Published online May 26, 2022. doi: 10.12998/wjcc.v10.i15.4957
Peer-review started: October 17, 2021
First decision: December 17, 2021
Revised: December 27, 2021
Accepted: April 9, 2022
Article in press: April 9, 2022
Published online: May 26, 2022
Processing time: 219 Days and 4.5 Hours
Osteosarcoma is one of the most common primary malignant bone tumors and is more common in adolescents. The femur is the most common site of osteosar
The case we report was a 15-year-old patient who was admitted to the hospital 15 days after the discovery of a right thigh mass. The diagnosis was osteosarcoma of the right femoral shaft. After completion of neoadjuvant chemotherapy and preoperative preparation, total right femoral resection + artificial total femoral replacement was performed. Then, chemotherapy was continued after surgery. The patient recovered well after treatment, and the function of the affected limb was good. No recurrence, metastasis, prosthesis loosening, dislocation, fracture or other complications were found during 18 years of follow-up. At present, the patient can still work and lives normally. The results of the medium- and long-term follow-up were satisfactory.
Artificial total femur replacement is a feasible limb salvage operation for patients with femoral malignant tumors, and the results of medium- and long-term follow-up are satisfactory.
Core Tip: Artificial total femur replacement is a feasible limb salvage operation for patients with femoral malignant tumors, and the results of medium- and long-term follow-up are satisfactory.
- Citation: Yang YH, Chen JX, Chen QY, Wang Y, Zhou YB, Wang HW, Yuan T, Sun HP, Xie L, Yao ZH, Yang ZZ. Total femur replacement with 18 years of follow-up: A case report. World J Clin Cases 2022; 10(15): 4957-4963
- URL: https://www.wjgnet.com/2307-8960/full/v10/i15/4957.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i15.4957
Osteosarcoma is one of the most common primary malignant bone tumors and is more common in adolescents[1] than in adults. Since the 1970s, with the application of neoadjuvant chemotherapy, the 5-year survival rate of osteosarcoma patients has exceeded 70%[2]. After the 20th century, due to the development of reconstruction materials and surgical techniques, limb salvage has become the mainstream treatment for limb osteosarcoma patients, and 85% of patients in early and middle stages can undergo limb salvage therapy[3]. Osteosarcoma can occur in bones throughout the body, with the femur being the most common site of osteosarcoma, usually in the metaphysis of the femur[4]. However, as the frequency of cases increase, several abnormalities in case presentation stand out; for example, tumors may have jumping lesions at the other end of the femur; malignant tumors in the proximal or distal tumors may have a wide range of invasion, reaching or even exceeding 1/2 of the femur; and backbone malignant tumors involve the proximal and distal femurs. In these cases, only hip amputation or hemipelvic amputation can be performed. In 1965, Buchman et al[5] performed the world's first total femur replacement. The application of artificial total femoral replacement surgery avoids amputation, retains the movement and weight-bearing function of the affected limb, reduces psychological trauma, and greatly improves quality of life[6]. We report a case of artificial total femoral prosthesis replacement for stage IIB osteosarcoma of the femoral shaft and follow-up for 18 years. Combined with relevant literature reports, cases of this type are summarized and analyzed to improve the understanding of this procedure.
Find a mass in the middle and lower part of the right thigh with pain for 15 d.
A 15-year-old male patient was admitted to the hospital on August 5, 2003, after finding a mass in the middle to lower part of the right thigh with pain going back 15 d.
There was no previous history of pain.
There is no history of family inheritance.
Physical examination demonstrated that the patient’s general condition was good, and palpation of systemic superficial lymph node did not reveal swelling. No abnormalities were found in the heart, lungs or abdomen. There was localized swelling to the middle and lower thigh, and a 10 cm × 6 cm × 4 cm mass was found, characterized by hard, fixed, unclear boundaries, tenderness, increasing local skin temperature and filling superficial veins. Left lower limb blood flow and feeling were good, and the muscle strength was grade 4.
Blood routine was normal, ALP 222U/L.
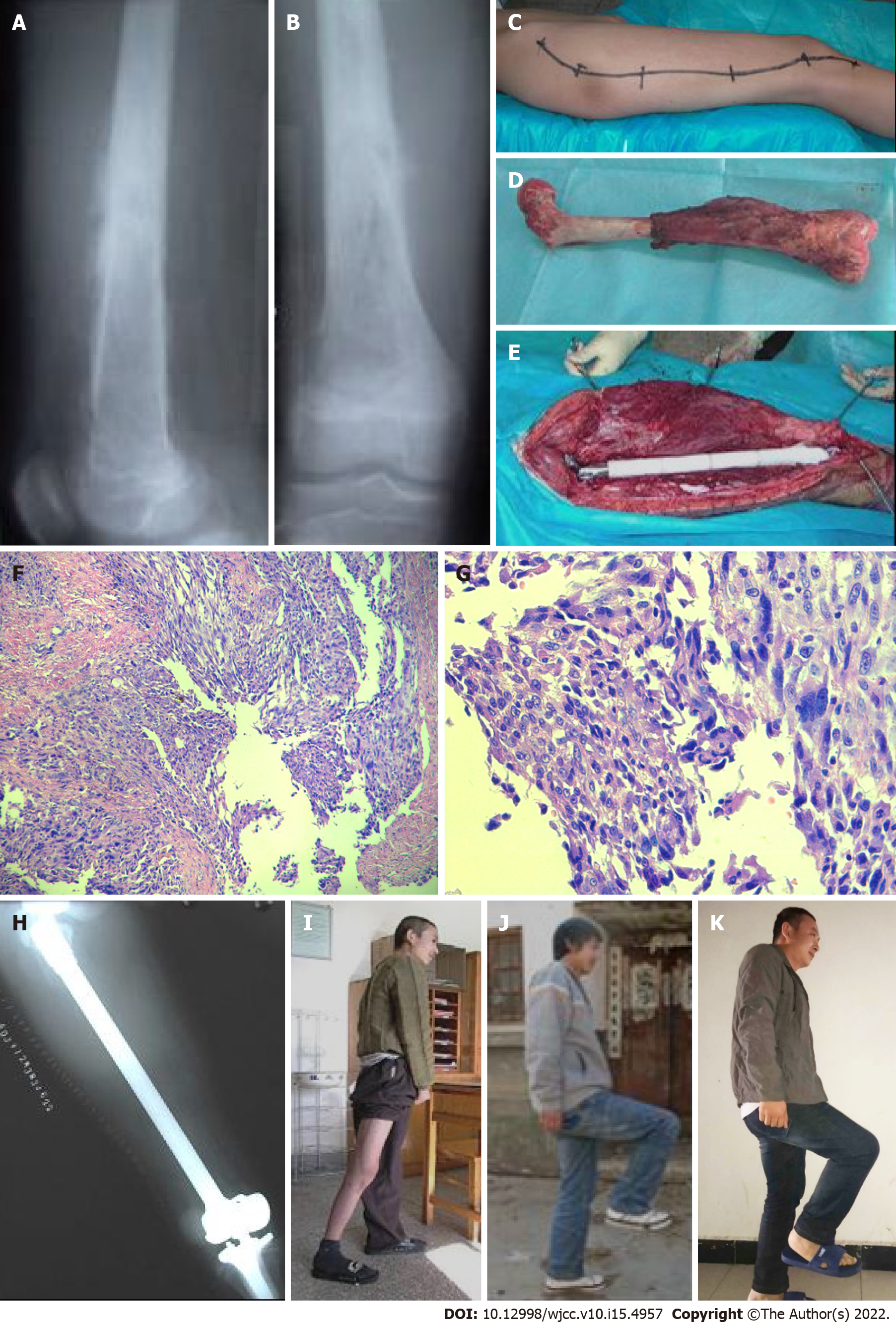
X-ray showed osteolytic destruction of the middle and lower segments of the right femur, accompanied by a periosteal reaction (Figure 1A and B). Enneking staging was IIB.
Conventional osteosarcoma of the right femur (Enneking stage: G2T2M0 Stage IIB).
Biopsy of the mass revealed right femoral osteosarcoma. Adjuvant chemotherapy with doxorubicin, cisplatin, high-dose methotrexate and vincristine was administered on September 1, 2003. Thigh pain was relieved after chemotherapy, and the mass was reduced to 8 cm × 4 cm × 2 cm. Artificial total femoral replacement under general anesthesia (compartment resection of osteosarcoma) was performed on November 20, 2003. The Watson Jones incision of the hip joint was performed during surgery, which then extended to the outside of the knee joint along the outside of the thigh and distal end, starting from 3.5 cm above the tip of the femoral trochanter and ending at the lateral edge of the tibial tubercle (Figure 1C). The whole femur was resected at the surgical margin of the tumor response area (Figure 1D). According to tumor knee arthroplasty standards, the tibial plateau and medullary cavity were repaired, and a bone cement-type artificial tibia prosthesis was partially implanted and fixed in the tibial medullary cavity; attention was given to avoid varus or angulation deformities in the tibial axis. According to the size of the acetabulum, an appropriate double-acting femoral head was selected, and the reduction and rotation axes of the knee joint were installed (Figure 1E). The anteversion angle of the femoral neck was kept at 15-20°. To wash, establish hemostasis and repair the hip joint, large and small rotor stumps were sutured with the iliopsoas, gluteus maximus and gluteus medius to the ear-shaped holes of the artificial femur, the large and small trochanter attachments were reconstructed, the knee joint capsule was repaired, the lateral femoral muscle, tensor fascia lata, and iliotibial tract covering the prosthesis were sutured, and the subcutaneous tissue and skin were sutured. Two negative pressure drainage tubes were placed on the right hip and lateral knee. After the operation, the hip joint strap was fixed externally, the right lower limb was abducted 15-20° in a neutral position, and the patient was given "Ding" shoes to wear in order to prevent lower extremity external rotation. The drainage tube was pulled out 5 d after the operation, and the X-ray revealed that the prosthesis was in good position, with no dislocation (Figure 1H). After 5 d, the right quadriceps, ankle and toe functions were exercised. The postoperative pathological diagnosis was osteosarcoma of the right femur, which was considered conventional according to the WHO classification of bone tumors (Figure 1F-G). The sutures were removed 18 d after the operation, and incision I/a had healed. Chemotherapy was initiated 4 wk after surgery with the same scheme as before.
At the 6th week, the patient began to walk on crutches, kept a neutral position of abduction, and was told not to cross his knees, bend his legs, squat excessively or bend his hip no more than 90°. The patient returned to the hospital for re-examination 1 year (Figure 1I) and 4 years (Figure 1J) after surgery. Presently, the patient was followed up after 18 years (Figure 1K). There was no local tumor recurrence, with no metastasis in either lung. X-ray showed that there were no complications, including loosening, dislocation or fracture of the artificial femur. At present, the patient still works and lives normally.
To review the cases of femoral shaft malignant tumors treated by artificial whole femoral prostheses in China and abroad, we used the following literature search terms: ("total femur replacement" or "total femoral replacement" or "total femur and knee joint replacement" or "total femoral and knee joint replacement" or "total femoral endoprosthetic replacement") and ("malignant bone tumor" or "bone neoplasm" or "bone cancer" or "bone malignant tumor" or "malignant tumor of bone" or "osteosarcoma" or "Ewing sarcoma" or "chondrosarcoma"). Our search encompassed 40 years of cases in Medline and China Zhiwang. Using this strategy, we found a total of 446 cases in 37 studies. The relevant literature reports are summarized in Supplementary Table 1.
Due to existing methods of neoadjuvant chemotherapy combined with complete tumor resection and limb reconstruction have achieved satisfactory clinical results. For patients whose soft tissue conditions are not poor, the main neurovasculature is not invaded, certain limb functions can be preserved after surgery and local recurrence rate will not be increased, limb salvage surgery can be performed[7]. This osteosarcoma case included a wide range of tumor invasion and was easily combined with pathological fractures. Autologous tumor bone replantation has problems, since it is difficult to retain the intact bone shell, and the strength is reduced after inactivation of the tumor bone. Allogeneic bone replacement requires a long healing time, and has a higher propensity for fractures and joint degeneration, while artificial joints have high strength and are specially formulated according to the patient’s clinical needs to fill bone defects and rebuild joint function. Patients can also bear weight and exercise soon after surgery[8]. In this case, the right femoral lesion had exceeded 1/2 the length of the femur. If lengthened knee arthroplasty had been used, the prosthesis could easily loosen due to the large leverage force and the lack of surrounding soft tissue fixation, and the tumor may recur due to the insufficient osteotomy plane. Therefore, artificial total femoral replacement was the best treatment for this case. Our experience was that during the operation, we should protect the normal muscle tissue, firmly reconstruct the attachment points of the large and small rotator muscles, repair the hip and knee joint capsule, and rebuild the muscle balance. After the operation, we should emphasize the correct posture and correct functional exercise, which plays an important role in reducing the incidence of complications and improving the limb function of patients.
Total femoral prosthesis replacement is an ideal method for removing malignant femoral tumors to preserve the limbs and maximize the function of the lower extremities. It is necessary however to pay attention to the surgical indications and case selection to determine if surgical border resection is required during the operation. Currently, the recognized surgical indications for consideration include[9-13]: (1) Malignant tumors originating from the femoral shaft accumulate in the proximal or distal femur; (2) tumors in the proximal or distal femur which have jumping lesions at the other end; (3) patients who can still save their limbs by total femoral replacement to prevent local tumor recurrence; (4) the replacement of the proximal or distal femur prosthesis or composite prosthesis fails, due to the nonunion of bone, fracture or loosening of the prosthesis, which cannot be repaired by other methods; (5) patients with multiple bone metastases on a single limb with pathological fractures who are expected to survive for > 6 mo; or (6) some benign lesions with repeated pathological fractures and long healing time and appear to have limb deformities, which have seriously affected the patient’s work and quality of life. The patient described here meets indication[1]. Due to the expansion of the indications for artificial total femoral replacement, the procedure has been gradually applied to nontumor lesions, including revision of hip and knee joint replacements with serious bone defects and invalid conventional methods or serious hip and knee arthritis on the same limb side, among other conditions.
Since Buchman's first customized cobalt chromium molybdenum alloy femoral prosthesis was applied[5] the design of the whole femoral prosthesis has been improving with the progress of biomaterial technology. Early prostheses were all homemade[14], later developed into custom-made prostheses[9,15-18], and then assembled prostheses[15,16]. At present, patients can use assembled prostheses without waiting for the prosthesis to be manufactured, and they can also be assembled according to their own specific conditions. Metal materials have also evolved from titanium nitride[15] and stainless steel[19] to titanium alloys[20]. The prosthesis used in this patient was a customized titanium alloy prosthesis, and the design was based on the patient's bilateral total femoral X-ray. The length of the customized prosthesis was the same as the healthy leg or slightly shorter by 1-2 cm, and the size of the femoral head was similarly measured. A bipolar artificial femoral head is recommended to reduce the dislocation of the hip joint prosthesis[21]. The use of a rotary axis knee joint can reduce the loosening of the knee prosthesis[22]. In recent years, there have also been many special types of total femoral prostheses developed. Since traditional total femoral replacement requires the removal of many muscle attachment points, the function of the affected limb is poor after surgery, and hip dislocation is more common. Ward et al[10] and Gorter et al[23] have developed a full-femoral intramedullary prosthesis to replace the traditional full-femoral prosthesis. This surgical method retains the attachment points of some bones and muscles, maintains stability to the maximum extent, and yields better function. Additionally, complications of hip dislocation cannot easily occur, and the risk of incision infection is also reduced. To solve the problem of unequal lengths of the lower limbs after total femoral replacement in children, Schindler et al[24] designed an extendable total femoral prosthesis. In response to the problem of deep infection and abscess formation after total femoral replacement, Glehr et al[25] applied a silver ion-coated total femoral prosthesis to reduce the incidence of postoperative infection complications.
There are few reports including long-term follow-up after total femoral replacement surgery, which are mainly based on case reports. The main reason for this is related to the poor effect of postoperative radiotherapy and chemotherapy, the early occurrence of distant metastasis and the short overall survival period. It is generally acknowledged that the first case of total femoral replacement was performed by Professor Buchman in 1965, but actually, the earliest case can be traced back to 1952 and was also performed by Professor Buchman. This case was followed up for 35 years and is also the case with the longest follow-up time reported in the literature. It was reported by Present in 1990[14]. This case was diagnosed as having multiple fibrous dysplasia in the left femur and secondary low-grade chondrosarcoma. Thirty-two years after total femoral replacement, the patient underwent hip arthroplasty due to severe pain in the thigh and sinus formation. Postoperative examination showed that there was no recurrence of the tumor. Nakamura et al[21] reported 2 patients with total femoral replacement surgery, including over 10 years of follow-up. One case was diagnosed as osteosarcoma with skin necrosis that occurred after the operation requiring a skin graft. There was no loosening, dislocation or local recurrence of the prosthesis after 12 years of follow-up. The MSTS score of the postoperative patients was 60%. Another patient was diagnosed with Ewing's sarcoma, and sciatic nerve palsy occurred after surgery, requiring external fixation and crutches. After 11 years of follow-up, no prosthesis loosening, dislocation, or local recurrence was found. The functional MSTS score of the patient after operation was 63%. The patient in this paper was followed up for 18 years. The patient did not experience local tumor recurrence or distant metastasis. The images suggest that the prosthesis has not been loosened, dislocated, or broken. The patient could walk normally on crutches, and the current MSTS score was reported as 67%.
Artificial total femur replacement is a feasible limb salvage operation for patients with femoral malignant tumors, and the results of medium- and long-term follow-up are satisfactory.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hakozaki M, Japan; Limaiem F, Tunisia S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Yang Y, Han L, He Z, Li X, Yang S, Yang J, Zhang Y, Li D, Yang Y, Yang Z. Advances in limb salvage treatment of osteosarcoma. J Bone Oncol. 2018;10:36-40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 2. | Bernthal NM, Federman N, Eilber FR, Nelson SD, Eckardt JJ, Eilber FC, Tap WD. Long-term results (>25 years) of a randomized, prospective clinical trial evaluating chemotherapy in patients with high-grade, operable osteosarcoma. Cancer. 2012;118: 5888-5893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 128] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 3. | Federman N, Bernthal N, Eilber FC, Tap WD. The multidisciplinary management of osteosarcoma. Curr Treat Options Oncol. 2009;10: 82-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 4. | Yao W, Cai Q, Wang J, Gao S. Treatment of osteosarcoma around the knee in skeletally immature patients. Oncol Lett. 2017;14: 5241-5248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Buchman J. Total femur and knee joint replacement with a vitallium endoprosthesis. Bull Hosp Joint Dis. 1965;26: 21-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 6. | Yonemoto T, Kamibeppu K, Ishii T, Iwata S, Hagiwara Y, Tatezaki S. Psychosocial outcomes in long-term survivors of high-grade osteosarcoma: a Japanese single-center experience. Anticancer Res. 2009;29: 4287-4290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Fujiki M, Kimura T, Takushima A. Limb-salvage surgery with vascular reconstruction after lower extremity sarcoma resection: A systematic review and meta-analysis. Microsurgery. 2020;40: 404-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Plötz W, Rechl H, Burgkart R, Messmer C, Schelter R, Hipp E, Gradinger R. Limb salvage with tumor endoprostheses for malignant tumors of the knee. Clin Orthop Relat Res. 2002;207-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 86] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Marcove RC, Lewis MM, Rosen G, Huvos AG. Total femur and total knee replacement. A preliminary report. Clin Orthop Relat Res. 1977;147-152. [PubMed] [DOI] [Full Text] |
| 10. | Ward WG, Dorey F, Eckardt JJ. Total femoral endoprosthetic reconstruction. Clin Orthop Relat Res. 1995;195-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 58] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Guo C, Gan L, Tu ZQ. Total femoral prosthesis replacement in the treatment of recurrent osteosarcoma. Huaxi Yixue Za Zhi. 2003;86-87. [DOI] [Full Text] |
| 12. | Berend KR, Lombardi AV Jr, Mallory TH, Adams JB, Dodds KL. Total femoral arthroplasty for salvage of end-stage prosthetic disease. Clin Orthop Relat Res. 2004;162-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Lombardi AV Jr, Berend KR. The shattered femur: radical solution options. J Arthroplasty. 2006;21: 107-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Present DA, Kuschner SH. Total femur replacement. A case report with 35-year follow-up study. Clin Orthop Relat Res. 1990;166-167. [PubMed] [DOI] [Full Text] |
| 15. | Hu QT, Jiang QW, Su GL, Shen JZ, Shen X. Total femur and adjacent joint replacement with endoprosthesis: report of 2 cases. Chin Med J (Engl). 1980;93: 86-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 72] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Steinbrink K, Engelbrecht E, Fenelon GC. The total femoral prosthesis. A preliminary report. J Bone Joint Surg Br. 1982;64: 305-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Capanna R, Ruggieri P, Biagini R, Gamberini G, Rock M, Campanacci M. Subtotal and total femoral resection: an alternative to total femoral prosthetic replacement. Int Orthop. 1986;10: 121-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Nerubay J, Katznelson A, Tichler T, Rubinstein Z, Morag B, Bubis JJ. Total femoral replacement. Clin Orthop Relat Res. 1988;143-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Natarajan MV, Balasubramanian N, Jayasankar V, Sameer M. Endoprosthetic reconstruction using total femoral custom mega prosthesis in malignant bone tumours. Int Orthop. 2009;33: 1359-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Ahmed AR. Total femur replacement. Arch Orthop Trauma Surg. 2010;130: 171-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 21. | Nakamura S, Kusuzaki K, Murata H, Takeshita H, Hirata M, Hashiguchi S, Hirasawa Y. More than 10 years of follow-up of two patients after total femur replacement for malignant bone tumor. Int Orthop. 2000;24: 176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Sevelda F, Schuh R, Hofstaetter JG, Schinhan M, Windhager R, Funovics PT. Total Femur Replacement After Tumor Resection: Limb Salvage Usually Achieved But Complications and Failures are Common. Clin Orthop Relat Res. 2015;473: 2079-2087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 23. | Gorter J, Ploegmakers JJW, Ten Have BLEF, Schreuder HWB, Jutte PC. The push-through total femoral prosthesis offers a functional alternative to total femoral replacement: a case series. Int Orthop. 2017;41: 2237-2244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Schindler OS, Cannon SR, Briggs TW, Blunn GW, Grimer RJ, Walker PS. Use of extendable total femoral replacements in children with malignant bone tumors. Clin Orthop Relat Res. 1998;157-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 25. | Glehr M, Leithner A, Friesenbichler J, Goessler W, Avian A, Andreou D, Maurer-Ertl W, Windhager R, Tunn PU. Argyria following the use of silver-coated megaprostheses: no association between the development of local argyria and elevated silver levels. Bone Joint J. 2013;95-B: 988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |