Published online Jun 6, 2022. doi: 10.12998/wjcc.v10.i16.5373
Peer-review started: August 8, 2021
First decision: September 29, 2021
Revised: October 11, 2021
Accepted: April 2, 2022
Article in press: April 2, 2022
Published online: June 6, 2022
Processing time: 297 Days and 18.6 Hours
The accessory bones are common bone variations around the feet and ankles, which usually originate from nonunion of the secondary ossification center adjacent to the main bone mass, and most of them remain asymptomatic. Os subcalcis is an accessory bone at the plantar aspect of the calcaneus, which is located just posterior to the insertion of the plantar fascia. Focal bone formation at the calcaneal plantar pole with heel pain has rarely been reported.
A 55-year-old man presented to our clinic with left plantar heel pain and a progressive swelling for 8 years. X-ray, computer tomography and magnetic resonance imaging showed a large os subcalcison the plantar side of the calcaneus, located at the insertion of the plantar fascia. He underwent surgical excision of the lesion. Microscopically the bony trabeculae were intermingled with fat and covered with cartilage.
This is a rare case with accessory os subcalcis leading to heel pain. It highlights the awareness of os subcalcis and helps avoid future misdiagnosis of heel pain.
Core Tip: We present a case of a 55-year-old male patient who suffered from heel pain. Imaging examination revealed a large accessory bone located on the plantar surface of the calcaneus, slightly behind the insertion point of the plantar fascia. The heel pain was alleviated by the removal of os subcalcis.
- Citation: Saijilafu, Li SY, Yu X, Li ZQ, Yang G, Lv JH, Chen GX, Xu RJ. Heel pain caused by os subcalcis: A case report. World J Clin Cases 2022; 10(16): 5373-5379
- URL: https://www.wjgnet.com/2307-8960/full/v10/i16/5373.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i16.5373
The accessory bones usually originate from nonunion of the secondary ossification center adjacent to the main bone mass[1,2]. They are common bone variations around the feet and ankles and remain mostly asymptomatic[3]. Os subcalcis is an accessory bone at the plantar aspect of the calcaneus, which is located just posterior to the insertion of the plantar fascia[4]. Focal bone formation at the calcaneal plantar pole has rarely been reported. We here report a case of bone formation of the plantar calcaneus in a man.
A 55-year-old man presented to our clinic with left plantar heel pain and a progressive swelling for 8 years.
Eight years previously, he felt pain in his left heel, especially when standing and walking, and a progressive swelling of the heel. Three years ago, he received a local blockage in the left heel, which temporarily relieved his pain. In recent two months, the pain was aggravated and affected his walking. He denied any previous trauma to the left heel.
After the patient was hospitalized, the preoperative examination identified diabetes which the patient was unaware of. Following drug treatment, the patient’s blood sugar has been well controlled.
The patient had unremarkable personal and familial medical history, including psycho-social history.
Physical examination showed that the callosity was approximately 3 cm in diameter, and could be seen at the bottom of the left heel (Figure 1).
His red blood cell count, hemoglobin, white blood cell, white blood cell differential count, platelet, C-reactive protein, erythrocyte sedimentation rate, rheumatoid factor and uric acid test results were within normal limits.
X-ray, computer tomography and magnetic resonance imaging (MRI) showed a large os subcalcison the plantar side of the calcaneus, located at the insertion of the plantar fascia (Figure 2). The accessory bone was in the shape of an inverted pyramid, about 35 mm × 35 mm × 25 mm in size.
The final diagnosis was large os subcalcis on the plantar side of left calcaneus.
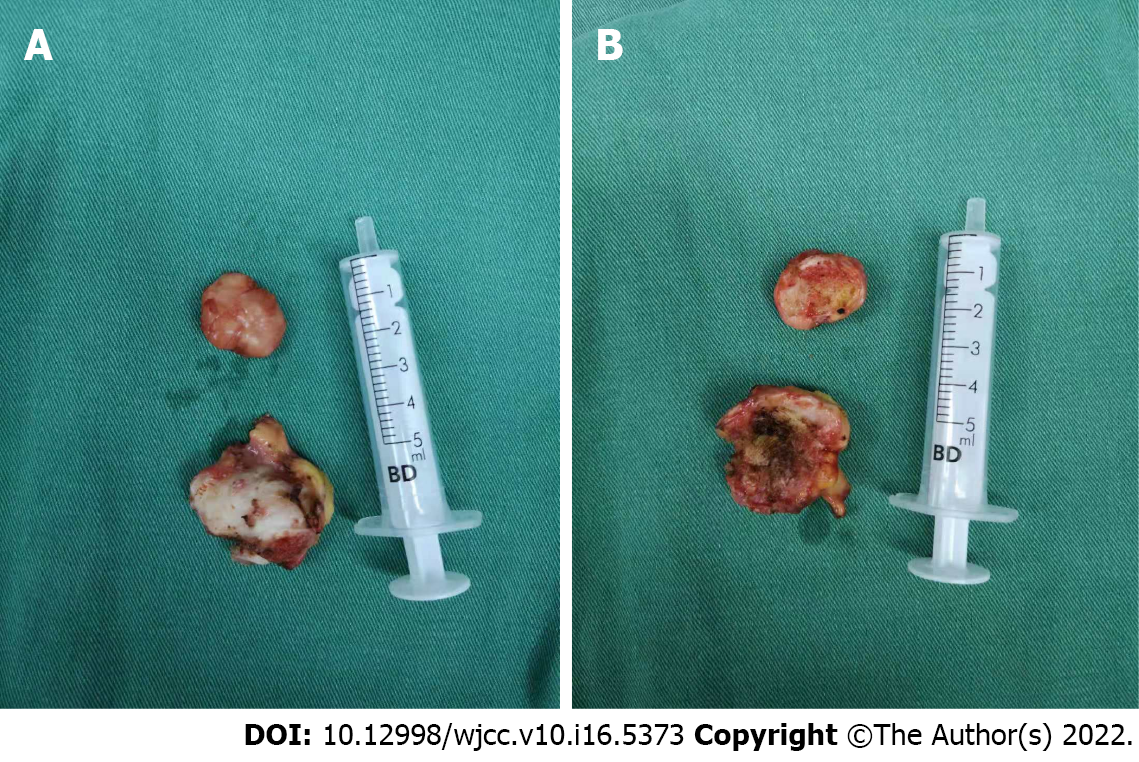
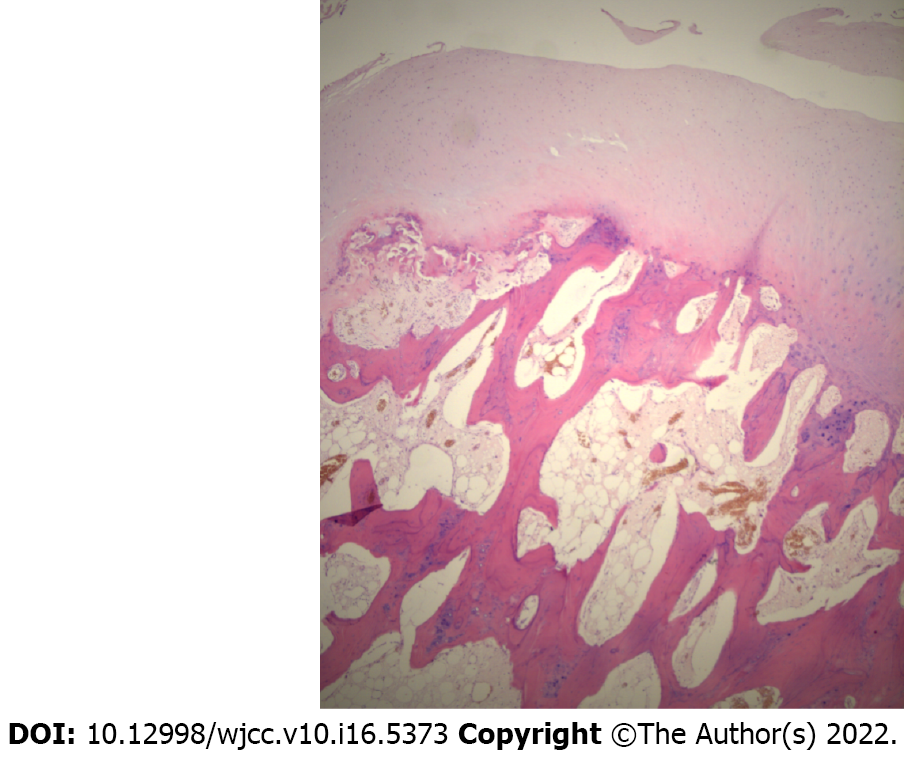
The large os subcalcis was excised under spinal anesthesia in the prone position. The left leg and foot were prepared using Anerdian. The skin and subcutaneous tissue were cut layer by layer through a longitudinal spindle incision on the heel bone surface. At the plantar surface of the os subcalcis, a bursa was present. The surrounding fibrous soft tissue was released and the os subcalcis was exposed. Along the surfaces of the neo-arthrosis between the oscalcis and os subcalcis, fibrous tissue and cartilage-like tissues were observed. The os subcalcis and the bursa were completely resected (Figure 3). Following hemostasis, the skin incision was sutured intermittently. The resected os subcalcis was sent for histological examination. Macroscopically, the resected bone was pyramid shaped and measured 35 mm × 35 mm × 25 mm. Microscopically, the bony trabeculae were intermingled with fat and covered with cartilage (Figure 4). Celecoxib was orally administered at 200 mg twice daily after surgery for analgesia.
The radiography at the first postoperative day demonstrated that the os subcalcis was completely resected (Figure 5). No weight-bearing on the heel was allowed until the incision healed. At 3 wk after surgery, the heel pain was relieved, and the patient was able to walk freely.
Plantar heel pain is the most common foot problem, which can be caused by bone, soft tissue, nerve or systemic diseases. Although accurate diagnosis and proper management are important, it is difficult to distinguish the various causes of highly similar symptoms. The bone disorders include calcaneal stress fracture, calcaneal apophysitis, osteomyelitis and inflammatory arthritis. Soft tissue pathology includes fat pad atrophy or contusion, plantar fascia rupture and plantar fasciitis. Neurological factors include the first branch of the lateral plantar nerve, the medial calcaneal branch of the posterior tibial nerve, and S1 radiculopathy, tarsal tunnel syndrome and peripheral neuropathy[5]. There are few reports on plantar heel pain caused by os subcalcis in the literature.
The accessory bones usually originate from nonunion of the secondary ossification center adjacent to the main bone mass. They are common bone variations around the feet and ankles. The percentage of adult feet with accessory bones ranges from 18% to 30%.
Kruse et al[6] investigated more than 1200 foot X-ray films from the DuPont Institute in Wilmington, DE, United States, in order to estimate the incidence of accessory bones around the foot and ankle. Cilli et al[7] performed anteroposterior and lateral plantar X-rays on 464 male patients in Kayseri, Turkey, to analyze the presence, incidence and distribution of accessory bones. Coskun et al[8] investigated 984 foot X-rays from the medical schools of Akdeniz University and Hacettepe University in Turkey to estimate the incidence of accessory bones around the ankle. Longo et al[9] investigated the prevalence of accessory ossicles and sesamoid bones in a population of Italian women with hallux valgus. A total of 505 women aged 26 to 80 years at the time of hallux valgus correction were examined. Udoaka et al[10] conducted a study of 520 radiographs in Nigeria to ascertain the prevalence of sesamoidbones. Koo et al[11]retrospectively reviewed foot images of 213 patients taken at a tertiary hospital in Seoul, Korea. Neither these investigations nor some reviews mentioned os subcalcis[3,12-14].
We found a very few case reports of os subcalcis in the literature. Milliken[4] was the first to describe os subcalcis in the literature. In 1937, a 65-year-old farmer with a small bony structure on the plantar side of the calcaneus was described. The ossicle was removed, and the histological examination demonstrated a spongy bone covered with cartilage, with well-oriented trabecula. Varounis et al[15] reported an 11-year-old female who presented with a bony mass separate from the posterior portion of the calcaneus. Clinically, the os subcalcaneum displayed a syndesmotic attachment to the calcaneus. Husebye et al[16] presented the case of a 72-year-old female with a volume-expanding os subcalcis. Histological examination demonstrated that cartilage covered the surface of os subcalcis with endochondral ossification between the cancellous bone and the cartilage. Combined with the above reports[4,15,16], we believe that the surgical indications of os subcalcis are: (1) progressive enlargement of the heel mass; (2) significant heel pain or walking instability caused by the heel mass; and (3) broken heel skin caused by the heel mass.
Imaging plays a crucial role in the diagnosis of plantar subcalcis. Among imaging tests, MRI can clearly reveal the cartilage covered surface of os subcalcis, trabecular bone structure and the well demarcated and formed cortical findings[17]. MRI helps us in differential diagnosis with heterotopic ossification, ectopic calcification, osteochondroma[18], periosteal osteosarcoma[19]. In addition, ultrasonography performed with high-resolution broadband linear-array probes due to low cost, fast, readily available, and free of ionizing radiation. It is becoming increasingly important in the evaluation of the ligaments around the ankle joint. Ultrasound has an additional role in the first level differential diagnosis of ankle and heel pain as well as in detection of accessory bones[20,21]. The use of a gel stand-off pad can detect otherwise-missed peri- or intra-lesional flow signals on Doppler imaging, increasing the diagnostic role of this technique in differential diagnosis of heel pain[22].
We report a rare case of a patient with accessory os subcalcis leading to heel pain. The accessory os subcalcis was completely excised, and the heel pain disappeared after surgery. This case report may improve the orthopedic awareness of os subcalcis and help avoid future misdiagnosis of heel pain.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Badessi G, Italy; Ghimire R, Nepal; Sabr A, Morocco S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | O'Rourke J, Stone P, Stern M, McGarry J. Accessory bone or unusual congenital anomaly. J Am Podiatr Med Assoc. 1997;87:407-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Vaz A, Trippia CR. Small but troublesome: accessory ossicles with clinical significance. Radiol Bras. 2018;51:248-256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Mellado JM, Ramos A, Salvadó E, Camins A, Danús M, Saurí A. Accessory ossicles and sesamoid bones of the ankle and foot: imaging findings, clinical significance and differential diagnosis. Eur Radiol. 2003;L164. [RCA] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 111] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Milliken RA. Os subcalcis. Am J Surg. 1937;116. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Yi TI, Lee GE, Seo IS, Huh WS, Yoon TH, Kim BR. Clinical characteristics of the causes of plantar heel pain. Ann Rehabil Med. 2011;35:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Kruse RW, Chen J. Accessory bones of the foot: clinical significance. Mil Med. 1995;160:464-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Beytemür O, Öncü M. The age dependent change in the incidence of calcaneal spur. Acta Orthop Traumatol Turc. 2018;52:367-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Coskun N, Yuksel M, Cevener M, Arican RY, Ozdemir H, Bircan O, Sindel T, Ilgi S, Sindel M. Incidence of accessory ossicles and sesamoid bones in the feet: a radiographic study of the Turkish subjects. Surg Radiol Anat. 2009;31:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 89] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 9. | Longo UG, Marinozzi A, Petrillo S, Spiezia F, Maffulli N, Denaro V. Prevalence of accessory ossicles and sesamoid bones in hallux valgus. J Am Podiatr Med Assoc. 2013;103:208-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Udoaka AI, Didia BC. Prevalence and types of accessory ossicles and sesamoid bones of the feet of adult Southern Nigerians. Research Journal of Medical Sciences. 2013;25. [DOI] [Full Text] |
| 11. | Koo BS, Song Y, Lee S, Sung YK, Sung IH, Jun JB. Prevalence and distribution of sesamoid bones and accessory ossicles of the foot as determined by digital tomosynthesis. Clin Anat. 2017;30:1072-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Keles-Celik N, Kose O, Sekerci R, Aytac G, Turan A, Güler F. Accessory Ossicles of the Foot and Ankle: Disorders and a Review of the Literature. Cureus. 2017;9:e1881. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Nwawka OK, Hayashi D, Diaz LE, Goud AR, Arndt WF, 3rd, Roemer FW, Malguria N, Guermazi A. Sesamoids and accessory ossicles of the foot: anatomical variability and related pathology. Insights Imaging. 2013;581. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 14. | Vora BMK, Wong BSS. Common accessory ossicles of the foot: imaging features, pitfalls and associated pathology. Singapore Med J. 2018;59:183-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Varounis G, Pasternack WA. Os subcalcaneum. J Am Podiatr Med Assoc. 1989;79:517-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 16. | Husebye EE, Stødle A, Lund-Iversen M, Hvaal K. Unilateral, Volume-expanding Os Subcalcis: Patient History and Treatment: A Case Report. J Foot Ankle Surg. 2021;60:209-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Lucas P, Kaplan P, Dussault R, Hurwitz S. MRI of the foot and ankle. Curr Probl Diagn Rad. 1997;209. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Jung HG, Carag JA, Park JY, Bae EJ, Lim SD, Kim HS. Osteochondroma of the calcaneus presenting as Haglund's deformity. Foot Ankle Surg. 2011;17:e20-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Singh D, Sen R, Chaudhary S, Tripathy SK. Periosteal osteosarcoma of the calcaneum: a case report. Foot Ankle Spec. 2012;5:121-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Fessell DP, Vanderschueren GM, Jacobson JA, Ceulemans RY, Prasad A, Craig JG, Bouffard JA, Shirazi KK, van Holsbeeck MT. US of the ankle: technique, anatomy, and diagnosis of pathologic conditions. Radiographics. 1998;18:325-340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Sconfienza LM, Orlandi D, Lacelli F, Serafini G, Silvestri E. Dynamic high-resolution US of ankle and midfoot ligaments: normal anatomic structure and imaging technique. Radiographics. 2015;35:164-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 22. | Corvino A, Sandomenico F, Corvino F, Campanino MR, Verde F, Giurazza F, Tafuri D, Catalano O. Utility of a gel stand-off pad in the detection of Doppler signal on focal nodular lesions of the skin. J Ultrasound. 2020;23:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |