Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6580
Peer-review started: December 24, 2021
First decision: February 8, 2022
Revised: February 12, 2022
Accepted: May 13, 2022
Article in press: May 13, 2022
Published online: July 6, 2022
Processing time: 181 Days and 19.2 Hours
Klinefelter syndrome (KS) is a genetic disease of male sex chromosome malformations that affects sperm production and reduces testosterone production. It has been reported that there is currently more than 10 cases of KS combined with antiphospholipid syndrome.
Here, we describe a 31-year-old male patient with chromosome 47, XXY type, who suffered deep vein thrombosis of the lower limbs accompanied by abnormal antiphospholipid antibody, lupus anticoagulant and factor VIII. After treatment with immunoadsorption therapy, glucocorticoids, cyclophosphamide, intra
Immunoadsorption combined with glucocorticoid and cyclophosphamide shock comprehensive treatment has achieved significant results for patients with KS combined with antiphospholipid syndrome.
Core Tip: We describe a 31-year-old male patient with chromosome 47 XXY type who suffered from deep vein thrombosis of the lower limbs accompanied by abnormal antiphospholipid antibody, lupus anticoagulant and factor VIII. After treatment with immunoadsorption therapy, glucocorticoids, cyclophosphamide, intravenous immunoglobulin and anticoagulant therapies, the patient showed dramatic symptomatic improvement. During the follow-up, the patient did not develop any new thrombotic events.
- Citation: Song Y, Xiao YZ, Wang C, Du R. Immunoadsorption therapy for Klinefelter syndrome with antiphospholipid syndrome in a patient: A case report. World J Clin Cases 2022; 10(19): 6580-6586
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6580.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6580
Klinefelter syndrome (KS) patients are prone to hypercoagulability states due to sex glucocorticoid disorders in the body. The relationship between KS and thrombosis was first reported in 1993[1]. A follow-up study of 412 male KS patients found that the risk of thrombosis was significantly increased and the prevalence of venous ulcers was 20-50 times higher than the general population[2].
Regarding the case of KS combined with antiphospholipid syndrome (APS), it is currently a diagnosis that is relatively rare in the world. There is a total of about 10 cases reported worldwide and venous thrombosis is seen in the majority. Ayli et al[3] reported a 26-year-old man with KS combined with type 2 diabetes who had severe venous thromboembolism, heterozygous factor V Leiden and prothrombin G20210A mutations. Lapecorella et al[4] presented that severe venous thromboembolism occurred in a young man with KS and heterozygosis for both G20210A prothrombin and factor V Leiden mutations. Recurrent deep vein thrombosis and pulmonary embolism in a 21-year-old man with KS and heterozygous mutation of MTHFR-677C>T and 1298A>C was described by Angel et al[5].
The case we presented in the department of rheumatology was due to recurring deep vein thrombosis in the lower extremities. To our knowledge, it is noteworthy that in our case, for the first time, that immunoadsorption (IAS) combined with glucocorticoid (GCs) and cyclophosphamide (CTX) shock comprehensive treatments has achieved significant results in the patient with KS combined with antiphospholipid syndrome.
It is shown that the patient suffered from a left lower extremity deep vein thrombosis event for 4 years and now presented with a new onset of right lower extremity deep vein thrombosis for the past 10 d.
The patient first developed left lower extremity deep vein thrombosis 4 years ago without obvious incentives. After the thrombus was removed, rivaroxaban 20 mg once a day was started and stopped after half a year. Deep vein thrombosis of the right lower extremity occurred again 10 d ago. Among the clinical symptoms, except for the lower extremity edema caused by venous thrombosis of the right lower extremity, the patient had no rash, Raynaud's phenomenon or other autoimmune disease symptoms when he was admitted to the rheumatology department.
The patient was diagnosed with KS when he was 28-years-old and his karyotype was 47 XXY; 15 sites of AZFa, AZFb and AZFc showed no deletions detected by Polymerase chain reaction.
The patient was diagnosed as suffering from KS when he was 28-years-old and his karyotype was 47 XXY; 15 sites of AZFa, AZFb and AZFc showed no deletions detected by Polymerase chain reaction. But dramatically, it was discovered at the age of 33 that both the patient and his father were heterozygous mutations in bone morphogenetic protein receptor type-2 (BMPR2).
Obvious edema of the right lower extremity with no obvious abnormality found in the rest of his body according to physical examination.
Serological examination revealed that many abnormalities in rheumatic immunological indicators were manifested in the obvious increase of anticardiolipin antibodies, lupus anticoagulants and FVIII: C%, and the autoimmune antibodies (antinuclear antibodies was nuclear homogeneous Type 1: 320, anti-SS-A antibody, anti-dsDNA antibody, anti-nucleosome, anti-histone).
The glucocorticoids level examination showed the following three aspects respectively: (1) The first is the increase of luteinizing glucocorticoid, follicle stimulating glucocorticoid and pituitary prolactin; (2) The second is the decrease of corticotropin and dehydroepiandrosterone levels; and (3) The final aspect indicates that the progesterone, estradiol, testosterone, human growth glucocorticoid and pancreatic islet function were all normal.
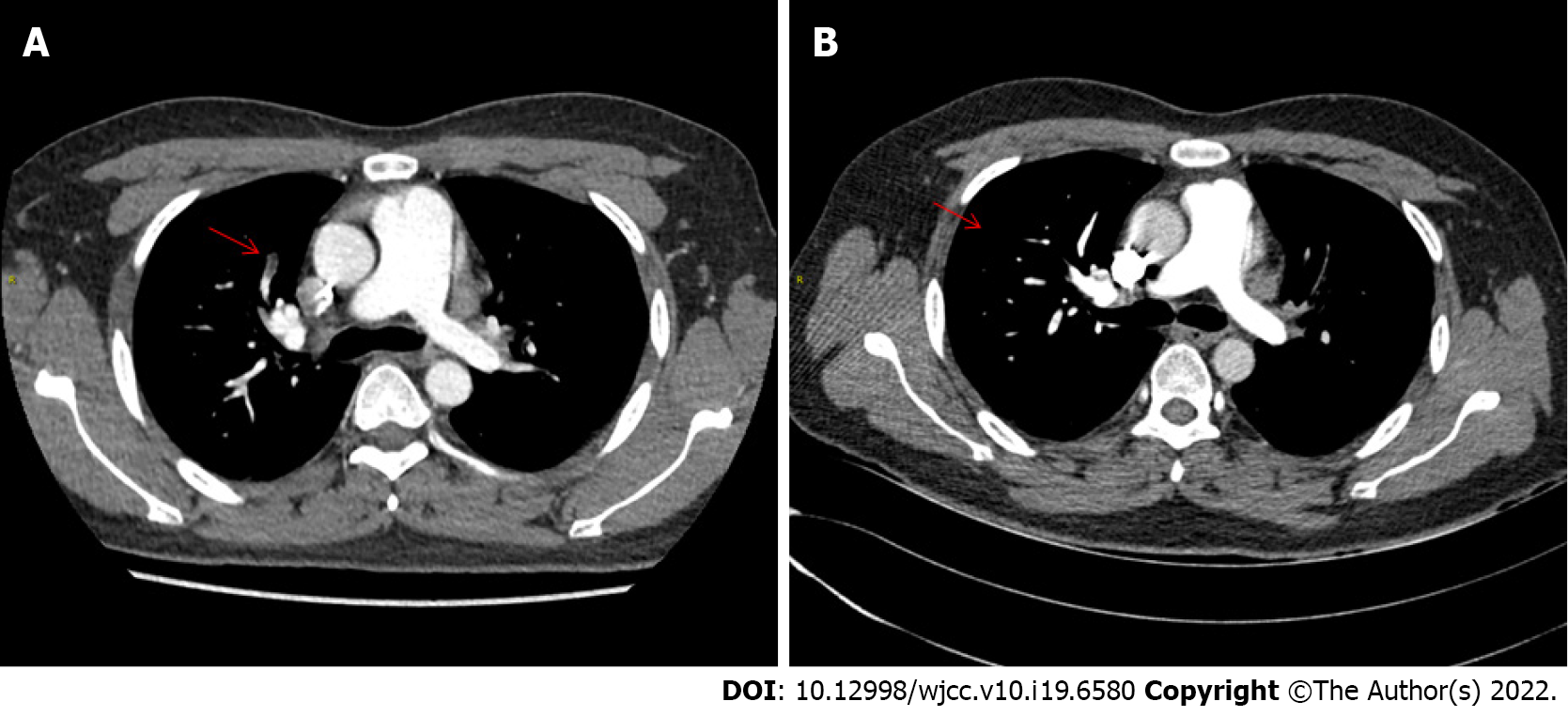
During the imaging examination, the patient had multiple arteriovenous thrombosis throughout the body, the most typical of which was pulmonary embolism, as shown in Figure 1A.
Due to the patient's recurrent thrombotic events and abnormal autoimmune antibodies, he was diagnosed with APS which was initially thought to be caused by abnormalities in coagulation caused by KS.
Given the patient's extremely elevated antiphospholipid antibodies (APL-Ab), coupled with multiple systemic thrombosis, there is a tendency for catastrophic antiphospholipid syndrome. If the antibody titer would not decrease as soon as possible, serious consequences might occur in the short term. Finally, we decided to use blood purification technology to reduce antibody titers quickly in a short period of time. Considering the poor selectivity and greater (large) side effects of ordinary plasma exchange separation technology, we finally chose the IAS.
A month or so after his second venous thromboembolism event (VTE), he accepted the first immunoadsorption therapy (IAS). Fortunately, the original pulmonary embolism miraculously disappeared (Figure 1B).
It is worth noting that after the first use of IAS, he experienced a significant drop in platelets. At this time, we urgently suspended IAS and added sufficient glucocorticoids (GCs) and intravenous immunoglobulin (IVIG) therapy. His platelets quickly returned to normal.
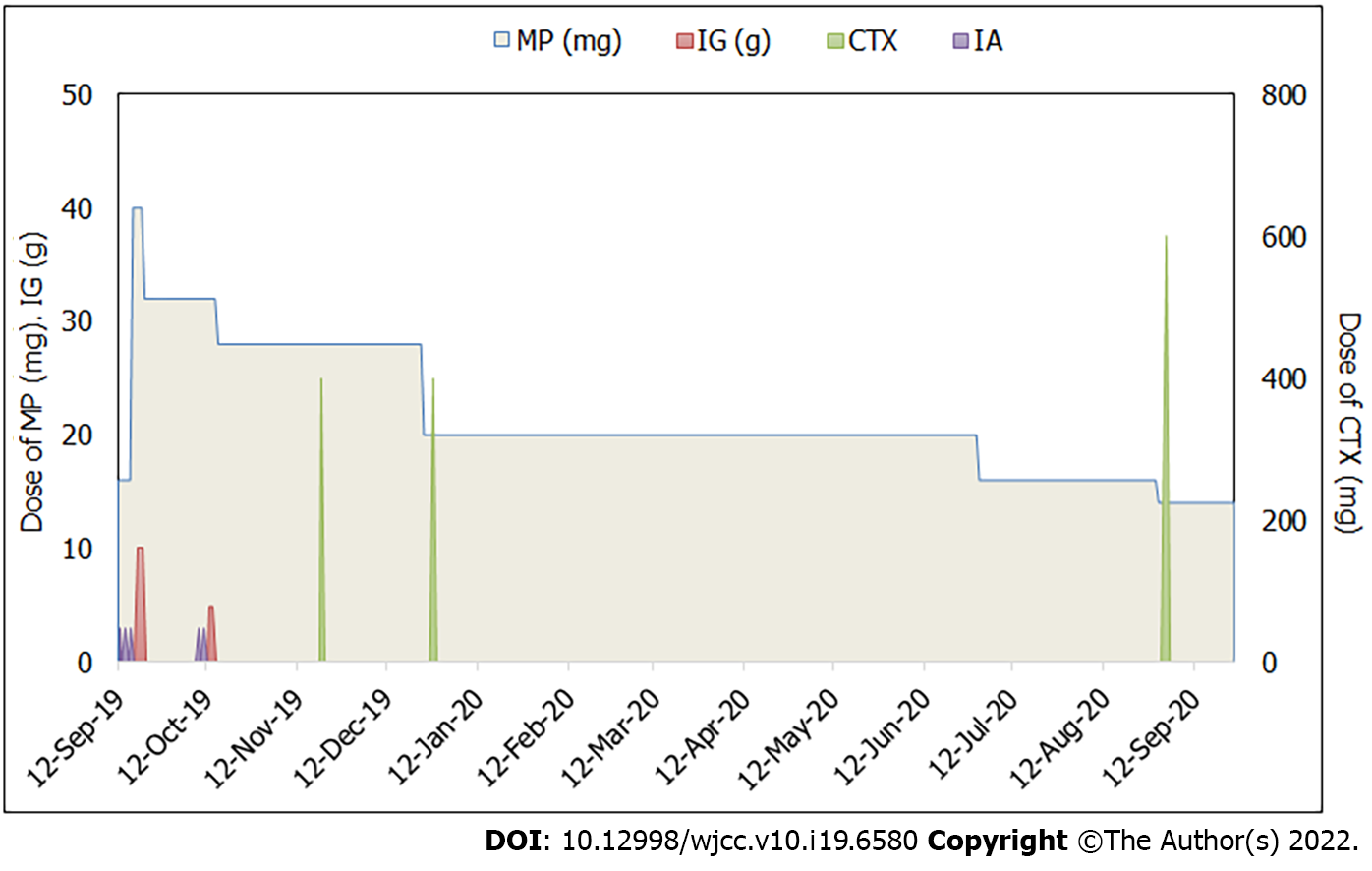
Anticoagulant therapy was used throughout the entire course of the disease with rivaroxaban 20 mg once a day. The dose of glucocorticoid was gradually adjusted according to his condition from 40 mg once a day to the current 14 mg/d. Cyclophosphamide pulse therapy(CTX) was given four times during the 1-year follow-up. The treatment plan is shown in Figure 2.
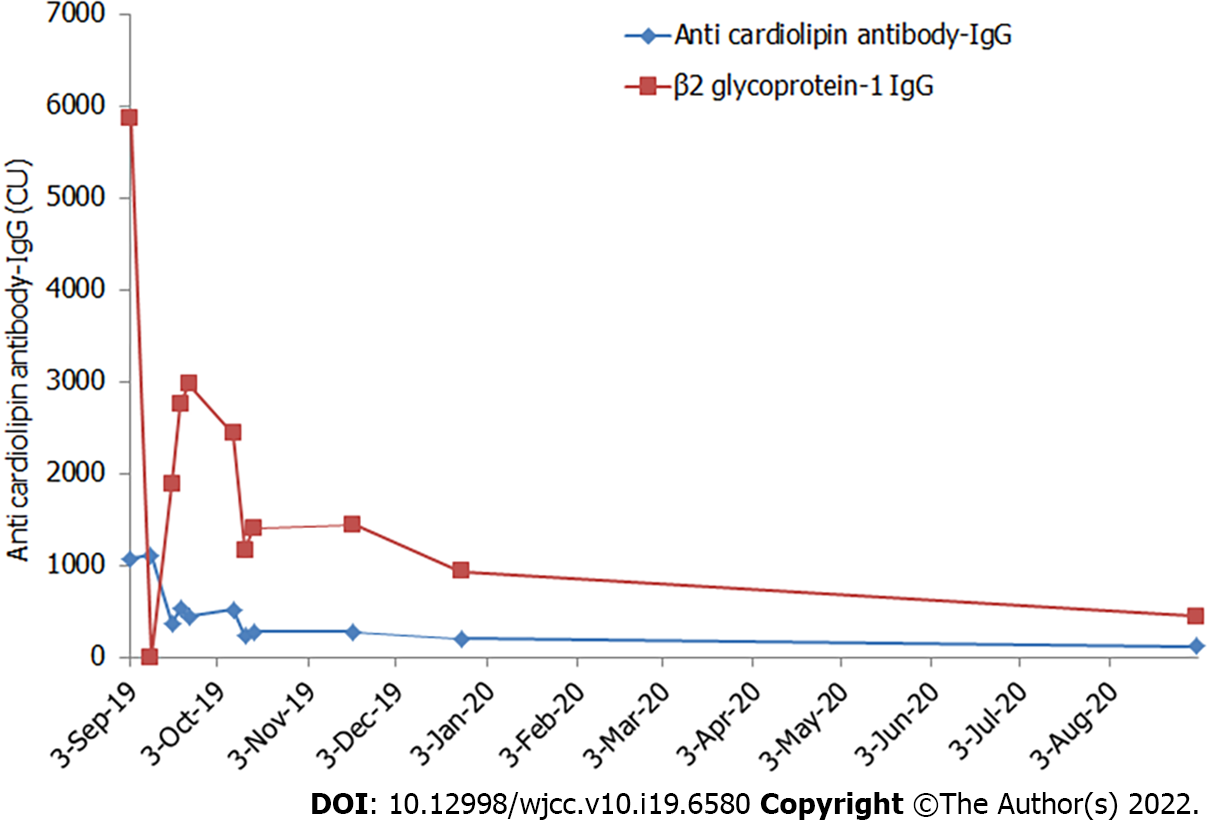
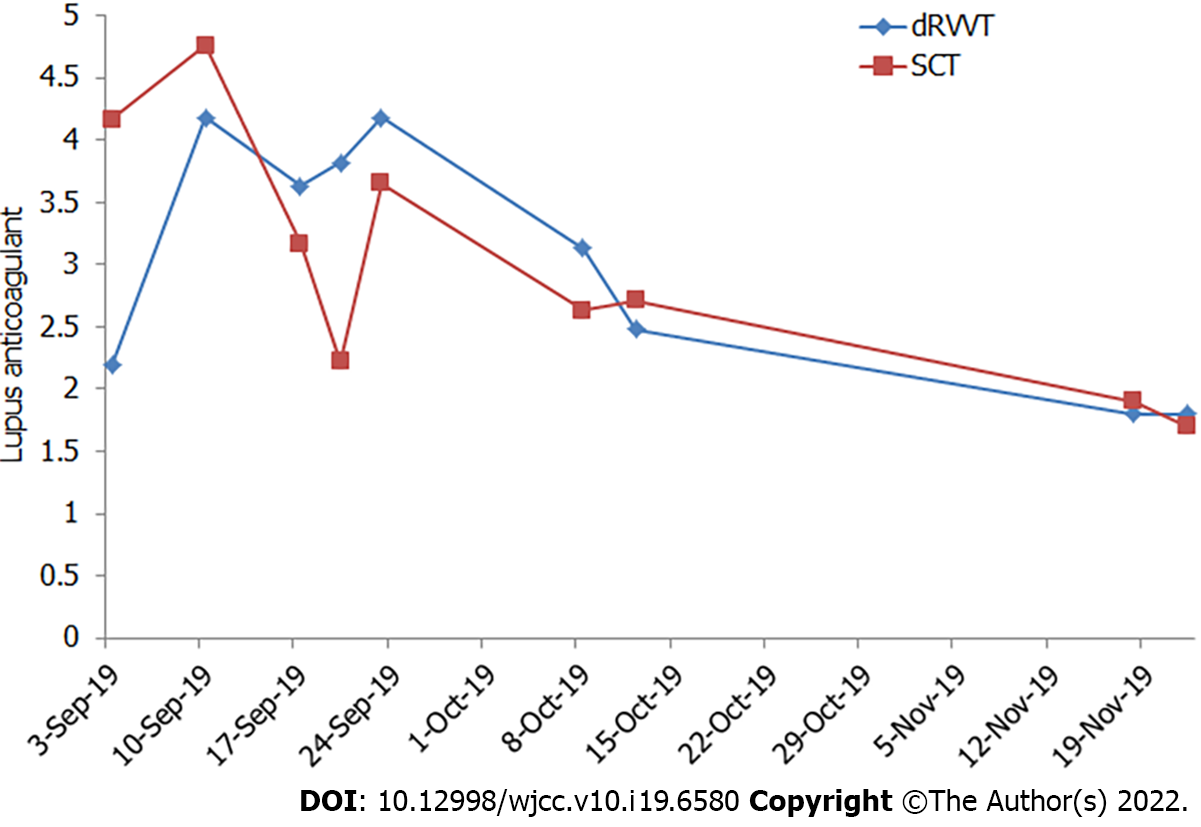
After comprehensive treatment with IAS, GCs, CTX injection and IVIG once, his condition significantly improved. During the 1-year follow-up, no more thrombotic events recurred for him. In addition, the APL-IgG titer and lupus anticoagulant showed a significant decline during the follow-up of the past year. Performance in his cardiolipin antibody-IgG titer dropped from 1071.4CU to 116.7CU and beta2 glycoprotein antibody 1-IgG titer had been in decline from 5870.7 CU to 444.6 CU. Diluted russell viper venom time (dRVVT) screening/confirmation in lupus anticoagulant (LAC) decreased from 2.19 to 1.8, sickle cell trait screening/confirmation (Figure 3), reduced from 4.17 to 1.7 (Figure 4).
There is no direct evidence that can prove the relationship between KS and APS. Some hypotheses explained why KS patients were prone to hypercoagulability. The levels of testosterone in patients with KS are decreased, while the low testosterone levels increase the synthesis of plasminogen activator inhibitor-1 (PAI-1). Elevated levels of PAI-1 can inhibit the activity of tissue-type plasminogen activator (t-PA), prevent the degradation of plasminogen into plasmin and even induce thrombosis[6]. There was also a hypothesis that the higher ratio of β-thrombin in patients with KS is part of the reason of underlying hypercoagulable states of KS[7]. In recent years, some scholars stated that the increase of Factor Ⅷ (FVIII) and high platelet aggregation will increase the risk of individual thromboembolism[8]. In this case, the apparent increase in his FVIII: C% serological level also supports this conjecture.
The patient has a family history of BMPR2 mutations, so it can explain the syndrome of pulmonary embolism, but it is not clear whether BMPR2 mutations will affect the formation of multiple thrombosis throughout the body.
During the 1-year follow-up, the patient did not re-appear with deep vein thrombosis in the lower extremities. Currently, IAS has not been used for 10 mo, and his overall condition has stabilized. Combined with previous case analysis, the first thrombotic event in this type of patient usually occurs earlier, mostly between 20-years-old to 30-years-old and patients often had multiple thrombotic events repeatedly. It is particularly important to assess their coagulation function in their lifetime. The focus of treatment in such patients is to reduce thrombotic events and the anticoagulation therapy has become very important. In the past reported cases from around the world, intravenous or oral anticoagulants were widely used. Our patient did not take anticoagulants regularly after the first thrombosis event and we believe that is the reason why deep vein thrombosis of the lower extremities occurred to him again after 3 years. Therefore, we recommend that he should take anticoagulants for a long time or even for life. Oral anticoagulants should be started when the first thromboembolic event occurs. The duration of anticoagulant therapy should be determined according to the individual conditions. If thromboembolic events would occur repeatedly during the course of the disease or APL-Ab would be significantly increased, short-term IAS combined with GCs therapy could be used under close monitoring.
Due to recurrent deep venous thrombosis in our patient and much higher titers of anticardiolipin antibodies and lupus anticoagulant, the imaging examination revealed that his body was covered with multiple arteriovenous thrombosis which belongs to the acute stage of the disease. In order to avoid recurrence of thrombotic events, we considered using blood purification technology to rapidly reduce antibody titers over a short period of time. Considering the poor selectivity and huge side effects of ordinary plasma exchange separation technology, we selected IAS. This is the first internationally known case to use IAS and it has shown to have a great effect.
According to the observation of the timing and dosage of GCs usage in Klinefelter, unfortunately the syndrome is still unclear so we decided to use methylprednisolone on a trial basis considering the patients high autoantibody titers at the initial diagnosis. Then we gradually adjusted the dosage of methylprednisolone on the basis of the antibody titer. During the GCs reduction period, in order to avoid recurrence, short-term supplementary CTX impulse therapy was applied.
In addition, testosterone replacement therapy (TRT) is also another treatment method used purposefully for patients with KS combined with autoimmune diseases whose androgen levels are reduced and gonadotropins are raised[9]. In the long-term follow-up process, we found that their autoantibody has a certain downward trend[10]. However, the result showed that it does not reduce the incidence of venous thrombosis and thrombotic mortality in patients with KS. The extent to which androgen levels declined in the patients we described was not significant therefore TRT is not recommended.
We will continue to track the patient’s prognosis and evaluate the long-term effectiveness of these treatment programs. Although this is a rare case, we have clarified the exact efficacy of IAS combined with glucocorticoids and immunosuppressants on patients with KS and APS. Although this patient is only an occasional case, and our treatment experience is limited, the purpose of our reported case is that we hope to provide this successful experience and provide a basis for earlier identification of the same types of patients in the future.
We would like to appreciate our patient for consenting to have his case presented and published.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Rheumatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Tanaka H, Japan; Wang CR, Taiwan S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Durand JM, Quiles N, Kaplanski G, Soubeyrand J. Lupus anticoagulant and Klinefelter's syndrome. J Rheumatol. 1993;20:920-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Campbell WA, Price WH. Venous thromboembolic disease in Klinefelter's syndrome. Clin Genet. 1981;19:275-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 60] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Ayli M, Ertek S. Serious venous thromboembolism, heterozygous factor V Leiden and prothrombin G20210A mutations in a patient with Klinefelter syndrome and type 2 diabetes. Intern Med. 2009;48:1681-1685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Lapecorella M, Marino R, De Pergola G, Scaraggi FA, Speciale V, De Mitrio V. Severe venous thromboembolism in a young man with Klinefelter's syndrome and heterozygosis for both G20210A prothrombin and factor V Leiden mutations. Blood Coagul Fibrinolysis. 2003;14:95-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Angel JR, Parker S, Sells RE, Atallah E. Recurrent deep vein thrombosis and pulmonary embolism in a young man with Klinefelter's syndrome and heterozygous mutation of MTHFR-677C>T and 1298A>C. Blood Coagul Fibrinolysis. 2010;21:372-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Seth A, Rajpal S, Penn RL. Klinefelter's syndrome and venous thrombosis. Am J Med Sci. 2013;346:164-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Wautrecht JC, Vincent G, Dereume JP. [Venous thromboembolic disease and Klinefelter's syndrome]. J Mal Vasc. 1986;11:125-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Dissemond J, Knab J, Lehnen M, Goos M. Increased activity of factor VIII coagulant associated with venous ulcer in a patient with Klinefelter's syndrome. J Eur Acad Dermatol Venereol. 2005;19:240-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Olsen NJ, Kovacs WJ. Case report: testosterone treatment of systemic lupus erythematosus in a patient with Klinefelter's syndrome. Am J Med Sci. 1995;310:158-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 40] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Kasten R, Pfirrmann G, Voigtländer V. [Klinefelter's syndrome associated with mixed connective tissue disease (Sharp's syndrome) and thrombophilia with postthrombotic syndrome]. J Dtsch Dermatol Ges. 2005;3:623-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |