Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8728
Peer-review started: March 17, 2022
First decision: May 30, 2022
Revised: June 12, 2022
Accepted: July 18, 2022
Article in press: July 18, 2022
Published online: August 26, 2022
Processing time: 151 Days and 9.7 Hours
The skull and dura are uncommon sites for the metastasis of hepatocellular carcinoma (HCC). Spontaneous acute epidural hematoma (AEDH) is also very rare. We report here a spontaneous AEDH secondary to skull and dural meta
A 48-year-old male patient with a history of HCC developed unconsciousness spontaneously. Head computed tomography showed "a huge AEDH in the left parietal and occipital region with osteolytic destruction of the left parietal bone. Emergent operation was performed to evacuate the hematoma and resect the lesion. Pathological study revealed that the lesion was the metastases from HCC. The patient died of lung infection, anemia, and liver failure 3 wk after operation.
Spontaneous AEDH caused by hepatocellular carcinoma (HCC) dural and skull metastases is extremely rare, the outcome is poor. So, early diagnosis is important. If the level of AFP does not decrease with the shrinkage of intrahepatic lesions after treatment, it is necessary to be alert to the existence of extrahepatic metastases. Since most of the patients had scalp and bone masses, physicians should pay attention to the patient's head palpation. Once a patient with the history of HCC had sudden neurological dysfunction, the possibility of spontaneous AEDH caused by the skull and dura mater metastases should be considered. Since hemorrhage is common in the skull HCC metastases, for patients with spontaneous AEDH accompanied by skull osteolytic lesions, it is also necessary to be alert to the possibility of HCC. For AEDH secondary to HCC metastases, early diagnosis and timely treatment are critical to improve the patients’ outcomes.
Core Tip: We present a case of hepatocellular carcinoma (HCC) metastasis to the skull and dura mater with spontaneous acute epidural hematoma (AEDH). This is the first report of spontaneous AEDH secondary to skull and dura mater metastasis from HCC in the Chinese population. Pathological examination provided evidence that the dura mater was one of the targets for HCC metastasis and could also lead to AEDH in addition to the reported skull metastases. We summarize the characteristics of the 8 reported cases worldwide, discuss the possible cause of AEDH, and offer advice for clinical practice.
- Citation: Lv GZ, Li GC, Tang WT, Zhou D, Yang Y. Spontaneous acute epidural hematoma secondary to skull and dural metastasis of hepatocellular carcinoma: A case report. World J Clin Cases 2022; 10(24): 8728-8734
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8728.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8728
Hepatocellular carcinoma (HCC) is one of the common malignant tumors in adults, with a high incidence in Southeast Asia where hepatitis B and C are prevalent[1]. Lung and bone metastases are the most common events in the terminal stage of the disease, but metastasis to the skull and the central nervous system is relatively rare[2]. Although traumatic acute epidural hematoma (AEDH) is quite often, the spontaneous AEDH is extremely rare. We are presenting a case of HCC metastasis to the skull and dura mater with spontaneous AEDH.
A 48-year-old male patient was found to be unconscious and accompanied by vomiting 3 h before admission.
The patient was diagnosed as HCC and received transarterial chemoembolization (TACE) 6 mo ago. 3 h before admission, he was found to be unconscious and accompanied by vomiting. He was transferred to our emergency by ambulance.
The patient had a history of hepatitis B, but did not take regular antiviral therapy as prescribed by the doctor. He was diagnosed as HCC (BCLC stage: B) and received TACE 6 mo ago in another hospital, the detailed treatment records were unavailable. The patient did not follow the doctor's suggestion for comprehensive treatment, nor did he have regular follow-up visits to the doctors.
No special personal and family history.
On arrival, physical examination revealed that the patient was in deep coma, Glasgow Coma score was 5 (E1V1M3). The left pupil dilated and the light reflection disappeared. No obvious traumatic change was observed on the scalp. A fixed elastic mass was found in the parieto-occipital area, without swelling or ulceration.
Laboratory examination revealed that alanine aminotransferase (ALT) was 80U/L, aspartate aminotransferase (AST) was 77U/L, the γ-glutamine transpeptidase (GGT) was 339 U/L, the albumin level was 42.6 g/L and the total bilirubin was 10.70μmol/L. The alpha-fetoprotein of this patient was over 1210 ng/mL. The platelet count of this patient was 132 × 109/L. The results of coagulation test showed: Prothrombin time (PT) 15.20 s, activated partial thromboplastin time (APTT) 36.00 s. Immunological test results for hepatitis B were HBsAg 691.19 IU/mL, HBeAg 0.01 IU/mL, HBeAb 0.75 IU/mL and HBcAg 146.13 IU/mL. The hepatitis B virus- deoxyribonucleic acid of this patient was 3.75 × 104 copies/mL.
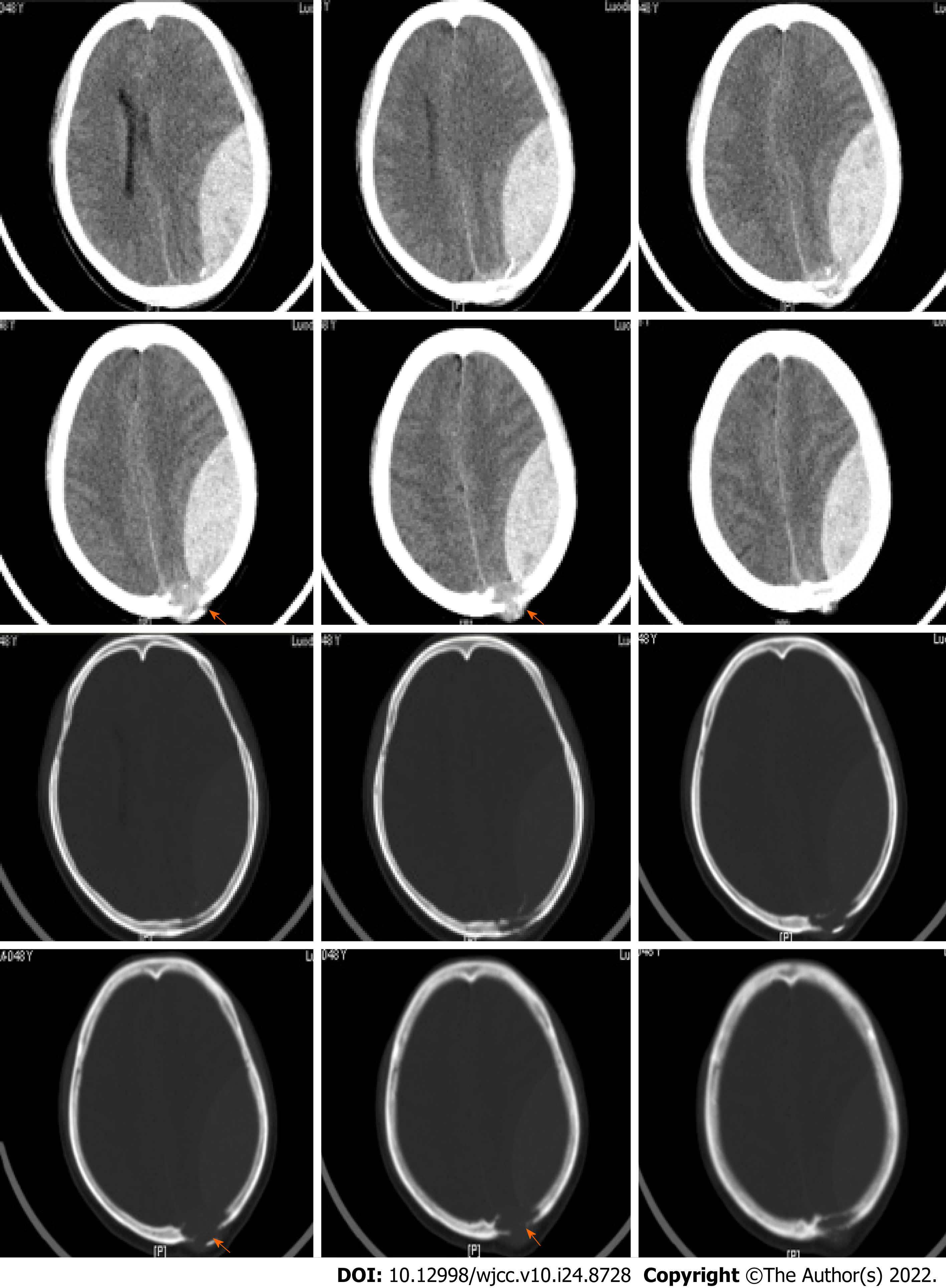
Head computed tomography (CT) showed “a huge AEDH in the left parietal and occipital region with osteolytic destruction of the left parietal bone” (Figure 1).
Cerebral hernia, Acute epidural hematoma, skull and dural metastasis of HCC (BCLC stage: C), hepatitis B infection, cirrhosis (Child-Pugh grade A).
The patient received emergency craniotomy to evacuate the hematoma. During the operation, the parietal bone was found being invaded by a gray-red elastic mass. After removing the bone flap and evacuating the hematoma, the base of the mass was found to be located on the dura mater, with abundant blood supply. The tumor and the invaded dura mater were resected. The base of the tumor was adjacent to the superior sagittal sinus, but did not invade the sinus. No hematoma or tumor invasion was found during the exploration of the subdural space. After resection of the skull lesion, the bone flap was put back and fixed properly.
After the operation, the pupils of the patient retracted to normal and were sensitive to light reflection, but the patient remained in light coma and underwent tracheotomy. A comprehensive postoperative examination revealed that the patient had lung and bone metastases. Later, the patient developed secondary lung infection, anemia, and liver failure, and died 3 wk after the operation.
Regional lymph nodes, lungs and bones are common sites for HCC metastasis. Osseous metastasis of HCC often occurs in vertebrae, pelvis and ribs, the skull is a rare metastatic site for HCC[2]. Spontaneous ADEH is very rare, and may be caused by infection, dural vascular anomalies, tumors or coagulopathies[3]. Most of the reported cases are spinal spontaneous AEDH. Intracranial spontaneous AEDH caused by metastases are extremely rare. Delgado et al[4] reported that epidural hematoma was the first presentation of HCC in a tiny portion of patients. As far as we know, only 8 cases of spontaneous AEDH caused by metastatic HCC have been reported so far, which are summarized below (Table 1). All of the patients were male and over 40 years old, 7/8 cases were from Asian countries, including South Korea and Japan. The geographical distribution of these cases may be related to the epidemiology of hepatitis virus infection. 7/8 patients came to the doctors due to AEDH related symptoms. Only 5/8 of the patients had known histories of HCC. The parieto-occipital region seems to be the preferred metastatic site (5/8). The metastatic HCC is highly invasive, all of the cases had osteolytic changes. Nearly half of the patients had lesions close to the sinus, where the arachnoid particles or the sinus might be eroded by the tumor and lead to hemorrhage. In addition, the lesions located at the base of the middle cranial fossa or the large wing of the sphenoid bone may be related to the erosion of the middle meningeal artery. Impaired liver function induced coagulopathy also contributed to the bleeding in 2 of the patients. The hematomas were huge in most of the cases, 5 of them had deteriorating consciousness and 4 of them developed brain herniation on diagnosis. The outcome of the patients was poor, only 1 patient survived, 1 patient left vegetative state, and the other 6 patients died of liver failure and related complications shortly after operation.
| Ref. | Age | Gender | Country | Metastases location | Close to the sinusor MMA | Osteolytic change | Clinical manifestations | Cerebral hernia | Previous diagnosed HCC | Coagulopathy | Outcome |
| Kim et al[2], 2016 | 41 | M | South Korea | Left parieto-occipital region | Y | Y | Headache, vomiting, drowsiness | N | Y | N | Died of liver failure, 4 mo later |
| McIver et al[5], 2001 | 50 | M | United States | Left parietal region | N | Y | Headache, right- sided weakness | N | N | NA | Survive |
| Hayashi et al[6], 2000 | 70 | M | Japan | Right parietal bone | N | Y | Headache, left-sided weakness | N | Y | Y | Died of liver failure and pneumonia 2 mo later |
| Kanai et al[7], 2008 | 56 | M | Japan | Left parieto-occipital region | Y | Y | Headache, deteriorating consciousness | Y | N | N | Died of liver failure 3 wk later |
| Nakagawa et al[8], 1992 | 52 | M | Japan | Occipital area | Y | Y | Headache, deteriorating consciousness | Y | N | NA | Died of liver tumor 4 mo later |
| Woo et al[9], 2010 | 46 | M | Korea | The greater wing of the right sphenoidBone | Y | Y | Severe headache, deteriorating consciousness | Y | Y | Y | Died of multi-organ failure 5 d later |
| Kim et al[10], 2010 | 53 | M | Korea | Right middleCranial fossa floor | Y | Y | Sudden mentalDeterioration to semicoma | Y | Y | NA | Vegetative state |
| Nakao et al[11], 1992 | 58 | M | Japan | Left frontal bone | N | Y | Scalp and bone mass | N | Y | N | Died of liver failure 15 mo later |
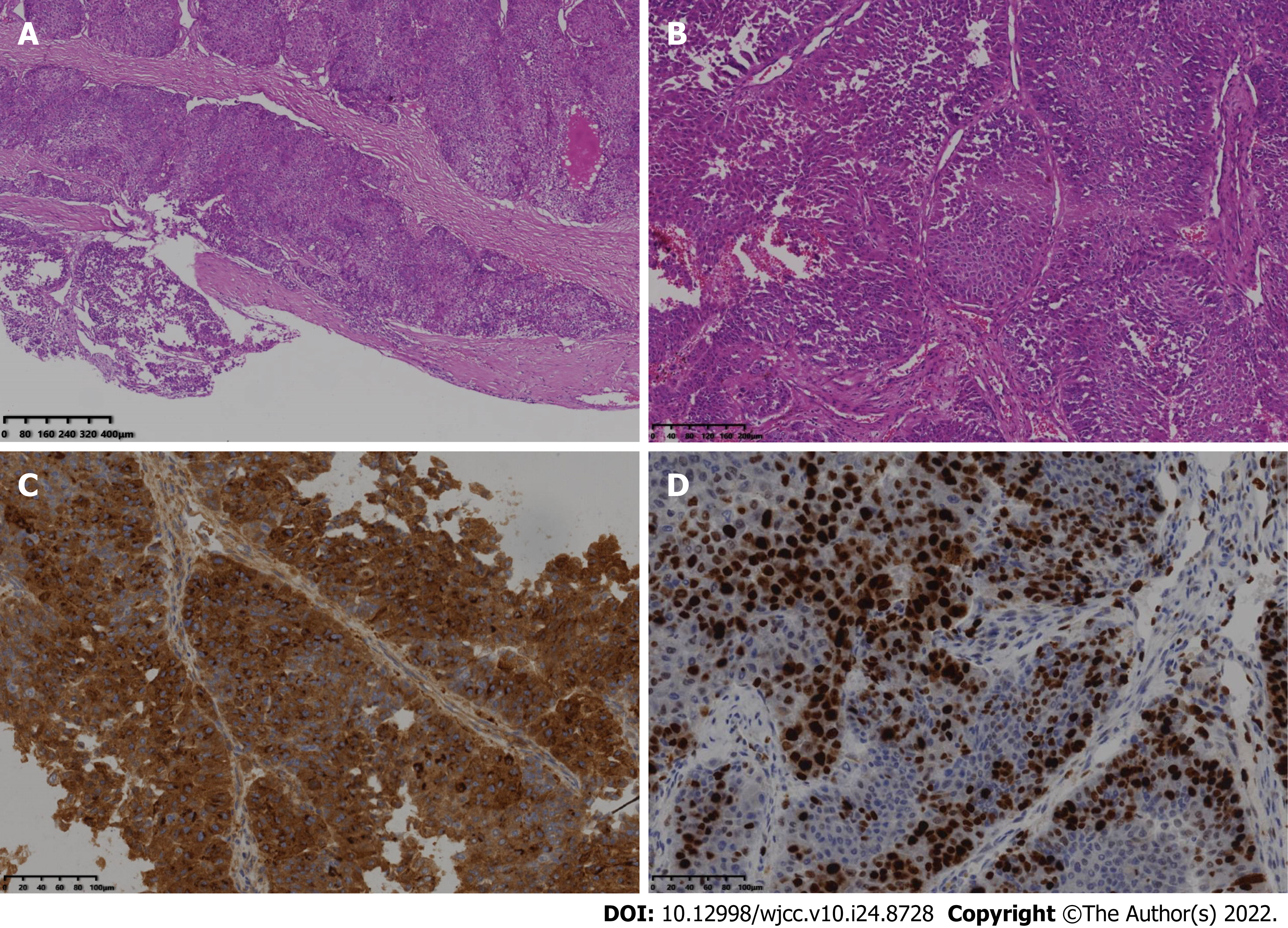
This is the first report of the spontaneous AEDH secondary to the skull and dura mater metastasis from HCC in the Chinese population. In this case, the spontaneous AEDH was huge and developed brain herniation. The patient died of liver failure shortly after the operation. Pathological study revealed that the tumor had a sinusoid structure and the dura mater was invaded by the metastatic tumor (Figure 2), which provided the evidence that the dura mater was also a target for HCC metastasis and could also lead to AEDH besides the reported skull metastases. Blood-rich sinusoid structure of HCC and the erosion of the adjacent sinus might contribute to the AEDH in this case. Postoperative coma delayed comprehensive treatment of the primary HCC. Due to the rapid progression of AEDH, timely and effective surgery can save the neurological function of patients to the greatest extent. According to the guiding role of BCLC staging in the treatment and prognosis of HCC, the post-operative Eastern Cooperative Oncology Group performance status (ECOG-PS) of these patients is important to the assessment of anti-cancer effect and expected survival[12]. If neurosurgical procedure restored the performance status to ECOG-PS 0 to 2, these patients could be defined as BCLC grade C, systemic therapy can be beneficial to these patients with the following anti-cancer options: Atezolizumab combined with bevacizumab, sorafenib, and Renvatinib as first-line therapy. Regorafenib and cabozantinib have been recommended as second-line treatments. With systemic anti-cancer treatment, the overall survival of these patients is expected between 8 to 13 mo. If surgical therapy cannot restore the ECOG-PS to under 2, the prognosis of these patients is pessimistic. Best supportive care can only prolong the survival up to 3 mo. So, the early diagnosis and timely treatment of AEDH secondary to HCC metastasis is extremely important. Therapies such as nucleoside analogues and anti-viral agents are also considered beneficial to these patients. Physicians should pay attention to whether the dynamic change of AFP is parallel to the liver associated manifestation. If the intrahepatic nodules shrink after TACE, but the AFP remain stable or even increase with follow-up, extrahepatic metastasis should be considered. A systemic physical examination and multiple organ imaging examinations such as PET/CT allowed these patients to discover the asymptomatic metastases which require timely intervention. Early diagnosis of the metastases is the key to prevent lethal complications such as AEDH.
Spontaneous AEDH caused by HCC dural and skull metastases is extremely rare, the outcome is poor. So, early diagnosis is important. If the level of AFP does not decrease with the shrinkage of intrahepatic lesions after treatment, it is necessary to be alert to the existence of extrahepatic metastases. Since most of the patients had scalp and bone masses, physicians should pay attention to the patient's head palpation. Once a patient with the history of HCC had sudden neurological dysfunction, the possibility of spontaneous AEDH caused by the skull and dura mater metastases should be considered. Since hemorrhage is common in the skull HCC metastases, for patients with spontaneous AEDH accompanied by skull osteolytic lesions, it is also necessary to be alert to the possibility of HCC. For AEDH secondary to HCC metastases, early diagnosis and timely treatment are critical to improve the patients’ outcomes.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu CH, Taiwan; Su YY, Taiwan S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16:589-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2184] [Cited by in RCA: 2893] [Article Influence: 482.2] [Reference Citation Analysis (17)] |
| 2. | Kim YS, Moon KS, Lee KH, Jung TY, Jang WY, Kim IY, Jung S. Spontaneous acute epidural hematoma developed due to skull metastasis of hepatocelluar carcinoma: A case report and review of the literature. Oncol Lett. 2016;11:741-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Zhang B, Chen J, Zou N, Wang L, Wang H, Jiang J, Chen D, Lu X. Spontaneous resolution and complete recovery of spontaneous cervical epidural hematoma: Report of two cases and literature review. Neurochirurgie. 2019;65:27-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Delgado Maroto A, Del Moral Martinez M, Dieguez Castillo C, Casado Caballero FJ. Acute epidural haematoma as a presentation of hepatocellular carcinoma: Case report and literature review. Gastroenterol Hepatol. 2019;42:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | McIver JI, Scheithauer BW, Rydberg CH, Atkinson JL. Metastatic hepatocellular carcinoma presenting as epidural hematoma: case report. Neurosurgery. 2001;49:447-449.. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Hayashi K, Matsuo T, Kurihara M, Daikoku M, Kitange G, Shibata S. Skull metastasis of hepatocellular carcinoma associated with acute epidural hematoma: a case report. Surg Neurol. 2000;53:379-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Kanai R, Kubota H, Terada T, Hata T, Tawaraya E, Fujii K. Spontaneous epidural hematoma due to skull metastasis of hepatocellular carcinoma. J Clin Neurosci. 2009;16:137-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Nakagawa Y, Yoshino E, Suzuki K, Tatebe A, Andachi H. Spontaneous epidural hematoma from a hepatocellular carcinoma metastasis to the skull--case report. Neurol Med Chir (Tokyo). 1992;32:300-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Woo KM, Kim BC, Cho KT, Kim EJ. Spontaneous epidural hematoma from skull base metastasis of hepatocellular carcinoma. J Korean Neurosurg Soc. 2010;47:461-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Kim BG, Yoon SM, Bae HG, Yun IG. Spontaneous intracranial epidural hematoma originating from dural metastasis of hepatocellular carcinoma. J Korean Neurosurg Soc. 2010;48:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Nakao N, Kubo K, Moriwaki H. Cranial metastasis of hepatocellular carcinoma associated with chronic epidural hematoma--case report. Neurol Med Chir (Tokyo). 1992;32:100-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2066] [Cited by in RCA: 3165] [Article Influence: 527.5] [Reference Citation Analysis (37)] |