Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3060
Peer-review started: December 2, 2021
First decision: January 10, 2022
Revised: January 24, 2022
Accepted: February 19, 2022
Article in press: February 19, 2022
Published online: April 6, 2022
Processing time: 117 Days and 2 Hours
Polycystic ovary syndrome (PCOS) is characterized by hyperandrogenism, hyperinsulinemia, ovarian polycystic changes, and irregular ovulation, often occurring in women of childbearing age for whom it can be a cause of infertility. Hypothalamus-pituitary-ovarian axis dysregulation is important in the pathogenesis of PCOS and the associated chronic excess of sex hormones can lead to cardiovascular and cerebrovascular diseases, diabetes, and malignancies such as endometrial cancer, and breast cancer. At present, most scholars agree that lifestyle interventions in conjunction with drug treatment can help PCOS patients achieve their goals of successful pregnancy and childbirth.
To investigate the clinical effect of an online and offline (O2O) preventive health management model on PCOS with kidney deficiency and phlegm dampness.
A total of 82 patients with PCOS of the kidney deficiency and phlegm dampness type who were admitted to Beijing Luhe Hospital Affiliated to Capital Medical University from April 2019 to June 2020 were randomly divided into two groups. The treatment group was treated with oral Diane-35 for 3 mo and received preventive O2O medical health management for 6 mo (including eating and living, exercise, drug management). The control group was treated with oral Diane-35 for 3 mo and completed outpatient health education. The traditional Chinese medicine (TCM) syndrome score, acne score, hair score, sex hormone level and clinical effects were compared between the two groups before and after the intervention.
After treatment, the TCM syndrome score, acne score, and serum luteinizing hormone/follicle stimulating hormone level were significantly lower in the treatment group than in the control group (P < 0.05). After 3 mo of treatment, the TCM syndrome curative effect index in the treatment group was 97.30% compared to 54.05% in the control group (P < 0.05), whereas the total treatment effect in the treatment group was 91.89%, compared to 54.05% in the control group (P < 0.05).
An integrated therapeutic approach incorporating medication, TCM methods and social media is more effective than standard treatment for PCOS.
Core Tip: The clinical manifestations of polycystic ovary syndrome are oligomenorrhea, anovulation, ovarian polycystic changes, infertility, obesity, acne, and hirsutism. The effects of a preventive online and offline health management model on polycystic ovary syndrome patients are greater than simple basic treatment, and have significant advantages in improving clinical symptoms and outcomes.
- Citation: Liu R, Li M, Wang P, Yu M, Wang Z, Zhang GZ. Preventive online and offline health management intervention in polycystic ovary syndrome. World J Clin Cases 2022; 10(10): 3060-3068
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3060.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3060
Polycystic ovary syndrome (PCOS) is an endocrine disorder common among women of reproductive age. The clinical manifestations are oligomenorrhea, anovulation, ovarian polycystic changes, infertility, obesity, acne, and hirsutism. The etiology has not been fully clarified, and existing theories suggest that it is related to primary ovarian dysfunction, adrenal dysfunction, hyperinsulinemia, hypothalamic dysfunction and other factors[1]. The clinical treatment of PCOS according to western medicine is focused on using ovulation promoting drugs, which, due to side effects, are poorly tolerated and thus ineffective for some patients. The development of new therapies for PCOS that can potentially be combined, has become the target of future research[2].
Traditional Chinese medicine (TCM) classifies PCOS into the categories of infertility, irregular menstruation and abdominal mass. Polycystic ovary syndrome is thought to be associated with kidney deficiency and liver depression, with phlegm dampness and blood stasis as the underlying causes. The treatment is based on tonifying the kidney and soothing the liver, as well as promoting blood circulation and addressing blood stasis[3]. At this stage, with the rapid development of Internet medical care and big data, the online and offline (O2O) health management model has gradually become popular, and has a good development prospects. The Chinese and Western medicine health management model in the era of "Internet +" has achieved good results in the treatment of various chronic diseases. The O2O health management model based on the theoretical system of Chinese medicine preventive treatment has been used in patients with ovulatory disorders. It has a good effect and plays an important role in preventing the disease before it occurs, preventing the disease after the disease, and preventing the relapse after recovery. Online and Offline health treatments also have the purpose of improving physical fitness and preventing the development of diseases[4]. The O2O health management model based on the theoretical system of preventive treatment of disease in traditional Chinese medicine can allow patients with gynecological diseases to monitor their conditions and own health care, and be actively involved with their treatment.
At present, there is no theory merging preventive treatment of disease and O2O healthcare management. Therefore, we aimed to conduct clinical research on the application of an O2O health management model to intervene in PCOS of the kidney deficiency and phlegm-dampness type.
Eighty-two patients with PCOS of the kidney deficiency and phlegm dampness type admitted to Beijing Luhe Hospital affiliated to Capital Medical University from April 2019 to June 2020 were randomly assigned into a treatment group and a control group, with 41 patients in each group. The inclusion criteria were: (1) Meeting the western diagnostic criteria of PCOS: presence of hirsutism, amenorrhea, oligo-ovulation or anovulation, based on the expert consensus on diagnosis and treatment of polycystic ovary syndrome written by the Chinese Medical Association, Obstetrics and Gynecology and Endocrinology group[5]; (2) Meeting the TCM diagnostic criteria for kidney deficiency and phlegm dampness syndrome as described in Clinical Guiding Principles of New Drugs of Traditional Chinese Medicine, and Gynecology of Traditional Chinese Medicine[6,7] issued by the 2002 National Food and Drug Administration; (3) Age between 24 and 40 years old; (4) Absence of other types of related treatment within the 3 mo prior to enrolling in the study; and (5) Completion of informed consent prior to initiation of treatment. Exclusion criteria: (1) Congenital gonadal dysplasia, reproductive tract structural abnormalities, tubal obstruction, pituitary tumors, malignant tumors of reproductive organs, Cushing’s syndrome, adrenal or ovarian androgen-secreting tumors, adrenal hyperplasia, hyperprolactinemia, thyroid or other endocrine dysfunction; (2) Use of contraceptives (other than barrier methods) or antipsychotics; (3) Refusal to use, or a history of allergy to, Diane-35; (4) Other concurrent related treatments; (6) Presence of combined heart, cerebrovascular, liver, kidney, hematopoietic, or psychiatric disorders; and (7) Lack of cooperation with study protocol.
All patients were treated with ethinylestradiol cyproterone tablets (brand name: Diane-35, Bayer Medical and Health Co., Ltd., specification: 2 mg of cyproterone acetate and 0.035 mg of ethinylestradiol in each tablet, Chinese medicine standard J20140114). One tablet per day was taken from the fifth day of the natural menstrual cycle and was continued for 21 d. Diane-35 treatment was repeated from the fifth day of the next menstrual cycle. In patients with amenorrhea using progesterone capsules for artificial menstruation, oral progesterone capsules at a dose of 100 mg/d were administered for 5 d to achieve withdrawal bleeding. Diane-35 was taken on the fifth day of drug withdrawal bleeding, following the same regimen as above. The treatment was continued for 3 mo.
The control group only completed outpatient health education. The treatment group received O2O preventive medical health management for 6 mo, including advice for eating and living, exercise, and drug management. A health management team was established to consult relevant literature with the keywords of: PCOS, O2O, TCM intervention and preventive medicine. The treatment group was divided into teams composed of 10-11 patients. The researchers educated the teams by delivering popular science lectures and answering questions. The main components of patient education were the basic idea of self-management of health issues, PCOS-related knowledge, the significance of self-management for PCOS, self-management methods, family intervention skills, diet management (including the consumption of tea), exercise management (including acupoint massage), and the use of standardized medications. The teams met once a month, for 1 h each time, and at the end of the meeting a handout titled “The health life of PCOS with kidney deficiency and phlegm dampness type” was distributed to the patients. The following personalized prescriptions were formulated and distributed to the patients: (1) According to height, weight and physical condition, the daily required heat and consumption of specific food portions and a reference diet were calculated. At the same time, patients were asked to download the Mint Health application to develop a diet and exercise plan and complete daily card printing; (2) Group activities: the patients participated in a WeChat group through which they exchanged questions and answers on daily diet, exercise, and medication diary cards; (3) A substitute tea drink: Sangjisheng 5 g, Chuandu 5 g, Tusizi 5 g, Gouqizi 5 g, Dazao 5 g, Dangshen 5 g, Fuling 5 g, Baizhu 5 g, boiled for 30 minutes and consumed once per day was used as a substitute for tea; and (4) Acupoint massage: the patients were advised to massage the following acupoints: Sanyinjiao, Guanyuan, Qihai, Zhongji, Zigong, using the tips of the thumbs or the middle fingers with a certain degree of strength, and in a clockwise fashion, focusing on firm contact of the fingers with the skin and avoiding shifting of the fingers for 3-5 min, 2-3 times a day. The patients were followed for 6 mo, and the efficacy was evaluated at the end of this period.
The clinical effects on TCM syndrome score, acne score, hair score, and sex hormone levels [androgen (T), luteinizing hormone (LH), and follicle stimulating hormone (FSH)] before and after the intervention were compared between the two groups.
Chinese medicine diagnostic criteria associated symptoms were given 0, 2, 4, or 6 points. Secondary symptoms such as: menstrual volume and color, edema and discomfort of the waist and knees, headaches, anorexia, loose stools, chest tightness, fullness, obesity, mouth dryness, sticky mouth or phlegm, were given 0, 1, 2, or 3 points, according to severity. The presence of a pale tongue with white greasy moss and a weak pulse corresponded to one plus two points. The sum of the main criteria, secondary criteria and tongue appearance score was the total score of TCM syndrome.
Acne severity was graded using the Pillsbury clinical grading system which generally consists of four grades: grade I (light, 1 point), blackhead acne with scattered and multiple inflammatory lesions; grade II (medium, 2 points), grade I plus superficial pustules, more inflammatory lesions, only limited to the face; grade III (severe, 3 points), grade II with more extensive inflammatory lesions, occurring in the face, neck and back; and grade IV (severe-cluster, 4 points), grade III plus cysts, propensity for scars, occurring in the upper body[8-11].
The hair score was calculated using the Freeiman-Gallwey scale. The score was mainly calculated from the body hair of the upper lip, mandible, chest, upper back, lower back, upper abdomen, lower abdomen and upper arm of the patient, and 1-4 points were given respectively. The higher the score, the denser the patient 's body hair[12,13].
The TCM syndrome curative effect index (n) was calculated as: [ (before treatment symptom score-after treatment symptom score)/before treatment symptom score] × 100% and was classified as: consistent with clinical recovery if n ≥ 90%; markedly effective if 70%≤ n < 90%; effective if 30% ≤ n < 70%; and invalid if n < 30%.
Based on the comprehensive curative effect, clinical cure was defined as achievement of pregnancy within 1 mo, menstrual recovery, a TCM curative effect index ≥ 90%, body mass index (BMI) ≤ 24, laboratory test results within normal range, biphasic basal body temperature (BBT) indicating regular ovulation. Markedly effective treatment was defined as: after treatment, the menstrual cycle tended to be normal (about 45 d), and the color quality was significantly improved, a TCM curative effect index of 70%-90%, the BMI was close to 24, the laboratory results were generally normal and the BBT was biphasic with a slight delay in ovulation. Effective treatment was defined as: menstruation occurring at least once within three months after treatment and the color quality was slightly improved compared with that before treatment, a TCM curative effect index of 30%-70%, the BMI was decreased and the BBT indicated prolonged delay of ovulation. Invalid treatment was defined as: menstruation did not improve after treatment, a TCM curative effect index < 30%, laboratory test results were not changed and in the absence of BBT fluctuation, consistent with the absence of ovulation.
Before treatment and 12 wk after treatment, 3 mL of venous blood was collected from patients at the early follicular phase, after fasting for at least 8 h. Venous blood samples were placed in EDTA anticoagulant containing tubes, and centrifuged within 1 h at a speed of 4000 r/min for 10 min. Serum T, LH and FSH were determined by radioimmunoassay, and LH/FSH values were calculated. The radioimmunoassay kits were all sourced from Roche, and they were analyzed using an HH6003 γ radioimmunoassay analyzer.
The age, BMI and course of disease of the patients in this study, which were tested for normal distribution and were consistent with normal or near normal distribution, are expressed as mean ± SD. The numerical data were expressed as percentages, and comparisons were performed by the t-test or χ2 test. All data were processed using the professional SPSS 21.0 software with a level of significance set as P < 0.05.
There was no statistically significant difference in age, BMI, course of disease, exercise, sleep and eating habits between the two groups (P > 0.05). Four patients in each group withdrew from the study (Table 1).
| Normal information | Therapy group (n = 41) | Control group (n = 41) | t/χ2 | P value |
| Age (yr) | 30.5 ± 3.1 | 29.9 ± 3.5 | 0.822 | 0.414 |
| BMI (kg/m2) | 27.7 ± 4.9 | 26.6 ± 4.2 | 1.091 | 0.278 |
| Course of disease (mo) | 31.0 ± 7.1 | 32.0 ± 8.4 | -0.582 | 0.562 |
| Exercise less (%) | 28 (68.29) | 28 (68.29) | 0.000 | 1.000 |
| Stay up late (%) | 32 (78.05) | 35 (85.37) | 0.734 | 0.391 |
| Spicy food (%) | 31 (75.61) | 30 (73.17) | 0.064 | 0.800 |
| Greasy (%) | 27 (65.85) | 32 (78.05) | 1.511 | 0.219 |
| Favorite sweets (%) | 27 (65.85) | 31 (75.61) | 0.943 | 0.332 |
| Like cold drinks (%) | 26 (63.41) | 21 (51.22) | 1.246 | 0.264 |
| Salty taste (%) | 15 (36.59) | 9 (21.95) | 2.121 | 0.145 |
| Bitter taste (%) | 7 (17.07) | 6 (14.63) | 0.091 | 0.762 |
| Sour taste (%) | 7 (17.07) | 3 (7.32) | 1.822 | 0.177 |
| Regular diet (%) | 7 (17.07) | 7 (17.07) | 0.000 | 1.000 |
| Obesity in childhood or adolescence (%) | 22 (53.66) | 18 (43.9) | 0.781 | 0.377 |
| Long time stress (%) | 15 (36.59) | 11 (26.83) | 0.901 | 0.342 |
| Family history of diabetes (%) | 25 (60.98) | 22 (53.66) | 0.449 | 0.503 |
Before treatment, there was no significant difference in TCM syndrome score, acne score and hair score between the two groups (P > 0.05). After treatment, the TCM syndrome score and acne score in the treatment group were significantly lower than those in the control group, as shown in Table 2.
| Index | Time | Therapy group (n = 37) | Control group (n = 37) | t | P value |
| TCM syndrome score | Before treatment | 29.32 ± 7.66 | 27.84 ± 7.20 | 0.856 | 0.395 |
| After treatment | 11.24 ± 3.72 | 24.29 ± 6.03 | -11.204 | 0.000 | |
| Acne score | Before treatment | 1.41 ± 0.56 | 1.56 ± 0.59 | -1.122 | 0.266 |
| After treatment | 0.56 ± 0.21 | 1.26 ± 0.38 | -9.807 | 0.000 | |
| Hair score | Before treatment | 12.10 ± 3.90 | 11.10 ± 4.61 | 1.007 | 0.317 |
| After treatment | 11.30 ± 2.70 | 10.79 ± 2.86 | 0.789 | 0.433 |
Before treatment, there were no significant differences in serum T, LH, FSH or LH/FSH levels between the two groups (P > 0.05). After treatment, the serum LH/FSH level in the treatment group was significantly lower than in the control group (Table 3).
| Index | Time | Therapy group (n = 37) | Control group (n = 37) | t | P value |
| T (ng/mL) | Before treatment | 0.56 ± 0.18 | 0.64 ± 0.24 | -1.622 | 0.109 |
| After treatment | 0.39 ± 0.11 | 0.42 ± 0.12 | -1.121 | 0.266 | |
| LH (mIU/mL) | Before treatment | 9.68 ± 2.31 | 10.70 ± 2.63 | -1.772 | 0.081 |
| After treatment | 8.02 ± 1.82 | 9.44 ± 7.66 | -1.097 | 0.276 | |
| FSH (mIU/mL) | Before treatment | 5.88 ± 1.22 | 6.46 ± 1.81 | -1.616 | 0.110 |
| After treatment | 5.42 ± 1.36 | 5.84 ± 1.59 | -1.221 | 0.226 | |
| LH/FSH | Before treatment | 1.80 ± 0.46 | 1.96 ± 0.58 | -1.315 | 0.193 |
| After treatment | 1.48 ± 0.62 | 2.14 ± 0.77 | -4.061 | 0.000 |
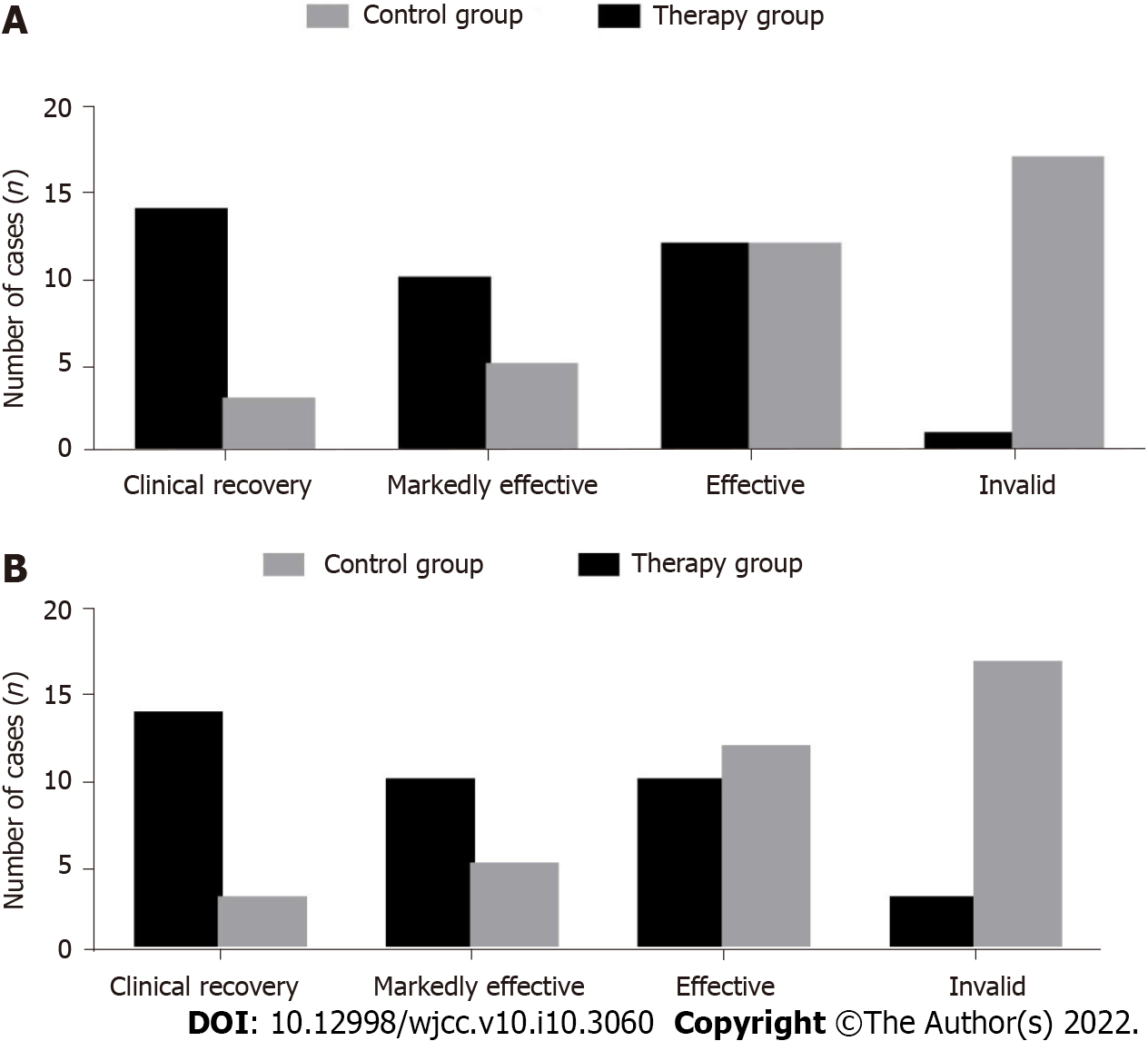
After 3 mo of treatment, the TCM syndrome curative effect index of the treatment group was 97.30%, which was significantly higher than the 54.05% of the control group (Table 4, Figure 1A).
| Group | n | Clinical recovery | Markedly effective | Effective | Invalid | Total effective rate |
| Therapy group | 37 | 14 | 10 | 12 | 1 | 36 (97.30) |
| Control group | 37 | 3 | 5 | 12 | 17 | 20 (54.05) |
| χ2 | 18.794 | |||||
| P value | 0.000 |
After 3 mo of treatment, the total treatment effect in the treatment group was 91.89%, which was significantly greater that the 54.05% found in the control group (Table 5, Figure 1B).
| Group | n | Clinical recovery | Markedly effective | Effective | Invalid | Total effective rate |
| Therapy group | 37 | 14 | 10 | 10 | 3 | 34 (91.89) |
| Control group | 37 | 3 | 5 | 12 | 17 | 20 (54.05) |
| χ2 | 13.430 | |||||
| P value | 0.000 |
In this study, O2O preventive health management achieved good therapeutic effect on PCOS, improving the TCM syndrome score and acne score as well as the total effective rate. It is suggested that the effect of a preventive O2O health management model on PCOS patients is greater than that of simple basic treatment. This is due to the preventive nature of the O2O health management model. Through literature review, a list of the possible complications of PCOS and adverse drug reactions was compiled which was then released to the WeChat group and other popular social platforms to help patients fully understand the harm of PCOS, master self-management methods, and be more actively involved in treatment decisions and interventions[14,15]. The patients’ self-management ability improved with family intervention in diet management (including a substitute tea drink), exercise management (including acupoint massage) and standardized medications. Personalized prescriptions were formulated for patients with specific food portions and a reference diet according to height, weight and physical condition. At the same time, patients were asked to download the Mint Health application to develop a diet and exercise plan and complete the daily card. Daily participation in the WeChat group led to exchange of information on diet, exercise and medication diaries. The use of tea drinks, acupoint massage and other methods to improve the patients’ well-being multiplied the effect the treatment[16,17].
The ovaries of PCOS patients synthesize too much T, with correspondingly increased levels of T in the follicular fluid. The stimulation of increased androgen and estrogen levels, leads to an increase in pituitary LH, and the negative feedback causes a drop in the FSH level, thereby inhibiting follicular development. Thus, an LH/FSH ratio > 2, is suggestive of PCOS[18,19]. In this study, we measured the levels of serum T, LH, FSH and LH/FSH in the two groups before and after treatment. We found that preventive O2O health management was helpful in regulating the endocrine profile of PCOS patients and relieving the inhibition of follicular development. This is also one of the mechanisms through which TCM syndrome score and clinical symptoms are reduced.
In recent years, with the acceleration of social changes, the incidence of PCOS in women of childbearing age is increasing due to the influence of high work-related pressure, irregular lifestyle, insufficient sleep, being overweight and other factors. The O2O health management model can help medical staff expand the scope of treatment, improve effectiveness of time management during follow up, expand the level of service, and reduce the cost of medical and health services[20]. The advantages of the O2O health management model based on the theory of preventive treatment are that: it can transform parts into wholes, patients health information can be uploaded to the central hospital information system to establish a health management database, and improve work efficiency, awareness and attention. The O2O health management model provides real and detailed information for gynecologists, pharmacists, and nutritionists based on the theory of TCM, so that medical staff can formulate targeted intervention measures. The process of O2O health management intervention is simple and easily followed online, breaking the limitations of time and place. Furthermore, the patients can be given timely feedback on any diversion from the treatment plan, which is conducive to better control of the disease.
However, the O2O health management model based on the theory of preventive treatment is rarely used in clinical practice, and may have limitations such as low efficiency and a lack of feedback and evaluation systems. In future research, it is necessary to further increase the level of health education and standardize the hospital management model to provide convenience for better patient service.
In conclusion, the effects of a preventive O2O health management model on PCOS patients are greater than simple basic treatment, and have significant advantages in improving clinical symptoms and outcomes.
The clinical treatment of polycystic ovary syndrome (PCOS) according to western medicine is focused on using ovulation promoting drugs, which, due to side effects, are poorly tolerated and thus ineffective for some patients. The development of new therapies for PCOS that can potentially be combined, has become the target of future research. At this stage, with the rapid development of Internet medical care and big data, the online and offline (O2O) health management model has gradually become popular, and has a good development prospects. The Chinese and Western medicine health management model in the era of "Internet +" has achieved good results in the treatment of various chronic diseases. The O2O health management model based on the theoretical system of Chinese medicine preventive treatment has been used in patients with ovulatory disorders. It has a good effect and plays an important role in preventing the disease before it occurs, preventing the disease after the disease, and preventing the relapse after recovery.
We aimed to conduct clinical research on the application of an O2O health management model to intervene in PCOS of the kidney deficiency and phlegm-dampness type.
To confirm that the therapeutic effect of prophylactic O2O health management model on patients with PCOS is better than that of basic treatment alone, and it has significant advantages in improving clinical symptoms and prognosis.
A total of 82 patients with PCOS of the kidney deficiency and phlegm dampness type were randomly divided into two groups. The treatment group was treated with oral Diane-35 for 3 mo and received preventive O2O medical health management for 6 mo. The control group was treated with oral Diane-35 for 3 mo and completed outpatient health education.
After treatment, the TCM syndrome score, acne score, and serum luteinizing hormone/follicle stimulating hormone level were significantly lower in the treatment group than in the control group. After 3 mo of treatment, the TCM syndrome curative effect index in the treatment group was 97.30% compared to 54.05% in the control group, whereas the total treatment effect in the treatment group was 91.89%, compared to 54.05% in the control group.
An integrated therapeutic approach incorporating medication, TCM methods and social media is more effective than standard treatment for PCOS.
In future research, it is necessary to further increase the level of health education and standardize the hospital management model to provide convenience for better patient service.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and Gynecology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Javed R, Srinivasan SP S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Jin P, Xie Y. Treatment strategies for women with polycystic ovary syndrome. Gynecol Endocrinol. 2018;34:272-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 2. | Wang B, Yan W, Hou LH, Wu XK. [Disorder of Tiangui (kidney essence) and reproductive dysfunction in patients with polycystic ovary syndrome]. Zhong Xi Yi Jie He Xue Bao. 2010;8:1018-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Wang Y, Zhao Y, Yu S, Hu Y. [Some issues from Effect of acupuncture and clomiphene in Chinese women with polycystic ovary syndrome in JAMA]. Zhongguo Zhen Jiu. 2017;37:1342-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Ma K. [Advantages of integrated Chinese and western medicine in diagnosis and treatment of anovulatory infertility due to kidney deficiency and blood stasis]. Zhongguo Zhong Yao Za Zhi. 2021;46:2623-2628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Wang XJ. [The Chinese medicine syndrome typing mode at the same level is the key point to explore the syndrome laws of disease. An inspiration from studying Chinese medicine syndrome laws of polycystic ovarian syndrome]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2012;32:1413-1415. [PubMed] |
| 6. | Jin C, Pang R, Xu L, Wu Z, Zhao J. [Clinical rules for acupoint selection and prescription composition in treatment of polycystic ovary syndrome with acupuncture]. Zhongguo Zhen Jiu. 2015;35:625-630. [PubMed] |
| 7. | Ma K, Li M. [Study on the mechanism of Bushen Culuan Chongji treating "kidney deficiency and blood stasis" in ovulatory dysfunctional infertility]. Zhongguo Zhong Yao Za Zhi. 2017;42:4445-4450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Li M, Ma K, Shan J. [Preliminary study on relationship of disease-syndrome-symptom of ovulatory disorder infertility based on factor analysis]. Zhongguo Zhong Yao Za Zhi. 2014;39:3860-3864. [PubMed] |
| 9. | Peigné M, Villers-Capelle A, Robin G, Dewailly D. [Hyperandrogenism in women]. Presse Med. 2013;42:1487-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Lima PDA, Nivet AL, Wang Q, Chen YA, Leader A, Cheung A, Tzeng CR, Tsang BK. Polycystic ovary syndrome: possible involvement of androgen-induced, chemerin-mediated ovarian recruitment of monocytes/macrophages. Biol Reprod. 2018;99:838-852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 11. | Puttabyatappa M, Padmanabhan V. Ovarian and Extra-Ovarian Mediators in the Development of Polycystic Ovary Syndrome. J Mol Endocrinol. 2018;61:R161-R184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Santos Simões R, Carbonel AAF, Borges FT, Baracat MCP, da Silva Sasso GR, Simões MJ, Serafini PC, Soares JM Júnior, Nader HB, Baracat EC. Analysis of hyaluronic acid in the endometrium of women with polycystic ovary syndrome. Gynecol Endocrinol. 2019;35:133-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Pundir J, Psaroudakis D, Savnur P, Bhide P, Sabatini L, Teede H, Coomarasamy A, Thangaratinam S. Inositol treatment of anovulation in women with polycystic ovary syndrome: a meta-analysis of randomised trials. BJOG. 2018;125:299-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 14. | Kowalczyk K, Franik G, Kowalczyk D, Pluta D, Blukacz Ł, Madej P. Thyroid disorders in polycystic ovary syndrome. Eur Rev Med Pharmacol Sci. 2017;21:346-360. [PubMed] |
| 15. | Forslund M, Landin-Wilhelmsen K, Schmidt J, Brännström M, Trimpou P, Dahlgren E. Higher menopausal age but no differences in parity in women with polycystic ovary syndrome compared with controls. Acta Obstet Gynecol Scand. 2019;98:320-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 16. | Kokanalı D, Karaca M, Ozakşit G, Elmas B, Engin Üstün Y. Serum Vitamin D Levels in Fertile and Infertile Women with Polycystic Ovary Syndrome. Geburtshilfe Frauenheilkd. 2019;79:510-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Bicer M, Alan M, Alarslan P, Guler A, Kocabas GU, Imamoglu C, Aksit M, Bozkaya G, Isil AM, Baloglu A, Aslanipoiur B, Calan M. Circulating insulin-like peptide 5 levels and its association with metabolic and hormonal parameters in women with polycystic ovary syndrome. J Endocrinol Invest. 2019;42:303-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Alur-Gupta S, Dokras A. Polycystic ovary syndrome: is the cardiometabolic risk increased after menopause? Menopause. 2019;26:331-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Rubin KH, Andersen MS, Abrahamsen B, Glintborg D. Socioeconomic status in Danish women with polycystic ovary syndrome: A register-based cohort study. Acta Obstet Gynecol Scand. 2019;98:440-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Jafari Khorchani M, Zal F, Neisy A. The phytoestrogen, quercetin, in serum, uterus and ovary as a potential treatment for dehydroepiandrosterone-induced polycystic ovary syndrome in the rat. Reprod Fertil Dev. 2020;32:313-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |