Published online Apr 26, 2023. doi: 10.12998/wjcc.v11.i12.2677
Peer-review started: February 17, 2023
First decision: March 10, 2023
Revised: March 12, 2023
Accepted: March 24, 2023
Article in press: March 24, 2023
Published online: April 26, 2023
Processing time: 67 Days and 14.1 Hours
Irritable bowel syndrome (IBS) is a common chronic functional gastrointestinal disorder affecting 10%-22% of adults. Its development is closely related to the gut microbiota, and the inflammatory and immune responses triggered by the gut microbiota can lead to IBS. Vitamin D (VD) effectively treats IBS with fewer side effects by improving gut microbiota, immune regulation, and anti-inflammatory effects. In the future, it is necessary to carry out epidemiological studies on the relationship between VD and IBS, clinical studies on the efficacy of supplementing VD to improve IBS, and animal studies on the mechanism of VD improving IBS. Therefore, this paper discussed the relationship between VD and IBS.
Core Tip: Irritable bowel syndrome (IBS) is a common chronic functional gastro
- Citation: Yu XL, Wu QQ, He LP, Zheng YF. Role of in vitamin D in irritable bowel syndrome. World J Clin Cases 2023; 11(12): 2677-2683
- URL: https://www.wjgnet.com/2307-8960/full/v11/i12/2677.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i12.2677
Irritable bowel syndrome (IBS) is a common chronic functional gastrointestinal disorder characterized by abdominal pain, bloating, urinary urgency, voiding incontinence, and altered bowel habits associated with structural and biochemical abnormalities[1] and affects 10%-22% of the adult population[2]. According to Rome IV criteria, IBS is divided into four types: IBS with constipation, IBS with diarrhea, IBS with mixed constipation and diarrhea, and IBS unclassified[3].
In the census statistics of Albanian adult samples, the prevalence of IBS in the study population was 8.6%. There was no sex difference, age differences, and regional differences. IBS with constipation is a common type[4]. However, in Western countries, the ratio of males to females with IBS is 2:1[5]. The disease is mild for most people but can be severe and even life-threatening in 1 in 20[6]. Although the etiology of IBS is unknown, current research suggests that it is related to host and environmental factors. Host factors include the gut-brain axis, serotonin pathway, and gut microbiota, and environmental factors include psychological stress, infection, antibiotic use, diet, and eating habits[7].
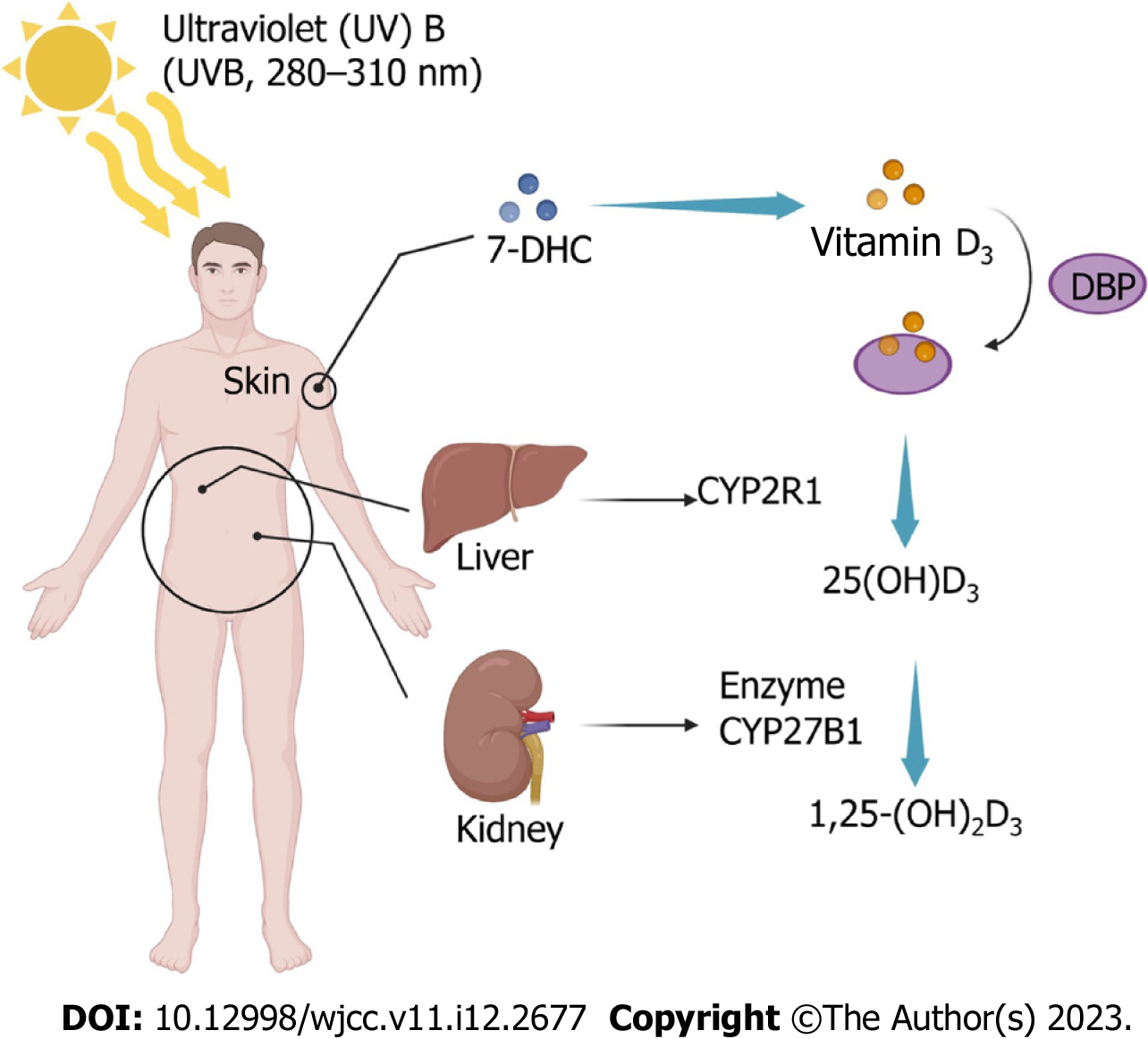
Vitamin D (VD) is a fat-soluble steroid that is a key regulator of calcium and phosphorus metabolism[8]. Two forms of VD play a major role in humans, D2 and D3, which are ergocalciferol and cholecalciferol, respectively, and they are similar in function. However, studies in recent years have shown that biochemical indicators show that VD2 seems to be cleared from the tissue faster than VD3. At the same dose, the efficacy of D2 is one-third to one-half of D3. When supplementing VD, we generally tend to choose VD3[9]. Studies have found a strong correlation between VD and type 1 diabetes mellitus[10,11] and obesity[12]. The main source of VD is sunlight, and very little is obtained from food. 7-dehydrocholesterol is converted in the skin to VD3 precursor upon exposure to ultraviolet B (280-310 nm). It isomerizes to VD3, which binds to vitamin D-binding protein. In the liver, VD3 attaches to vitamin D-binding protein and is hydroxylated by 25-hydroxylase to 25-hydroxyvitamin D3 [25(OH)D3], the main circulating form of VD. Later 25(OH)D is hydroxylated in the kidney and eventually converted to 1,25-dihydroxy VD3 [1,25-(OH)2D3][13,14]. Therefore, the main cause of VD deficiency is insufficient sun exposure[15], such as excessive indoor activity time and sun protection habits[16]. The Institute of Medicine defines VD deficiency as 25(OH)D below 20 ng/mL and VD deficiency as 25(OH)D below 21-29 ng/mL[17]. The literature shows that VD can regulate calcium and phosphorus metabolism[18], inhibit inflammation[19], regulate immune response[13], affect the intestinal barrier[20], and play an important role in the pathogenesis of diabetes[11], obesity, and IBS. This article provided an overview of research progress on the link between VD supplementation and the pathogenesis of IBS (Figure 1).
VD deficiency is closely related to IBS occurrence, development, and complications. Experiments by Nwosu et al[21], Cho et al[22], and Khayyat and Attar[23] showed that children and adults with IBS had insufficient or inadequate VD levels. Observational studies have also demonstrated that the prevalence of VD deficiency in IBS patients is as high as 82%[24]. Between April 2015 and April 2017, a prospective randomized controlled trial evaluated 112 VD-deficient adolescents aged 14 years to 18 years with IBS. Compared with the placebo, the clinical status of adolescents with IBS who took VD was significantly improved. This study suggests that VD supplementation effectively treats adolescent IBS[25].
Furthermore, a systematic review and meta-analysis assessed the efficacy of VD supplementation in improving IBS. Four randomized controlled trials found that VD supplementation improved symptoms and quality of life in people with IBS[26]. Nevertheless, Williams et al[27] conducted a randomized, double-blind, placebo-controlled study that demonstrated that there were no improvements in the IBS symptom severity and quality of life between the trial (VD supplementation) and placebo groups. However, the current research has not confirmed the clear pathogenesis of IBS. Many experimental results only prove a link between VD and IBS, but there is no definite explanation. Most of the guesses shown in the literature tend to be intestinal flora adjustment, inflammation inhibition, and mental relief in IBS patients.
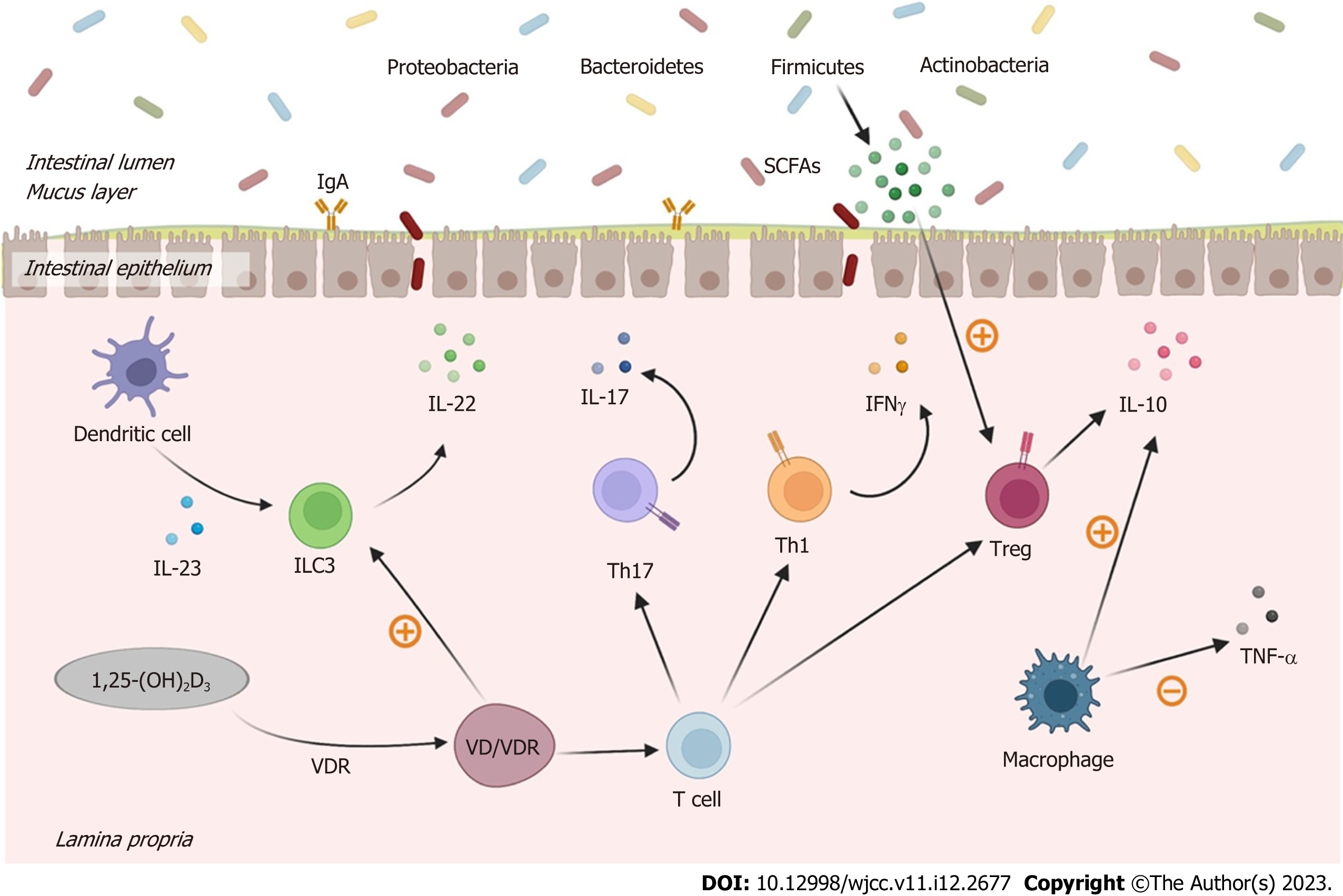
Gut microbial diversity maintains intestinal homeostasis, among which Firmicutes, Bacteroidetes, Proteobacteria, and Actinobacteria are the most important phyla. Disturbances in this microbial balance can lead to many diseases, including IBS[28]. However, VD supplementation may treat IBS by improving the type and abundance of gut microbes. A comprehensive systematic review of the gut microbiota and IBS revealed the presence of Enterobacteriaceae (phylum Proteobacteria), family Lactobacillaceae, and genus Bacteroides (phylum Bacteroidetes) in patients with IBS compared with normal individuals. In addition, IBS patients had potentially harmful microbiota, such as the family Lactobacillaceae and genus Bacteroides, which caused bloating and diarrhea[29]. VD is an essential hormone to maintain gut barrier function, along with many other roles in the gut[30]. Intervention studies in IBD have shown that VD alters the gut by increasing the relative abundance of beneficial bacteria (e.g., Ruminococcus, Akkermansia, Faecalibacterium, Lactococcus, Coprococcus, Bifidobacteria) and decreasing the Firmicutes microbial composition[28].
VD may play an immunomodulatory role by improving the gut microbiota. The intestinal epithelial barrier (IEB) is the primary interface between the in vitro and the in vivo environments[31]. In addition to absorbing water and nutrients, it is also responsible for defending against harmful substances. The IEB secures mucus, and substances are exchanged through intercellular and paracellular pathways. Meanwhile, in addition to secreting short-chain aliphatic hydrocarbons, such as acetate, propionate, and butyrate, specific gut microbes can also regulate the permeability of IEB[32]. Dysbiosis of gut microbes leads to a decrease in the abundance of short-chain aliphatic hydrocarbon-producing Akkermansia, Phaecococcus, and Coprococcus and an increase in the quantity of lipopolysaccharide-producing Enterobacteriaceae so that proinflammatory responses outweigh anti-inflammatory responses and cause intestinal inflammation[33]. Furthermore, Faecalibacterium prausnitzii increases butyrate production, which stimulates regulatory T (Treg) cell maturation, and better balances intestinal inflammation[33].
As an immunomodulator, VD can improve the gut microbiota[34], increase the production of antimicrobial peptides, improve the intestinal barrier, regulate the integrity of intestinal epithelial cells, inhibit helper T (Th) 1/Th17 cells, relieve Treg cells, and benefit the adaptive immune system[35]. The VD receptor (VDR) is a ligand-dependent transcription factor that could recognize 1,25-(OH)2D3[36]. VD requires the mediation of VDR to exert its biological actions[37]. The VD/VDR signaling pathway plays an inhibitory role in infection by activating the transcription of genes related to innate immunity[38], such as inducing and regulating autophagy[39]. Therefore, the VD/VDR axis may be an important inhibitor of inflammatory response. Under the influence of VD, macrophages can increase the secretion of interleukin (IL)-10 while reducing the secretion of tumor necrosis factor-α[40]. At the same time, studies have shown that the expansion of ILC3 requires VD, and the IL-22 secreted by ILC3 regulates epithelial tight junction proteins to enhance gut epithelial integrity and regulates the intestinal microbiota[41] (Figure 2).
Growing evidence suggests that the underlying pathophysiological mechanism of IBS is a disruption of brain-gut interactions. Up to 94% of IBS patients have also been diagnosed with psychiatric disorders[42], of which anxiety and depression are the most common[43]. Psychological stress alters gut motility and permeability, visceral sensitivity, immune response, and gut microbiota composition, leading to IBS[44]. Although research on VD and psychiatric disorders has not been well defined, there is evidence that adequate levels of VD are required for normal brain neuropsychiatric function and that VD regulated through brain cell differentiation, axonal growth, and calcium signaling, as well as neurotrophic factors, affect the brain[45]. In addition, VD can induce the expression of the tryptophan synthesis gene tryptophan hydroxylase 2 while inhibiting the expression of tryptophan hydroxylase 1, thereby preventing depression by maintaining normal serotonin levels[46]. Therefore, VD positively affects anxiety and depression in IBS patients.
Compared with the side effects of eating disorders and other drugs, VD supplements are significantly more effective, with only mild side effects. Long-term excessive VD intake is relatively rare. If the amount of VD supplementation is well-controlled, side effects can be effectively avoided[24]. It is also more convenient and efficient to get VD outdoors in sunlight. More research is needed to determine whether oral VD intake increases indoor exposure to ultraviolet B (280–310 nm) in people who work indoors for long periods.
IBS is a chronic gastrointestinal functional disorder whose etiology may be primarily relevant to gut microbiota and immune regulation. At the same time, VD can increase the number of beneficial bacteria in the gut, inhibit the inflammatory response, inhibit Th1/Th17 cells, stimulate Treg cells, and relieve the mental state of patients. However, the experiment of VD on IBS in the community population is more complicated, which increases the difficulty of the investigation and reduces the accuracy of the results. Hence, the treatment of VD on IBS is still controversial. In the future, it is necessary to carry out epidemiological studies on the relationship between VD and IBS, clinical studies on the efficacy of supplementing VD to improve IBS, and animal studies on the mechanism of VD improving IBS.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Choi YS, South Korea; Duan SL, China S-Editor: Liu XF L-Editor: Filipodia P-Editor: Zhang YL
| 1. | Altomare A, Di Rosa C, Imperia E, Emerenziani S, Cicala M, Guarino MPL. Diarrhea Predominant-Irritable Bowel Syndrome (IBS-D): Effects of Different Nutritional Patterns on Intestinal Dysbiosis and Symptoms. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 2. | Jang A, Hwang SK, Padhye NS, Meininger JC. Effects of Cognitive Behavior Therapy on Heart Rate Variability in Young Females with Constipation-predominant Irritable Bowel Syndrome: A Parallel-group Trial. J Neurogastroenterol Motil. 2017;23:435-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Simren M, Palsson OS, Whitehead WE. Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice. Curr Gastroenterol Rep. 2017;19:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 161] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 4. | Galica AN, Galica R, Dumitrascu DL. Epidemiology of Irritable Bowel Syndrome in Albania. J Gastrointestin Liver Dis. 2021;30:334-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Camilleri M. Sex as a biological variable in irritable bowel syndrome. Neurogastroenterol Motil. 2020;32:e13802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 6. | Grayson M. Irritable bowel syndrome. Nature. 2016;533:S101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Bonetto S, Fagoonee S, Battaglia E, Grassini M, Saracco GM, Pellicano R. Recent advances in the treatment of irritable bowel syndrome. Pol Arch Intern Med. 2021;131:709-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 8. | Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9399] [Cited by in RCA: 9398] [Article Influence: 522.1] [Reference Citation Analysis (1)] |
| 9. | Munns CF, Shaw N, Kiely M, Specker BL, Thacher TD, Ozono K, Michigami T, Tiosano D, Mughal MZ, Mäkitie O, Ramos-Abad L, Ward L, DiMeglio LA, Atapattu N, Cassinelli H, Braegger C, Pettifor JM, Seth A, Idris HW, Bhatia V, Fu J, Goldberg G, Sävendahl L, Khadgawat R, Pludowski P, Maddock J, Hyppönen E, Oduwole A, Frew E, Aguiar M, Tulchinsky T, Butler G, Högler W. Global Consensus Recommendations on Prevention and Management of Nutritional Rickets. Horm Res Paediatr. 2016;85:83-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 137] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 10. | Liu C, Lu M, Xia X, Wang J, Wan Y, He L, Li M. CORRELATION OF SERUM VITAMIN D LEVEL WITH TYPE 1 DIABETES MELLITUS IN CHILDREN: A META-ANALYSIS. Nutr Hosp. 2015;32:1591-1594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 11. | He LP, Song YX, Zhu T, Gu W, Liu CW. Progress in the Relationship between Vitamin D Deficiency and the Incidence of Type 1 Diabetes Mellitus in Children. J Diabetes Res. 2022;2022:5953562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Yao Y, Zhu L, He L, Duan Y, Liang W, Nie Z, Jin Y, Wu X, Fang Y. A meta-analysis of the relationship between vitamin D deficiency and obesity. Int J Clin Exp Med. 2015;8:14977-14984. [PubMed] |
| 13. | Medrano M, Carrillo-Cruz E, Montero I, Perez-Simon JA. Vitamin D: Effect on Haematopoiesis and Immune System and Clinical Applications. Int J Mol Sci. 2018;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 14. | Duchow EG, Sibilska-Kaminski IK, Plum LA, DeLuca HF. Vitamin D esters are the major form of vitamin D produced by UV irradiation in mice. Photochem Photobiol Sci. 2022;21:1399-1404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Cashman KD. Vitamin D Deficiency: Defining, Prevalence, Causes, and Strategies of Addressing. Calcif Tissue Int. 2020;106:14-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 198] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 16. | Bin Y, Kang L, Lili Y. Vitamin D status in irritable bowel syndrome and the impact of supplementation on symptoms: a systematic review and meta-analysis. Nutr Hosp. 2022;39:1144-1152. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911-1930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6974] [Cited by in RCA: 6793] [Article Influence: 485.2] [Reference Citation Analysis (0)] |
| 18. | Pludowski P, Holick MF, Grant WB, Konstantynowicz J, Mascarenhas MR, Haq A, Povoroznyuk V, Balatska N, Barbosa AP, Karonova T, Rudenka E, Misiorowski W, Zakharova I, Rudenka A, Łukaszkiewicz J, Marcinowska-Suchowierska E, Łaszcz N, Abramowicz P, Bhattoa HP, Wimalawansa SJ. Vitamin D supplementation guidelines. J Steroid Biochem Mol Biol. 2018;175:125-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 493] [Cited by in RCA: 425] [Article Influence: 60.7] [Reference Citation Analysis (0)] |
| 19. | Battistini C, Ballan R, Herkenhoff ME, Saad SMI, Sun J. Vitamin D Modulates Intestinal Microbiota in Inflammatory Bowel Diseases. Int J Mol Sci. 2020;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 20. | Yamamoto EA, Jørgensen TN. Relationships Between Vitamin D, Gut Microbiome, and Systemic Autoimmunity. Front Immunol. 2019;10:3141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 137] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 21. | Nwosu BU, Maranda L, Candela N. Vitamin D status in pediatric irritable bowel syndrome. PLoS One. 2017;12:e0172183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Cho Y, Lee Y, Choi Y, Jeong S. Association of the Vitamin D Level and Quality of School Life in Adolescents with Irritable Bowel Syndrome. J Clin Med. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Khayyat Y, Attar S. Vitamin D Deficiency in Patients with Irritable Bowel Syndrome: Does it Exist? Oman Med J. 2015;30:115-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 24. | Chong RIH, Yaow CYL, Loh CYL, Teoh SE, Masuda Y, Ng WK, Lim YL, Ng QX. Vitamin D supplementation for irritable bowel syndrome: A systematic review and meta-analysis. J Gastroenterol Hepatol. 2022;37:993-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | El Amrousy D, Hassan S, El Ashry H, Yousef M, Hodeib H. Vitamin D supplementation in adolescents with irritable bowel syndrome: Is it useful? Saudi J Gastroenterol. 2018;24:109-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Huang H, Lu L, Chen Y, Zeng Y, Xu C. The efficacy of vitamin D supplementation for irritable bowel syndrome: a systematic review with meta-analysis. Nutr J. 2022;21:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Williams CE, Williams EA, Corfe BM. Vitamin D supplementation in people with IBS has no effect on symptom severity and quality of life: results of a randomised controlled trial. Eur J Nutr. 2022;61:299-308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Tangestani H, Boroujeni HK, Djafarian K, Emamat H, Shab-Bidar S. Vitamin D and The Gut Microbiota: a Narrative Literature Review. Clin Nutr Res. 2021;10:181-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 29. | Pittayanon R, Lau JT, Yuan Y, Leontiadis GI, Tse F, Surette M, Moayyedi P. Gut Microbiota in Patients With Irritable Bowel Syndrome-A Systematic Review. Gastroenterology. 2019;157:97-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 453] [Article Influence: 75.5] [Reference Citation Analysis (0)] |
| 30. | Barbalho SM, Goulart RA, Araújo AC, Guiguer ÉL, Bechara MD. Irritable bowel syndrome: a review of the general aspects and the potential role of vitamin D. Expert Rev Gastroenterol Hepatol. 2019;13:345-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 31. | Turner JR. Intestinal mucosal barrier function in health and disease. Nat Rev Immunol. 2009;9:799-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2121] [Cited by in RCA: 2687] [Article Influence: 167.9] [Reference Citation Analysis (0)] |
| 32. | Barbara G, Barbaro MR, Fuschi D, Palombo M, Falangone F, Cremon C, Marasco G, Stanghellini V. Inflammatory and Microbiota-Related Regulation of the Intestinal Epithelial Barrier. Front Nutr. 2021;8:718356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 170] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 33. | Wellington VNA, Sundaram VL, Singh S, Sundaram U. Dietary Supplementation with Vitamin D, Fish Oil or Resveratrol Modulates the Gut Microbiome in Inflammatory Bowel Disease. Int J Mol Sci. 2021;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Skrobot A, Demkow U, Wachowska M. Immunomodulatory Role of Vitamin D: A Review. Adv Exp Med Biol. 2018;1108:13-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 35. | Lopez DV, Al-Jaberi FAH, Woetmann A, Ødum N, Bonefeld CM, Kongsbak-Wismann M, Geisler C. Macrophages Control the Bioavailability of Vitamin D and Vitamin D-Regulated T Cell Responses. Front Immunol. 2021;12:722806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 36. | Lee KY, Choi HS, Chung KY, Lee BJ, Maeng HJ, Seo MD. Quercetin Directly Interacts with Vitamin D Receptor (VDR): Structural Implication of VDR Activation by Quercetin. Biomol Ther (Seoul). 2016;24:191-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Clark A, Mach N. Role of Vitamin D in the Hygiene Hypothesis: The Interplay between Vitamin D, Vitamin D Receptors, Gut Microbiota, and Immune Response. Front Immunol. 2016;7:627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 106] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 38. | Ismailova A, White JH. Vitamin D, infections and immunity. Rev Endocr Metab Disord. 2022;23:265-277. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 161] [Article Influence: 53.7] [Reference Citation Analysis (0)] |
| 39. | Hou Y, Li J, Deng C. Vitamin D/vitamin D receptor, autophagy, and infection. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2022;47:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 40. | Fakhoury HMA, Kvietys PR, AlKattan W, Anouti FA, Elahi MA, Karras SN, Grant WB. Vitamin D and intestinal homeostasis: Barrier, microbiota, and immune modulation. J Steroid Biochem Mol Biol. 2020;200:105663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 140] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 41. | Lin YD, Arora J, Diehl K, Bora SA, Cantorna MT. Vitamin D Is Required for ILC3 Derived IL-22 and Protection From Citrobacter rodentium Infection. Front Immunol. 2019;10:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 177] [Cited by in RCA: 263] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 42. | Liu T, Gu X, Li LX, Li M, Li B, Cui X, Zuo XL. Microbial and metabolomic profiles in correlation with depression and anxiety co-morbidities in diarrhoea-predominant IBS patients. BMC Microbiol. 2020;20:168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 43. | Bercik P. The Brain-Gut-Microbiome Axis and Irritable Bowel Syndrome. Gastroenterol Hepatol (N Y). 2020;16:322-324. [PubMed] |
| 44. | Tang HY, Jiang AJ, Wang XY, Wang H, Guan YY, Li F, Shen GM. Uncovering the pathophysiology of irritable bowel syndrome by exploring the gut-brain axis: a narrative review. Ann Transl Med. 2021;9:1187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 45. | Zhang Z, Yang X, Jia Y, Wen Y, Cheng S, Meng P, Li C, Zhang H, Pan C, Zhang J, Chen Y, Zhang F. Vitamin D and the Risks of Depression and Anxiety: An Observational Analysis and Genome-Wide Environment Interaction Study. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 46. | Berridge MJ. Vitamin D and Depression: Cellular and Regulatory Mechanisms. Pharmacol Rev. 2017;69:80-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |