Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2559
Peer-review started: September 14, 2021
First decision: October 25, 2021
Revised: November 16, 2021
Accepted: February 10, 2022
Article in press: February 10, 2022
Published online: March 16, 2022
Processing time: 177 Days and 16.9 Hours
Isolated dislocations of the scaphoid are extremely rare types of injuries, commonly associated with severe ligament disruptions, and are occasionally misdiagnosed. Treatment options for dislocations of the scaphoid mainly include closed reduction, with or without internal fixation, and open reduction with ligament repair.
A 59-year-old male worker sustained a twisting trauma of his right wrist, caused by a moving belt while he was operating a machine. When he presented at our emergency department, the patient complained of swelling, tenderness, and restriction of movement of the right wrist. Radiographs confirmed a primary complex partial radial dislocation of the scaphoid and some chip fractures of the capitate and hamate. Closed reduction with K-wire internal fixation was performed with the assistance of arthroscopy, and an excellent prognosis was achieved.
Arthroscopy-assisted reduction is a minimally invasive method to reduce the dislocated scaphoid and maintain the blood supply.
Core Tip: Isolated scaphoid dislocations are extremely rare, commonly associated with severe ligament disruptions, and occasionally misdiagnosed. Treatment options for scaphoid dislocations mainly include closed reduction and open reduction with ligament repair. We present the case of a 59-year-old male who suffered an isolated scaphoid dislocation. Closed reduction with K-wire internal fixation was performed with the assistance of arthroscopy, and an excellent prognosis was achieved. Arthroscopy-assisted reduction is an efficient and minimally invasive method of reducing the dislocated scaphoid, while keeping the external ligament and capsule intact, preventing adhesion of the tendons and maintaining the blood supply.
- Citation: Liu SD, Yin BS, Han F, Jiang HJ, Qu W. Isolated scaphoid dislocation: A case report and review of literature. World J Clin Cases 2022; 10(8): 2559-2568
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2559.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2559
Isolated scaphoid dislocation is an extremely rare injury, with just a few cases reported in the English literature since the first case was reported in 1930 by Higgs[1]. When we encountered such a case in our department, we reviewed the literature to better understand the cause and treatment of scaphoid dislocations. The mechanism of such injuries is believed to involve the wrist sustaining an axial load in a dorsiflexion and ulnar deviation position. The classifications of these types of injuries were described by Leung et al[2] in 1998.
A variety of treatment methods have been reported, including closed or open reduction, with or without K-wire fixation and arthroscopic assistance, as well as different fixation methods, including suture anchors and screws. Most of these procedures have resulted in an excellent prognosis. We chose arthroscopy-assisted reduction with K-wire internal fixation in a scaphoid type of cast for treatment of our patient and achieved an excellent prognosis.
A 59-year-old male worker sustained a twisting trauma to his right wrist caused by a moving belt while he was operating a machine. The patient complained of swelling, tenderness, and restriction of movement of his right wrist when he presented at our emergency department.
The patient had no history of present illness.
The patient had no relevant medical history.
The patient had no relevant personal or family history.
The patient’s vital signs were normal. Swelling, tenderness, and restriction of movement of his injured wrist were evident. There were no signs of neurovascular injury.
Findings from laboratory examinations were normal.
Radiographs and computed tomography scans revealed a primary complex partial radial dislocation of the scaphoid and some chip fractures of the capitate and hamate (Figure 1).
Isolated scaphoid dislocation.
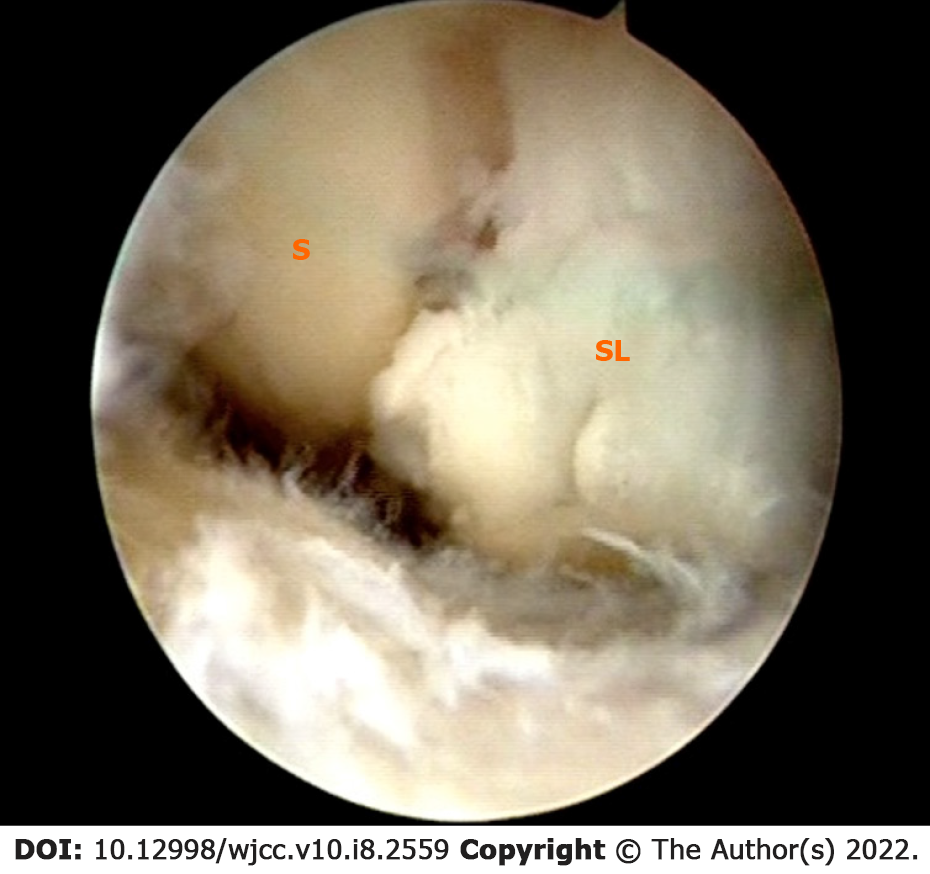
Closed reduction was attempted under general anesthesia, and arthroscopy was then performed in the midcarpal and radiocarpal joint. The arthroscopy confirmed a complete tear of the radioscaphocapitate ligament and scapholunate interosseous ligament; the lunotriquetral interosseous ligament was intact. The scapholunate diastasis was Geissler grade IV (Figure 2). As most of the stabilizers of the scaphoid were injured, the scaphoid had become extremely unstable, so it was difficult to stabilize the scaphoid to the lunate in a proper position. Thus, two K-wires were set into the scaphoid as a joystick temporarily, to reduce the scaphoid.
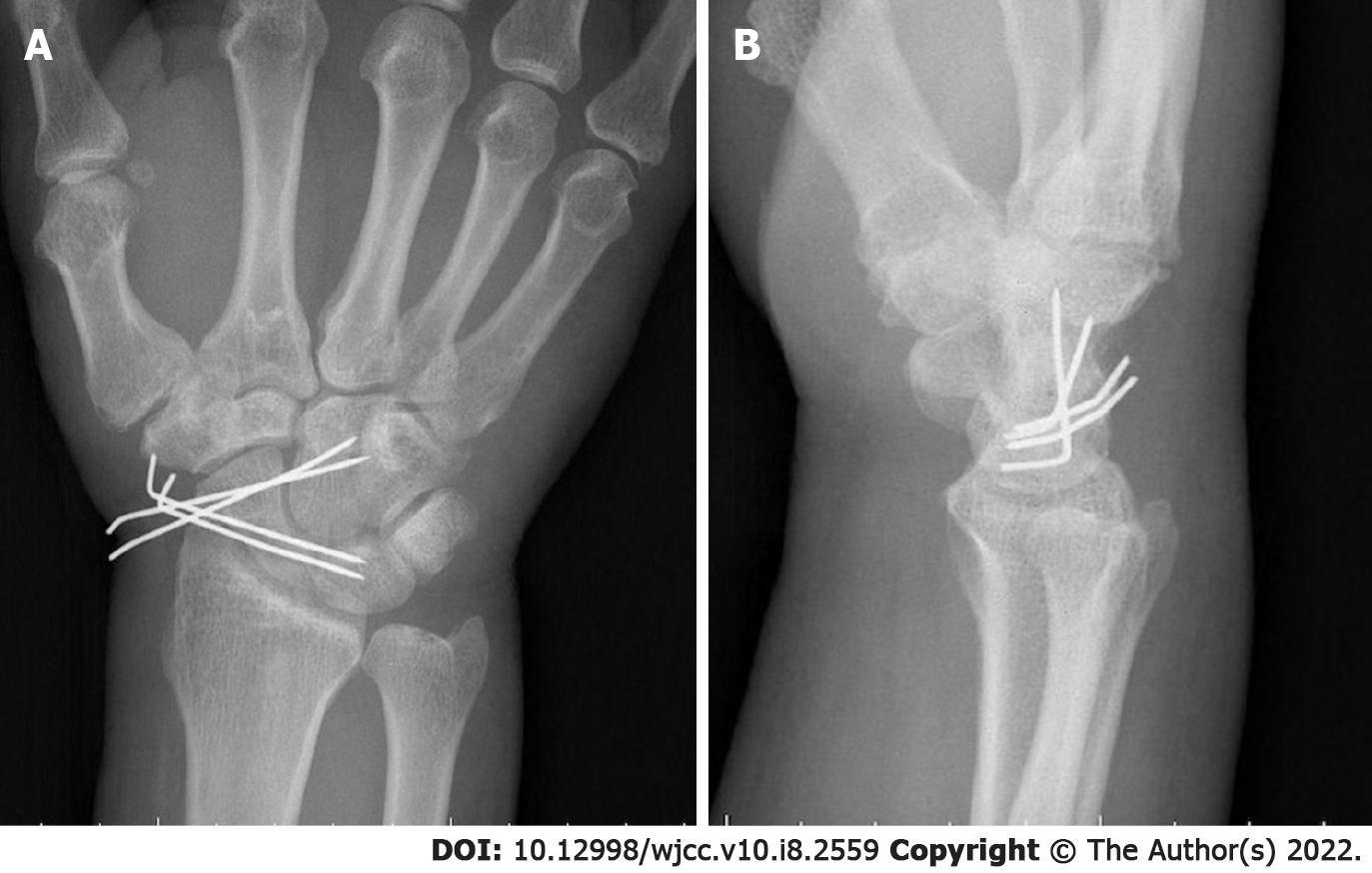
After performing debridement of the injured ligaments, the carpal alignment was maintained by internal fixation with four percutaneous K-wires under arthroscopic guidance and assistance (two to stabilize the scaphoid and lunate, and the other two to stabilize the scaphoid and capitate), which ensured precise reduction of the scapholunate joint (Figure 3). The wrist was postoperatively immobilized in a scaphoid-type cast. Six weeks later, the cast and K-wires were removed, and physical therapy was initiated.
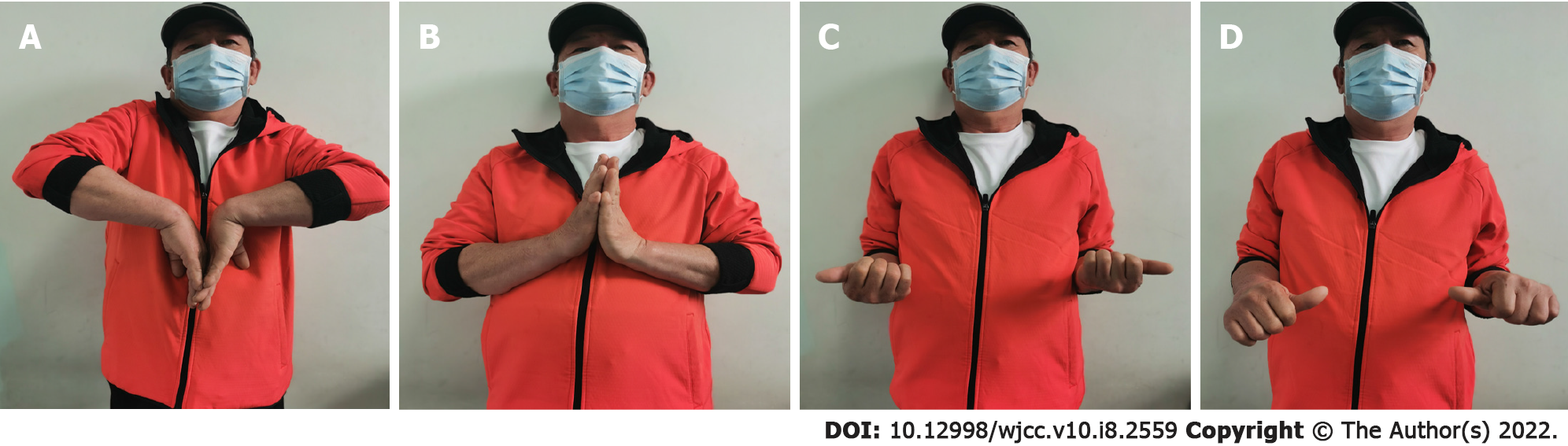
At the 6-mo follow-up, the patient had returned to work without any limitations or tenderness of the wrist. The clinical outcomes were assessed according to the modified Mayo wrist scoring system, which consisted of pain, range of motion, grip strength, and function[3]. The outcome was evaluated subjectively using the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire[4] and the Patient-Rated Wrist Evaluation (PRWE) score[5]. Standard lateral and posteroanterior X-rays were used to assess carpal bones. The flexion/extension of the injured wrist was 80°/70° compared with 80°/80° on the contralateral side. The pronation/supination was 80°/90° compared with 90°/90° on the contralateral side (Figure 4). Grip strength was 60 kg compared with 70 kg on the contralateral side. The modified Mayo wrist score was excellent. The DASH and PRWE scores were 16 and 10, respectively, and radiographs revealed neither avascular necrosis of the proximal pole of the scaphoid nor scapholunate diastasis (Figure 5).
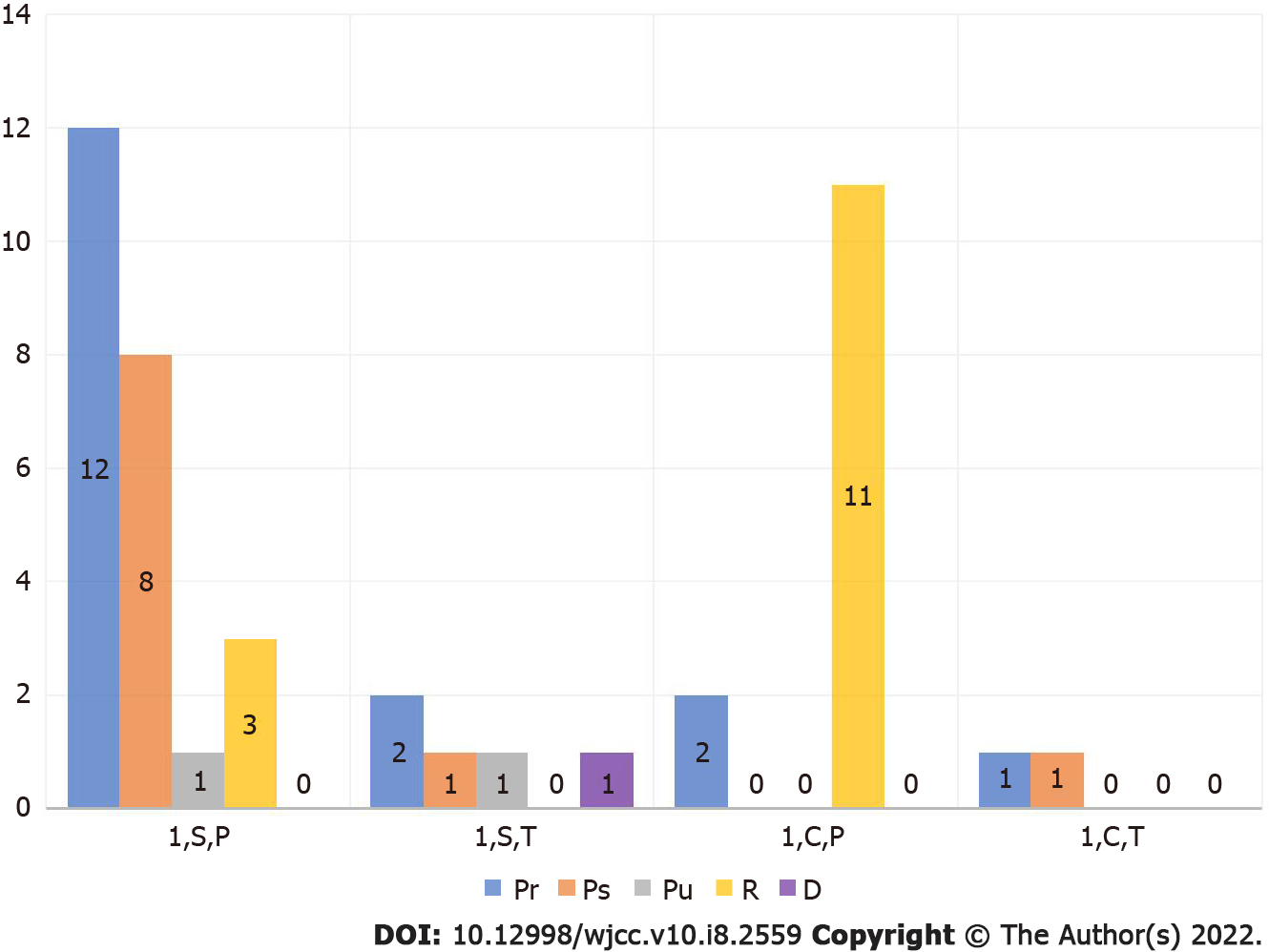
A literature search was performed using isolated or solitary dislocation of the scaphoid as key words; this search identified 58 cases reported in English since the first isolated scaphoid dislocation was reported in 1930[1,2,6-42]. The classification of isolated scaphoid dislocation is based on the description by Leung et al[2], and can be used to distinguish dorsal dislocation from dorsal intercalated segment instability caused by scapholunate ligament injury, even though the treatment options for these two injuries may be the same. The key difference between these two injuries is that the radioscaphocapitate ligament connecting the scaphoid and radius is disrupted in the former[2], and the most accurate way to ascertain whether the ligament is intact or not is through arthroscopy or open surgery[21]. Consequently, we set the radioscaphocapitate ligament status as an inclusion criterion to diagnose isolated dislocation of the scaphoid, especially those diagnosed as dorsal dislocation types according to Leung’s classification. From these criteria, a total of 48 cases were identified in the literature, and the clinical features of these cases were analyzed and summarized.
For all 48 cases identified in the literature, the patient’s age, sex, and injured side were reported (Table 1). The mean age was 41 years, ranging from 18-71 years. The patients were overwhelmingly male (44/48), but the number of scaphoid dislocations injuries was almost the same on each side (25 right vs 23 Left).
| Number of cases1 | ||
| Age in yr | 18-71 | |
| Sex | Male | 44/48 |
| Female | 4/48 | |
| Injured side | Left | 23/48 |
| Right | 25/48 | |
| Causes of injuries | Traffic accidents (motorcycle; car) | 15/48; 10/48 |
| Entrapment or rolling forces | 11/48 | |
| Falling from height | 6/48 | |
| Others | 6/48 | |
| Delayed diagnosis | 17/48 | |
| Reasons for the delays | Missed diagnoses | 8/14 |
| Delayed attendance | 6/14 | |
| Complications | Scapholunate diastasis | 4/48 |
| Degenerative joint | 5/48 | |
| Scaphoid avascular necrosis | 1/48 | |
The major cause of isolated scaphoid dislocation injuries was traffic accidents (25/48), among which 15 were motorcycle accidents and 10 were car accidents (Table 1). This might be explained by the injury mechanism. It is believed that the scaphoid is squeezed out of its fossa when the wrist is forced by axial loading into a dorsiflexion and ulnar deviation[15,21,39]. Although this might render a fracture of the styloid or the scaphoid more likely, most of the wrists of the traffic accident victims in this study experienced an axial force while they were holding the steering wheel or the handlebar in a dorsiflexion and ulnar deviation position.
The most common causes of isolated scaphoid dislocation after traffic accidents included entrapment or rolling forces (9/48) and falling from height (6/48).
The classification of isolated scaphoid dislocation was as described by Leung et al[2]. Only four cases (4/48) were categorized as secondary dislocation, and were all reported by Thompson et al[38]. Among the 44 primary dislocations, 29 were simple (24 partial, 5 total) and 15 were complex (13 partial, 2 total). Almost all of the dislocations were palmar and radial in orientation (Figure 6). Only one dorsal dislocation was reported[13]. That patient’s wrist was forced into dorsiflexion when he tried to prevent a 300 kg barrel from rolling over. The scaphoid, of which the proximal pole was out of its fossa, was found in a tent of the extensor retinaculum and devoid from all its ligamentous attachments; the reduction was made through a dorsal approach. This injury cannot be appropriately explained by the injury mechanism mentioned above; it seemed likely that a direct force on the palmar facet of the scaphoid, not a squeezing force, pushed the scaphoid out of its fossa dorsally. Two cases of palmar and ulnar dislocations were also included in the literature, both of which had median nerve compression by the proximal pole of the scaphoid[2,26].
In approximately 35% of the cases (17/48), diagnosis of isolated scaphoid dislocation was delayed, with the time delay ranging from 2 d to 9 mo. In three cases, the reasons for the delays were not mentioned in the literature; the others are summarized in Table 1. It is astonishing that in over half of the delayed cases (8/14), the delays were due to missed diagnoses. Four of these cases were diagnosed as a sprain without any X-ray at the first visit, while the others were misdiagnosed as a normal or scaphoid fracture, or overlooked due to concomitant injuries after an X-ray examination. As a delay of approximately 1 wk in diagnosis might result in the failure of closed reduction and a poor prognosis, such as stiffness and arthritis, it is very important for surgeons to diagnose precisely at the first visit[2,15].
Thirty-one percent of the cases (15/48) underwent closed reduction successfully (Table 2). All of these cases were diagnosed without delay, and the scaphoid was only partially dislocated[17,21,22]. Twelve of the 15 cases were immobilized by casts without any internal fixation, and most had fully recovered wrist functions after follow-up (durations of 3 mo to 10 years). The exception to this involved two cases classified as secondary dislocation, where the patients suffered from severe stiffness and mild pain of the wrist, as reported by Thompson et al[38]. The other three were immobilized using K-wires to reduce the scapholunate diastasis under arthroscopic assistance and achieved good outcomes as well[17,21,22]. It was reported that 69% of the perilunate dislocations that achieved initial anatomical reduction after closed reduction might lose reduction later[43], so Szabo et al[21] recommended that all reduced scaphoids should be stabilized with K-wires in a cast, even though the scapholunate joint showed no diastasis.
| Number of cases1 | ||
| Closed reduction | 15/48 | |
| Cast immobilization | 12/15 | |
| K-wire fixation | 3/15 | |
| Open reduction | 33/48 | |
| Dorsal approach | 12/33 | |
| Volar approach | 9/33 | |
| Radial approach | 3/33 | |
| Dorsal + volar | 1/33 | |
| Salvage operation | 3/33 (2, PRC; 1, STT fusion) | |
| Not mentioned | 5/33 | |
Eventually, 69% of the cases (33/48) underwent open reduction, including all 17 delayed diagnosis cases and 7 total dislocation-type cases. It was suggested that a delayed diagnosis of almost 1 wk made open reduction inevitable due to changes in the soft tissues[2,15], and this idea was supported by the literature. As all the ligaments to stabilize the scaphoid were compromised in the total dislocation-type, it seemed impossible to reduce the scaphoid through traction and dorsiflexion of the wrist.
Five of the open reduction cases were due to residual scapholunate diastasis after closed reduction. One cause for the residual scapholunate diastasis was that the scapholunate interosseous ligament was invaginated into the scapholunate interval, preventing reduction of the scapholunate diastasis. Another cause might be the scaphoid paradox, which is that to close the scapholunate gap, radial angulation is required, and to obtain correct scapholunate angulation, ulnar deviation is required[44]. A retrospective review of the perilunate dislocations showed that ligament repair with internal fixation maintained the anatomy of scapholunate reduction better than closed reduction and pinning[45]. A case report by Horton et al[17] suggested that ligament reconstruction through open surgery provided excellent anatomic and functional results. However, the use of wrist arthroscopy has expanded in both diagnosis and treatment of wrist abnormalities in recent years, and carpal instabilities, especially scapholunate dislocation caused by scapholunate interosseous ligament injuries, are commonly treated with arthroscopic assistance[44-46]. We believe that arthroscopy might demonstrate great advantages in the treatment of isolated scaphoid dislocations, as it allows extrication of the invaginated ligament and reduction of the diastasis through a joystick under direct vision, and can even enable minimally-invasive repair of the injured ligament.
For open reduction, a dorsal approach was chosen in 12 cases, a volar approach in 9 cases, and a radial approach in 3 cases (Table 2). Some authors recommended the volar approach for better vision and proper preservation of the dorsal blood supply and the superficial branch of the radial nerve[9]. Attention should be paid to palmar–ulnar scaphoid dislocations; open reduction in a volar approach is recommended because in all cases with such types of dislocation, the median nerve was compressed by the proximal pole of the scaphoid, and nerve decompression was necessary[2,26].
Possible complications of isolated scaphoid dislocation might be degenerative joint and carpal instability, which are likely to be seen in neglected cases[6,7]. However, in this literature review, 4 of the 48 cases showed scapholunate diastasis during the follow-up after open reduction, although in none of them was diagnosis delayed[16,21,33,38]. A degenerative joint developed in 5 cases (5/48), and of those, diagnosis was delayed in 3, with delay time ranging from 2.5 mo to 9 mo before the patients underwent salvage procedures[13,26,38].
Another rare complication was scaphoid avascular necrosis. To date, only 1 case showed necrosis of the scaphoid classified as primary complex total palmar radial dislocation[21]. The others, even the total dislocations in which the scaphoid had detached from all of its surrounding soft tissues, showed no necrosis. It seemed that the undisturbed intraosseous vascular channels inside the intact scaphoid allowed rapid revascularization from the surrounding soft tissues[2]. A delay in diagnosis was believed to be a key adverse factor for poor prognosis because of secondary finger stiffness, stiffness of the wrist, and degenerative changes[26].
A variety of casts were introduced by surgeons, but there is still a lack of clinical research to demonstrate which type of cast is the most appropriate. The dominant factor at present might be the surgeon’s preference.
There are some limitations to this study. First, as a case report, only 1 patient was diagnosed and treated, so there were no group comparisons of other treatment options. Second, the follow-up period was short. As we did not repair the scapholunate interosseous ligament directly during the operation, whether the ligament was healed or just scar-connected was unknown. Further observation is necessary.
Isolated scaphoid dislocation is a rare type of injury that can be diagnosed easily with radiography. However, delayed diagnosis of such cases may cause poor prognosis. Treatments for these injuries include closed reduction, with or without internal fixation, and open reduction with ligament repair, which seems to have become more commonly adopted in recent years. As arthroscopy is used in the diagnosis and treatment of wrist abnormalities more widely, we consider arthroscopy-assisted reduction an efficient and minimally invasive method of reducing the dislocated scaphoid while keeping the external ligament and capsule intact, preventing adhesion of the tendons and maintaining the blood supply.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oley MH, Shariati MBH S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Higgs SL. Two Cases of Dislocation of Carpal Scaphoid. Proc R Soc Med. 1930;23:1337-1339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Leung YF, Wai YL, Kam WL, Ip PS. Solitary dislocation of the scaphoid. From case report to literature review. J Hand Surg Br. 1998;23:88-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;136-147. [PubMed] |
| 4. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 46] [Reference Citation Analysis (0)] |
| 5. | MacDermid JC. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9:178-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 300] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 6. | Sefcik R, Andrews K, Stirton J, Lea J, Tanios M, Skie M. A Case Report of an Isolated Dislocation of the Scaphoid in a Lesser Arc Injury and a Review of the Literature. Case Rep Orthop. 2018;2018:9591502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Ballas EG, Raptis K, Stathopoulos IP, Stavropoulos NA, Spyridonos SG. Unusual Complete Isolated Scaphoid Dislocation, Report of a Case. Arch Bone Jt Surg. 2017;5:332-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Baek JR, Cho SH, Lee YS, Roh YH. Neglected isolated scaphoid dislocation. Indian J Orthop. 2016;50:693-696. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Kiliç M, Kalali F, Unlü M, Yildirim OS. Isolated carpal scaphoid dislocation. Acta Orthop Traumatol Turc. 2012;46:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Akinci M, Yildirim AO, Kati YA. Late-presenting, isolated, complete radial dislocations of the scaphoid treated with the Szabo technique. J Hand Surg Eur Vol. 2012;37:901-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Somford MP, Sturm MF, Vroemen JP. Reconstruction of isolated scaphoid dislocation with carpal dissociation, associated with a carpal anomaly. Strategies Trauma Limb Reconstr. 2010;5:105-110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Kanaya K, Wada T, Yamashita T. Scaphoid dislocation associated with axial carpal dissociation during volar flexion of the wrist: a case report. Hand Surg. 2010;15:229-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Amaravati RS, Saji M, Rajagopal H, Gururaj. Neglected dorsal dislocation of the scaphoid. Indian J Orthop. 2009;43:213-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Kolby L, Larsen S, Jørring S, Sørensen AI, Leicht P. Missed isolated volar dislocation of the scaphoid. Scand J Plast Reconstr Surg Hand Surg. 2007;41:264-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Chloros GD, Themistocleous GS, Zagoreos NP, Korres DS, Efstathopoulos DG, Soucacos PN. Isolated dislocation of the scaphoid. Arch Orthop Trauma Surg. 2006;126:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Kennedy JG, O'Connor P, Brunner J, Hodgkins C, Curtin J. Isolated carpal scaphoid dislocation. Acta Orthop Belg. 2006;72:478-483. [PubMed] |
| 17. | Horton T, Shin AY, Cooney WP 3rd. Isolated scaphoid dislocation associated with axial carpal dissociation: an unusual injury report. J Hand Surg Am. 2004;29:1102-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Cherif MR, Ben Ghozlen R, Chehimi A, Annabi H, Trabelsi M, Mbarek M, Ben Hassine H. [Isolated dislocation of the carpal scaphoid. A case report with review of the literature]. Chir Main. 2002;21:305-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Sakada T, Ninomiya S, Ohmori M. Simultaneous dislocation of the scaphoid and hamate bones. J Hand Surg Br. 1998;23:93-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Yasuda T. Isolated dislocation of the carpal scaphoid: a case report. Nihon Geka Hokan. 1997;66:59-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 21. | Szabo RM, Newland CC, Johnson PG, Steinberg DR, Tortosa R. Spectrum of injury and treatment options for isolated dislocation of the scaphoid. A report of three cases. J Bone Joint Surg Am. 1995;77:608-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Sides D, Laorr A, Greenspan A. Carpal scaphoid: radiographic pattern of dislocation. Radiology. 1995;195:215-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Milankov M, Somer T, Jovanović A, Brankov M. Isolated dislocation of the carpal scaphoid: two case reports. J Trauma. 1994;36:752-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Richards RS, Bennett JD, Roth JH. Scaphoid dislocation with radial-axial carpal disruption. AJR Am J Roentgenol. 1993;160:1075-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | McNamara MG, Corley FG. Dislocation of the carpal scaphoid: an 8-year follow-up. J Hand Surg Am. 1992;17:496-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Takami H, Takahashi S, Ando M. Dislocation of the carpal scaphoid associated with median nerve compression: case report. J Trauma. 1992;33:921-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Inoue G, Maeda N. Isolated dorsal dislocation of the scaphoid. J Hand Surg Br. 1990;15:368-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Ritchie DA, Gibson PH. Isolated dislocation of the scaphoid. Injury. 1988;19:405-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Stambough JL, Mandel RJ, Duda JR. Volar dislocation of the carpal scaphoid. Case report and review of the literature. Orthopedics. 1986;9:565-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Fishman MC, Dalinka MK, Osterman L. Case report 309. Diagnosis: complete volar subluxation of the right scaphoid bone and fracture of the right capitate bone. Skeletal Radiol. 1985;13:245-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 31. | Engkvist O, Ekenstam F. Closed dislocation of the scaphoid. A case report and review of the literature. Scand J Plast Reconstr Surg. 1986;20:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Maki NJ, Chuinard RG, D'Ambrosia R. Isolated, complete radial dislocation of the scaphoid. A case report and review of the literature. J Bone Joint Surg Am. 1982;64:615-616. [PubMed] |
| 33. | Murakami Y. Dislocation of the carpal scaphoid. Hand. 1977;9:79-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 34. | Thomas HO. Isolated dislocation of the carpal scaphoid. Acta Orthop Scand. 1977;48:369-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Parkes JC, Stovell PB. Dislocation of the carpal scaphoid: a report of two cases. J Trauma. 1973;13:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 36. | Reid JM. Isolated dislocation of the carpal scaphoid. Australas Radiol. 1969;13:376-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 37. | Taylor AR. Dislocation of the scaphoid. Postgrad Med J. 1969;45:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 38. | Thompson TC, CAMPBELL RD Jr, ARNOLD WD. PRIMARY AND SECONDARY DISLOCATION OF THE SCAPHOID BONE. J Bone Joint Surg Br. 1964;46:73-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 39. | Connell MC, DYSON RP. Dislocation of the carpal scaphoid; report of a case. J Bone Joint Surg Br. 1955;37-B:252-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Russell TB. Inter-carpal dislocations and fracture-dislocations; a review of 59 cases. J Bone Joint Surg Br. 1949;31B:524-531, illust. [PubMed] |
| 41. | Walker GBW. Dislocation of the carpal scaphoid reduced by open operation. Br J Surg. 1943;30:380-381. |
| 42. | Kuth JR. Isolated dislocation of the carpal navicular: a case report. J Bone Jt Surg. 1939;21:479-483. |
| 43. | Adkison JW, Chapman MW. Treatment of acute lunate and perilunate dislocations. Clin Orthop Relat Res. 1982;199-207. [PubMed] |
| 44. | Whipple TL. The role of arthroscopy in the treatment of scapholunate instability. Hand Clin. 1995;11:37-40. [PubMed] |
| 45. | Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg Am. 1997;22:344-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 109] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 46. | Mathoulin C. Treatment of dynamic scapholunate instability dissociation: Contribution of arthroscopy. Hand Surg Rehabil. 2016;35:377-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |