Copyright
©The Author(s) 2021.
World J Clin Cases. Jun 6, 2021; 9(16): 4016-4023
Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.4016
Published online Jun 6, 2021. doi: 10.12998/wjcc.v9.i16.4016
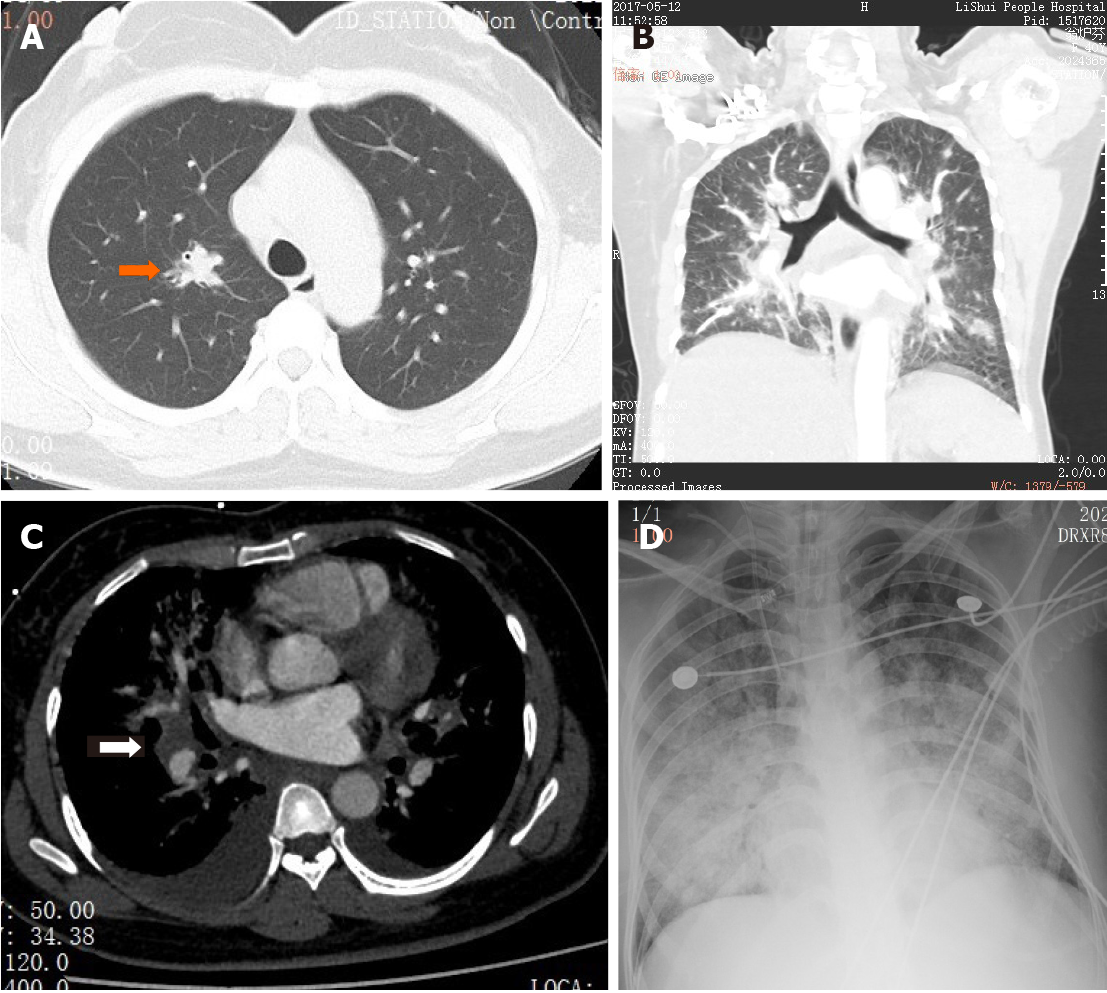
Figure 1 A 40-year-old woman presented with a 6-d history of fever (up to 38.
0 °C), non-productive cough, and exertional dyspnea. A: Chest computed tomography (CT; transverse section) at admission showed a solid nodule (arrow), 15 mm in diameter, with a poorly defined boundary in the upper lobe of the right lung. Several smaller solid nodules were seen in both lungs; B: Chest CT at admission (coronal section); C: A pulmonary CT angiogram showed normal pulmonary vasculature, but diffuse patchy shadows with poorly defined boundaries were seen in both lungs, with bilateral pleural effusion and an enlarged lymph node (25 mm × 21 mm) in the right hilum; D: Chest X-ray showed diffuse patchy shadows throughout both lungs.
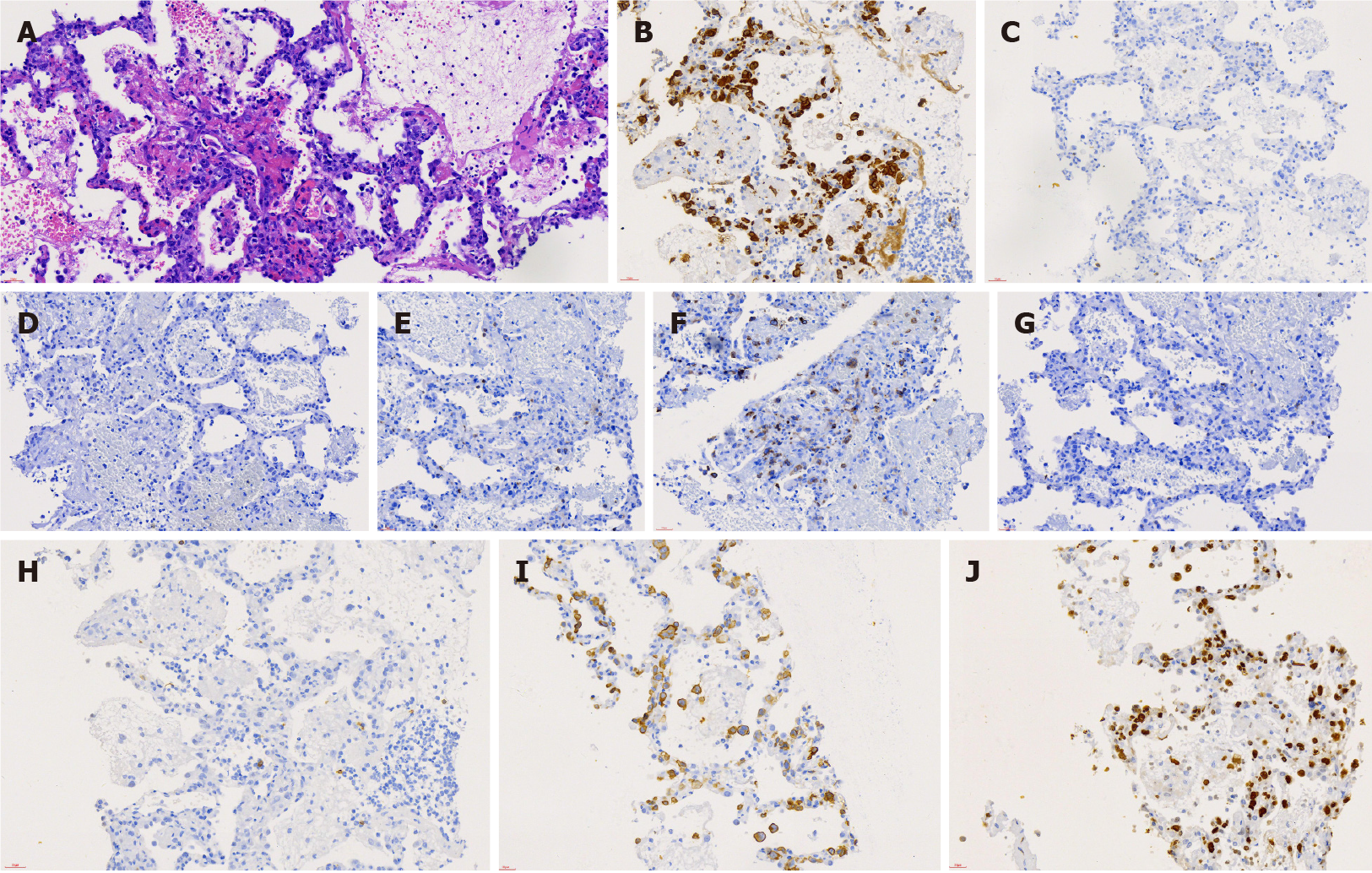
Figure 2 Pathological images of lung tissue biopsy at day 5 of hospitalization.
A: Hematoxylin-eosin staining showed the alveolar structure of the lung tissue with massive infiltration by large anaplastic lymphocytes in the alveolar septum with scattered neutrophils. Magnification, 400 ×; B-J: Immunostaining revealed that the tumor cells were ALK(+) (anaplastic lymphoma kinase) (B), CD3(-) (C), CD4(-) (D), CD5(-) (E), CD7(+) (F), CD8(-) (G), CD20(-) (H), CD30 (+) (I), and Ki-67(+) (J). Magnification, 400 ×.
- Citation: Jiang JH, Zhang CL, Wu QL, Liu YH, Wang XQ, Wang XL, Fang BM. Rapidly progressing primary pulmonary lymphoma masquerading as lung infectious disease: A case report and review of the literature. World J Clin Cases 2021; 9(16): 4016-4023
- URL: https://www.wjgnet.com/2307-8960/full/v9/i16/4016.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i16.4016