Published online Apr 16, 2023. doi: 10.12998/wjcc.v11.i11.2502
Peer-review started: December 2, 2022
First decision: January 5, 2023
Revised: January 14, 2023
Accepted: March 21, 2023
Article in press: March 21, 2023
Published online: April 16, 2023
Processing time: 125 Days and 2.5 Hours
We aimed to investigate the effectiveness of endoscopic retrograde cholangiopancreatography (ERCP) for treating obstructive jaundice (OJ) post hepatoblastoma (HB) surgery (post-HB OJ) by analyzing the data of a case and performing a literature review.
Clinical data of one patient with post-HB OJ treated by ERCP were retrospectively analyzed. Furthermore, clinical characteristics and insights into the diagnosis and treatment of post-HB OJ in children were summarized via searching various databases and platforms, such as China National Knowledge Infrastructure, Wanfang database, CQVIP database, PubMed, Ringer Link, and Google Scholar. The patient reported herein underwent five chemotherapy sessions after the diagnosis of HB and right hemihepatectomy after tumor size reduction; these were followed by two postoperative chemotherapy sessions. Three months postoperatively, the patient developed icteric sclera, strong tea-colored urine, and clay-like stools, and showed signs of skin itchiness; blood analysis showed significantly an increased conjugated bilirubin (CB) level (200.3 μmol/L). Following the poor efficacy of anti-jaundice and hepatoprotective treatments, the patient underwent ERCP. Intraoperative imaging showed a dilated bile duct in the porta hepatis with significant distal stenosis. A 5 Fr nasopancreatic tube was placed in the dilated area through the stricture for external drainage, and the patient was extubated on postoperative day 6. Postoperatively, the patient’s stool turned yellow, and the CB level decreased to 78.2 μmol/L. Fifteen days later, ERCP was repeated due to unrelieved jaundice symptoms, wherein a 7 Fr naso
Post-HB OJ is rare. Compared to biliary tract reconstruction, ERCP is less invasive and has a better therapeutic effect.
Core Tip: This study aimed to investigate the effectiveness of endoscopic retrograde cholangiopancreatography (ERCP) in the treatment of obstructive jaundice following hepatoblastoma surgery by analyzing the data of a case and performing a literature review. We found that ERCP is less invasive and has a better therapeutic effect compared to biliary tract reconstruction.
- Citation: Shu J, Yang H, Yang J, Bian HQ, Wang X. Application of endoscopic retrograde cholangiopancreatography for treatment of obstructive jaundice after hepatoblastoma surgery: A case report. World J Clin Cases 2023; 11(11): 2502-2509
- URL: https://www.wjgnet.com/2307-8960/full/v11/i11/2502.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i11.2502
Hepatoblastoma (HB) is a common malignant, solid tumor that affects children’s livers and accounts for approximately two-thirds of all liver malignancies; it has an overall survival rate of 70% to 80%[1]. Presently, a surgery-based multidisciplinary management strategy with chemotherapy is the standard treatment modality for HB. HB-related postoperative complications include obstructive jaundice (OJ), which is rare. OJ is manifested clinically as generalized yellowing of the skin and sclera, skin pruritus, yellow urine, and clay-like stools. Furthermore, perioperative liver function impairment, biliary tract infection, and liver failure are also observed, and they critically affect the patient’s postoperative recovery[2]. The effectiveness and safety of endoscopic retrograde cholangiopancreatography (ERCP) in the management of adult biliary and pancreatic diseases are well known; however, its application in children is scarce due to the low incidence of biliopancreatic diseases in children, lack of relevant pediatric instruments, special characteristics associated with pediatric cases, and operational difficulties. This paper reports a case of post-HB surgery OJ (post-HB OJ) treated by ERCP. Moreover, effective diagnosis and treatment methods are explored based on a literature review.
A one-year-old female child presented to a local hospital with an abdominal mass.
The patient presented with icteric sclera and symptoms of itchy skin at 3 mo after a right hemihepatectomy.
The patient was examined and diagnosed with HB for which she underwent five chemotherapy sessions and a right hemihepatectomy after tumor size reduction. These were followed by two postoperative chemotherapy sessions. These were followed by two postoperative chemotherapy sessions.
Strong tea-colored urine and clay-like stools were reported. Blood examinations revealed significantly increased conjugated bilirubin (CB) (200.3 μmol/L) and total bilirubin (293.6 μmol/L) levels.
The patient’s gamma-glutamyl transpeptidase (1834 U/L), alanine transaminase (104 U/L), and aspartate aminotransferase (210 U/L) levels were elevated. However, atomolam, inosine, intravenous ornithine aspartate drip, oral ursodeoxycholic acid, and compound glycyrrhizin tablet administered at the local hospital proved ineffective.
Magnetic resonance cholangiopancreatography (MRCP) showed a dilated bile duct in the porta hepatis (widest diameter, approximately 12 mm) (Figure 1).
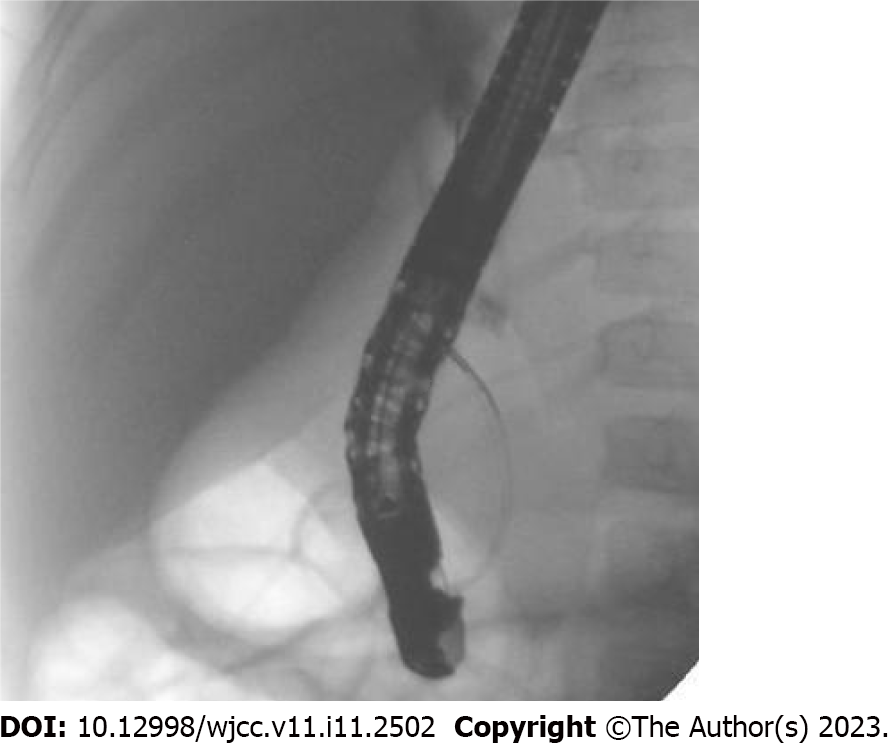
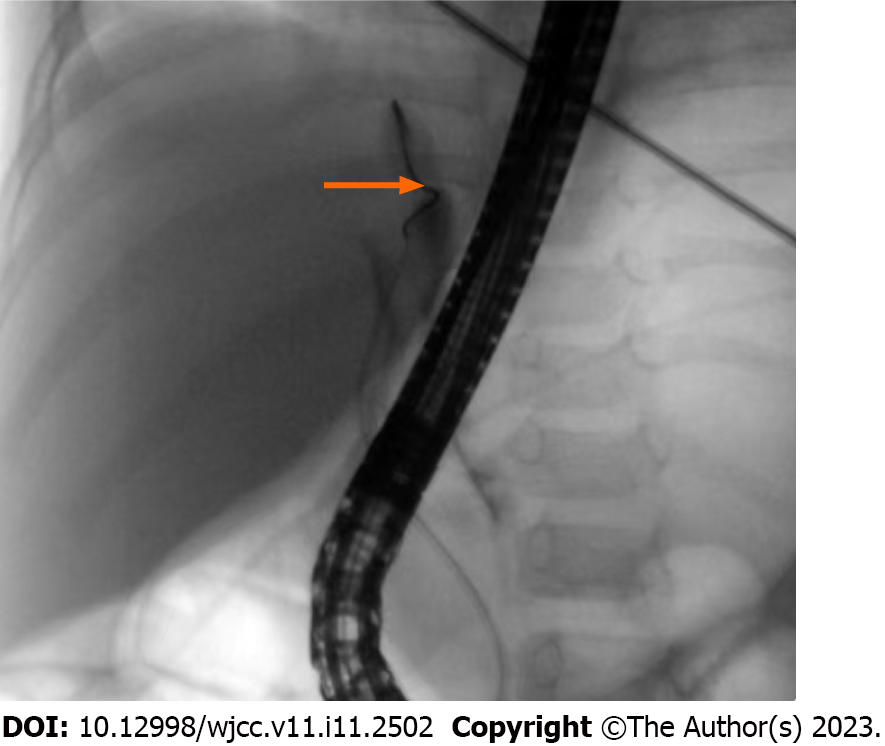
The patient underwent ERCP under general anesthesia in our hospital. After routine intubation, MRCP showed a slender common bile duct (2 mm) and contrast agent accumulation in the porta hepatis, and the intrahepatic bile duct and the middle and lower common bile ducts could not be visualized (Figure 2). Pressurized contrast imaging demonstrated a dilated bile duct in the porta hepatis with significant stenosis at its distal terminal. The difficult passage at this site caused the guidewire to bend, leading to a filling defect (Figure 3).
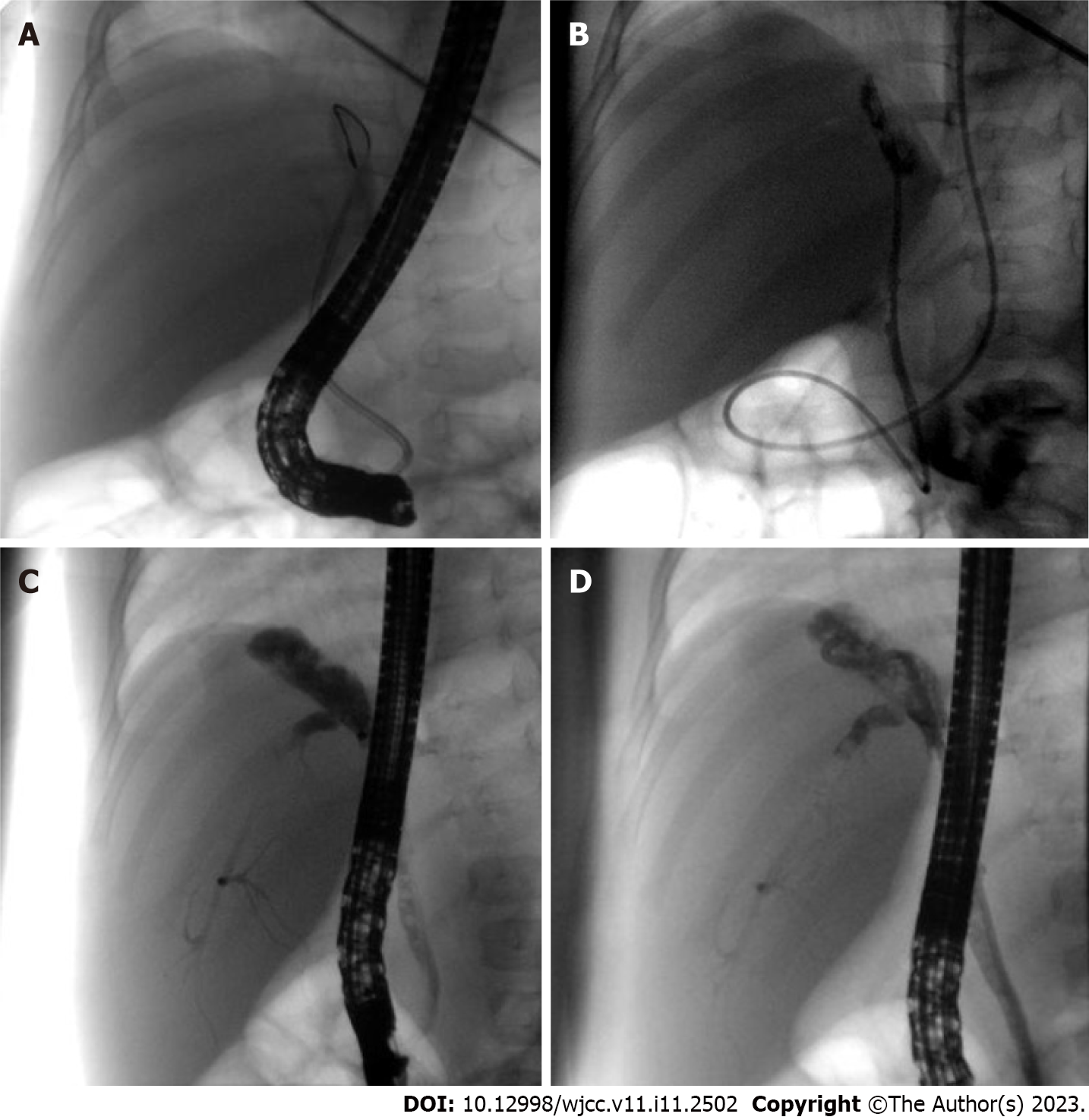
A 7 Fr nasobiliary drainage tube could not pass through the stricture (Figure 4A), and with great difficulty, a 6 Fr nasobiliary drainage tube was passed through. Subsequently, on poatoperative day 6, a 5 Fr nasopancreatic tube was placed at the dilatation through the stricture for external drainage (Figure 4B) and the patient was extubated. During this time, the patient’s stools turned yellow, and the CB level decreased to 78.2 μmol/L. Fifteen days later, ERCP was repeated due to unalleviated jaundice symptoms. Although the imaging results still suggested bile duct dilatation in the porta hepatis, the intrahepatic bile duct, and the lower and middle common bile ducts could not be visualized (Figure 4C), along with balloon dilatation of the stenosis. Finally, a 7 Fr nasobiliary drainage tube was successfully inserted (Figure 4D).
Three months after the second ERCP, the patient’s jaundice symptoms mostly resolved; furthermore, the patient’s CB level decreased to 33.2 μmol/L. A one-year follow-up revealed that the jaundice symptoms had disappeared and the patient had normal bilirubin level.
China National Knowledge Infrastructure, Wanfang database, CQVIP database, PubMed, Ringer Link, and Google Scholar were searched until April 2022 with the keywords hepatoblastoma, obstructive jaundice, and biliary obstruction. The inclusion criteria for the studies were as follows: (1) Patients with a diagnosis of HB with surgical treatment; (2) Those with postoperative OJ; and (3) Those who underwent treatment of OJ via surgical methods, including biliary tract reconstruction and ERCP. Duplicate cases reported by the same author, institute, hospital, and database were excluded.
Five studies that met the requirements were included in the review; two studies were written in English and three in Chinese. A total of six cases were analyzed, of which five met the inclusion criteria. One patient with HB developed post-HB OJ and died of liver failure without surgical treatment and was excluded from the review. Finally, five patients from the retrieved studies and the patients in this case report were included (Table 1). All children presented with post-HB OJ within 14 d to 4 mo postoperatively. Five patients developed OJ due to intraoperative biliary injury; whereas, one patient developed OJ and elevated liver stiffness which was attributed to biliary injury-related bile leakage[3]. Furthermore, one patient developed biliary obstruction due to a postoperatively regenerated liver that compressed the bile duct[4]. Four patients underwent biliary tract reconstruction[3-6] and recovered well postoperatively. One patient developed severe malnutrition post percutaneous transhepatic cholangial drainage (PTCD); however, subsequent biliary tract reconstruction facilitated good recovery[7]. As mentioned previously, the patient in this report was treated by ERCP and recovered well after surgery.
| Ref. | Case | Age (mo) | Sex | Surgery | Time of postoperative obstructive jaundice | Reason | Solution | Prognosis |
| Canty[4], 1991 | 2 | 6 | Male | Right hemihepatectomy | 4 mo | Postoperative liver regeneration caused biliary obstruction | Biliary tract reconstruction operation | Good |
| 2 | Male | Right hemihepatectomy | 14 d | Postoperative liver regeneration caused biliary obstruction | - | Died of jaundice and liver failure 4 mo after surgery | ||
| Murphy et al[7], 2012 | 1 | 12 | Female | Right hemihepatectomy | 2.5 mo | Left hepatic duct injury | PTCD failed followed by biliary tract reconstruction operation | Good |
| Liu et al[5], 2015 | 1 | 1 | — | — | — | Right hepatic duct injury | Biliary tract reconstruction operation | Good |
| Yao et al[6], 2018 | 1 | 11 | Male | Left hemihepatectomy and VII/VIII section resection | 16 d | Right hepatic duct injury | Biliary tract reconstruction operation | Good |
| Feng et al[3], 2020 | 1 | — | — | — | — | Biliary tract injury forms biliary leakage | Biliary tract reconstruction operation | Good |
| This Study | 1 | 12 | Female | Right hemihepatectomy | 3 mo | Hepatic duct injury | ERCP | Good |
Post-HB OJ is a rare complication and is associated with injury or compression of trunk ducts, such as the right or left hepatic ducts. Incomplete ligation of small bile ducts in the hepatectomy section dislodged ligatures, and necrosis are responsible for bile leakage. In five of the six children included in this review, OJ developed due to injury to the main hepatic duct. Moreover, a rare case of OJ due to postoperative liver regeneration was also noted[4]. Remarkable liver regeneration is observed post hepatectomy, which is typically initiated within a few days postoperatively and is completed within a few months. Rapid macronodular regeneration of the liver leads to stretching, compression, and eventual ischemic fibrosis of the extrahepatic biliary system, resulting in OJ. One child in this review developed postoperative bile leakage due to damage to the main hepatic duct. However, the bile leakage did not resolve after drainage, and local infection and encapsulated effusion were observed. Long-term conservative treatment led to inflammatory scar formation and tissue fragility around the bile leakage site, leading to OJ and increased liver stiffness[3]. However, damage to the main hepatic duct does not consistently lead to bile leakage. In one child, the left hepatic duct was ligated extremely close to the common hepatic duct, resulting in a slight angle at the convergence of the right hepatic duct into the common hepatic duct and causing OJ due to poor bile flow[6].
Children with biliary tract infections present with abdominal pain. In addition, children who develop OJ after bile leakage may present with intestinal obstruction, localized and systemic infections, and liver stiffness due to severe abdominal infection. In such cases, hematological tests may demonstrate elevated total bilirubin levels, especially CB levels, with increased transaminases. Ultrasound is the preferred diagnostic modality for biliary obstruction because it is noninvasive, simple, efficient, and economical. However, computed tomography (CT), MPCP, and ERCP are required for confirming the diagnosis. Enhanced CT can demonstrate the tumor’s recurrence post-HB surgery, locate the bile duct obstruction site, and determine the degree of bile duct dilatation. Additionally, it can also characterize the morphology and thickness of the bile duct wall. The diagnostic value of MRCP for pancreaticobiliary duct disease is well recognized as it clearly shows the pancreatic-bile duct structure; however, it is not ideal for diagnosing microscopic stones or lesions when pancreaticobiliary duct obstruction and dilatation are not apparent, especially when combined with ascites.
Effective treatments for post-HB OJ include biliary tract reconstruction, PTCD, and ERCP, of which biliary tract reconstruction is the most commonly used method. Despite its definite efficiency, its drawbacks are apparent, including the need for re-laparotomy for choledochojejunostomy and major surgical strikes. PTCD puncture requires a skilled surgeon with expertise in X-ray or ultrasound-guided puncture, and the continuous flow of bile into the abdominal cavity after failed catheterizing leads to acute peritonitis, requiring emergency surgery in severe cases[8]. PTCD is more effective for bile drainage; however, it is prone to complications, such as drainage tube blockage, infection, dislodgement, and bile loss, which cause an imbalance in the internal homeostasis of the body. Furthermore, pediatric care is highly demanding. Despite managing jaundice by external drainage with PTCD, one child developed severe malnutrition; however, the final biliary tract reconstruction facilitated spontaneous recovery[7]. Compared to ERCP, placement of inner support via PTCD is a highly traumatic procedure with the formation of a dead zone and is prone to migration into the duodenum, thus possibly triggering intestinal perforation[9].
Biliary stricture is a common complication observed post-liver transplantation and biliary surgery in adults. Its incidence after liver transplantation and due to direct injury during cholecystectomy is approximately 10%-40% and 0.5%, respectively[10,11]. Placement of balloon-dilated stents via the ERCP route for biliary strictures is safe, effective, minimally invasive, and the first-line treatment option for benign biliary strictures[12]. ERCP is the preferred treatment modality for simple anastomotic stenosis combined with bile duct calculi and can remarkably improve a patient’s clinical symptoms and quality of life; however, patients undergoing ERCP require multiple removals and replacements of plastic stents with poor biocompatibility. Biodegradable biliary stents and tectorial self-expanding metal stents are used clinically and have a longer drainage time and reduce the frequency of stent replacements in a short period. ERCP has a low cure rate in patients with non-anastomotic strictures, especially diffuse strictures combined with calculus; nevertheless, it can provide short-term relief by alleviating the patient’s clinical symptoms and improving the general condition. Thus, ERCP can be used as a transitional treatment modality. Moreover, failures of ERCP or poor treatment outcomes do not aggravate the patients’ clinical conditions, and PTCD or surgical treatment is still feasible.
The lower frequency of ERCP use as a treatment modality in children compared to adults may be attributed to the relatively low probability of ERCP use in childhood, lack of physicians with extensive relevant experience, and lack of specialized equipment for children[13]. Recent years has witnessed increased use of ERCP for the treatment of pediatric pancreaticobiliary diseases, including congenital pancreaticobiliary diseases, biliary calculi, biliary strictures, pancreas divisum, and acute and chronic pancreatitis in children. This can be attributed to the advancements of duodenoscopic techniques in children and the involvement of adult endoscopists. Although MRCP has become a routine imaging modality for biliary obstructive disease, ERCP remains the gold standard for the diagnosis of biliary obstructive diseases since it allows for simultaneous examination and treatment[14]. The goal of biliary obstruction treatment is long-term bile duct decompression and maintenance of bile duct patency, and endoscopic balloon dilation followed by placement of stents is one of the primary treatment modalities. Jaundice symptoms of our case disappeared 6 mo after the placement of a 7 Fr nasobiliary drainage tube via ERCP, and normal bilirubin levels were observed. In addition, the patient lived normally after extubation. Based on the results of a subsequent follow-up examination of the child, a 9 Fr biliary stent can be considered feasible for dilation and drainage when necessary. Despite the good efficacy of external nasobiliary drainage under ERCP, the tube had to be placed for a long period, remarkably influencing her and her family members. Therefore, placement of a biliary stent under ERCP for internal drainage may be a more optimal option for the treatment of biliary obstruction[15].
We recommend patients who meet the following indications to apply ERCP procedure: (1) Patients who are 10 kg or over or 1 year old or over; (2) A history of hepatectomy which may cause iatrogenic biliary stricture during surgery; and (3) Postoperative clinical findings, laboratory examination, and imaging examination results suggested biliary obstruction.
The effectiveness of ERCP in treating these cases is also affected by the following factors: (1) Scope of the first surgical resection and the degree of bile duct injury; (2) The patient's own ability to repair and regenerate the biliary tract; (3) The patient's degree of adaptation to biliary balloon dilatation; (4) The unobstructed time of the bile stent; and (5) Biliary tract infection and systemic infection of the patient. And the need of multiple ERCP operations is also the limitation of the therapy.
In summary, post-HB OJ is rare. ERCP aids in avoiding unnecessary surgical procedures, is less invasive, and shows better treatment outcomes than biliary tract reconstruction.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Thailand; Rashid R, Bangladesh S-Editor: Li L L-Editor: Wang TQ P-Editor: Li L
| 1. | Hiyama E, Hishiki T, Watanabe K, Ida K, Yano M, Oue T, Iehara T, Hoshino K, Koh K, Tanaka Y, Kurihara S, Ueda Y, Onitake Y. Mortality and morbidity in primarily resected hepatoblastomas in Japan: Experience of the JPLT (Japanese Study Group for Pediatric Liver Tumor) trials. J Pediatr Surg. 2015;50:2098-2101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Saxena P, Kumbhari V, Zein ME, Khashab MA. Preoperative biliary drainage. Dig Endosc. 2015;27:265-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Feng J, Wang HM, Qin H, Yang W, Han W, Cheng HY, Chang XF, Zhu ZY, Han JY. [Diagnosis and treatment of postoperative biliary fistula in children with hepatoblastoma]. Zhonghua Xiaoer Waike Zazhi. 2020;19:794-799. [DOI] [Full Text] |
| 4. | Canty TG Sr. Biliary obstruction from hepatic regeneration following extended right hepatectomy for tumor. J Pediatr Surg. 1991;26:830-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Liu GB, Liu BH, Ma YY, Li K, Dong KR. [Neonatal hepatoblastoma: a report of 8 cases with a literature review]. Zhonghua Xiaoer Waike Zazhi. 2015;36:269-272. [DOI] [Full Text] |
| 6. | Yao W, Dong KR, Xiao XM, Zheng JC, Li Km, Liu XQ, Liu BH, Zheng S. [Associating liver partition and portal vein ligation for staged hepatectomy for hepatoblastoma: a report of one case]. Zhonghua Xiaoer Waike Zazhi. 2018;39:597-603. [DOI] [Full Text] |
| 7. | Murphy AJ, Rauth TP, Lovvorn HN 3rd. Chronic biloma after right hepatectomy for stage IV hepatoblastoma managed with Roux-en-Y biliary cystenterostomy. J Pediatr Surg. 2012;47:e5-e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Du CX, Li JX, Li DR, Su MB, Ya XQ, Wang WB, Liu JH. [A study comparing PTCD with ENBD on jaundiced patients before laparoscopic pancreaticoduodenectomy]. Zhonghua Gandan Waike Zazhi. 2022;28:4. [DOI] [Full Text] |
| 9. | Sun D, Liu YG, Yang JQ, Liu S, Zhu GQ. [Therapeutic effect of PTCD in combination with ERCP on malignant obstructive jaundice]. Zhonghua Gandan Waike Zazhi. 2010;(4):308-309. [DOI] [Full Text] |
| 10. | Hildebrand T, Pannicke N, Dechene A, Gotthardt DN, Kirchner G, Reiter FP, Sterneck M, Herzer K, Lenzen H, Rupp C, Barg-Hock H, de Leuw P, Teufel A, Zimmer V, Lammert F, Sarrazin C, Spengler U, Rust C, Manns MP, Strassburg CP, Schramm C, Weismüller TJ; German PSC Study Group. Biliary strictures and recurrence after liver transplantation for primary sclerosing cholangitis: A retrospective multicenter analysis. Liver Transpl. 2016;22:42-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 11. | Grönroos JM. Endoscopic management of postcholecystectomy bile duct strictures. J Am Coll Surg. 2008;207:786-7; author reply 787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Kuroda Y, Tsuyuguchi T, Sakai Y, K C S, Ishihara T, Yamaguchi T, Saisho H, Yokosuka O. Long-term follow-up evaluation for more than 10 years after endoscopic treatment for postoperative bile duct strictures. Surg Endosc. 2010;24:834-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Jang JY, Yoon CH, Kim KM. Endoscopic retrograde cholangiopancreatography in pancreatic and biliary tract disease in Korean children. World J Gastroenterol. 2010;16:490-495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Park ET. Endoscopic Retrograde Cholangiopancreatography in Bilioenteric Anastomosis. Clin Endosc. 2016;49:510-514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Sun B, Yu D, Chen J, Tang Y, Wu H. Endoscopic biliary drainage management for children with serious cholangitis caused by congenital biliary dilatation. Pediatr Surg Int. 2018;34:897-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |