus and gracilis tendons. The tibial insertion was located by point-to-point sight (Smith and Nephew), and the medial side of the femoral lateral condyle was located via the tibia, and the femoral side was fixed by an Endobutton (Smith and Nephew). The graft was tightened at 30° flexion of the knee and tibial fixation was achieved using an interference screw (Smith and Nephew).
The rehabilitation protocol for the AIST and TBT technique cohorts were the same. The affected limbs of the two groups were fixed with braces after surgery. Quadriceps isometric exercises were started on the 2nd d after surgery, straight leg raising exercises were started on the 3rd d after surgery with gradual weight-bearing under brace protection, and complete weight-bearing was achieved 4 wk after surgery. Passive knee flexion and extension exercise were started the 2nd wk after surgery, increasing by 30° every week, and reaching > 120° (close to normal) 6 wk after surgery. Activities of daily living were resumed the 4th mo after surgery and physical exercises were gradually resumed 6 mo after surgery.
All patients underwent an extensive clinical, subjective, and objective evaluation preoperatively. Visual analogue scale (VAS) scores were evaluated and recorded 1, 3, and 7 d, 2 wk, 1 and 6 mo, and 1 and 2 years postoperatively for each patient. The operative duration, and International Knee Documentation Committee (IKDC) and Lysholm scores of the affected knee at the last follow-up evaluation were recorded.
To determine the difference between the two-sample means, normal distribution measurement data are expressed as the mean ± standard deviation. T-test and repeated measurement data analysis of variance were used. The Fisher test was used for enumeration data, and the Kruskal-Wallis test was used for multi-valued ordinal data. Statistical analyses were performed with commercially-available software (SPSS version 18.0). A P < 0.05 was considered statistically significant.
All patients had follow-up evaluations for 24-36 mo (mean, 27.5 ± 1.8 mo). There was no significant difference in the operative duration between the two groups. One patient in each group had grade C knee function postoperatively. Two patients in the traditional group had numbness at the graft site postoperatively; the numbness was significantly relieved 1 year postoperatively. There was no significant difference in the IKDC score between the two groups (Table 1). The Lysholm scores of all patients were > 90°. There was no significant difference in the mean scores between the two groups (Table 2). The VAS score of the internal group was lower than the traditional group (P < 0.05). All patients were pain-free 6 mo, and 1 year and 2 years postoperatively (Table 3). No complications, such as ligament re-injuries and infections, occurred in the two groups during the follow-up period.
| IKDC score | AIST group | TBT group | χ2 value | P value |
| Grade A | 30 | 24 | 1.657 | 0.233 |
| Grade B | 11 | 13 | ||
| Grade C | 1 | 1 |
| Group | Patient | Preoperative | 6 wk postoperatively | 12 wk postoperatively |
| AIST group | 42 | 63.3 ± 5.6 | 75.3 ± 6.5 | 86.7 ± 5.8 |
| Group | 38 | 64.6 ± 4.8 | 74.6 ± 7.1 | 85.5 ± 6.6 |
| t value | 0.765 | 0.799 | 0.631 | |
| P value | 0.365 | 0.434 | 0.523 |
| Time | TBT | 95%CI | AIST | 95%CI | P value |
| Day 1 | 9.4 ± 0.6 | 1.0 | 7.5 ± 0.5 | 0.9 | 0.032 |
| Day 3 | 7.5 ± 0.5 | 0.9 | 4.8 ± 0.8 | 0.8 | 0.028 |
| Day 7 | 4.1 ± 0.6 | 0.8 | 2.5 ± 0.7 | 0.7 | 0.004 |
| 2 wk | 2.6 ± 0.5 | 0.8 | 0.6 ± 0.5 | 0.5 | 0.011 |
| 1 mo | 1.2 ± 0.5 | 0.6 | 0.5 ± 0.5 | 0.5 | 0.023 |
| 6 mo | 0.8 ± 0.6 | 0.4 | 0.6 ± 0.5 | 0.4 | 0.815 |
| 1 yr | 0.4 ± 0.5 | 0.2 | 0.3 ± 0.6 | 0.3 | 0.782 |
| 2 yr | 0.3 ± 0.3 | 0.1 | 0.1 ± 0.5 | 0.2 | 0.769 |
An ACL injury is one of the most common sports-related knee injuries. With the advances in arthroscopic technology, arthroscopic ACL reconstruction is a widely performed surgical procedure. Some studies[17,19]; however, have shown that the absence of the hamstring tendon of the knee will lead to a reduction in the flexion internal rotation force of the knee by 5%-10%. Yosmaoglu et al[20] have shown that preserving the gracilis muscle is crucial for postoperative rehabilitation training, especially for patients who participate in knee flexion exercises > 70°. Preservation of the gracilis muscle significantly accelerates recovery of knee function after ACL reconstruction. Volpi et al[21] believed that to restore joint motion and function, the clinical effect of the all-inside technique is similar to traditional single-beam reconstruction surgery. The bone tunnel of the tibia in the AIST group was drilled from outside-in, and the tunnel was thin outside and thick inside, which is conducive to reducing the leakage of joint fluid and thereby reducing the risk of infection. Based on a retrospective analysis, Connaughton et al[22] concluded that the operative time, Lysholm score, and IKDC score were not significantly different between the AIST and TBT groups, but the postoperative VAS score of the AIST group was significantly lower than the TBT group (P < 0.05). Connaughton et al[22] believed that the efficacy of all-inside reconstruction was similar to the traditional group, but the postoperative pain of the all-inside group was less severe. Benea et al[23] also reported that the pain at the graft removal site was apparent in the short term after surgery, and only one tendon could be removed to alleviate postoperative pain. Within 1 mo after surgery, the pain among patients in the all-inside group was significantly lower than the traditional group. This study also confirmed that the VAS score of the all-inside group was significantly lower than the traditional reconstruction group, and the patients felt well. In our study, the VAS score for postoperative pain in the all-inside group was lower than the traditional group. The reasons for this finding were as follows: The diameter of the cortical tibial tunnel in the all-inside group was 3.5 mm and 7 or 8 mm in the traditional group; and only semitendinosus muscle was taken as the graft in the all-inside group, which caused less injury to the surrounding soft tissues.
Kouloumentas et al[24] showed that fixed and adjustable loop buttons of the femoral end fixation greatly exceed the mechanical strength required for early knee exercises in the maximum load biomechanical test, which met the needs of patients for early functional exercises. In a randomized controlled study involving 188 patients, Boyle et al[25] showed that there was no statistical difference in the test results of KT-1000, the graft failure rate, and the graft failure time between adjustable and fixed loops at the femoral end. The tibial lateral fixation method was changed from the traditional inter-facial screw extrusion fixation to suspension fixation. Biomechanical tests confirmed that extrusion screw fixation had a lower relaxation rate of graft elongation and ideal anti-pull-out performance, while suspension fixation had a higher load limit and did not show increased graft displacement compared with screw fixation[26]. A meta-analysis concluded that there was no significant difference between suspension fixation and tunnel extrusion screw fixation in terms of normal knee relaxation, the graft failure rate, patient satisfaction, and recovery to the pre-injury activity rate. Therefore, it can be concluded that both the all-inside suspension fixation technique and the traditional total tibial tunnel interface extrusion screw fixation technique achieved excellent results in ACL reconstruction[27,28]. Our study also showed that the tension of the all-inside reconstruction graft and the stability of the knee postoperatively were ideal, and there was no graft relaxation or failure. There was no significant difference in the treatment effect and postoperative knee function recovery between the two groups. The two groups achieved satisfactory treatment effects in pain improvement and recovery of knee motor function.
In our study the all-inside technique was used to reconstruct the ACL. Only the semitendinosus tendon was used as a graft, which reduced loss of the internal rotation force in flexion of the affected knee after surgery and was beneficial to postoperative rehabilitation. One patient in the traditional group had numbness at the graft site after surgery, which may have been caused by injury of the inferior patellar branch of the saphenous nerve during tendon extraction, leading to numbness on the medial aspect of the proximal knee. In the all-inside group, one patient had a postoperative knee extension limitation of 8°. This patient underwent ACL reconstruction on the 19th d after the injury. The reason for this finding may be that the operation was too close to the injury time, thus resulting in knee stiffness. Andernord et al[29] showed that ACL reconstruction in the early stage after injury increased the incidence of knee stiffness, and the mechanism may be related to the influence of operation timing on postoperative joint fibrosis.
In addition, the femoral tunnel is independently drilled through the foot location area of the anterolateral entrance of the positioning hook, which does not require excessive flexion of the affected knee and is in agreement with the concept of anatomic reconstruction[30,31], which effectively avoids pain caused by the impact of the non-anatomic reconstruction graft on the intercondylar fossa or posterior cruciate ligament during knee activity[23]. Lubowitz et al[17] also reached the same conclusion in a prospective randomized controlled study. The bone tunnel of the whole inner group of the tibia was drilled from inside-to-outside, which effectively preserved the cortical bone of the proximal tibia and avoided a burst fracture. In addition, the tunnel is thin outside and thick inside, and the tunnel communicating with the outside world is very small, so the joint fluid will not leak, thus reducing the risk of infection[21]. The tibia and femur sides of the all-inside group were suspended and fixed by a TightRope locking loop bone plate, which not only makes full use of the tendon-bone interface and promotes tendon-bone healing, but also effectively avoids the cutting effect of squeeze nails on the graft[32]. Compared with an Endobutton, the TightRope has an adjustable locking wire loop[31], so there is no need to reserve the loop turning distance when making the bone tunnel, which reduces bone loss and keeps the graft close to the bottom of the bone tunnel, thus effectively avoiding the "bungee effect" of suspensory fixation[33,34].
In conclusion, the all-inside technique has the same efficacy as the traditional technique with respect to knee function and exercise level, but has less postoperative pain, higher tendon utilization, and less injury. In addition, the all-inside technique has little damage to the proximal tibial cortex and only uses one hamstring muscle, which is of great value in simultaneous ACL reconstruction with high tibial osteotomy, multiple knee ligament reconstruction, and revision surgery for ACL re-tears.
We compare clinical outcomes of knee anterior cruciate ligament (ACL) autograft reconstruction using all-inside quadruple semitendinosus (AIST) and traditional hamstring tendon (TBT) techniques.
To seek a good fixation method to reconstruct the ACL and reduce the failure rate.
To compare clinical outcomes of knee ACL autograft reconstruction using AIST and TBT techniques.
From January 2017 to October 2019, the clinical data of 80 patients with ACL reconstruction were retrospectively analyzed, including 67 males and 13 females. The patients had an average age of 24.3 ± 3.1 years (age range: 18-33 years). The AIST technique was used in 42 patients and the TBT technique was used in 38 patients. The time between operation and injury, operative duration, postoperative visual analogue scale (VAS) score and knee functional recovery were recorded and compared between the two groups. The International Knee Documentation Committee (IKDC) and Lysholm scoring system were used to comprehensively evaluate clinical efficacy.
Eighty patients were followed for 24-36 mo, with an average of follow-up duration of 27.5 ± 1.8 mo. There were no significant differences in the time between surgery and injury, operative duration, IKDC and Lysholm scores of the affected knee at the last follow-up evaluation between the two groups. There were significant differences in VAS scores 1 d, 3 d, 7 d, 2 wk and 1 mo after surgery (P < 0.05). There was no significant difference in VAS score at 3 mo, 6 mo and 1 year after operation.
The efficacy of the AIST ACL reconstruction technique was comparable to the TBT technique, but the postoperative pain was less with the AIST technique. Thus, the AIST technique is an ideal treatment choice for ACL reconstruction.
Arthroscopic reconstruction of the ACL is the main method of repair, the optimal ACL reconstruction technique has not been determined.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bernardes A, Portugal; Velázquez-Saornil J, Spain S-Editor: Fan JR L-Editor: Filipodia P-Editor: Li X
| 1. | Hettrich CM, Dunn WR, Reinke EK; MOON Group, Spindler KP. The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41:1534-1540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 229] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 2. | Poulsen E, Goncalves GH, Bricca A, Roos EM, Thorlund JB, Juhl CB. Knee osteoarthritis risk is increased 4-6 fold after knee injury - a systematic review and meta-analysis. Br J Sports Med. 2019;53:1454-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 183] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 3. | Ho B, Edmonds EW, Chambers HG, Bastrom TP, Pennock AT. Risk Factors for Early ACL Reconstruction Failure in Pediatric and Adolescent Patients: A Review of 561 Cases. J Pediatr Orthop. 2018;38:388-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 4. | Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to Sport After Pediatric Anterior Cruciate Ligament Reconstruction and Its Effect on Subsequent Anterior Cruciate Ligament Injury. J Bone Joint Surg Am. 2017;99:897-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 194] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 5. | Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90 % of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26:1019-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 119] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 6. | Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Trends in Incidence of ACL Reconstruction and Concomitant Procedures Among Commercially Insured Individuals in the United States, 2002-2014. Sports Health. 2018;10:523-531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 220] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 7. | Werner BC, Yang S, Looney AM, Gwathmey FW Jr. Trends in Pediatric and Adolescent Anterior Cruciate Ligament Injury and Reconstruction. J Pediatr Orthop. 2016;36:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 215] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 8. | Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42:675-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 321] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 9. | Johnsen MB, Guddal MH, Småstuen MC, Moksnes H, Engebretsen L, Storheim K, Zwart JA. Sport Participation and the Risk of Anterior Cruciate Ligament Reconstruction in Adolescents: A Population-based Prospective Cohort Study (The Young-HUNT Study). Am J Sports Med. 2016;44:2917-2924. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Allen MM, Pareek A, Krych AJ, Hewett TE, Levy BA, Stuart MJ, Dahm DL. Are Female Soccer Players at an Increased Risk of Second Anterior Cruciate Ligament Injury Compared With Their Athletic Peers? Am J Sports Med. 2016;44:2492-2498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 83] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 11. | Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 311] [Cited by in RCA: 372] [Article Influence: 33.8] [Reference Citation Analysis (0)] |
| 12. | Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport. Am J Sports Med. 2014;42:1567-1573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 454] [Cited by in RCA: 572] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 13. | Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA. 20-Year Outcomes of Anterior Cruciate Ligament Reconstruction With Hamstring Tendon Autograft: The Catastrophic Effect of Age and Posterior Tibial Slope. Am J Sports Med. 2018;46:531-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 231] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 14. | Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 325] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 15. | Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Am J Sports Med. 2016;44:1861-1876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 996] [Cited by in RCA: 870] [Article Influence: 96.7] [Reference Citation Analysis (0)] |
| 16. | Lubowitz JH. No-tunnel anterior cruciate ligament reconstruction: the transtibial all-inside technique. Arthroscopy. 2006;22:900.e1-900.11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Lubowitz JH, Schwartzberg R, Smith P. Randomized controlled trial comparing all-inside anterior cruciate ligament reconstruction technique with anterior cruciate ligament reconstruction with a full tibial tunnel. Arthroscopy. 2013;29:1195-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 18. | Browning WM 3rd, Kluczynski MA, Curatolo C, Marzo JM. Suspensory Versus Aperture Fixation of a Quadrupled Hamstring Tendon Autograft in Anterior Cruciate Ligament Reconstruction: A Meta-analysis. Am J Sports Med. 2017;45:2418-2427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 19. | Segawa H, Omori G, Koga Y, Kameo T, Iida S, Tanaka M. Rotational muscle strength of the limb after anterior cruciate ligament reconstruction using semitendinosus and gracilis tendon. Arthroscopy. 2002;18:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 97] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Yosmaoglu HB, Baltaci G, Ozer H, Atay A. Effects of additional gracilis tendon harvest on muscle torque, motor coordination, and knee laxity in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19:1287-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Volpi P, Bait C, Cervellin M, Denti M, Prospero E, Morenghi E, Quaglia A. No difference at two years between all inside transtibial technique and traditional transtibial technique in anterior cruciate ligament reconstruction. Muscles Ligaments Tendons J. 2014;4:95-99. [PubMed] |
| 22. | Connaughton AJ, Geeslin AG, Uggen CW. All-inside ACL reconstruction: How does it compare to standard ACL reconstruction techniques? J Orthop. 2017;14:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 23. | Benea H, d'Astorg H, Klouche S, Bauer T, Tomoaia G, Hardy P. Pain evaluation after all-inside anterior cruciate ligament reconstruction and short term functional results of a prospective randomized study. Knee. 2014;21:102-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Kouloumentas P, Kavroudakis E, Charalampidis E, Kavroudakis D, Triantafyllopoulos GK. Superior knee flexor strength at 2 years with all-inside short-graft anterior cruciate ligament reconstruction vs a conventional hamstring technique. Knee Surg Sports Traumatol Arthrosc. 2019;27:3592-3598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Boyle MJ, Vovos TJ, Walker CG, Stabile KJ, Roth JM, Garrett WE Jr. Does adjustable-loop femoral cortical suspension loosen after anterior cruciate ligament reconstruction? Knee. 2015;22:304-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 26. | Mayr R, Heinrichs CH, Eichinger M, Coppola C, Schmoelz W, Attal R. Biomechanical comparison of 2 anterior cruciate ligament graft preparation techniques for tibial fixation: adjustable-length loop cortical button or interference screw. Am J Sports Med. 2015;43:1380-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 27. | Desai VS, Anderson GR, Wu IT, Levy BA, Dahm DL, Camp CL, Krych AJ, Stuart MJ. Anterior Cruciate Ligament Reconstruction With Hamstring Autograft: A Matched Cohort Comparison of the All-Inside and Complete Tibial Tunnel Techniques. Orthop J Sports Med. 2019;7:2325967118820297. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 28. | Zanchi N, Posner M, Herickhoff P. All-Inside Tibial Tunnel Drilling: How to Calculate a Safe Drilling Length to Avoid Anterior Cortex Violation. Arthrosc Tech. 2022;11:e2371-e2381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 29. | Andernord D, Desai N, Björnsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015;43:121-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 150] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 30. | Jones PE, Schuett DJ. All-Inside Anterior Cruciate Ligament Reconstruction as a Salvage for Small or Attenuated Hamstring Grafts. Arthrosc Tech. 2018;7:e453-e457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Papaloucas N. All-Inside Technique for ACL-Reconstruction using a FlipCutter® and the TightRope® System. Surg Technol Int. 2018;32:337-345. [PubMed] |
| 32. | Nuelle CW, Balldin BC, Slone HS. All-Inside Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2022;38:2368-2369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 33. | Monaco E, Fabbri M, Redler A, Gaj E, De Carli A, Argento G, Saithna A, Ferretti A. Anterior cruciate ligament reconstruction is associated with greater tibial tunnel widening when using a bioabsorbable screw compared to an all-inside technique with suspensory fixation. Knee Surg Sports Traumatol Arthrosc. 2019;27:2577-2584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 34. | Zeman P, Kautzner J, Havel O, Matějka J, Pavelka T, Havlas V. [Anatomical All-Inside Anterior Cruciate Ligament Reconstruction Using Quadrupled Semitendinosus Tendon Graft with Posteromedial Harvest - Clinical Results of Prospective Study at a Minimum 12-Months Follow-up]. Acta Chir Orthop Traumatol Cech. 2018;85:94-101. [PubMed] |