Copyright
©The Author(s) 2023.
World J Clin Cases. May 16, 2023; 11(14): 3248-3255
Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3248
Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3248
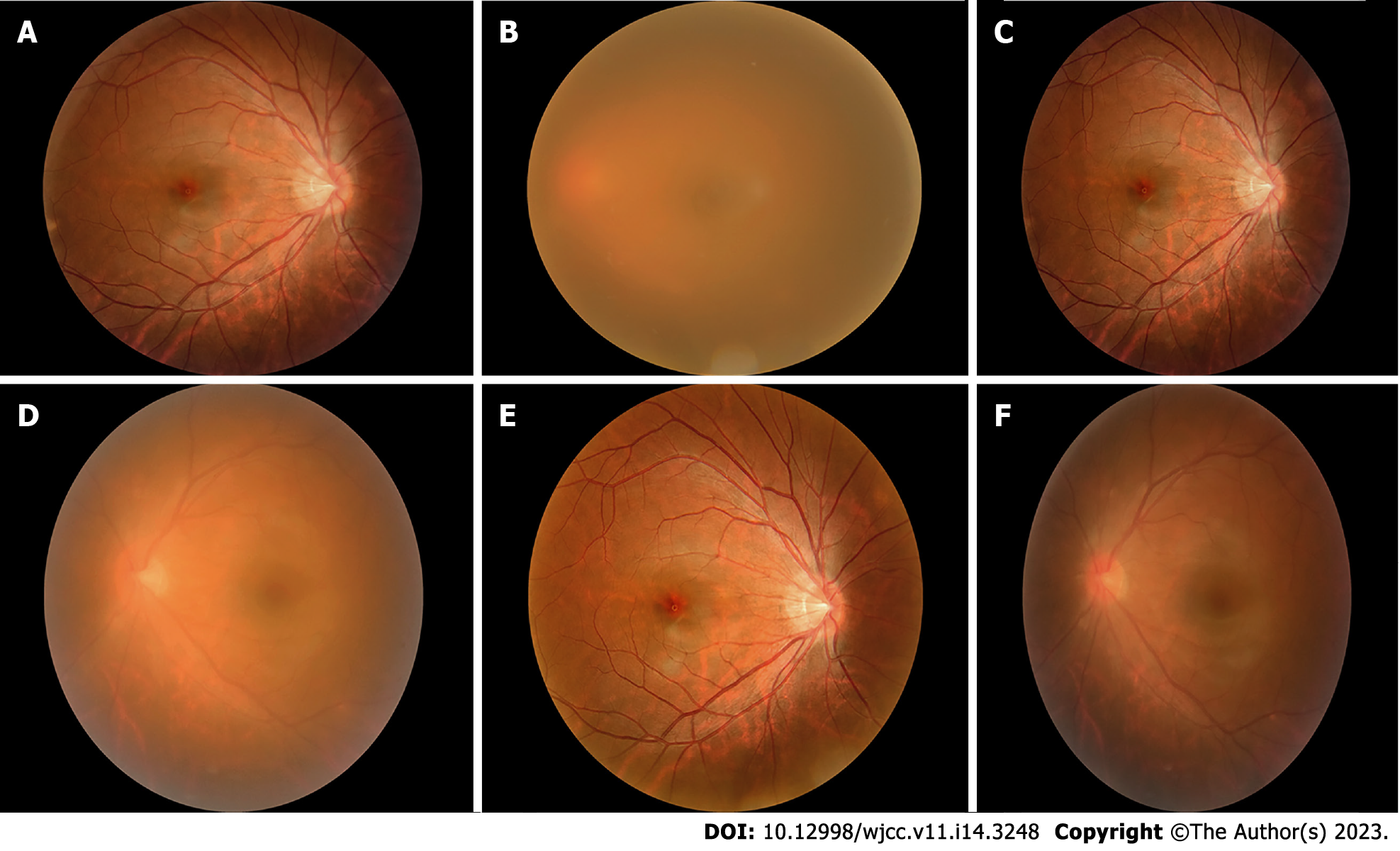
Figure 1 Fundus photography.
A: The edge of the optic disc in the right eye is clear, and yellow-white exudation and linear hemorrhage can be seen below the center of the macula (August 31st); B: The refractive interstitium in the left eye is not clear, and the fundus is unclear (August 31st); C: The optic disc edge in the right eye is clear, yellow-white exudation and linear hemorrhage are absorbed below the center of the macula (October 13th); D: The refractive interstitium in the left eye is slightly clearer than before, and the optic disc and large blood vessels are vaguely visible in the fundus (October 13th); E: The fundus in the right eye is almost normal (November 19th); F: The refractive interstitium in the left eye is clearer than before, the edge of the optic disc is clear, and the large blood vessels can run (November 19th).
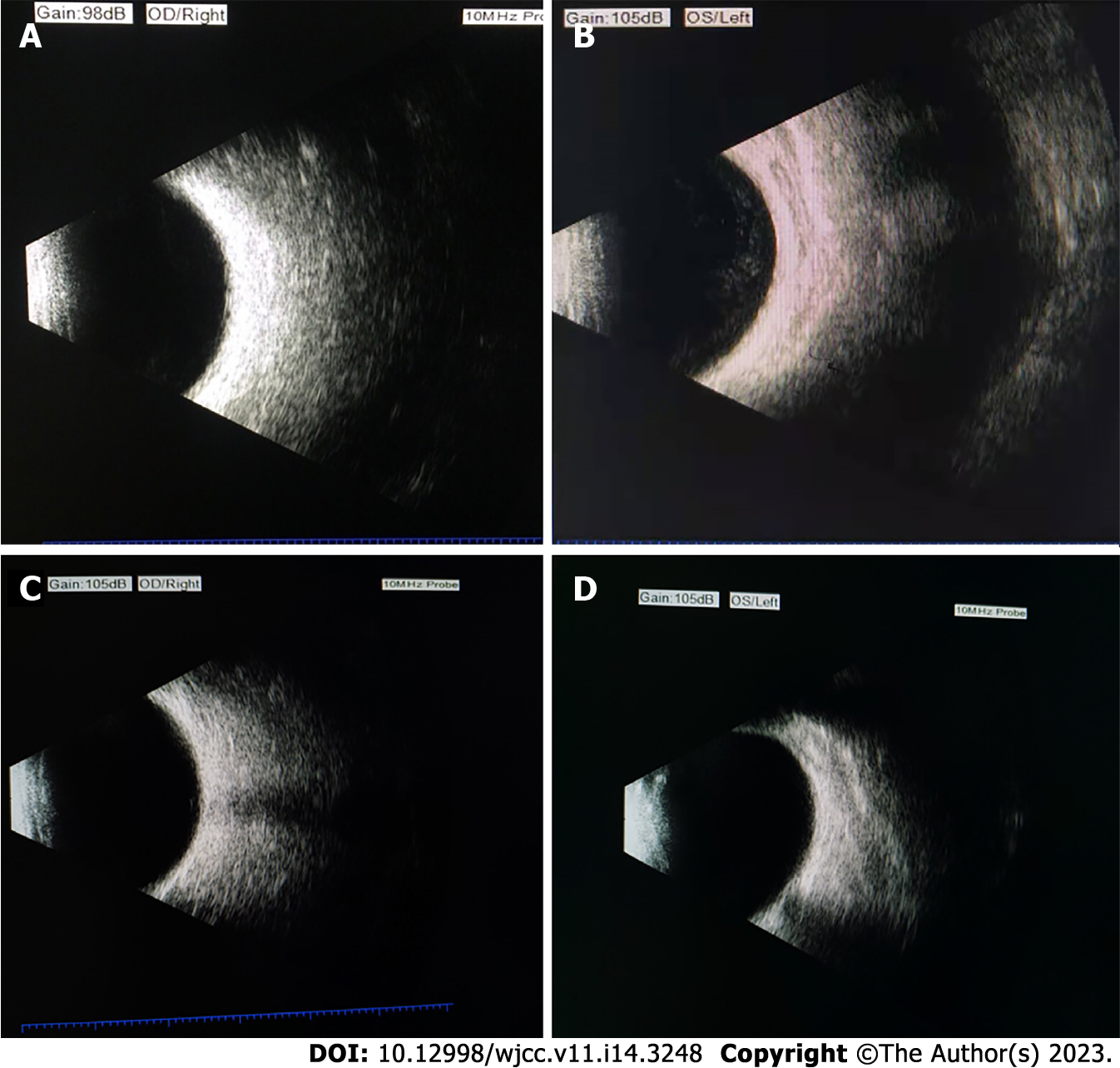
Figure 2 Changes in ocular B-ultrasound.
A: B-ultrasound showed no obvious abnormal echo in the vitreous cavity of the right eye (August 31st); B: B-ultrasound left eye vitreous haze 4+ (August 31st); C: B-ultrasound showed no obvious abnormal echo in the vitreous cavity of the right eye (November 19th); D: B-ultrasound left eye vitreous opacity changed to 0.5+ (November 19th).
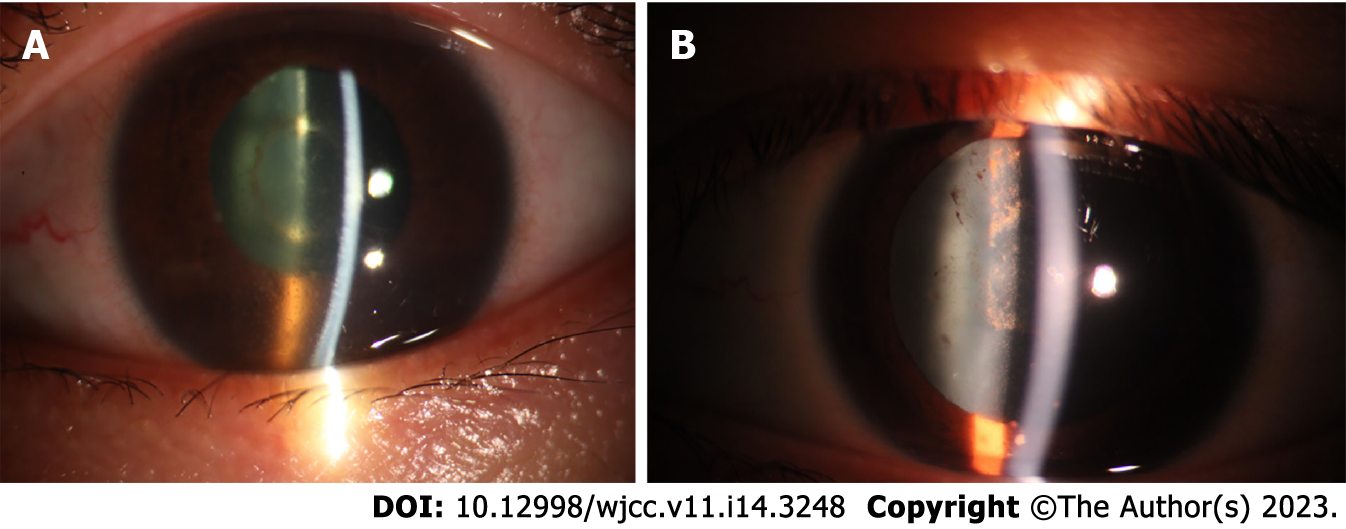
Figure 3 The results of eye photography before and after treatment showed that the eye was significantly improved.
A: Left eye anterior segment before treatment: Keratic precipitate (KP) (++), anterior chamber inflammatory cells 4+ (August 31st); B: Left eye anterior segment after treatment: Corneal suet-like KP (-), anterior chamber inflammatory cells 0.5+ (November 19th). The presence of KP indicates that the patient has chronic or granulomatous inflammation.
- Citation: Zhang YK, Guan Y, Zhao J, Wang LF. Diagnosis of tuberculous uveitis by the macrogenome of intraocular fluid: A case report and review of the literature. World J Clin Cases 2023; 11(14): 3248-3255
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3248.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3248