Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2604
Peer-review started: October 2, 2021
First decision: December 10, 2021
Revised: December 14, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: March 16, 2022
Processing time: 159 Days and 12.6 Hours
Mantle cell lymphoma (MCL) is a subtype of Non-Hodgkin's lymphoma (NHL). MCL frequently affects extranodal sites while endobronchial involvement is uncommon. Only 5 cases of MCL with endobronchial involvement have been previously reported.
A 56-year-old male patient arrived at the hospital complaining of a dry cough. A mass in the right upper lobe of the lung was revealed in Chest computed tomography (CT). Right lung hilar and mediastinal lymphadenopathies were also found by CT scan. The patient was diagnosed with central-type lung cancer with multiple lymph node metastases after positron emission tomography (PET) CT scan examination. The fiber optic bronchoscope examination revealed diffuse neoplasm infiltration in the inlet of the right up lobar bronchus. The patient was finally diagnosed with MCL based on the bronchoscopy and mediastinoscopy biopsy results.
MCL could masquerade as central type lung cancer. An endobronchial biopsy examination is necessary for the early diagnosis of MCL.
Core Tip: We reported a case of mantle cell lymphoma (MCL) with endobronchial involvement. MCL with endobronchial involvement is very rare. Only five such cases have been previously reported. Positron emission tomography - computed tomography is recommended for differential diagnosis and detection of extranodal sites of MCL. A pathological diagnosis can be made based on an endobronchial biopsy by bronchoscopy but doctors should prompt efforts to establish enough tissues.
- Citation: Ding YZ, Tang DQ, Zhao XJ. Mantle cell lymphoma with endobronchial involvement: A case report. World J Clin Cases 2022; 10(8): 2604-2609
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2604.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2604
Mantle cell lymphoma (MCL) is a subtype of Non-Hodgkin's lymphoma (NHL). Over expression of cyclin D1 and reciprocal chromosomal translocation t(11;14)(q13;q32) are the distinguishing features of MCL[1,2]. MCL represents approximately 4%-6% of all NHL[3,4]. This disease is more often diagnosed in male patients in their 60s and almost all patients present with advanced stages III–IV of the disease. Extranodal involvements, include the bone marrow, gastrointestinal tract, liver, spleen, skin, Waldeyer's ring, lacrimal glands and central nervous system, are very common[5,6]. Even though, airway involvement is very rare[7-9]. We represent here a case of MCL with endobronchial as well as multiple lymph node involvement. Bronchoscopy and mediastinoscopy biopsies of the endobronchial and mediastinal lymph nodes were done to confirm the diagnosis.
A 56-year-old male patient arrived at the hospital complaining of dry cough for two months.
The patient suffered from dry cough for the past two months prior to his visit to our hospital. The chest computed tomography (CT) scan performed at the local hospital revealed a mass in the right upper lobe of the lung, with right lung hilar and mediastinal lymphadenopathies.
The patient had no prior medical history and was a smoker with 30 pack-years.
The patient was healthy and have no personal or family history of tumors.
The patient presented mild coarse breath sounds in the right upper lung during auscultation.
Laboratory tests revealed an increased percentage of neutrophilic leukocytes (78.4%) with normal hematocrit and platelet count values. His CYFRA 21-1 level was 4.03 ng/mL, which was far above the maximum normal limit (3.3 ng/mL). Other tumor markers were all in the normal range.
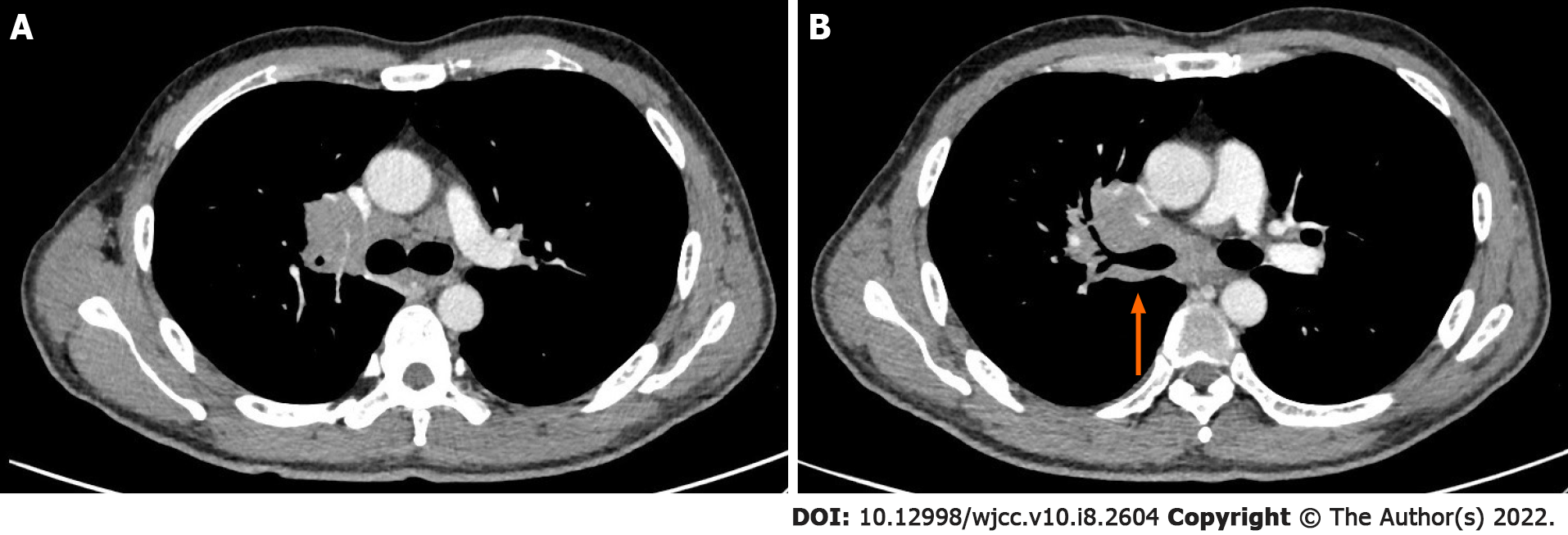
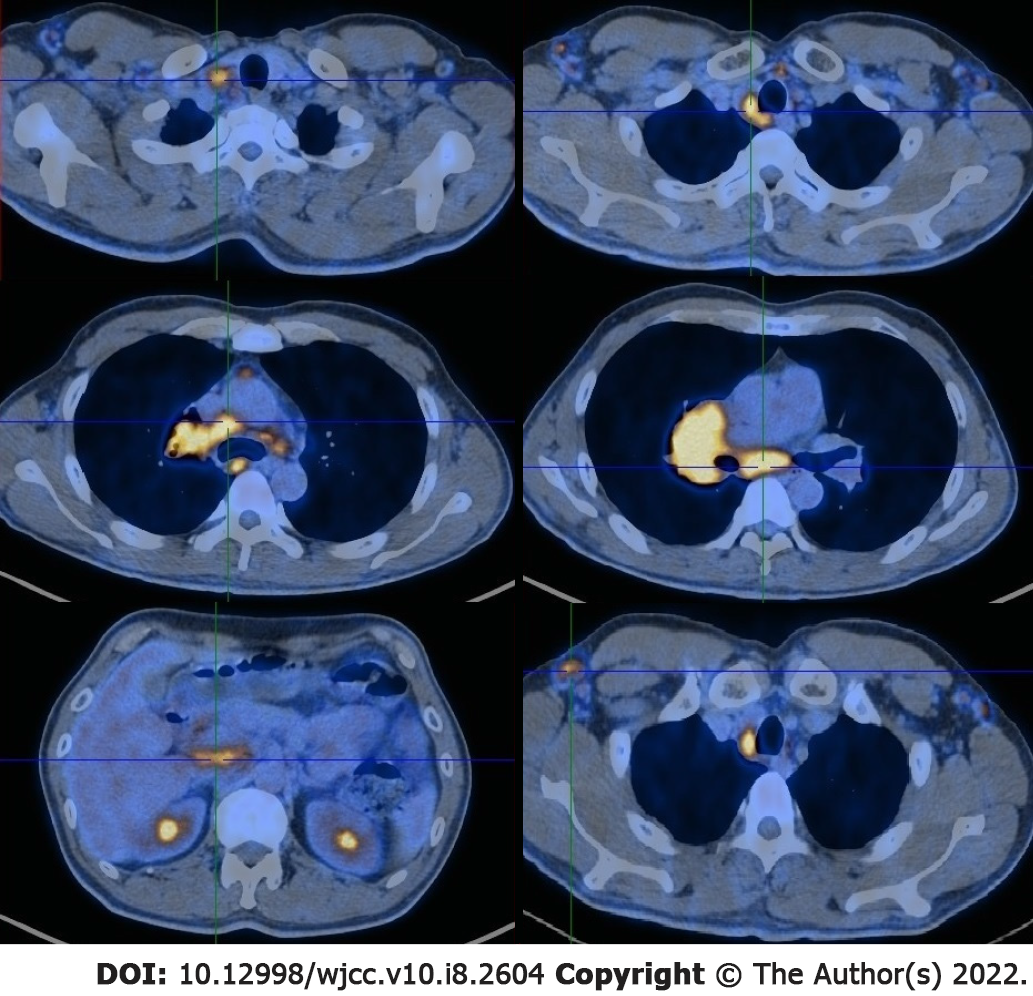
Chest enhanced CT scans revealed a central-type mass in the right lung with enlarged lymph nodes in the right lung hilar, mediastinal and bilateral axillary areas (Figure 1A). The CT also displayed thickening of the right bronchial wall (Figure 1B). PET-CT showed an increased uptake of 18-fludeoxyglucose in the mass of the right lung hilum and the fear of malignancy was a major concern. This examination also revealed lymph node metastases in the right lung hilar, mediastinal, celiac, right cervical, right supraclavicular and bilateral axillary areas (Figure 2).
Flexible bronchoscopy revealed mucosal infiltrative changes at the level of the right upper lobe inlet and the right upper lobe bronchus was obstructed (Figure 3). The other bronchial mucosa was normal. The mucosal endobronchial biopsy at the level of the right upper lobe inlet showed lymphoid hyperplasia. These cells were CD20 positive B-cells and Bcl-2, CD5, CD19, and cyclin D1 were also expressed. This result indicates the possibility of MCL. As the tissue sample of the endobronchial biopsy was insufficient, a mediastinoscopy biopsy of the mediastinal lymph nodes was scheduled.
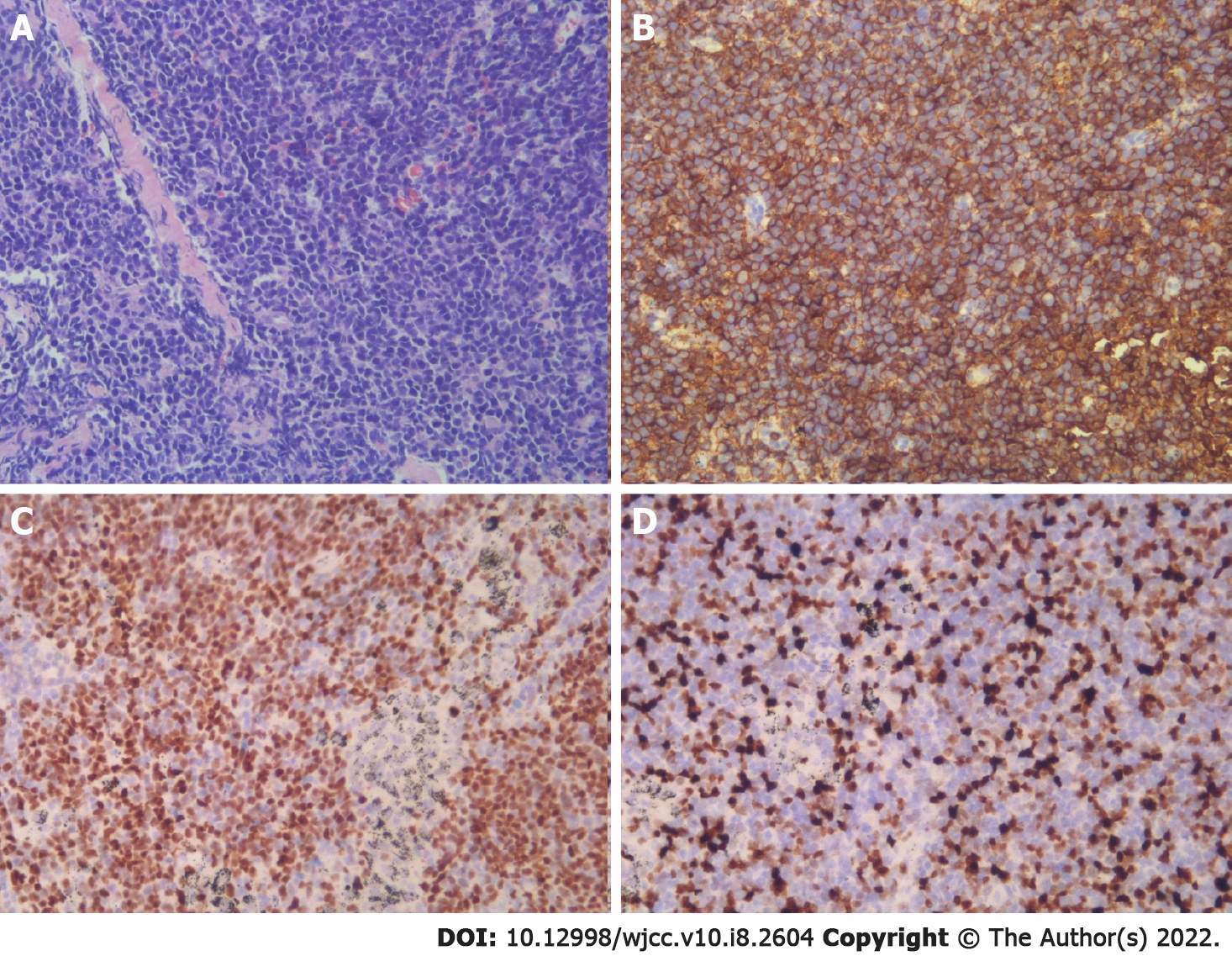
Subcarinal lymph node biopsy was performed under mediastinoscopy. The specimen also showed lymphoid hyperplasia. The immunohistochemical staining showed that these cells were positive for Bcl-2, CD5, CD19, CD20, Cyclin D1 and SOX11 while negative for Bcl-6, CD3, CD10, CD21 and CD23. The percentage of Ki67 positive cells was 25% (Figure 4). Therefore, the diagnosis of MCL was confirmed.
The final diagnosis for this patient was MCL.
After the diagnosis of MCL, the patient was transferred to the hematology department of another hospital. The therapy was proceeded to rituximab and bendamustine maintenance.
The review of recent communication exchanges with his wife indicated that he was tolerating chemo
MCL is a kind of B cell aggressive NHL with the feature of hyperplasia of B-cells. These B-cells is a subset arising from antigen-experienced B cells resembling those found in the follicular mantle zones [1]. Immunohistochemical staining was positive for Bcl-2, CD5, CD19, CD20 and cyclin D1 and negative for Bcl-6, CD10 and CD23[9]. According to the latest research, SOX11 has been described as a very important diagnostic marker when cyclin D1 is negative as it is equally expressed in D1-positive and D1-negative MCL[9].
Although MCL was more likely to have extranodal involvement, endobronchial involvement is uncommon[5,6]. As far as we know, only 5 cases of MCL with tracheobronchial involvement have been represented in the literature (Table 1)[1,2,10-12]. Lymphoma with endobronchial involvement is divided into two types: Diffuse submucosal infiltration (type I) and localized solitary mass (type II)[13]. Interestingly, all 5 cases exhibited a type I pattern[13]. In contrast, the case presented in this report exhibited a type II pattern, and the mechanisms of endobronchial metastasis may be caused by direct bronchial invasion from a parenchymal mass or mediastinal mass.
| Ref. | Age | Gender | Time between MCL first diagnosis and endobronchial involvement | Smoking history | Presenting symptoms | CyclinD1 |
| Figgis et al[10] | 53 | Female | More than three years (second relapse) | N/A | Cough, dyspnoea, wheeze | N/A |
| Miyoshi et al[11] | 70 | Female | Five years (fifth relapse) | N/A | Stridor, respiratory failure | Positive |
| Imai et al[12] | 86 | Male | Two years (first relapse) | N/A | Dyspnoea | N/A |
| Katono et al[2] | 87 | Male | 0 (diagnosed by endobronchial biopsy) | Never-smoker | Dyspnoea on exertion | Positive |
| Tong et al[1] | 65 | Male | 0 (diagnosed by endobronchial biopsy) | Current smoker with 40 pack-years | Productive cough, dyspnoea | Positive |
| Current case | 56 | Male | 0 (diagnosed by endobronchial biopsy) | Current smoker with 30 pack-years | Cough | Positive |
Type II endobronchial MCL has a large chance of being diagnosed as central-type lung cancer. PET-CT was useful in the differential diagnosis and detection of extranodal involvement. In addition, for detecting both nodal and extranodal involvement in patients with MCL, PET has a high sensitivity[14].
The diagnosis of MCL should be made on the basis of lymph node biopsy results, tissue, bone marrow, or blood phenol type[5]. Typical positive results of immunohistochemistry and morphology of infiltrating small-to-medium-sized cells were displayed in most cases[15]. In cases where endobronchial involvement is suspected, bronchoscopy with endobronchial biopsy results is an important and useful diagnostic tool. However, it is worth mentioning that the sample of tissue may be too small to determine a pathological diagnosis. In this case report, the patient underwent mediastinoscopy to obtain sufficient tissue from mediastinal lymph nodes, and then the diagnosis of MCL was confirmed.
MCL is one of the most difficult-to-treat B-cell lymphomas[1]. In previously untreated patients, conventional chemotherapy is the most common treatment and the remission rates is high. However, relapse within a few years is common and median survival of five to seven years is low[9]. Proteasome inhibitors, mTOR inhibitors, and lenalidomide are available in addition to conventional chemotherapy for the treatment of relapsed MCL patients[1]. But their mechanisms of action and determinants of efficacy were still unclear[9].
In conclusion, we have reported a case of MCL with endobronchial involvement. MCL with endo
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Acik DY, Shariati MBH S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Tong L, Gan G, Xu C, Yuan L, Li Z, Li H. Tracheobronchial involvement of mantle cell lymphoma. Respirol Case Rep. 2018;6:e00346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Katono K, Shirasawa M, Harada S, Niwa H, Nakahara Y, Igawa S, Yokoba M, Kubota M, Masuda N. Endobronchial involvement of mantle cell lymphoma: A case report. Respir Med Case Rep. 2016;19:77-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Zhou Y, Wang H, Fang W, Romaguer JE, Zhang Y, Delasalle KB, Kwak L, Yi Q, Du XL, Wang M. Incidence trends of mantle cell lymphoma in the United States between 1992 and 2004. Cancer. 2008;113:791-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 202] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 4. | The world health organization classification of malignant lymphomas in japan: incidence of recently recognized entities. Lymphoma Study Group of Japanese Pathologists. PatholInt. 2000;50:696-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 343] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 5. | Vose JM. Mantle cell lymphoma: 2015 update on diagnosis, risk-stratification, and clinical management. Am J Hematol. 2015;90:739-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 6. | Sander B, Quintanilla-Martinez L, Ott G, Xerri L, Kuzu I, Chan JK, Swerdlow SH, Campo E. Mantle cell lymphoma--a spectrum from indolent to aggressive disease. Virchows Arch. 2016;468:245-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 59] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Depew ZS, Vassallo R. Pulmonary mantle cell lymphoma: a rare manifestation of an uncommon condition. Rare Tumors. 2012;4:e11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Baheti AD, Tirumani SH, Sewatkar R, Sachin SS, Shinagare AB, Ramaiya NH. MDCT of extranodal mantle cell lymphoma: a single institute experience. Abdom Imaging. 2015;40:1693-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Pérez-Galán P, Dreyling M, Wiestner A. Mantle cell lymphoma: biology, pathogenesis, and the molecular basis of treatment in the genomic era. Blood. 2011;117:26-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 306] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 10. | Figgis PA, Rainer SP, Ma D, Glanville AR. Endobronchial mantle cell lymphoma. Intern Med J. 2003;33:261-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Miyoshi I, Togitani K, Kuwayama Y, Daibata M, Matsumoto M, Taguchi H. Bilateral endobronchial involvement in mantle cell lymphoma. Intern Med. 2007;46:429-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Imai H, Ogura K, Endo M, Ikeda T. Recurrence of mantle cell lymphoma occurring in the tracheobronchial wall. Intern Med. 2012;51:1143-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Solomonov A, Zuckerman T, Goralnik L, Ben-Arieh Y, Rowe JM, Yigla M. Non-Hodgkin's lymphoma presenting as an endobronchial tumor: report of eight cases and literature review. Am J Hematol. 2008;83:416-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Alavi A, Shrikanthan S, Aydin A, Talanow R, Schuster S. Fluorodeoxyglucose-positron-emission tomography findings in mantle cell lymphoma. Clin Lymphoma MyelomaLeuk. 2011;11:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Ghielmini M, Zucca E. How I treat mantle cell lymphoma. Blood. 2009;114:1469-1476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 144] [Article Influence: 9.0] [Reference Citation Analysis (0)] |