Copyright
©The Author(s) 2021.
World J Clin Cases. Nov 16, 2021; 9(32): 9997-10005
Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9997
Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9997
Figure 1 Positive and lateral view of lower digestive tract radiography.
Dilatation of the rectum and distal colon was not observed.
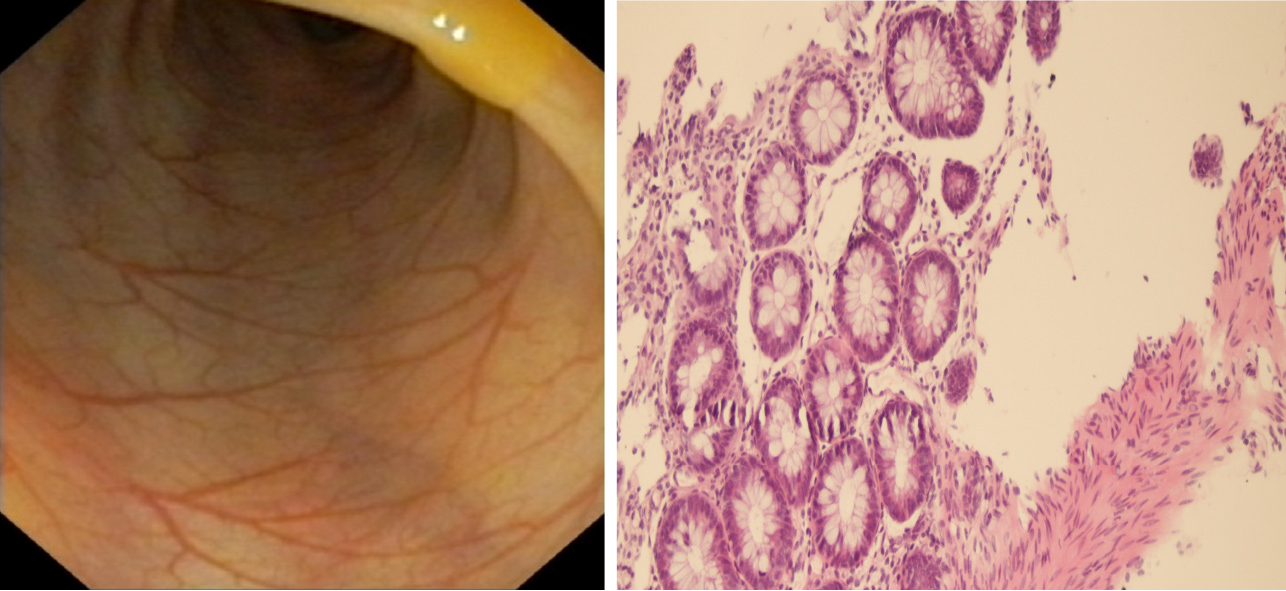
Figure 2 Colonoscopy and colonic biopsy showing chronic mucosal inflammation without granulomas, fissures, or bowel wall thickening.
Hematoxylin and eosin stain, magnification: 20 ×.
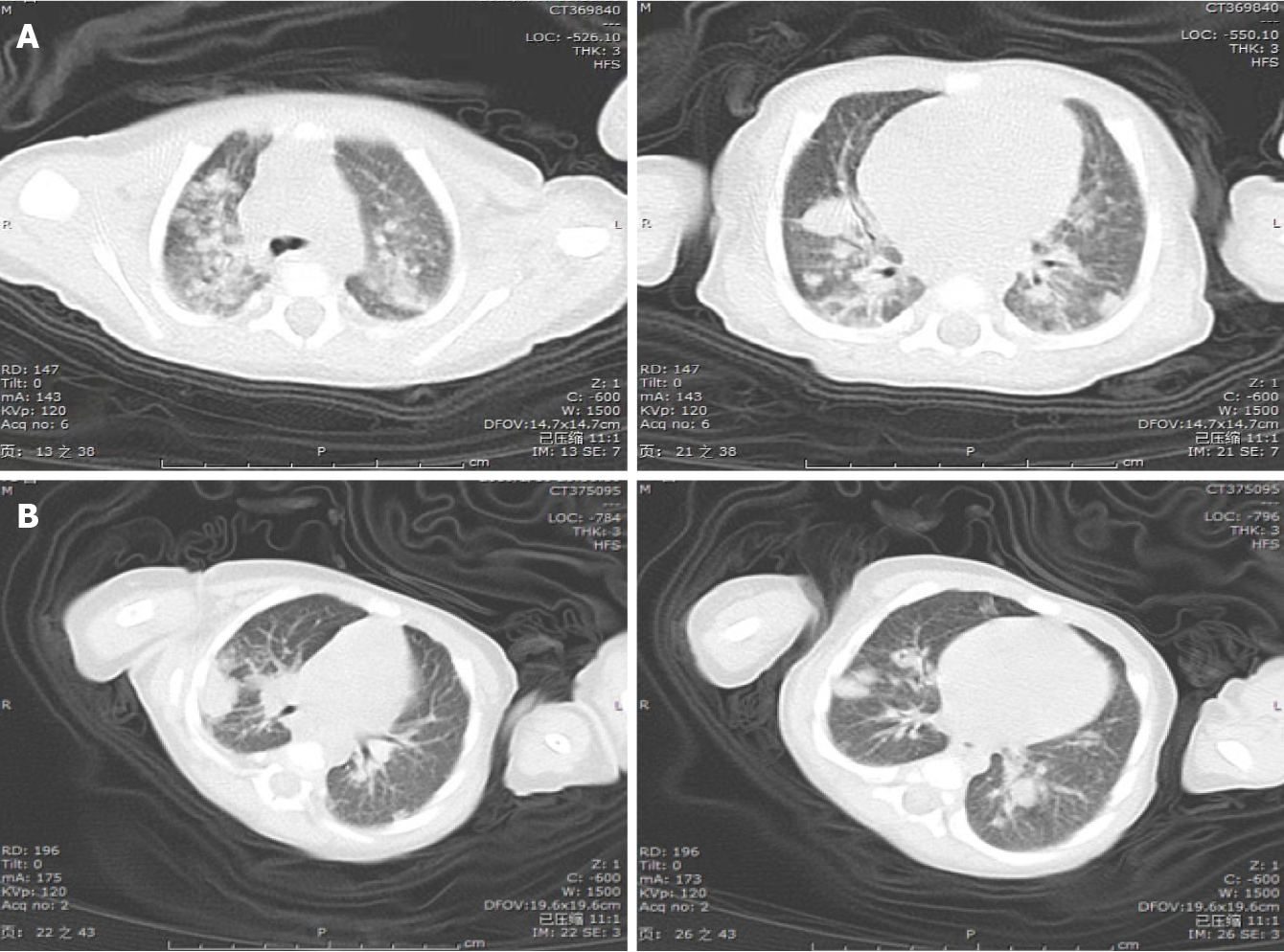
Figure 3 Computed tomography scan of the thorax.
A: Bilateral diffuse, scattered nodules and consolidation areas in different lung areas; B: The reduction of nodules and consolidations in the lungs.
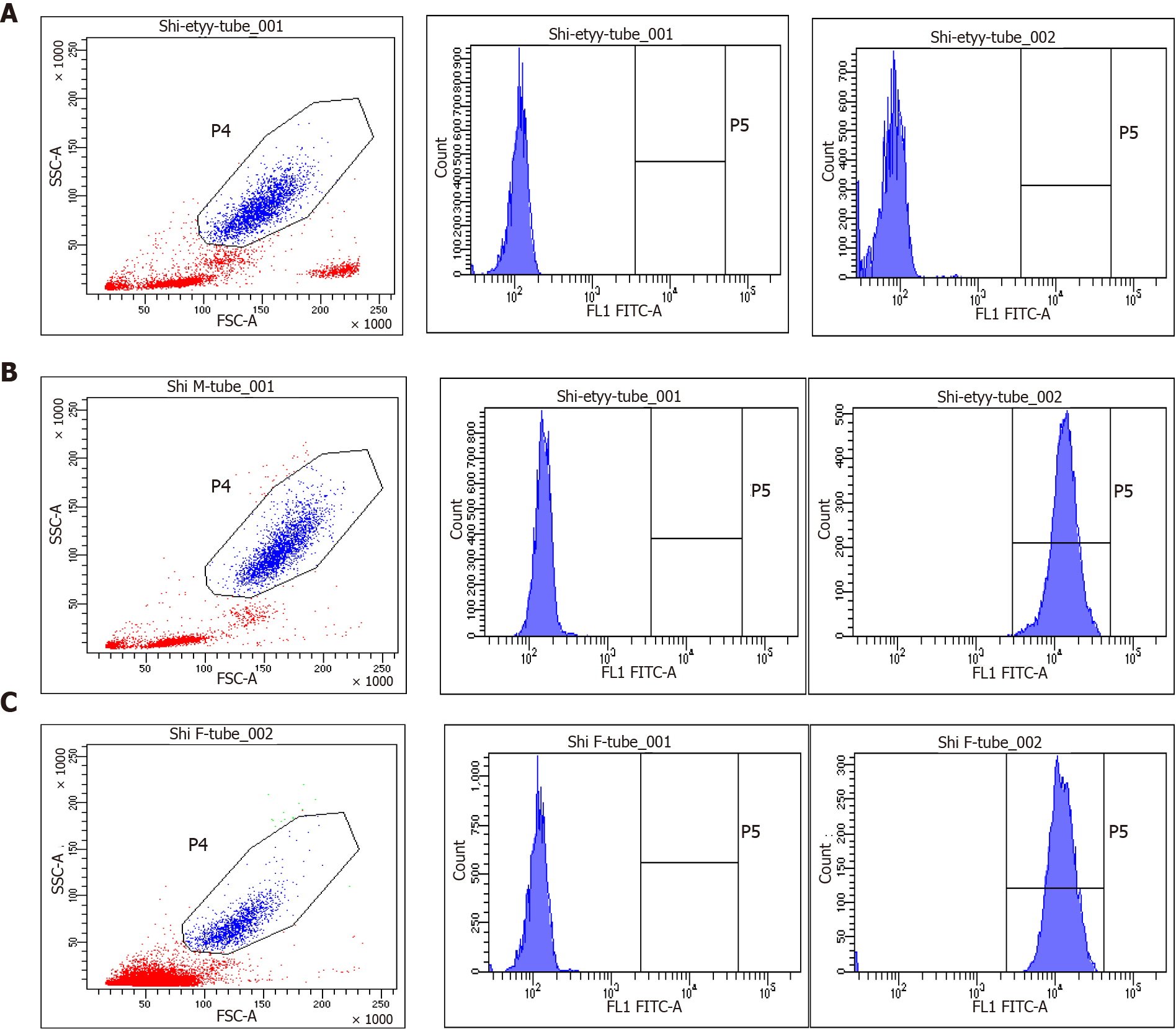
Figure 4 Histograms of the dihydrorhodamine assay of granulocytes from the male pediatric patient, his mother and father.
Histograms of the dihydrorhodamine (DHR) assay of the patient’s granulocyte (A) revealed the absence of fluorescence upon granulocyte stimulation. The DHR assay of granulocytes from the patient’s mother (B) and father (C) showed that the ratio of activated neutrophils was 99.6% and 98.5%, respectively.
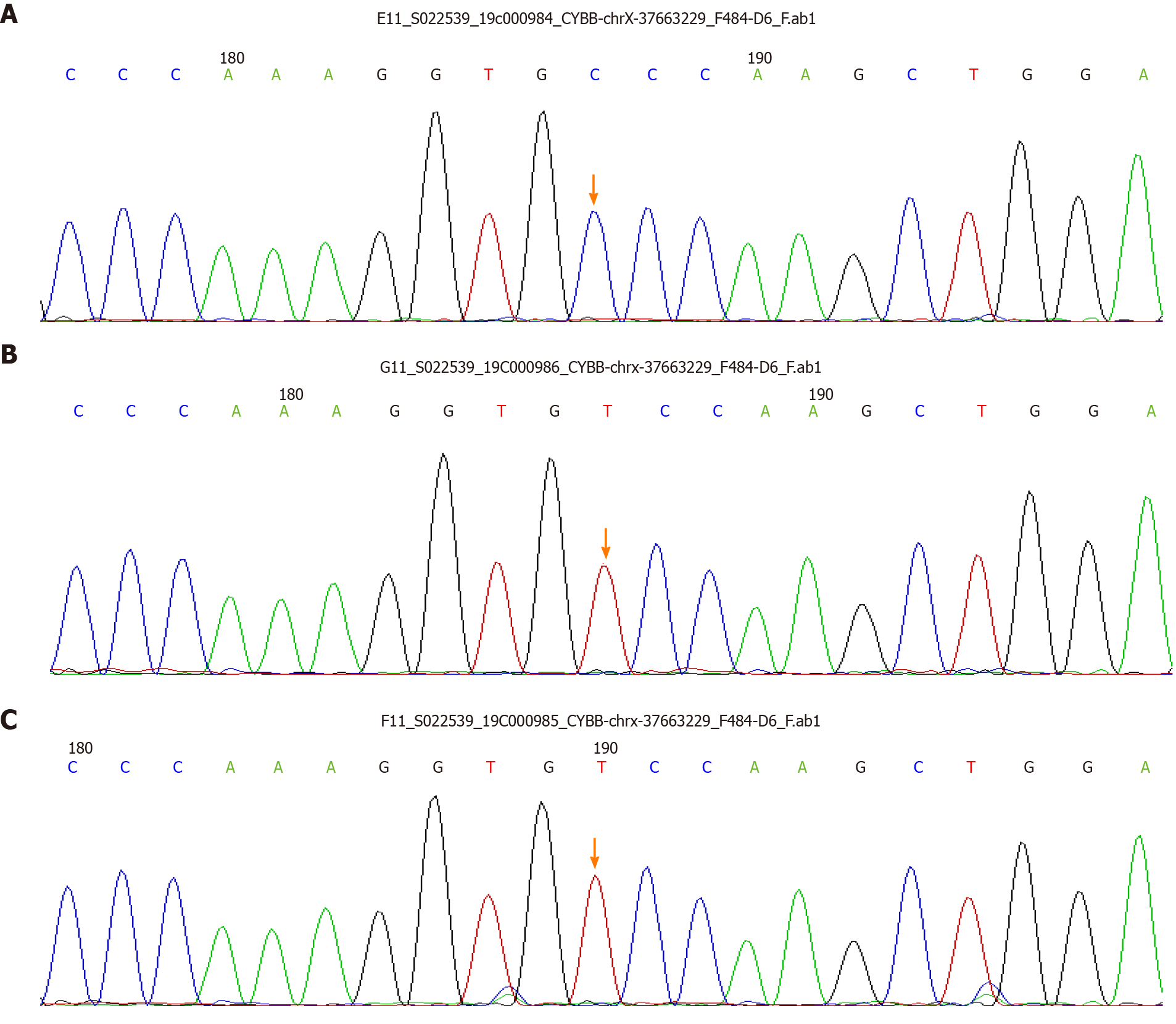
Figure 5 Analysis of a CYBB gene exon of the patient and his parents.
Chromatogram of a CYBB exon of the patient showed a missense mutation, c.997T>C (p.S333P). A: Patient; B: The patient’s mother; C: The patient’s father.
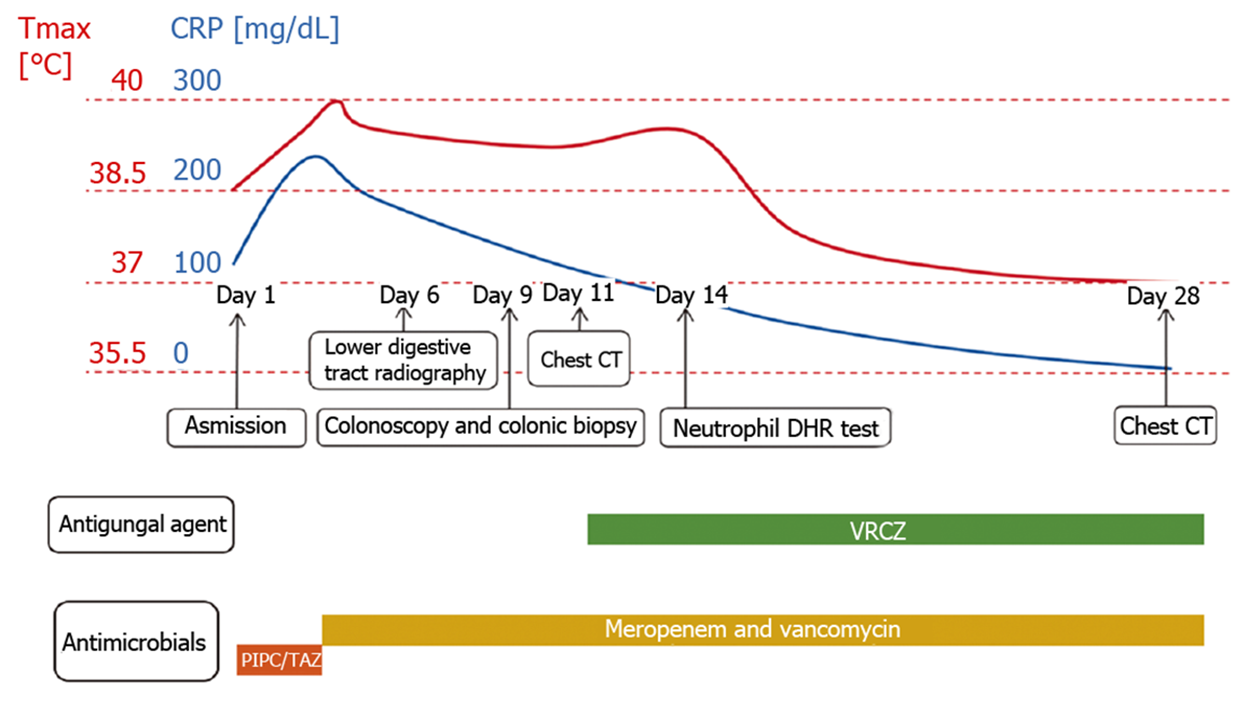
Figure 6 Clinical time course of the patient.
CRP: C-reactive protein; CT: Computed tomography; DHR: Dihydrorhodamine; VRCZ: Voriconazole; PIPC/TAZ: Piperacillin/tazobactam.
- Citation: Meng EY, Wang ZM, Lei B, Shang LH. Gastrointestinal symptoms as the first sign of chronic granulomatous disease in a neonate: A case report. World J Clin Cases 2021; 9(32): 9997-10005
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9997.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9997