Published online Feb 16, 2022. doi: 10.12998/wjcc.v10.i5.1623
Peer-review started: July 31, 2021
First decision: October 25, 2021
Revised: October 28, 2021
Accepted: December 28, 2021
Article in press: December 28, 2021
Published online: February 16, 2022
Processing time: 195 Days and 2.9 Hours
Synovial sarcoma is a malignant mesenchymal neoplasm with variable epithelial differentiation. Most synovial sarcoma cases are reported in young adults and can arise in any body site. Notably, primary orbital synovial sarcoma is rare.
An 8-year-old east Asian girl with 1-month history of gradual painless proptosis and lacrimation of the right eye was admitted. The patient presented with painless proptosis, downward eyeball displacement, and upward movement disorders. According to clinical manifestations, imaging examinations and postoperative immunohistochemical examinations, the diagnosis was monophasic synovial sarcoma with calcification. The patient underwent anterior orbitotomy procedure for removal of the right orbital mass under general anesthesia. The diagnosis of monophasic synovial sarcoma with calcification was confirmed finally through histological and immunohistochemical exam. The follow-up period was 6 mo, and no recurrence was observed during this period.
Primary orbital monophasic synovial sarcoma with calcification is a rare sarcoma, and clinical manifestations and imaging results are not specific. The tumor may present similar features as a benign tumor. Comprehensive analysis of clinical, radiological, and pathological findings is critically important for making the right diagnosis. Conventional treatment approach for synovial sarcoma is surgical resection with adjuvant or neoadjuvant radiotherapy, which is highly effective for localized tumors.
Core Tip: We describe a patient with 1-month history of gradual painless proptosis and lacrimation of the right eye. The patient underwent anterior orbitotomy procedure for removal of the right orbital mass under general anesthesia. The diagnosis of monophasic synovial sarcoma with calcification was confirmed finally through histological and immunohistochemical exam. The follow-up period was 6 mo, and no recurrence was observed during this period. This case illustrates the tumor may present similar features as a benign tumor. Comprehensive analysis of clinical, radiological, and pathological findings is critically important for making the right diagnosis.
- Citation: Ren MY, Li J, Li RM, Wu YX, Han RJ, Zhang C. Primary orbital monophasic synovial sarcoma with calcification: A case report. World J Clin Cases 2022; 10(5): 1623-1629
- URL: https://www.wjgnet.com/2307-8960/full/v10/i5/1623.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i5.1623
Synovial sarcoma is a malignant mesenchymal neoplasm with variable epithelial differentiation. It mainly occurs in young adults and can arise at several sites[1]. It mainly commonly occurs in deep soft tissue of the extremities in adolescents and young adults[2]. Synovial sarcoma of the head and neck region is very rare, and only a few cases of sarcoma arising from the orbit have been reported[3,4]. The current study reports a case of primary orbital monophasic synovial sarcoma which was characterized by calcification in an 8-year old patient.
An 8-year-old east Asian girl with 1-mo history of gradual painless proptosis and lacrimation of the right eye was admitted to our hospital.
The patient presented with gradual painless proptosis and lacrimation of the right eye for 1 mo. The proptosis was gradual and painless. No special treatment was perfor
The patient had no history of any previous disease.
There was no family history of malignant neoplasm.
Physical examination showed no neurological signs. The patient presented with painless proptosis, downward eyeball displacement, and upward movement disor
Blood and urine tests were normal.
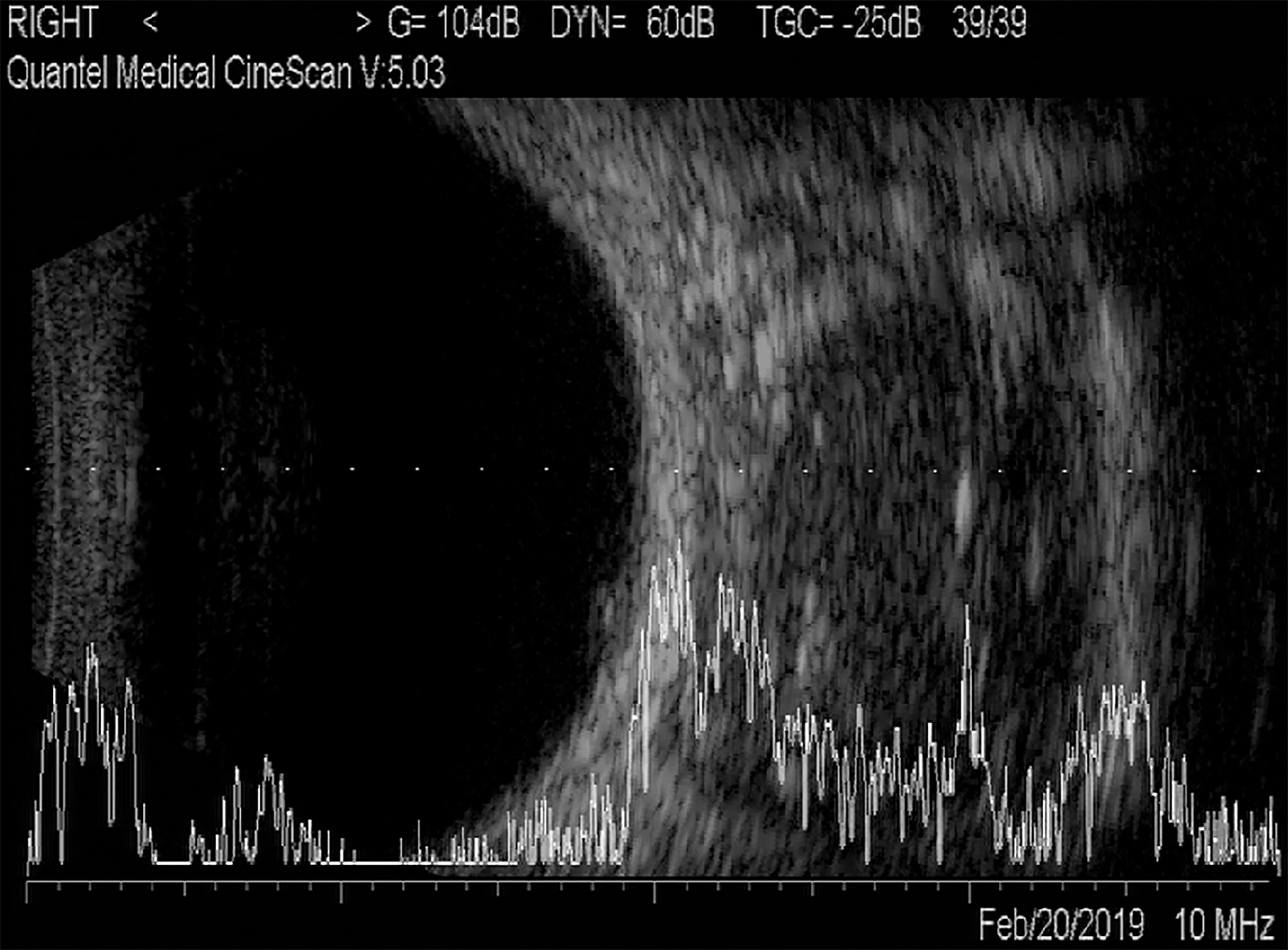
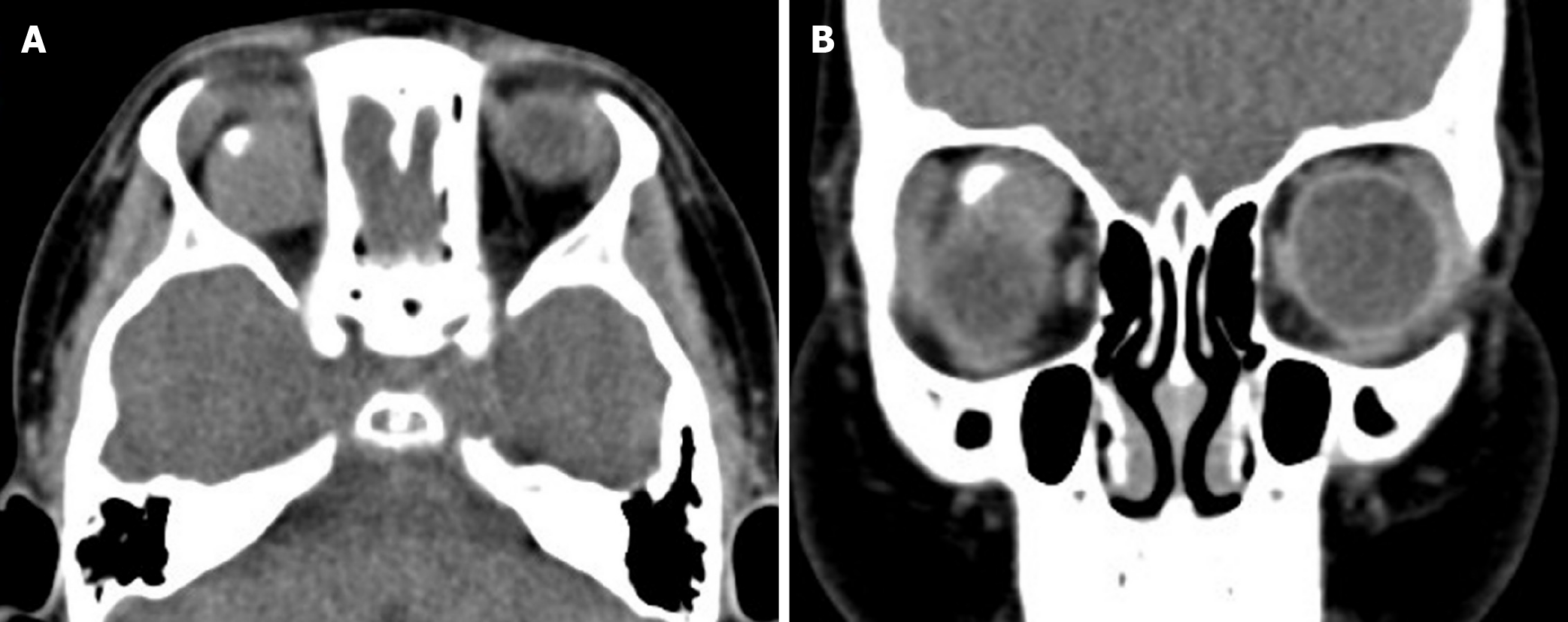
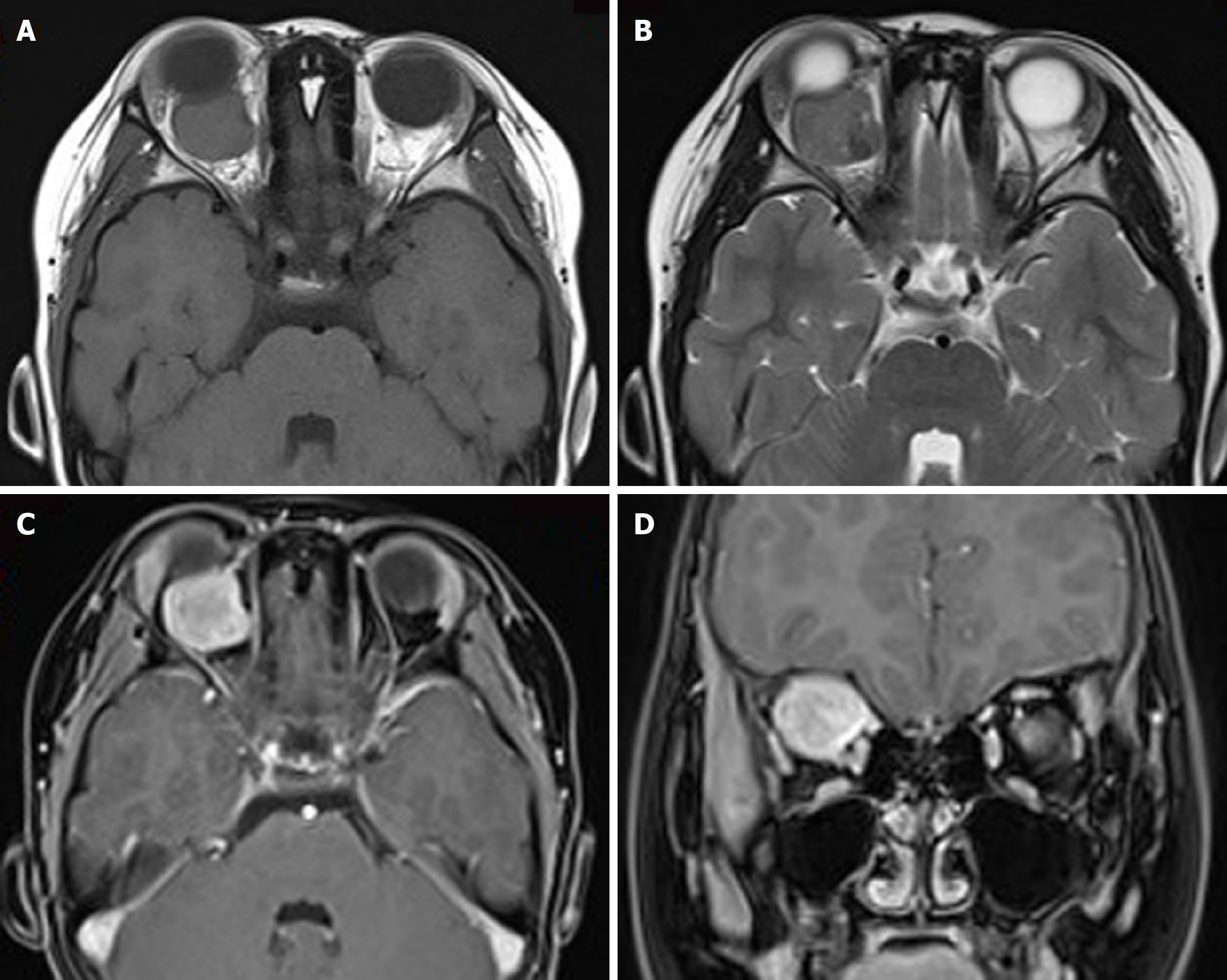
A/B-scan showed moderate echogenic lesions in the right eye orbital. Echoes were uneven, well-distributed and sound transmission normal. Patchy strong echoes and sound shadows were detected (Figure 1). Orbital CT scan showed a well-defined soft tissue density mass in the right orbit, with flaky high-density shadows observed inside the right orbital. The size of the mass was approximately 20 mm × 20 mm × 19 mm, and exophthalmos; extraocular muscles and optic nerve were compressed (Figure 2). Orbital magnetic resonance imaging showed a circular-like mass in the right orbital. T1-weighted images (T1WI) showed moderate signals, whereas T2-weighted images (T2WI) showed mixed signals, with high number of moderately high signals. T1WI and T2WI were characterized by low-signal regions. Most part of the lesion was significantly and unevenly enhanced, whereas local lesions did not exhibit any enhancement (Figure 3).
Based on the findings described above, the preliminary diagnosis was rhabdomyosarcoma or other malignant neoplasm.
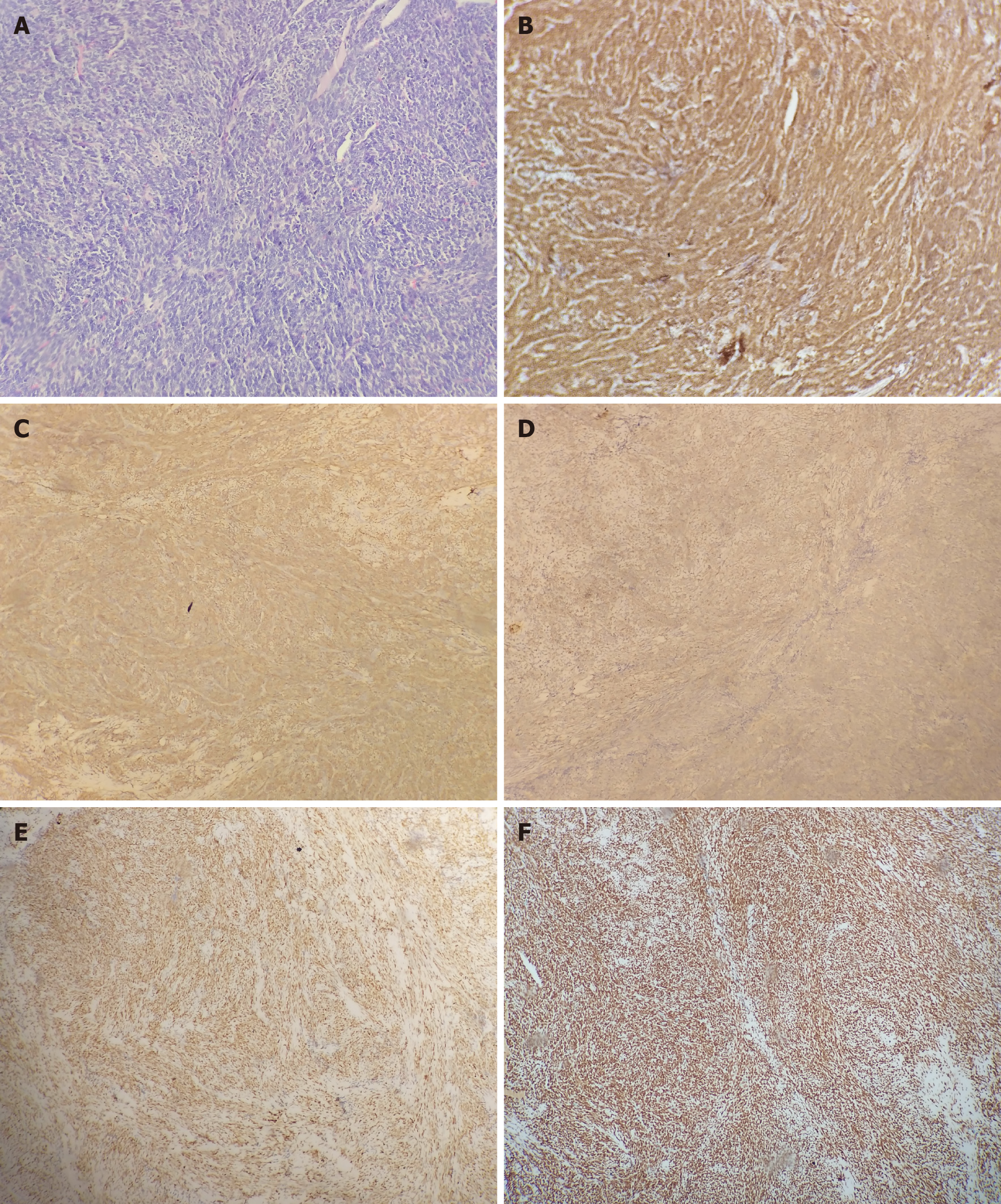
Histological examination showed that the tumor was monophasic synovial sarcoma with calcification. Immunohistochemical analysis showed positive staining for CD34, CD99, Bcl-2, CKpan, TLE1, INI-1 and Ki-67 (25%), and negative staining for SMA, Vimentin, Myogenin, Myoglobin, Syn, CgA, NSE, S-100, PGP9.5, EMA, CK7, CK (AE1/AE3), CD65, Calretinin, TTF1 and MUC-4 (Figure 4).
After preoperative examination, the patient underwent anterior orbitotomy procedure for removal of the right orbital mass under general anesthesia. The operation showed an oval tumor above the optic nerve in the right orbit. The tumor margins were well defined, however, it was significantly large, reddish, unmovable, and adhesive to the levator palpebrae muscle (Figure 5). The levator palpebrae muscle was cut along its path, the tumor was carefully separated from the muscle and removed. The levator palpebrae muscle was sutured before the end of the operation. After treatment, the patient was transferred to the tumor hospital and underwent systemic chemotherapy.
The follow-up period was 6 mo, and no recurrence was observed during this period.
Synovial sarcoma accounts for 10%-20% of soft tissue sarcomas. It is a high-grade soft-tissue sarcoma occurring mainly in older children and young adults. Approximately 7% of soft tissue sarcoma cases occur in the head and neck region, and synovial sarcoma represents less than 0.1% of all head and neck cancers[5,6]. Orbital synovial sarcoma is a rare kind of malignancy. Therefore, diagnosis of orbital synovial sarcoma in clinical practice is challenging, and required an integrated approach that incorporates specific clinical, histological, immunohistochemical, and molecular analyses.
Synovial sarcoma is a rare kind of orbital tumor and the clinical characteristics have not been fully elucidated. Clinical manifestations include gradual painless proptosis, eyelid swelling, a palpable painless mass, epiphora, ptosis, and periorbital spontaneous pain or tenderness. However, these clinical manifestations are not unique to synovial sarcoma. Characteristic findings are not reported in current imaging studies due to the small number of cases. A case of monophasic synovial sarcoma primarily arising in the left supero-nasal orbital region was reported in a 24-year-old woman, which was clinically mistaken for a periocular cyst[6]. However, the lesion was characterized by calcification similar to the current case.
The calcification can be pathologically divided into dystrophic calcification and metastatic calcification. In the current case, the growth of the lesion was relatively rapid, resulting in ischemia and necrosis of the tumor. Significant calcification of the lesion may be caused by dystrophic calcification. Occurrence of a lesion with cal
Orbital tumor such as vascular lesions, vascular malformations, other benign lesions and orbital malignancies should be considered when there is a lesion characterized by calcification in the orbit during childhood. Irregular calcification is common in malignant tumors and partially benign lesions. In the current case, orbital computed tomography and magnetic resonance imaging scans showed a well-defined soft tissue density mass in the right orbital. The tumor may present similar features as benign tumors. Differential diagnosis may identify findings that do not perfectly fit preliminary diagnosis of benign tumors. In such cases comprehensive consideration of clinical, radiological, and pathological findings is critically important[10].
Synovial sarcoma is a type of highly malignant soft tissue sarcoma, with poor survival of patients. Conventional treatment approach is surgical resection with adjuvant or neoadjuvant radiotherapy, which are highly effective for localized tumors. Synovial sarcoma is relatively sensitive to chemotherapy. Ifosfamide and ifosfamide combinations are effective for treatment of synovial sarcoma[5,11,12]. A combinatory treatment of doxorubicin and ifosfamide is the preferred first-line therapy for patients with metastatic cases. On the other hand, sequential doxorubicin and ifosfamide can be considered for localized tumors. Pazopanib and trabectedin are effective as second-line therapies and for subsequent treatment[11].
A previous study reported high local recurrence rates despite surgical and postoperative radiotherapy, adjuvant chemotherapy and distant metastasis rates were not reduced by these approaches[2]. The disease is characterized by early and late recurrences, and the 10-year disease-free survival is approximately 50%[5]. Several new approaches for treatment of metastatic synovial sarcoma are currently under investigation, both at preclinical and clinical levels, including receptor tyrosine kinase inhibitors, epigenetic modulators, compounds interfering with DNA damage response (DDR), and immunotherapy[11].
Histological analysis shows that synovial sarcoma is monophasic, biphasic, or poorly differentiated and exhibits a specific chromosomal translocation t (X; 18) (p11.2; q11.2) in > 95% of cases[6]. Genetic analysis shows that synovial sarcoma tumors have a characteristic fusion protein, SS18-SSX, implicated in promoting disease development. BRD9 is a component of SS18-SSX containing BAF complexes in synovial sarcoma cells. Studies report that BRD9 is implicated in oncogenic mechanisms underlying the SS18-SSX fusion in synovial sarcoma and targeted degradation of BRD9 is a potential therapeutic approach for treatment of synovial sarcoma[13].
These findings show that primary orbital synovial sarcoma cases with calcification are rare, and clinical manifestations and imaging results are not specific. The tumor may exhibit similar features as a benign tumor. Therefore, these cases require comprehensive clinical, radiological, and pathological analysis to achieve the right diagnosis. The conventional treatment approach for surgical resection with adjuvant or neoadjuvant radiotherapy, which are highly effective for localized tumors. However, a longer follow-up time is required to determine effectiveness of the treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Maglangit SACA S-Editor: Guo X L-Editor: Kerr C P-Editor: Guo X
| 1. | Thway K, Fisher C. Synovial sarcoma: defining features and diagnostic evolution. Ann Diagn Pathol. 2014;18:369-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 213] [Article Influence: 19.4] [Reference Citation Analysis (1)] |
| 2. | Gervasio KA, Ramesh S, Sivalingam MD, Markovitz M, Milman T. Primary Synovial Sarcoma of the Orbit: A Case Report and Update on Diagnostic Techniques. Ophthalmic Plast Reconstr Surg. 2021;37:e155-e157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Xu P, Chen J. Primary Synovial Sarcoma of the Orbit. Ophthalmol Eye Dis. 2017;9:1179172117701732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Shukla PN, Pathy S, Sen S, Purohit A, Julka PK, Rath GK. Primary orbital calcified synovial sarcoma: a case report. Orbit. 2003;22:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Nielsen TO, Poulin NM, Ladanyi M. Synovial sarcoma: recent discoveries as a roadmap to new avenues for therapy. Cancer Discov. 2015;5:124-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 123] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 6. | Portelli F, Pieretti G, Santoro N, Gorelli G, De Giorgi V, Massi D, Dei Tos AP, Mazzini C. Primary Orbital Synovial Sarcoma Mimicking a Periocular Cyst. Am J Dermatopathol. 2019;41:655-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Dai XZ, Wang LY, Shan Y, Qian J, Xue K, Ye J. Clinicopathological analysis of 719 pediatric and adolescents' ocular tumors and tumor-like lesions: a retrospective study from 2000 to 2018 in China. Int J Ophthalmol. 2020;13:1961-1967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Jurdy L, Merks JH, Pieters BR, Mourits MP, Kloos RJ, Strackee SD, Saeed P. Orbital rhabdomyosarcomas: A review. Saudi J Ophthalmol. 2013;27:167-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Wladis EJ, Farber MG, Nepo AG. Metastatic synovial sarcoma to the orbit. Ophthalmic Plast Reconstr Surg. 2012;28:e131-e132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Fujibuchi T, Miyawaki J, Kidani T, Imai H, Kiyomatsu H, Kitazawa R, Miura H. Intraosseous synovial sarcoma of the distal ulna: a case report and review of the literature. BMC Cancer. 2019;19:116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Desar IME, Fleuren EDG, van der Graaf WTA. Systemic Treatment for Adults with Synovial Sarcoma. Curr Treat Options Oncol. 2018;19:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 12. | Ferrari A, De Salvo GL, Brennan B, van Noesel MM, De Paoli A, Casanova M, Francotte N, Kelsey A, Alaggio R, Oberlin O, Carli M, Ben-Arush M, Bergeron C, Merks JH, Jenney M, Stevens MC, Bisogno G, Orbach D. Synovial sarcoma in children and adolescents: the European Pediatric Soft Tissue Sarcoma Study Group prospective trial (EpSSG NRSTS 2005). Ann Oncol. 2015;26:567-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 110] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 13. | Brien GL, Remillard D, Shi J, Hemming ML, Chabon J, Wynne K, Dillon ET, Cagney G, Van Mierlo G, Baltissen MP, Vermeulen M, Qi J, Fröhling S, Gray NS, Bradner JE, Vakoc CR, Armstrong SA. Targeted degradation of BRD9 reverses oncogenic gene expression in synovial sarcoma. Elife. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 134] [Article Influence: 19.1] [Reference Citation Analysis (0)] |