Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10663
Peer-review started: April 27, 2022
First decision: July 29, 2022
Revised: August 12, 2022
Accepted: September 6, 2022
Article in press: September 6, 2022
Published online: October 16, 2022
Processing time: 155 Days and 2.6 Hours
Chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) is often associated with an increased risk of developing subsequent neoplasms of epithelial and mesenchymal origin. Coincidence of CLL/SLL and urothelial carcinoma (UC) is very rare. Herein, we report a case of synchronous renal pelvis carcinoma with SLL.
A 78-year-old man presented with the complaint of terminal painless gross hematuria for the past 2 mo. On physical examination, enlarged lymph nodes were palpable in the cervical and axillary regions. The patient’s peripheral blood film was normal. He had a significant smoking history for the past 50 years. Cystoscopy revealed bleeding in the left upper urinary tract. Abdominal com
This is the first case of coincident CLL/SLL and upper tract UC in the literature. Cancer patients with lymphadenopathies should always be investigated to rule out the possibility of synchronous or metachronous malignancy.
Core Tip: Coincidence of chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) and urothelial carcinoma (UC) is very rare. We report a case of synchronous renal pelvis carcinoma with SLL. This is the first case of coincident CLL/SLL and upper tract UC in the literature. Cancer patients should always be investigated to rule out the possibility of a synchronous or metachronous malignancy.
- Citation: Yang HJ, Huang X. Synchronous renal pelvis carcinoma associated with small lymphocytic lymphoma: A case report. World J Clin Cases 2022; 10(29): 10663-10669
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10663.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10663
Chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL) is often associated with an increased risk of developing subsequent neoplasms of epithelial and mesenchymal origin[1,2]. Coincidence of CLL/SLL and urothelial carcinoma (UC) is very rare. Only five cases of coincident CLL/SLL and bladder cancer have been reported[2-5]. Upper tract UCs (UTUCs) are uncommon, accounting for only 5%-10% of UCs worldwide[6]. Here, we present a case of synchronous CLL/SLL and renal pelvis carcinoma diagnosed in laparoscopic radical nephroureterectomy specimens. To our knowledge, this is the first case of coincident CLL/SLL and UTUC in the literature.
A 78-year-old male farmer presented with the complaint of terminal painless gross hematuria without frequency or urgency during micturition for the past 2 mo.
No history of present illness.
The patient’s medical history was significant for hypertension for 10 years, and his blood pressure was well controlled with levotide amlodipine and timisartan tablets. He also had a significant history of smoking for the past 50 years.
No familial history of cancer and other illness.
Enlarged lymph nodes were palpable in the cervical and axillary regions.
The patient’s urinalysis results were positive for red blood cells (+++). The peripheral blood parameters were normal: White blood cell count (6.6 × 109/L), neutrophil percentage (54.9%), lymphocyte percentage (25.9%), hemoglobin (129 g/L), and platelet count (169 × 109/L).
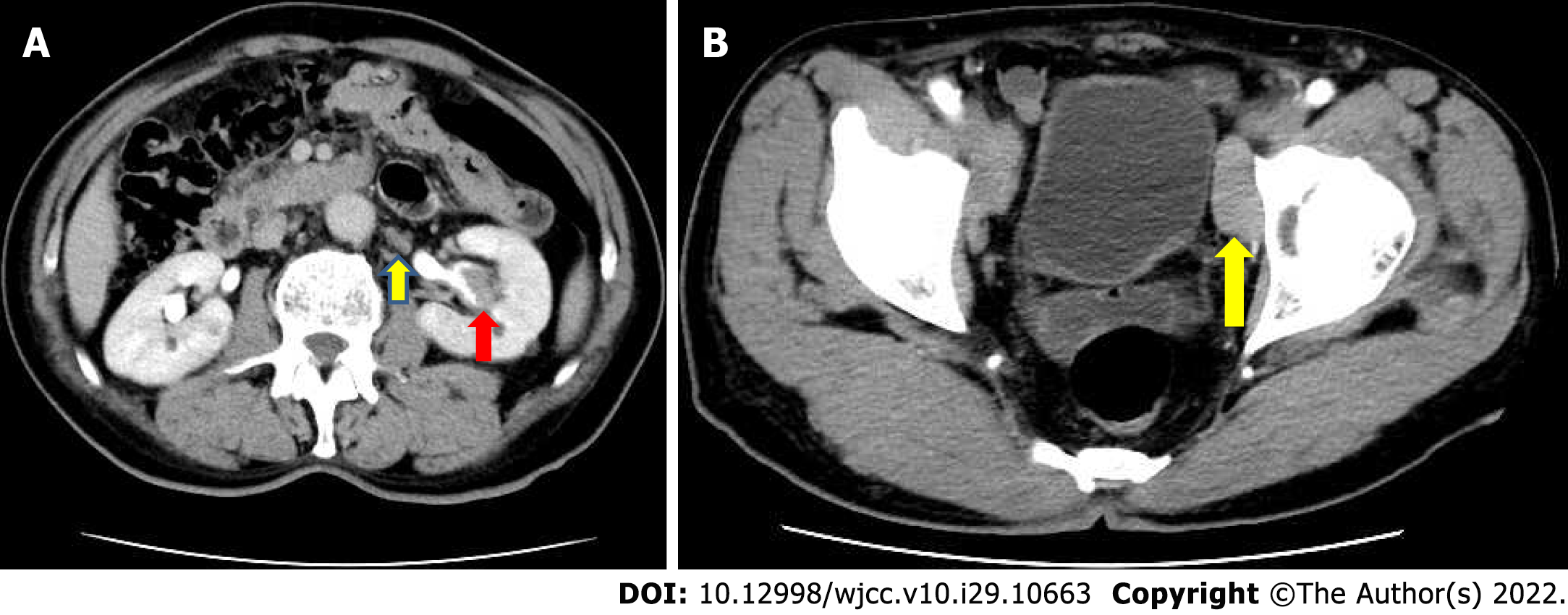
Cystoscopy revealed that the urinary tract bleeding originated from the left upper urinary tract. Abdominal computed tomography imaging demonstrated a tumor mass of approximately 2.7 cm × 1.5 cm × 1 cm in the central part of the left renal pelvis cavity (Figure 1A). Multiple enlarged lymph nodes were noted in the retroperitoneal and pelvic walls (Figure 1). Bone and chest radiographs were negative for metastases.
UTUC of the left renal pelvis with possible lymphatic metastasis.
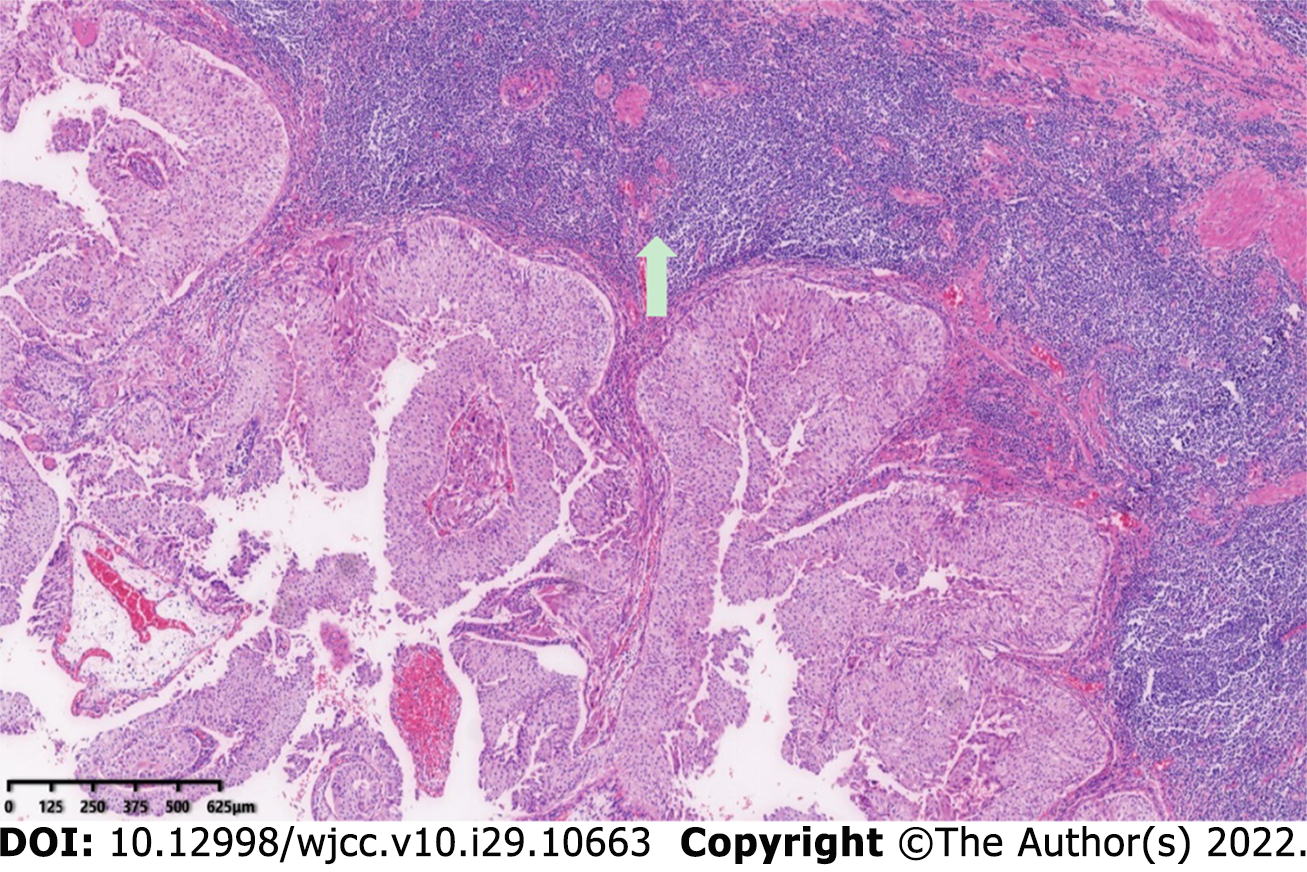
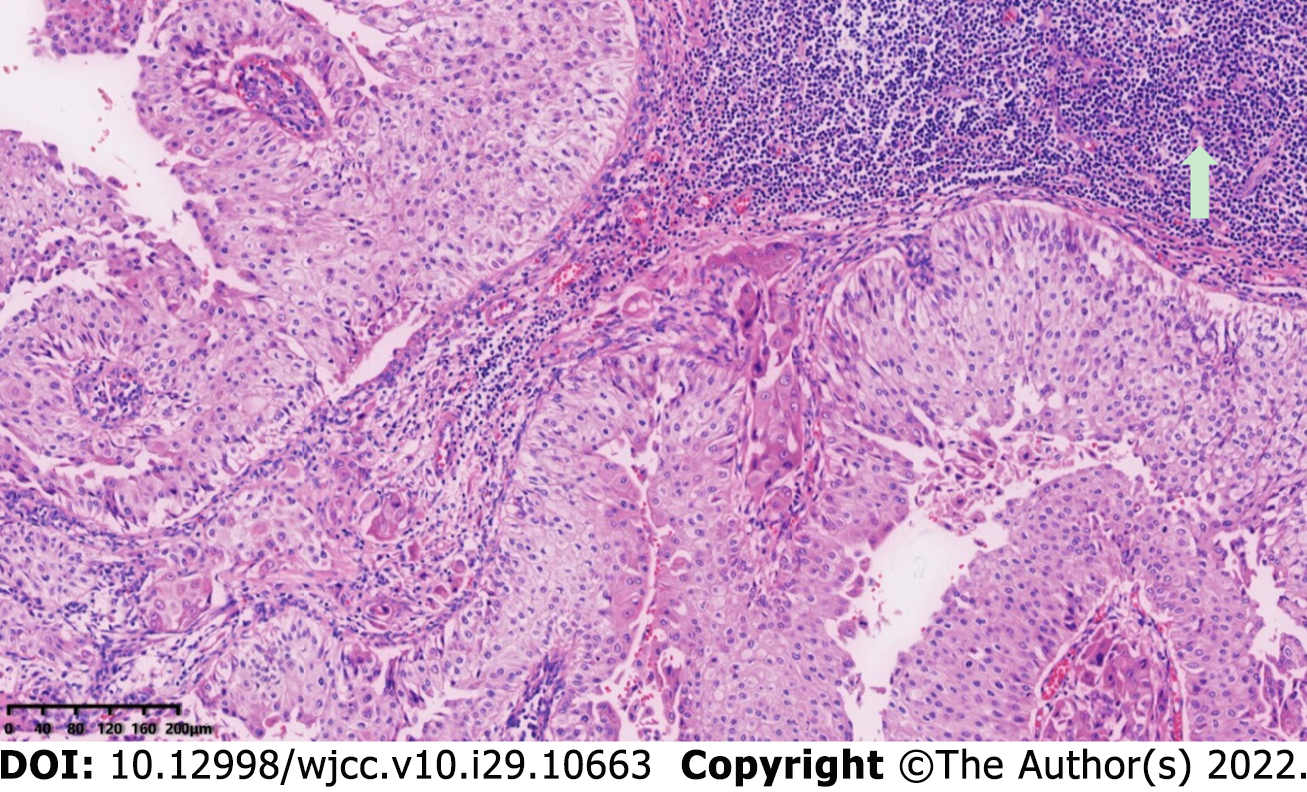
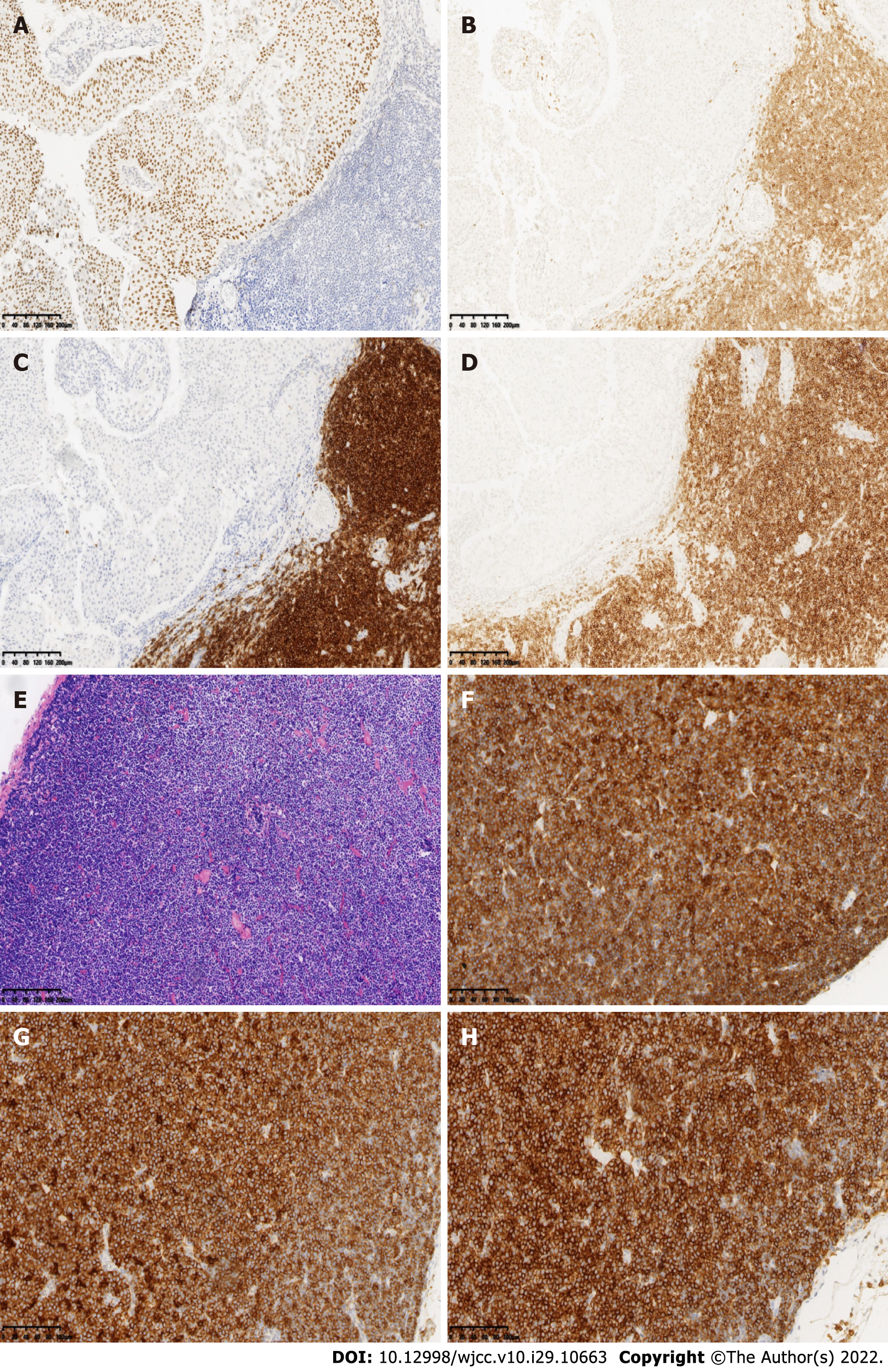
A 2.7 cm × 1.5 cm × 1.0 cm tumor was found in the renal pelvis in an isolated kidney specimen. The resected specimen was fixed in 10% neutral buffered formalin. Routine H&E staining was performed for histological examination. Immunohistochemistry was conducted on the formalin–fixed, paraffinembedded tissue sections. Light microscopic examination confirmed the diagnosis of UTUC of the renal pelvis urothelium extending into the lamina propria (Figure 2). A large amount of diffuse small lymphocytic infiltration was observed along the periphery of the tumor mucosa. The lymphocytes were well differentiated and were of the same type (Figure 3). Immunohistochemistry studies revealed that the urothelial tumor cells were positive for P63 (Figure 4A). Retroperitoneal renal pedicle enlarged lymph nodes showed diffuse architectural effacement due to the proliferation of small lymphocytes with variably prominent scattered proliferation centers composed of prolymphocytes and paraimmunoblasts, and were positive for CD5, CD20, and CD23. No UC metastases were observed in the lymph nodes. Renal pelvis lymphatic tissue and lymphocytes were positive for CD5, CD20, and CD23 (Figure 4). In addition, the following results were obtained: CD3 (-), Ki-67 (30%+), Bcl-2 (+), Bcl-6 (+), CD10 (-), CD79a (+), CD43 (+), CyclinD1 (-), CD21 (-), MUM1 (partial +), CD138 (-), Kappa K (-), Lambda λ (-), and CD30 (-). The final diagnosis was left renal pelvis high-grade invasive papillary UC and left retroperitoneal SLL with left kidney involvement (Figures 2 and 3).
After an additional diagnosis of CLL/SLL was made, the patient underwent a retrospective examination for a complete hematology evaluation. Enlarged lymph nodes were detected in the bilateral cervical, axillary, and inguinal regions by ultrasound, with a maximal lymph node size of 2.8 cm × 1.4 cm. Enlarged lymph nodes were also detected around the pancreas with a maximal lymph node size of 3.6 cm × 3.2 cm at the pancreatic tail. The patient’s peripheral blood parameters were normal after surgery. Bone marrow aspiration results showed hypocellular hematopoietic tissue with trilineage growth inhibition. Focal aggregation of the same type of small lymphocytes was observed between the bone trabeculas. The bone marrow fibrosis (MF) grading in the silver-stained bone marrow biopsy sections suggested MF-1. Immunohistochemistry studies showed that the small lymphocytes were positive for CD5, CD19, CD20, and CD23. These results confirmed the diagnosis of CLL/SLL with bone marrow involvement.
The patient underwent laparoscopic radical nephroureterectomy under general anesthesia.
The patient smoothly recovered from the surgery without any complications and was discharged after 7 d of hospitalization. His CLL/SLL situation did not require any medication according to the related guidelines from hematology. The patient stopped smoking following the physician’s advice. After 2 years of regular follow-up, he was doing well with UTUC and CLL/SLL.
The occurrence of multiple primary cancers (MPCs) is a very rare situation. They usually grow in elderly people, as the morbidity of malignancies increases with age[1]. Based on the time of diagnosis at each primary site, MPCs are classified into two categories: Synchronous occurrence of more than one tumor or metachronous occurrence of another tumor in a known case of carcinoma. Synchronous malignancy is defined as the occurrence of two tumors within 6 mo[7]. UC coincident with CLL/SLL is very rare with only five cases of bladder cancer reported in the literature[2-5]. The coincidence of CLL/SLL and UTUC is extremely rare. In those reported bladder cancer coincident with CLL/SLL cases, most patients had abnormal peripheral blood smear of leukocytosis with absolute lymphocytosis[2-5]. No lymphadenopathy was noted. This apparent abnormality gave the chance to detect the CLL/SLL at the beginning of diagnosis. In our case, the patient had no peripheral blood abnormality. The only abnormality was multiple enlarged lymph nodes in the retroperitoneal and pelvic walls which implied possible lymphatic metastasis of UTUC. The SLL was found in the renal pedicle lymph nodes and parenchyma of the renal pelvis during the pathological diagnosis procedure after a RUN surgery for renal pelvis carcinoma. The limitation of our case is that we did not perform a biopsy to detect the CLL/SLL before surgery. This is the first case of coincident CLL/SLL and UTUC reported.
The incidence of coincident malignancies in patients with CLL/SLL is increased because of immune dysregulation and consequent treatment[8,9]. Tsimberidou et al[10] demonstrated that the frequency of other malignancies in CLL/SLL patients is 2.2 times higher than that in the general population. Breast, brain, skin, and prostate tumors have been reported to be common coincident malignancies of CLL/SLL. However, UC coincident with CLL/SLL is a rare situation[2-5]. The etiology of MPCs is complex and includes environmental factors, genetic susceptibility, immunological impairment, previous medical treatment, hormonal factors, and sex[11]. Many kinds of chemical agents including tobacco, aniline dyes, benzidine, aromatic amines, and rubber have been reported to cause bladder cancer[12]. Although the relationship between these two cancers is unclear, one possible explanation involves the glutathione S transferase M1 (GSTM1), which is important for the metabolism of environmental carcinogens, reactive oxygen species, and chemotherapeutic agents. Cigarette smoke carcinogens inactivate the GSTM1, and the smokers exhibit the GSTM1 null genotype. Increased risk of bladder cancer has been reported in all cigarette smokers with GSTM1 null status[13]. The cause of MPCs in our patient may have been the long-term history of tobacco consumption. Further tests revealed that the patient had both invasive renal pelvis carcinoma and SLL. As a result, this case highlights the importance of lymphocytic infiltration in UC. Patients with cancer should always be investigated to rule out the possibility of a synchronous or metachronous malignancy.
Coincidence of CLL/SLL and UTUCs is an extremely rare situation. In a known case of malignancy, the presence of lymph nodes may indicate metastasis and may be misdiagnosed as advanced stage disease. The possibility of secondary malignancies such as lymphoma should be considered, and biopsy should be performed to confirm the diagnosis and stage the disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Spain; Ismail MAA, Egypt S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | Royle JA, Baade PD, Joske D, Girschik J, Fritschi L. Second cancer incidence and cancer mortality among chronic lymphocytic leukaemia patients: a population-based study. Br J Cancer. 2011;105:1076-1081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 2. | Chawla J, Selhi PK, Narang V, Sood N. Synchronous high-grade bladder carcinoma associated with chronic lymphocytic leukemia: A rare entity in Indian literature. J Cancer Res Ther. 2020;16:180-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Ramadan KM, Kyle A, McManus D, O'Rourke D, Cuthbert RJ. Urinary bladder infiltration with chronic B-lymphocytic leukemia: two cases with unusual presentation. Leuk Lymphoma. 2006;47:1184-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Baseskiogulu B, Canaz F, Kaya C, Dönmez T. The type of lymphocyte infiltration near urothelial carcinoma is diagnostic for chronic lymphocytic leukemia. Urol Ann. 2013;5:47-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Gajendra S, Sharma R, Sahoo MK. Triple cancer: chronic lymphocytic leukemia with bladder and prostate carcinoma. Malays J Pathol. 2015;37:159-163. [PubMed] |
| 6. | Rouprêt M, Babjuk M, Compérat E, Zigeuner R, Sylvester R, Burger M, Cowan N, Böhle A, Van Rhijn BW, Kaasinen E, Palou J, Shariat SF; European Association of Urology. European guidelines on upper tract urothelial carcinomas: 2013 update. Eur Urol. 2013;63:1059-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 343] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 7. | Lee TK, Myers RT, Scharyj M, Marshall RB. Multiple primary malignant tumors (MPMT): study of 68 autopsy cases (1963-1980). J Am Geriatr Soc. 1982;30:744-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Kelsh MA, Alexander DD, Kalmes RM, Buffler PA. Personal use of hair dyes and risk of bladder cancer: a meta-analysis of epidemiologic data. Cancer Causes Control. 2008;19:549-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Pathak AB, Advani SH, Gopal R, Nadkarni KS, Saikia TK. Urinary bladder cancer following cyclophosphamide therapy for Hodgkin's disease. Leuk Lymphoma. 1992;8:503-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Tsimberidou AM, Wen S, McLaughlin P, O'Brien S, Wierda WG, Lerner S, Strom S, Freireich EJ, Medeiros LJ, Kantarjian HM, Keating MJ. Other malignancies in chronic lymphocytic leukemia/small lymphocytic lymphoma. J Clin Oncol. 2009;27:904-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 166] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 11. | Müller D, Tomasović-Loncarić C, Galeic-Iljubanović D, Heinzl R, Savić I, Marusić P. Renal cell carcinoma with concurrent urothelial carcinoma of urinary bladder and non-Hodgkin lymphoma. Coll Antropol. 2012;36:1049-1052. [PubMed] |
| 12. | Lin CL, Lin CY, Chen SW. Coexisting transitional cell carcinoma and chronic lymphocytic leukemia/small lymphocytic lymphoma in urinary bladder. Zhonghua Zhongliu Xuebao. 2009;25:222-228. |
| 13. | Engel LS, Taioli E, Pfeiffer R, Garcia-Closas M, Marcus PM, Lan Q, Boffetta P, Vineis P, Autrup H, Bell DA, Branch RA, Brockmöller J, Daly AK, Heckbert SR, Kalina I, Kang D, Katoh T, Lafuente A, Lin HJ, Romkes M, Taylor JA, Rothman N. Pooled analysis and meta-analysis of glutathione S-transferase M1 and bladder cancer: a HuGE review. Am J Epidemiol. 2002;156:95-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 151] [Article Influence: 6.6] [Reference Citation Analysis (0)] |