Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5406
Peer-review started: September 16, 2021
First decision: December 17, 2021
Revised: February 9, 2022
Accepted: April 2, 2022
Article in press: April 2, 2022
Published online: June 6, 2022
Processing time: 258 Days and 21.4 Hours
Glomangiomatosis (also known as diffuse glomus tumor) is extremely rare, accounting for only 5% of glomus tumors. The prevalence of glomus tumors is only 2% of soft tissue tumors. Lesions can recur after resection. Although growth may be diffuse or infiltrating and invasive, definitive identifying standards for malignant glomus tumors are lacking. This article describes a case of glomangiomatosis with many nodular masses in the soft tissues of the right foot and calf. A review of the Chinese and English-language literature is included.
A case of glomangiomatosis in a 55-year-old Chinese woman who presented clinically with many nodular masses in the soft tissues of the right foot and calf. The tumor was examined histologically and immunostaining was performed.
Glomangiomatosis occurs most often in young people, in the distal extremities, but is rare. Multiple nodules are even rarer. Only 15 clinicopathological analyses of glomangiomatosis have been reported in the combined Chinese- and English-language literature. In the present case, microscopically, nested vascular globular cells were observed around the blood vessel wall. Immunohistochemistry revealed diffuse immunoreactivity for smooth muscle actin, vimentin, type IV collagen, and Bcl-2. Caldesmon, CD34, and calponin were weakly, partially, and slightly positive, respectively. There was no recurrence 1 year after resection.
Core Tip: We describe a case of glomangiomatosis with many nodular masses in the soft tissues of the right foot and calf, presented by a 55-year-old woman. Pigmented villous nodular synovitis was observed via imaging. Microscopically, nested vascular globular cells around the blood vessel wall were observed. After resection, there was no recurrence during the 1-year follow-up. Although growth may be diffuse or infiltrating and invasive, glomangiomatosis does not meet the identifying standards for malignant glomus tumors.
- Citation: Wu RC, Gao YH, Sun WW, Zhang XY, Zhang SP. Glomangiomatosis - immunohistochemical study: A case report. World J Clin Cases 2022; 10(16): 5406-5413
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5406.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5406
The 2020 World Health Organization Classification of Tumors of Soft Tissue and Bone[1] (Fourth Edition) defined glomus tumor as a mesenchymal tumor in normal glomus, with cells resembling modified smooth muscle cells. Glomus tumor may be classified as benign, intermediate glomangiomatosis (also known as diffuse glomus tumor), or malignant (ICD-O: 8711/0, ICD-O: 8711/1, and ICD-O: 8711/3, respectively). Glomus tumors account for fewer than 2% of soft tissue tumors, and glomus hemangioma disease makes up 5% of glomus tumors.
Glomangiomatosis is very rare but occurs most often in young people, in the distal extremities. It is multiple, deep, and wide ranging and often causes pain. The lesions can recur after resection. The tumor shows diffuse growth, with an overall structure that is similar to angiomatosis, except that the vessel wall is surrounded by nests of glomus cells[2]. Although it may be diffuse or infiltrative and aggressive, it lacks the standard morphology of malignancy.
A 55-year-old female presented with idiopathic pain in the dorsum of the right foot and lateral leg, for more than 2 mo.
There was no obvious cause for pain on the back of the right foot and the outside of the lower leg for more than 2 mo. When the pain was severe, it affected movement of the affected limb.
The patient had no significant medical history.
The personal and family history did not reveal any problems.
Physical examination revealed pigmentation of about 6 cm × 6 cm on the right foot dorsum, with a clear boundary and pain upon pressure; local pressing pain on the lateral side of the right leg; limited ankle joint activity; good peripheral blood supply; and normal sensation. During surgery, many nodular masses around the ankle joint were observed, and the incision surface of the tumor was brown.
The prothrombin and partial thromboplastin times were slightly low, and D-dimers were normal. The blood biochemistries and urinalysis were normal. The blood analysis, electrocardiogram, chest x-ray, and arterial blood gas were also normal.
Magnetic resonance imaging showed multiple nodules and soft tissue swelling around the right ankle, which was consistent with pigmented villonodular synovitis.
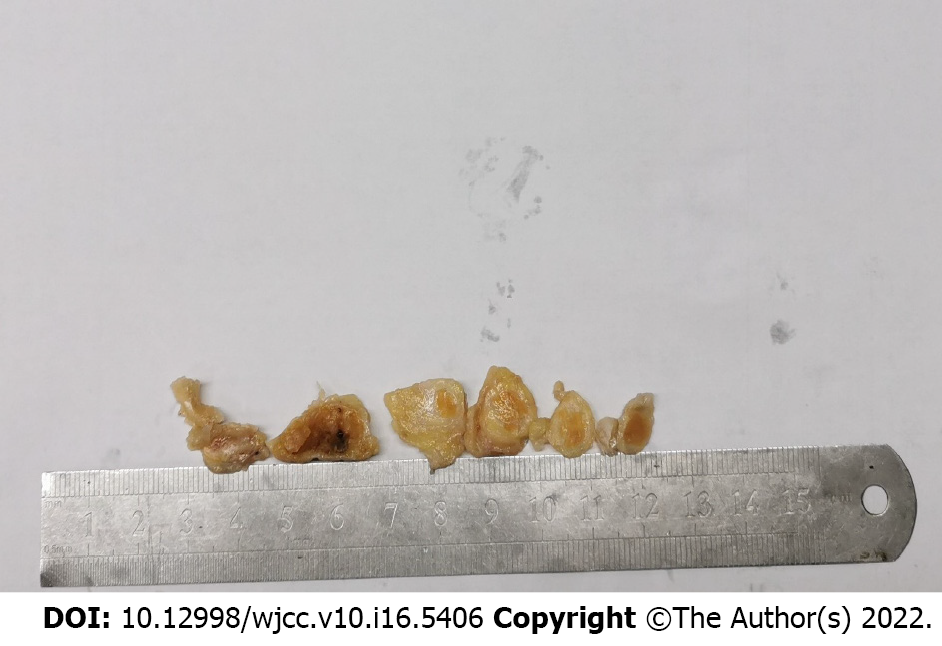
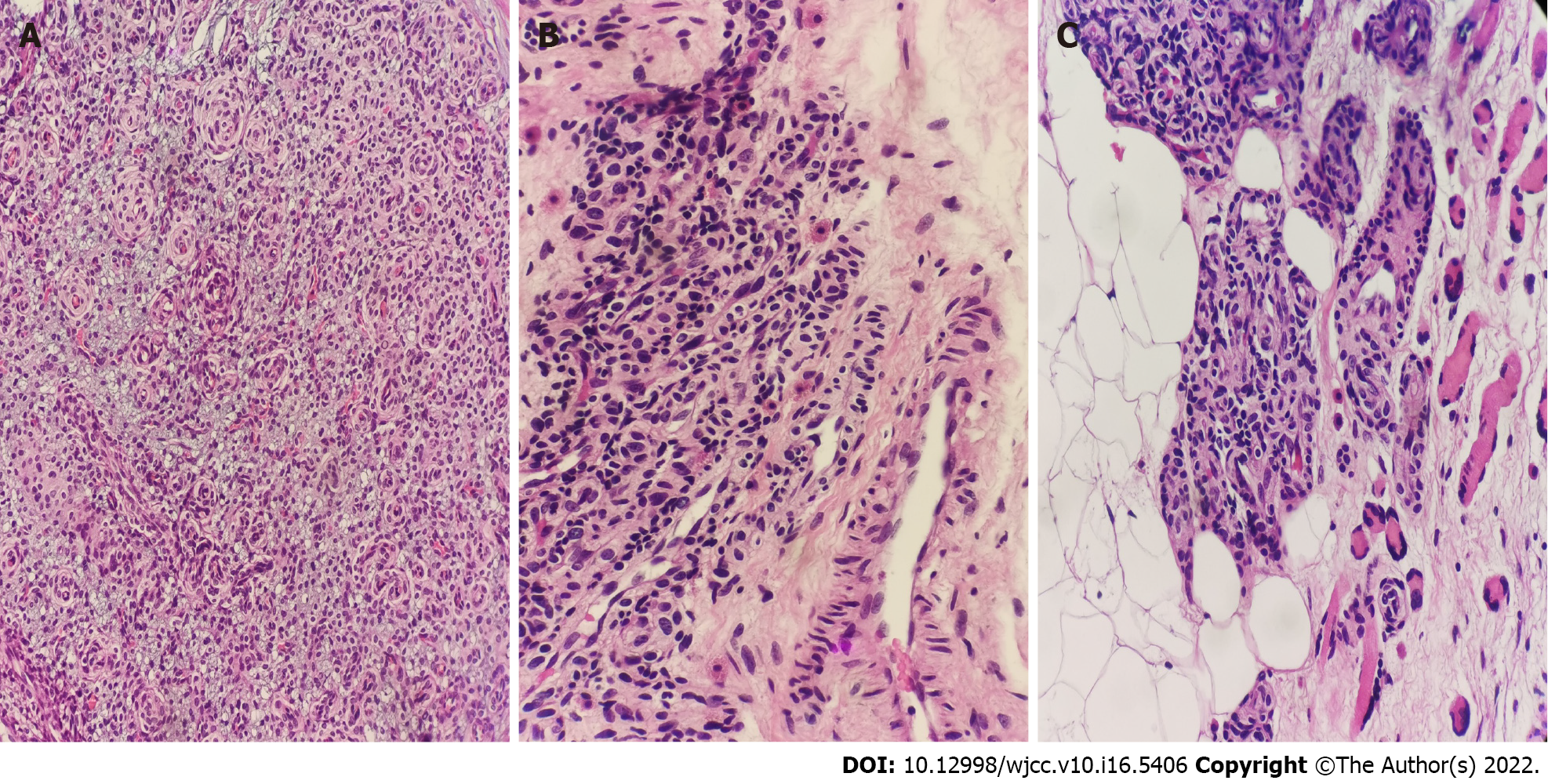
Pathological examination revealed grayish-yellow irregular tissues, with a total volume of 7 cm × 6 cm × 1.5 cm, with multiple nodules within. The largest was 2.5 cm × 1.5 cm × 1.2 cm, and the smallest was 0.8 cm × 0.7 cm × 0.5 cm. The section was grayish-white and grayish-yellow and slightly tough (Figure 1). Under the microscope, the tumor cells in the fibrous connective tissue were nodular and lobulated, and the tumor cells grew around blood vessels. The blood vessels consisted of small arteries and veins, capillaries, and dilated veins showing diffuse hyperplasia (Figure 2A). With eosinophilic staining, the tumor cells appeared round or oval, uniform in size, with abundant cytoplasm and clear boundary. Necrosis and pleomorphism were absent. In the surrounding adipose tissue, a proliferation of oval cells adjacent to small vessels was observed, which was consistent with tumor cell morphology (Figure 2B). Mast cells were scattered in the stroma (Figure 2C).
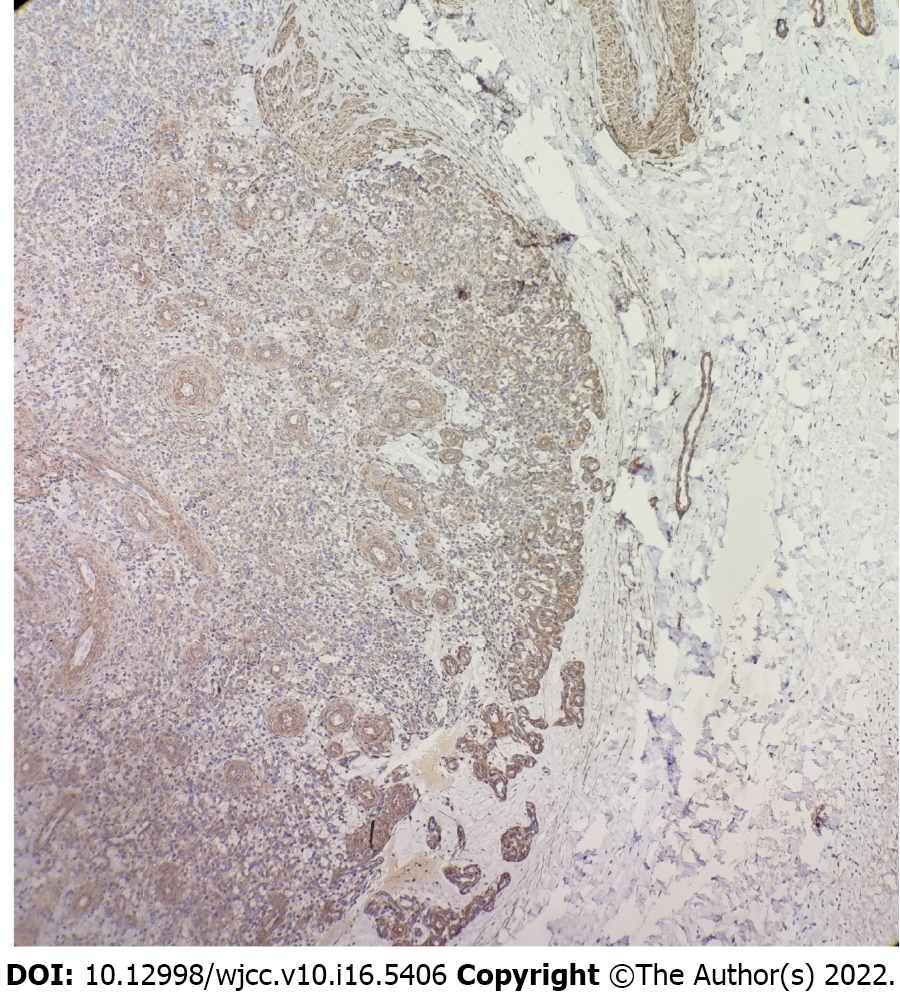
Immunohistochemistry revealed diffuse immunoreactivity for smooth muscle actin (SMA, Figure 3), vimentin, type IV collagen, and Bcl-2. Caldesmon was weakly positive, CD34 was partially positive, and calponin was slightly positive. The Ki-67 value-added index was about 3%. Desmin, S-100, and HMB-45 were negative.
The pathological diagnosis was glomangiomatosis of the right ankle joint.
Extended resection of the tumor.
After the extensive resection, no recurrence was found at the 2-year follow-up, and the prognosis was good.
The 2020 World Health Organization Classification of Tumors of Soft Tissue and Bone (Fourth Edition) defined glomus tumor as a mesenchymal tumor in normal glomus, with cells similar to modified smooth muscle cells. Glomus tumor may be classified as benign, intermediate glomangiomatosis (also known as diffuse glomus tumor), or malignant (ICD-O: 8711/0, ICD-O: 8711/1, and ICD-O: 8711/3, respectively). Glomus tumors account for fewer than 2% of soft tissue tumors, and glomus hemangioma disease makes up 5% of glomus tumors[1].
Glomangiomatosis is very rare but occurs most often in young people, in the distal extremities. It is multiple, deep, and wide ranging and often produces pain. The lesions can recur after resection. The tumor shows diffuse growth, with an overall structure that is similar to angiomatosis, except that the vessel wall is surrounded by nests of glomus cells[2]. Although it may be diffuse or infiltrative and aggressive, it lacks the standard morphology of malignancy.
Due to its rarity, only 15 clinicopathological analyses have been reported in the Chinese and English literature (Tables 1 and 2)[2-16]. In total, there have been 16 patients, of which 5 and 11 were women and men, respectively. The average and median ages were 32 years and 31.5 years. Eleven and 3 cases (68.75% and 18.75%) involved the lower and upper limbs. Other sites (25%) included the head and neck, chest wall, and paravertebral region. Unlike classic glomus tumor, none of these tumors were found under the nail but mostly in the hand, wrist, and foot, and the location was deep. The sizes of the lesions ranged from 1.5 to 22 cm. Therefore, glomangiomatosis is larger than glomus tumor, with extensive lesions and deep location, and all cases were infiltrative. In the present case, lesions were on the back of the right foot and the outer side of the calf and ranged from 0.8 to 2.5 cm in diameter. The deep location and clinical and imaging considerations led to a diagnosis of pigmented villous nodular synovitis.
| Ref. | Age (yr)/sex | Clinical symptoms | Site | Size1 | Depth of tumor |
| Fan et al[9] | 33, M | Pain in the R ankle recurred for 2 yr and aggravated for 1 wk | Medial part of the lower leg and 2 medial malleolus of the R foot | 1.5 × 1.2 × 1; 2 × 1.5 × 1, 1.8 × 1.2 × 1 | Invaded the surrounding striated muscle and adipose tissue |
| Fitzhugh et al[10] | 33, M | Multiple leg pain; lumps present at birth; neurofibromatosis considered in imaging | R leg and joint, 2 | 5; 1.5 | Infiltrative growth with adipose tissue |
| Folpe et al[4] | 25, F | Unknown | Ankle | — | Deep soft tissue |
| Gould et al[11] | 17, F | Palpable mass | Hand and palm | 2-4 mm | Skeletal muscle |
| 29, M | Tumor | Right parotid gland | 4 × 2 × 1.8 | Skeletal muscle | |
| Hayes et al[12] | 32, F | Slow growing mass | Nasal region | — | Deep soft tissue |
| Jalali et al[2] | 17, M | Pain; enlargement | Forearm, hand, and finger tips | — | |
| Kim et al[5] | 48, M | Two masses in the R plantar and R ankle, intermittent pain; history of trauma | R plantar and R ankle 2 | 2; 1 × 1.5 × 1.7; 0.9 × 1.4 × 1.7 | Invasion of surrounding soft tissue |
| Kumar et al[6] | 14, M | L leg cramp for 4 y | Closely related to the sciatic nerve | 6.7 × 4.3 × 3 | Infiltrative growth |
| Laughlin et al[7] | 56, M | Sudden pain in the R foot, aggravating symptoms, extended to the foot and ankle for 3 mo | Sural nerve, 7-cm long distended area | 7 | Infiltrating nerve |
| Lumley et al[13] | 24, F | Pain | R foot; leg | Unknown | Deep in Achilles tendon |
| Negri et al[14] | 21, F | Pain | L thigh | 22 × 11 × 6 | Skeletal muscle |
| Rao et al[15] | 36, M | Unknown | Chest wall > 3 | Skeletal muscles and ribs | |
| Sano et al[8] | 59, M | Multiple glomus tumor of R ankle | R ankle, 5 | 5; 1 × 1 × 1 to 8 × 3 × 2 | Unknown |
| Skelton et al[16] | 32, M | Slow growing painful nodule | R wrist | Deep skin | |
| Zhou et al[3] | 39, M | 20 yr chronic low back pain, 10 yr severe pain | Paraspinal region | 5 × 4 × 3.3 | Deep |
| Ref. | Preop course1 | Treatment | Margin2 | Outcome | FU |
| Fan et al[9] | 2 yr | Resection | Positive | Patients FU for 4 mo | 4 mo |
| Fitzhugh et al[10] | 5 yr | Resection | Unknown | No recurrence 5 yr after resection | 5 yr |
| Folpe et al[4] | NS | Excision | Positive | Recurrence 3 × in 5 yr | 60 mo |
| Unknown | Excision | Negative | No recurrence | 48 mo | |
| Gould et al[11] | 1 yr | Resection | Unknown | No recurrence | 24 mo |
| 2 yr | Incomplete resection | Positive | Recurrence 4 yr later and resected | 48 mo | |
| Hayes et al[12] | 4 mo | Complete resection, each | Positive | Six relapses in 14 yr | 180 mo |
| Jalali et al[2] | 7 mo | Second resection | NS | Small recurrence within 26 mo | 26 mo |
| Kim et al[5] | Trauma; no family history | Resection | Unknown | Unknown | Unknown |
| Kumar et al[6] | 4 yr | Palliative resection | Positive | After 16 mo, the tumor became larger and new nodules appeared | 7 mo3 |
| Laughlin et al[7] | 3 mo | Resection | Unknown | Unknown | Unknown |
| Lumley et al[13] | 4 yr | Incomplete resection, amputation | Positive | One 1 yr later the pain continued; 42 mo later, the knee was excised | 56 mo |
| Negri et al[14] | > 2 yr | Resection/extensive resection of cutting edge | Negative | Unknown | Unknown |
| Rao et al[15] | Unknown | Resection | Unknown | Recurrence 6 yr later | 72 mo |
| Sano et al[8] | 30 yr | Resection | Unknown | No recurrence | 2 yr |
| Skelton et al[16] | 1 mo | Complete resection | Negative | No recurrence | 12 mo |
| Zhou et al[3] | 20 yr | Incomplete resection | Positive | Survival with disease | 15 mo |
Unlike classic glomus tumor, there have been no reports of symptoms related to glomangiomatosis in childhood, although the possibility cannot be ruled out. If perhaps it is present in childhood, symptoms do not develop until early adulthood. Pain is an obvious symptom of the disease[3,4].
Histologically, the overall structure of glomangiomatosis resembles diffuse angiomatosis, except that in the former, glomus cells surround blood vessels. Among the 16 reported cases, all showed a diffuse and infiltrative growth pattern. Skeletal muscle infiltration was observed in 5 cases, and extensive nerve and peripheral invasion was seen in 1 case. However, some authors suggest that the glomus cells and angiomatosis components in glomus hemangioma, often accompanied by adipose tissue, are a sign of mesenchymal proliferation and not simple glomus cell proliferation[3,10]. Further study is necessary to determine whether adipose is one of its components or whether it infiltrates into the adipose tissue.
Fan et al[9] reported a case of glomus angiomatosis in a 33-year-old man who showed multiple glomus angiomatosis on the medial right foot and right lower leg. The patient developed repeated pain in the right ankle during 2 years, worsening in the week before presentation. Immunohistochemistry was positive for SMA and negative for CD34. Fitzhugh et al[10] reported a 33-year-old man with a mass on the distal right calf. Immunohistochemistry showed that the tumor cells were diffusely and strongly positive for SMA, and the vascular components were strongly positive for CD31 and CD34. In the current case, the tumor cells are diffusely and strongly positive for SMA, and negative for CD31 and CD34, which is consistent with the immunohistochemical expression of the above cases.
Masson proposed in 1924 that glomus angiomatosis may be caused by the overgrowth of normal globular cells[17]. Glomus tumor is a kind of interstitial tumor composed of variant smooth muscle cells similar to normal blood vessels. Glomus cells are located around the wall of the small bulb arteriovenous anastomosis. They are a variant of smooth muscle cells. Pericytes include vascular glomus cells. Pericytes were first discovered by Rouget in 1873 and further described by Zimmerman in 1923[3]. Most glomus hemangioma clinically manifests as small benign tumors, most often found in the dermis of the hand, especially in the subungual area, and distributed throughout the body. Most globular tumors have occurred at all ages.
Glomangiomatosis is a rare type of glomus tumor. Its overall structure resembles diffuse hemangioma, but the vessel wall surrounds the nest bulb cells. Combined with histological morphology and immunohistochemical staining of SMA and collagen IV, a diagnosis of glomus hemangioma is not difficult. The disease may be differentiated from other suspects by the characteristic features of each. For example, epithelioid angiomyolipoma is composed of blood vessels, smooth muscle, and fat. The tumor cells immunohistochemically show the presence of HMB45 and Melan A[10]. In paraganglioma, the tumor cells are arranged in an organ-like structure, and the stroma is rich in capillaries. Synaptophysin and chromogranin A can be observed in the main cells, while Sertoli cells show S-100 protein but not SMA[1]. The cells in malignant glomus tumor are heteromorphic, and the mitosis is pathological. Angiomatosis is composed of blood vessels of different sizes, but globular angiomatosis is surrounded by spheroid cells around the blood vessel wall, while the former is not surrounded by spheroid cells.
Studies of the molecular genetics of glomangiomatosis mainly focus on multiple familial cases. These studies show an autosomal dominant hereditary disease, caused by an inactivation mutation of the gene that encodes glomulin in the short arm of chromosome 1. It is possible that there is a family history of glomus angiomatosis, because genetic studies have revealed the truncation of the globulin gene on chromosome 1p21-22, and four germline mutations have been found[17]. However, there are also cases reported in which there was no familial genetic predisposition.
The treatment of glomangiomatosis is surgical resection. Although glomangiomatosis grows diffusely, conservative treatment is still advocated[3]. Local recurrence is related to the difficulty of resection. Zhou et al[3] retrospectively analyzed 11 cases of glomus tumors at home and abroad: 3 cases were not completely resected, 5 had positive margins at the first operation, 5 recurred after surgery, and 1 relapsed six times during 14 years. The patient described in the present article was followed for 1 year after resection, and no recurrence was found. Since the tumors in some cases were palliatively removed, glomangiomatosis should be regarded as a persistent disease rather than local recurrence. Therefore, complete resection of the mass is the most important prognostic factor. Due to the small number of known cases, the effect of adjuvant therapy is uncertain.
Glomangiomatosis is very rare but occurs most often in young people, in the distal extremities. Its overall structure resembles diffuse hemangioma, but the vessel wall surrounds the nest bulb cells. Multiple nodules in glomangiomatosis are even rarer. The treatment of glomangiomatosis is surgical resection.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, general and internal
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bredt LC, Brazil S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | The WHO Classification of Tumours of Editorial Board. WHO classification of tumours of soft tissue and bone. 5th ed. Lyon: International Agency for Research on Cancer Press, 2020: 179-181. |
| 2. | Jalali M, Netscher DT, Connelly JH. Glomangiomatosis. Ann Diagn Pathol. 2002;6:326-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Zhou P, Zhang H, Bu H, Yin X, Zhang R, Fu J, Zhang Z, Chen H, Wei B, Liu X. Paravertebral glomangiomatosis. Case report. J Neurosurg. 2009;111:272-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 406] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Kim M, Choi YS, Young KW, Joo JE. A Case of Glomangiomatosis of the Ankle and Foot: Ultrasonographic Appearance Correlated With the Magnetic Resonance Imaging Findings. Ultrasound Q. 2016;32:180-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Kumar R, Vu L, Madewell JE, Herzog CE, Bird JE. Glomangiomatosis of the sciatic nerve: a case report and review of the literature. Skeletal Radiol. 2017;46:807-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 7. | Laughlin RS, Suanprasert N, Dyck PJ, Spinner RJ, Folpe AL. Glomangiomatosis of the sural nerve. J Clin Pathol. 2014;67:190-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Sano K, Hosaka K, Ozeki S. Glomangiomatosis concentrated in the ankle with varied appearances: a case report. J Foot Ankle Surg. 2014;53:468-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Fan S, Liu Y, Lu M, Qi Q. [Multiple glomangiomatosis: report of a case]. Zhonghua Bing Li Xue Za Zhi. 2016;45:53-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Fitzhugh VA, Beebe KS, Wenokor C, Blacksin M. Glomangiomatosis: a case report. Skeletal Radiol. 2017;46:1427-1433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Gould EW, Manivel JC, Albores-Saavedra J, Monforte H. Locally infiltrative glomus tumors and glomangiosarcomas. A clinical, ultrastructural, and immunohistochemical study. Cancer. 1990;65:310-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Hayes MM, Van der Westhuizen N, Holden GP. Aggressive glomus tumor of the nasal region. Report of a case with multiple local recurrences. Arch Pathol Lab Med. 1993;117:649-652. [PubMed] |
| 13. | Lumley JS, Stansfeld AG. Infiltrating glomus tumour of lower limb. Br Med J. 1972;1:484-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Negri G, Schulte M, Mohr W. Glomus tumor with diffuse infiltration of the quadriceps muscle: a case report. Hum Pathol. 1997;28:750-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Rao VK, Weiss SW. Angiomatosis of soft tissue. An analysis of the histologic features and clinical outcome in 51 cases. Am J Surg Pathol. 1992;16:764-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 62] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Skelton HG, Smith KJ. Infiltrative glomus tumor arising from a benign glomus tumor: a distinctive immunohistochemical pattern in the infiltrative component. Am J Dermatopathol. 1999;21:562-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Goldblum JR, Folpe AL, Weiss SW. Perivascular tumors. In Enzinger and Weiss’s Soft Tissue Tumors, 6th Edition. Philadelphia, PA. Elsevier Saunders. 2014749-768. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |