Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8615
Peer-review started: April 11, 2022
First decision: May 30, 2022
Revised: June 11, 2022
Accepted: July 25, 2022
Article in press: July 25, 2022
Published online: August 26, 2022
Processing time: 126 Days and 17.7 Hours
Hypoxemia is a common complication in older patients during postoperative recovery and can cause pulmonary complications. Therefore, reducing the incidence of postoperative hypoxemia is a clinical concern.
To investigate the clinical efficacy of high-flow nasal cannula oxygen (HFNCO) in the resuscitation period of older orthopedic patients.
In this prospective randomized controlled trial, 60 older patients who underwent orthopedic surgery under general anesthesia were randomly divided into two groups: those who used conventional face mask and those who used HFNCO. All patients were treated with 60% oxygen for 1 h after extubation. Patients in the conventional face mask group were treated with a combination of air (2 L) and oxygen (2 L) using a traditional mask, whereas those in the HFNCO group were treated with HFNCO at a constant temperature of 34 °C and flow rate of 40 L/min. We assessed the effectiveness of oxygen therapy by monitoring the patients’ arterial blood gas, peripheral oxygen saturation, and postoperative complications.
The characteristics of the patients were comparable between the groups. One hour after extubation, patients in HFNCO group had a significantly higher arterial partial pressure of oxygen (paO2) than that of patients in conventional face mask group (P < 0.001). At extubation and 1 h after extubation, patients in both groups showed a significantly higher arterial partial pressure of carbon dioxide (paCO2) than the baseline levels (P < 0.001). There were no differences in the saturation of peripheral oxygen, paO2, and paCO2 between the groups before anesthesia and before extubation (P > 0.05). There were statistically significant differences in paO2 between the two groups before anesthesia and 1 h after extubation and immediately after extubation and 1 h after extubation (P < 0.001). However, there were no significant differences in the oxygen tolerance score before leaving the room, airway humidification, and pulmonary complications 3 d after surgery between the two groups (P > 0.05).
HFNCO can improve oxygen partial pressure and respiratory function in elderly patients undergoing orthopedic surgery under general endotracheal anesthesia. Thus, HFNCO can be used to prevent postoperative hypoxemia.
Core Tip: This prospective randomized controlled study involving 60 patients evaluated the effects of different oxygen delivery methods. Additionally, the study investigated the clinical efficacy of high-flow nasal cannula oxygen (HFNCO) on the recovery period of older orthopedic patients. The current results showed that HFNCO can improve oxygen partial pressure and respiratory function in older patients undergoing orthopedic surgery with general anesthesia under endotracheal intubation.
- Citation: Li XN, Zhou CC, Lin ZQ, Jia B, Li XY, Zhao GF, Ye F. High-flow nasal cannula oxygen therapy during anesthesia recovery for older orthopedic surgery patients: A prospective randomized controlled trial. World J Clin Cases 2022; 10(24): 8615-8624
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8615.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8615
With aging of the global population, the number of orthopedic surgeries required for older patients is increasing annually. With the advances in ultrasonography-guided nerve block technology, the combination of general anesthesia with nerve block is increasingly used in orthopedic surgeries for older patients. However, patients often present with hypoxemia when the tracheal tube is removed after surgery, due to pre-existing chronic diseases and a decline in organ reserve. Additionally, following general anesthesia, the clinical manifestations of inherent diseases and conditions, such as chronic obstructive pulmonary disease, slow anesthesia metabolism, and lung injury, become apparent again. Currently, the accepted diagnostic criterion for hypoxemia is saturation of peripheral oxygen (SpO2) ≤ 90%. The postoperative incidence of hypoxemia can reach 28%-50%. Hypoxemia may cause postoperative delirium and wound infection[1], and in severe cases, it may lead to multiple types of arrhythmia, nervous system injury, and abnormal changes in blood pressure. It can also increase the orthopedic perioperative risk in older patients, affect postoperative recovery, and even extend the length of hospital stay, and consequently, increase the economic burden. High-flow nasal cannula oxygen (HFNCO) is a new noninvasive oxygen therapy technology. As HFNCO can be used to improve oxygenation and manage hypoxemia rapidly and efficiently, it can heat and humidify inhaled air. Furthermore, it is convenient and comfortable[2] and has been gradually used in clinics in recent years. Clinical reports suggest that it can be applied in the comprehensive treatment of various respiratory diseases, especially in the transitional treatment before extubation, prevention and treatment of respiratory failure after extubation, and treatment of postoperative patients complicated with hypoxemia[3]. This randomized controlled trial aimed to report on the clinical efficacy of HFNCO and compare the effects of conventional mask oxygen and HFNCO on the recovery period of older (≥ 65 years) patients following orthopedic surgery. It was hypothesized that HFNCO may improve oxygen partial pressure and reduce the incidence of postoperative hypoxemia in older patients undergoing elective orthopedic surgery.
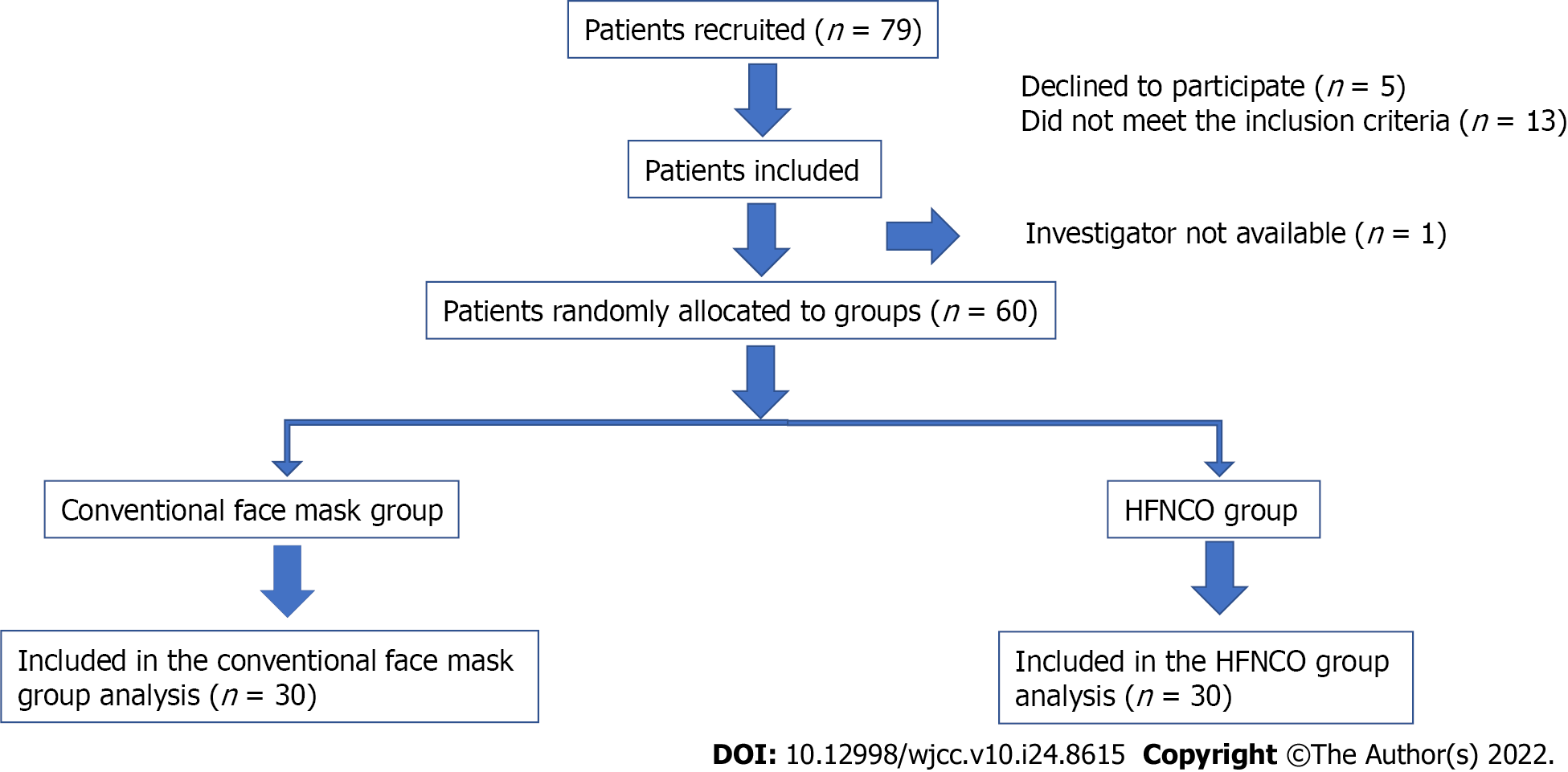
From February to August 2021, 60 older patients eligible for orthopedic surgery under general endotracheal anesthesia at the Department of Orthopedics, Guangdong Hospital of Traditional Chinese Medicine, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangdong Province, China, were selected and randomly assigned to receive conventional mask oxygen or nasal high-flow oxygen inhalation, with 30 patients in each group. The envelope method was adopted for random grouping using random codes made in advance, with each code placed into the envelope and independently sealed. After the patients who met the inclusion criteria were enrolled into the study, the envelopes were opened in sequence, and the patients were treated as directed by the random-assignment card (Figure 1).
Patients undergoing orthopedic surgery, who met the surgical requirements as assessed by an orthopedic clinician, were considered for inclusion in this trial. The inclusion criteria were orthopedic patients aged ≥ 65 years who were selected for endotracheal general anesthesia, with American Society of Anesthesiologists (ASA) grade I-III, and provided written informed consent after being oriented about the study. The exclusion criteria were severe bullae of the lung, severe or extremely severe lung function, grade IV cardiac function grading, with known mental illness and/or inability to communicate with language partners, and/or serious non-cooperation.
Electrocardiography, blood pressure, and SpO2 were routinely monitored in all older patients undergoing orthopedic surgery after entering the operating room, and radial artery catheterization was performed to establish arterial pressure monitoring. Induction and maintenance of anesthesia were performed as follows: (1) Induction: Sufentanil, 0.3-0.4 μg/kg; etomidate, 0.3 mg/kg; cis-atracurium, 0.1-0.15 mg/kg; and (2) maintenance: Sevoflurane, 1%-2%; intermittent addition of sufentanil and cis-atracurium. After endotracheal intubation or laryngeal mask placement, the anesthesia machine was connected to control the respiration. The tidal volume and respiratory rate were 6-8 mL/kg and 12-15 times/min, respectively, and the end-expiratory carbon dioxide was maintained at 35-45 mmHg. In the event of blood pressure fluctuations during anesthesia, the clinical team determined the cause, including anesthesia, operation, or patient-related factors. For example, in a case of systolic blood pressure fluctuation, the clinical team decided to use drugs to control the patient’s blood pressure; then, the patient was transferred to the postanesthesia care unit (PACU) for extubation after surgery. After extubation, patients were randomly assigned to one of two groups to receive either conventional mask or HFNCO therapy. Blood gas analysis, including evaluation of the arterial partial pressure of oxygen (paO2), arterial partial pressure of carbon dioxide (paCO2) and pH before induction of anesthesia, during extubation, and 1 h after extubation, was conducted for all older orthopedic patients. Additionally, the heart rate (HR), blood pressure, and SpO2 of all participants were observed before anesthesia induction, during extubation, and 10 min, 15 min, 30 min, and 1 h after extubation in older orthopedic patients. The patients’ oxygen tolerance scores were recorded as follows: (1) The patient was satisfied with the treatment; (2) the patient was not satisfied with the treatment; (3) the patient desired to remove the oxygen inhalation device but did not remove it by himself; (4) the patient removed the oxygen device by himself/herself; and (5) the patient refused to apply oxygen. Airway humidification was evaluated and was graded as satisfactory when the patient coughed up sputum easily, the sputum was thin, and the breathing was unobstructed. Conversely, humidification was unsatisfactory when the patient’s sputum was sticky and hard to cough up and the patient had a rapid HR and decreased peripheral blood oxygen saturation. Additionally, the incidence of complications 3 d after the operation were evaluated.
The conventional mask group was treated with conventional mask oxygen inhalation for 1 h after extubation, with a flow rate of 2 L air plus 2 L O2/min. Whereas, after extubation, the HNFCO group was treated with oxygen therapy using a high-flow nasal humidifier for 1 h via a special breathing line and nasal plug catheter. The gas flow rate was 40 L/min, the temperature was raised to 34 °C, and the inhaled oxygen concentration was 60%. If patients developed intolerance to HFNCO during treatment, the course of action was to immediately discontinue treatment and switch to conventional mask therapy to ensure safety and comfort.
The patient information database was created using Excel and SPSS 18.0 software packages. Continuous variables were described as median (interquartile range), while categorical variables were described as composition ratio and rate. For continuous variables with a normal distribution and homogeneity of variance, the independent t-test was used for inter-group comparison. The Mann-Whitney U test was used for continuous variables with non-normal distributions or uneven variance, and the paired t test (or Wilcoxon test) was used for intra-group comparison. When baseline values were unequal, univariate analysis of variance was performed. Between-group comparisons of categorical variables were performed using tests (or Fisher’s exact test). The rank sum test was used for comparison of grade data between groups. Significance level was set at α = 0.05 (normality test α = 0.10).
The preoperative baseline characteristics of the patients are presented in Table 1. There were no significant differences between the two groups in terms of sex, age, body weight, body mass index (BMI), and ASA grade (P > 0.05). There were no significant differences in the HR, mean arterial pressure (MAP), pH, paCO2, paO2, glucose level, and lactic acid level between the two groups before anesthesia and extubation. SpO2 was not significantly different from that before anesthesia, but was at extubation (P > 0.05, Table 2).
| Characteristic | Conventional mask group (n = 30) | HFNCO group (n = 30) | P value |
| Age (yr) | 72.8 ± 5.7 | 72.5 ± 4.3 | 0.778 |
| Sex | |||
| Male | 9 (30) | 10 (33.3) | 0.781 |
| Female | 21 (70) | 20 (66.7) | |
| Weight (kg) | 62.4 ± 10.5 | 63.1 ± 8.0 | 0.756 |
| BMI | 25.1 ± 3.8 | 25.3 ± 3.5 | 0.793 |
| ASA | |||
| II | 15 (50) | 21 (70) | 0.114 |
| III | 15 (50) | 9 (30) | |
| Operation type | 0.320 | ||
| TKA | 18 (60) | 13 (43.3) | |
| Spinal surgery | 6 (20) | 11 (36.7) | |
| Others | 6 (20) | 6 (20) |
| Conventional mask group (n = 30) | HFNCO group (n = 30) | P value | |
| Before anesthesia | |||
| HR | 75.9 ± 11.4 | 74.7 ± 9.6 | 0.652 |
| MAP | 118.8 (109.0, 128.3) | 119.8 (105.0, 126.6) | 0.6521 |
| SpO2 | 98.0 (97.0, 100.0) | 99.0 (97.0, 100.0) | 0.3211 |
| pH | 7.42 (7.40, 7.43) | 7.42 (7.41, 7.44) | 0.2611 |
| paCO2 | 37.7 (75.4, 39.7) | 38.9 (36.5, 40.6) | 0.3291 |
| paO2 | 78.9 (70.5, 85.3) | 76.8 (70.0, 84.0) | 0.9531 |
| Glucose | 5.5 (5.3, 6.6) | 5.6 (5.3, 6.3) | 0.9471 |
| Lactic acid | 1.3 (1.0, 1.8) | 1.3 (1.1, 1.5) | 0.6891 |
| Extubation | |||
| HR | 78.6 ± 11.8 | 73.9 ± 11.3 | 0.122 |
| MAP | 107.8 (102.3, 126.0) | 110.5 (96.8, 117.5) | 0.6631 |
| SpO2 | 100.0 (99.0, 100.0) | 100.0 (100.0, 100.0) | 0.0401 |
| pH | 7.33 (7.30, 7.35) | 7.33 (7.30, 7.37) | 0.3671 |
| paCO2 | 48.1 (43.6, 54.1) | 48.0 (43.6, 54.7) | 0.9761 |
| paO2 | 75.1 (64.0, 86.3) | 74.0 (67.2, 89.7) | 0.7511 |
| Glucose | 6.2 (5.7, 7.5) | 6.6 (5.4, 7.5) | 0.9001 |
| Lactic acid | 1.8 (1.5, 2.2) | 1.7 (1.3, 2.5) | 0.9411 |
Upon comparison of the outcome indexes after extubation between the two groups, the HFNCO group had significantly higher paO2 than the conventional mask group 1 h after extubation (P < 0.001). There was no significant difference in paCO2 between the two groups (P > 0.05). At extubation and 5 min, 15 min, and 30 min after extubation, the HFNCO group had significantly higher SpO2 than the conventional mask group (P < 0.05). At extubation and at 5 min, 15 min, 30 min, and 1 h after extubation, the SpO2 level of the HFNCO group was significantly higher than that of the conventional mask group. However, since there was a difference between the two groups before the intervention, i.e., at the time of extubation, we used the SpO2 level at the time of extubation as a covariable for covariance analysis, and the corrected results showed no statistically significant differences between the two groups. Additionally, there were no significant differences in HR, MAP, PH, glucose level, and lactic acid level between the two groups (P > 0.05, Table 3).
| Conventional mask group (n = 30) | HFNCO group (n = 30) | P value | |
| 5 min after extubation | |||
| HR | 76.0 ± 12.8 | 71.3 ± 11.0 | 0.138 |
| MAP | 108.3 (99.0, 120.5) | 105.5 (96.3, 115.1) | 0.4731 |
| SpO2 | 100.0 (97.8, 100.0) | 100.0 (100.0, 100.0) | 0.0321 |
| 15 min after extubation | |||
| HR | 76.6 ± 12.7 | 71.4 ± 10.5 | 0.091 |
| MAP | 108.5 (96.0, 121.9) | 105.3 (95.9, 118.6) | 0.6201 |
| SpO2 | 100.0 (98.0, 100.0) | 100.0 (100.0, 100.0) | 0.0011 |
| 30 min after extubation | |||
| HR | 75.9 ± 13.1 | 70.3 ± 8.8 | 0.054 |
| MAP | 107.5 (97.0, 117.6) | 111.0 (100.3, 117.8) | 0.6731 |
| SpO2 | 100.0 (98.8, 100.0) | 100.0 (100.0, 100.0) | 0.0021 |
| 1 h after extubation | |||
| HR | 76.5 ± 13.6 | 71.0 ± 9.2 | 0.073 |
| MAP | 105.8 (97.3, 119.1) | 107.5 (110.5, 121.0) | 0.6471 |
| SpO2 | 100.0 (99.0, 100.0) | 100.0 (100.0, 100.0) | 0.0031 |
| pH | 7.36 (7.34, 7.38) | 7.36 (7.33, 7.37) | 0.6521 |
| paCO2 | 44.0 (40.1, 48.2) | 45.3 (41.8, 49.8) | 0.7061 |
| paO2 | 114.0 (83.5, 147.6) | 194.9 (162.9, 242.2) | < 0.0011 |
| Glucose | 8.3 (6.5 ,8.9) | 7.6 (6.5, 8.7) | 0.5691 |
| Lactic acid | 1.4 (1.1, 1.7) | 1.4 (1.1, 1.8) | 0.9411 |
The paCO2 level of patients in the two groups was significantly higher at extubation and 1 h after extubation than before anesthesia (P < 0.001). The paCO2 level was significantly lower at 1 h after extubation than at extubation (P < 0.05). There was no significant difference in the paO2 level between the two groups before anesthesia and before extubation (P > 0.05). Both groups had significantly increased paO2 1 h after extubation compared with before anesthesia and at extubation (P < 0.001). The glucose level in both groups increased significantly 1 h after extubation compared with that before anesthesia and extubation (P < 0.001). In both groups, the lactic acid level was significantly increased at extubation compared with before anesthesia (P < 0.001) and significantly decreased at 1 h after extubation when compared with at extubation (P < 0.001).
Comparison of clinical efficacy indicators and complications between the two groups showed no significant differences in the oxygen tolerance score before PACU and pulmonary complications 3 d after surgery, based on airway humidification assessment (P > 0.05, Table 4).
| Conventional mask group (n = 30), n (%) | HFNCO group (n = 30), n (%) | P value | |
| Patients’ oxygen tolerance score | 0.0781 | ||
| 1 | 29 (96.7) | 30 (100) | |
| 2 | 0 | 0 | |
| 3 | 1 (3.3) | 0 | |
| 4 | 0 | 0 | |
| 5 | 0 | 0 | |
| Airway humidification | 0.237 | ||
| Yes | 27 (90) | 30 (100) | |
| No | 3 (10) | 0 |
Despite the development of new orthopedic surgery methods, age-related changes in lung physiology, such as the deterioration of respiratory compliance and reduced responses to hypoxemia and other protective airway reflexes, increase the incidence of hypoxemia and pulmonary complications following orthopedic surgery in older patients[4]. Studies have shown that nearly 100% of patients will have atelectasis during general anesthesia, and postoperative hypoxemia and pulmonary complications may occur[5]. To some extent, this increases the perioperative risk of older orthopedic patients, affects postoperative recovery, and even extends the hospital stay, thus increasing the economic burden on patients[6]. HFNCO was originally used as a non-invasive, easy-to-use respiratory support therapy for acute hypoxic respiratory failure in adults, and it has been proven to be effective in patients with acute respiratory failure[5,7]. In recent years, high-flow oxygen therapy has been widely used in different clinical settings; however, experience in the use of HFNCO during the recovery period in older patients following orthopedic surgery under general anesthesia is limited, which prompted us to conduct this study.
This study showed that among older patients undergoing elective orthopedic surgery, the paO2 in patients who used HFNCO was significantly higher than that in patients who used conventional mask. Additionally, paO2 increased significantly at 1 h after extubation compared with that before anesthesia and at extubation. HFNCO provides a flow rate of up to 60 L/min, with almost no entrainment of room air during inhalation; this is combined with exhaled air from the upper respiratory tract. These mechanisms ensure a more reliable high-oxygen concentration. Flushing of the dead airway cavity by a trans-nasal high-flow oxygen humidifier also improves ventilation efficiency, reduces respiratory work, and produces positive end-expiratory pressure (PEEP), which may counteract intrinsic PEEP, improve oxygenation, and provide back pressure to enhance airway patency at expiration, thereby achieving more complete lung emptying[8,9]. These findings suggest that HFNCO may be more beneficial for older patients undergoing elective orthopedic surgery after intubation. After extubation, the SpO2 level of the HFNCO group was significantly higher than that of the conventional mask group in covariance analysis, and the results showed no significant differences between the two groups after correction. Clinically, SpO2 ≤ 90% was defined as hypoxemia; the SpO2 level was > 90% in both the conventional mask and HFNCO groups at 15 min and 30 min after extubation. Although there was a significant difference, there was no specific clinical significance. Additionally, the inhaled oxygen concentration in the HFNCO group was the same as that in the mask group, but the HFNCO group had a higher oxygen flow; thus, better oxygen uptake could be achieved (higher arterial paO2). However, owing to the suctioning of air before anesthesia and extubation, the inhaled oxygen concentration was only 21%. Mechanical ventilation during surgery and anesthesia may cause lung injury. Additionally, there was a certain amount of oxygen reserve during extubation. In this study, four patients in the two groups had paO2 lower than 80 mmHg after 1 h of treatment with different oxygen administration methods. All four patients were in the conventional mask group, indicating that there were no patients with hypoxemia in the HFNCO group. Therefore, HFNCO may significantly reduce the incidence of hypoxemia.
In the HFNCO group, paCO2 increased from that before anesthesia to after extubation and decreased after 1 h of high-flow oxygen treatment. In the conventional mask group, paCO2 increased from that before anesthesia to after extubation and decreased after 1 h of high-flow oxygen treatment. However, there was no significant difference in paCO2 between the two groups at different time points, and the paCO2 level was significantly lower at 1 h after extubation than at extubation. In both groups, the paCO2 level was significantly higher at extubation and 1 h after extubation than before anesthesia. The patient may experience some lung injury during mechanical ventilation and surgery during anesthesia; thus, the paCO2 level was slightly higher at extubation than before. However, after oxygen treatment for 1 h after extubation, the paCO2 level was significantly lower than before indicating that adequate oxygen treatment after extubation may be conducive to the recovery of lung function.
The glucose levels in both groups at 1 h after extubation were significantly higher than those before anesthesia and at extubation. This was thought to be mainly related to surgical stress. Hyperglycemia in perioperative patients has been identified as a risk factor for a poor prognosis after various surgical procedures[10]. In this study, some patients had diabetes, suggesting that perioperative blood glucose control is also crucial. The lactic acid levels increased from 1.4 to 1.9 mmol/L and then decreased to 1.5 mmol/L in both groups. Although there was a significant difference, both were within the normal ranges and had no clinical significance. Perioperative adverse events can affect the prognosis of patients, especially during and after surgery, and possible anesthesia-related adverse events are often ignored. Intraoperative visceral tissue perfusion can easily be damaged. As a good indicator of tissue perfusion, lactic acid should not be ignored during the perioperative period. Oxygen is carried by blood flow, mainly by hemoglobin, for microcirculation. Perioperative patients with reduced circulating blood volume (insufficient cardiac output), insufficient hemoglobin, or reduced hematocrit will experience reduced oxygen delivery, resulting in tissue hypoperfusion[11,12]. Hypoperfusion and the resulting tissue hypoxia are common causes of a poor prognosis. During operation, patients are in a controlled environment and have relatively stable oxygen inhalation. However, because of various subjective and objective factors after catheterization, it is important to ensure a certain amount of oxygen inhalation to enable tissue perfusion, which is also an advantage of HFNCO.
In cases of coronavirus disease (COVID-19), patients with severe illness often have varying degrees of hypoxia and dyspnea; therefore, respiratory support is very important for these patients. Studies have shown that compared with conventional oxygen therapy[13], early HFNCO oxygen therapy can improve the oxygenation function and respiratory rate of patients with severe COVID-19, while improving the patient’s infection indicators and reducing the length of stay in the intensive care unit. Consistent with our study, Oczkowski et al[14] showed that HFNCO would lead to a higher paO2/FiO2 ratio and paO2 value, but has no significant effect on paCO2 value. In patients with no COVID-19, the European Respiratory Society recommends HFNCO instead of conventional nasal intubation and noninvasive ventilation for patients with hypoxic respiratory failure[14].
Multiple studies have shown that HFNCO can potentially promote spontaneous breathing, prevent patient fatigue, and reduce the risk of self-induced lung injury. HFNCO can improve patient comfort and tolerance compared with conventional mask oxygen delivery[15]. The patients included in this study were evaluated under different types of HFNCO environmental comfort. Oxygen treatment 1 h after extubation, the airway of wetting effect basic satisfaction, and oxygen tolerance grade, which may result in oxygen treatment for a shorter duration. This was one of the limitations of this experiment. Additionally, the postoperative follow-up time interval was shorter, and fewer participants were assessed for comfort. Thus, this may only be regarded as a secondary psychological result; for example, when the patients’ physical and psychological comfort requirements are satisfied, they will have a sense of relief. Overall, no postoperative complications were observed; this may be related to patients’ subjective reporting or the short observation time, which is thus another study limitation. There was no statistically significant difference in airway humidification between the two groups in our study. However, Wang et al[16] showed in their study that the application of HFNCO in senior patients with LRTI could improve respiratory humidification, reduce the number of sputum aspirations, and improve anti-inflammatory effects. This may be due to our short observation period and the relatively simple method for evaluating airway humidification.
This study found that HFNCO could effectively improve oxygen partial pressure and respiratory function in older patients undergoing elective orthopedic surgery. Thus, HFNCO can be used to prevent postoperative hypoxemia.
In the future, we can extend the follow-up time, refine the evaluation indicators, further clarify the postoperative complications of elderly orthopedic surgery patients and use traditional Chinese medicine for intervention.
High-flow nasal cannula oxygen (HFNCO) can improve oxygen partial pressure and respiratory function in elderly patients undergoing orthopedic surgery under general endotracheal anesthesia. Thus, HFNCO can be used to prevent postoperative hypoxemia.
In comparison between the two groups, arterial partial pressure of oxygen (paO2) in HFNCO group was significantly better than that in the conventional group, while no significant differences were observed in other indicators. In intra-group comparison, paO2 had statistical differences at all time periods, pressure of carbon dioxide (paCO2) had statistically significant differences before and after extubation, and the other data showed no significant differences.
In this prospective randomized controlled trial, 60 older patients who underwent orthopedic surgery under general anesthesia were randomly divided into two groups: those who used conventional face mask and those who used HFNCO. Blood gas analysis, including evaluation of the paO2, paCO2 and pH before induction of anesthesia, during extubation, and 1 h after extubation, was conducted for all older orthopedic patients. The patient information database was created and analysis using Excel and SPSS 18.0 software packages.
This randomized controlled trial aimed to report on the clinical efficacy of HFNCO and compare the effects of conventional mask oxygen and HFNCO on the recovery period of older (≥ 65 years) patients following orthopedic surgery.
As HFNCO can be used to improve oxygenation and manage hypoxemia rapidly and efficiently, it can heat and humidify inhaled air. Furthermore, it is convenient and comfortable and has been gradually used in clinics in recent years.
Hypoxemia may cause postoperative delirium and wound infection, and in severe cases, it may lead to multiple types of arrhythmia, nervous system injury, and abnormal changes in blood pressure. It can also increase the orthopedic perioperative risk in older patients, affect postoperative recovery, and even extend the length of hospital stay, and consequently, increase the economic burden. We hypothesized that HFNCO has an advantage over conventional mask oxygen in the resuscitation period of older orthopedic patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Chhabada S, United States; Li TY, Taiwan S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Nishimura M. High-Flow Nasal Cannula Oxygen Therapy in Adults: Physiological Benefits, Indication, Clinical Benefits, and Adverse Effects. Respir Care. 2016;61:529-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 276] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 2. | Masclans JR, Pérez-Terán P, Roca O. The role of high flow oxygen therapy in acute respiratory failure. Med Intensiva. 2015;39:505-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Porhomayon J, El-Solh AA, Pourafkari L, Jaoude P, Nader ND. Applications of Nasal High-Flow Oxygen Therapy in Critically ill Adult Patients. Lung. 2016;194:705-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Güldner A, Kiss T, Serpa Neto A, Hemmes SN, Canet J, Spieth PM, Rocco PR, Schultz MJ, Pelosi P, Gama de Abreu M. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123:692-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 270] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 5. | Helviz Y, Einav S. A Systematic Review of the High-flow Nasal Cannula for Adult Patients. Crit Care. 2018;22:71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 97] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 6. | Fraser JF, Spooner AJ, Dunster KR, Anstey CM, Corley A. Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax. 2016;71:759-761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 146] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 7. | Spoletini G, Alotaibi M, Blasi F, Hill NS. Heated Humidified High-Flow Nasal Oxygen in Adults: Mechanisms of Action and Clinical Implications. Chest. 2015;148:253-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 257] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 8. | Pisani L, Vega ML. Use of Nasal High Flow in Stable COPD: Rationale and Physiology. COPD. 2017;14:346-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 48] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 9. | Hommel I, van Gurp PJ, den Broeder AA, Wollersheim H, Atsma F, Hulscher MEJL, Tack CJ. Reactive Rather than Proactive Diabetes Management in the Perioperative Period. Horm Metab Res. 2017;49:527-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Kinaci E, Sevinc MM, Ozakay A, Bayrak S, Cakar E, Sari S. Intraoperative acidosis is a new predictor for postoperative pancreatic fistula after pancreaticoduodenectomy. Hepatobiliary Pancreat Dis Int. 2016;15:302-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, Prat G, Boulain T, Morawiec E, Cottereau A, Devaquet J, Nseir S, Razazi K, Mira JP, Argaud L, Chakarian JC, Ricard JD, Wittebole X, Chevalier S, Herbland A, Fartoukh M, Constantin JM, Tonnelier JM, Pierrot M, Mathonnet A, Béduneau G, Delétage-Métreau C, Richard JC, Brochard L, Robert R; FLORALI Study Group; REVA Network. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372:2185-2196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1232] [Cited by in RCA: 1377] [Article Influence: 137.7] [Reference Citation Analysis (0)] |
| 12. | Papazian L, Corley A, Hess D, Fraser JF, Frat JP, Guitton C, Jaber S, Maggiore SM, Nava S, Rello J, Ricard JD, Stephan F, Trisolini R, Azoulay E. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med. 2016;42:1336-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 196] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 13. | Teng XB, Shen Y, Han MF, Yang G, Zha L, Shi JF. The value of high-flow nasal cannula oxygen therapy in treating novel coronavirus pneumonia. Eur J Clin Invest. 2021;51:e13435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Oczkowski S, Ergan B, Bos L, Chatwin M, Ferrer M, Gregoretti C, Heunks L, Frat JP, Longhini F, Nava S, Navalesi P, Ozsancak Uğurlu A, Pisani L, Renda T, Thille AW, Winck JC, Windisch W, Tonia T, Boyd J, Sotgiu G, Scala R. ERS clinical practice guidelines: high-flow nasal cannula in acute respiratory failure. Eur Respir J. 2022;59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 170] [Article Influence: 42.5] [Reference Citation Analysis (0)] |
| 15. | Delorme M, Bouchard PA, Simon M, Simard S, Lellouche F. Effects of High-Flow Nasal Cannula on the Work of Breathing in Patients Recovering From Acute Respiratory Failure. Crit Care Med. 2017;45:1981-1988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 97] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 16. | Wang G, Wang H, Wang Y, Ba C. Therapeutic effects and the influence on serum inflammatory factors of high-flow nasal cannula oxygen therapy in senior patients with lower respiratory tract infections. Technol Health Care. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |