Copyright
©The Author(s) 2023.
World J Clin Cases. May 6, 2023; 11(13): 2981-2991
Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.2981
Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.2981
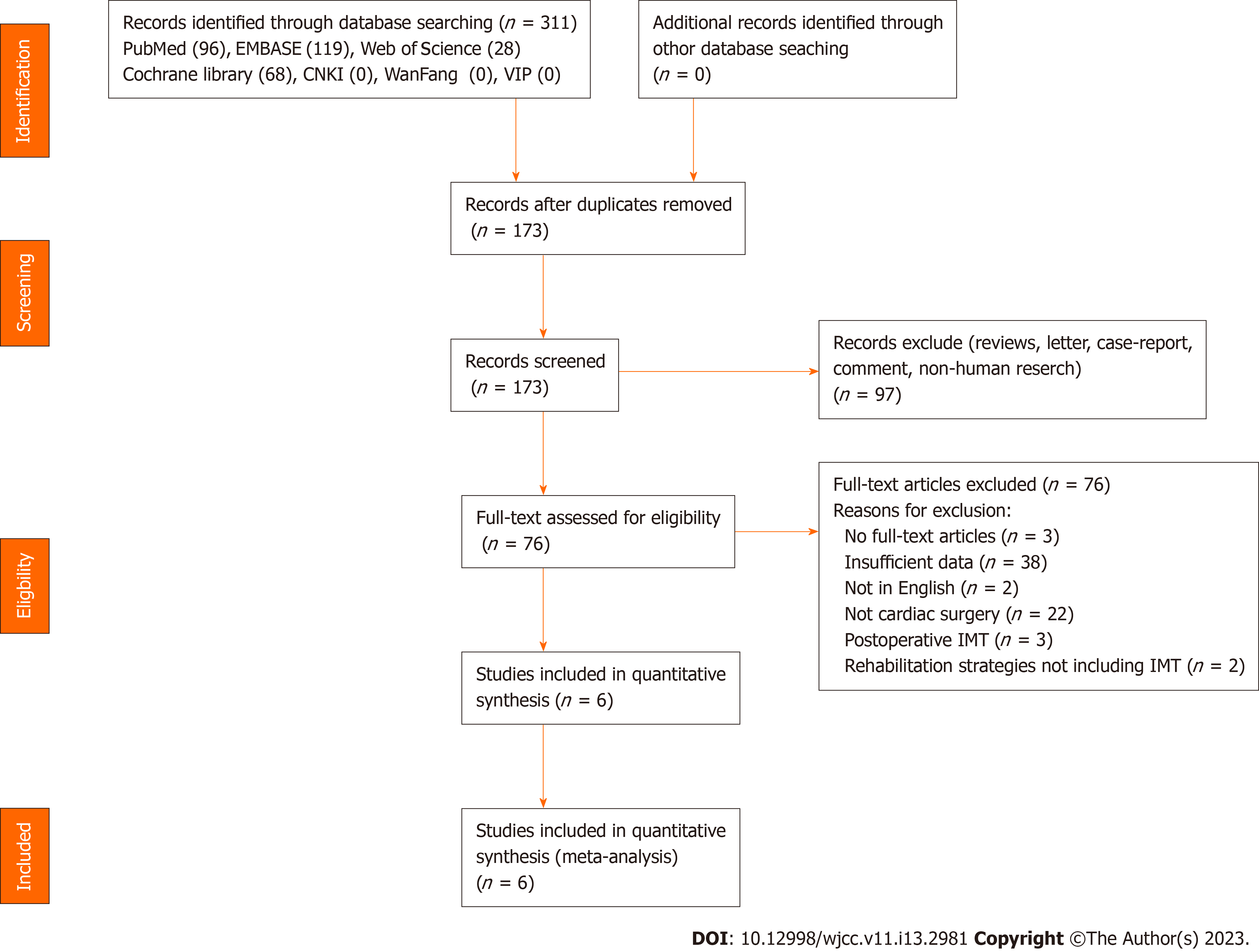
Figure 1 Flowchart of literature search.
After the initial search, 311 articles were selected. After a review of abstracts and full-text articles, only six trials met the inclusion criteria. CNKI: Chinese National Knowledge Infrastructure; IMT: Inspiratory muscle training.
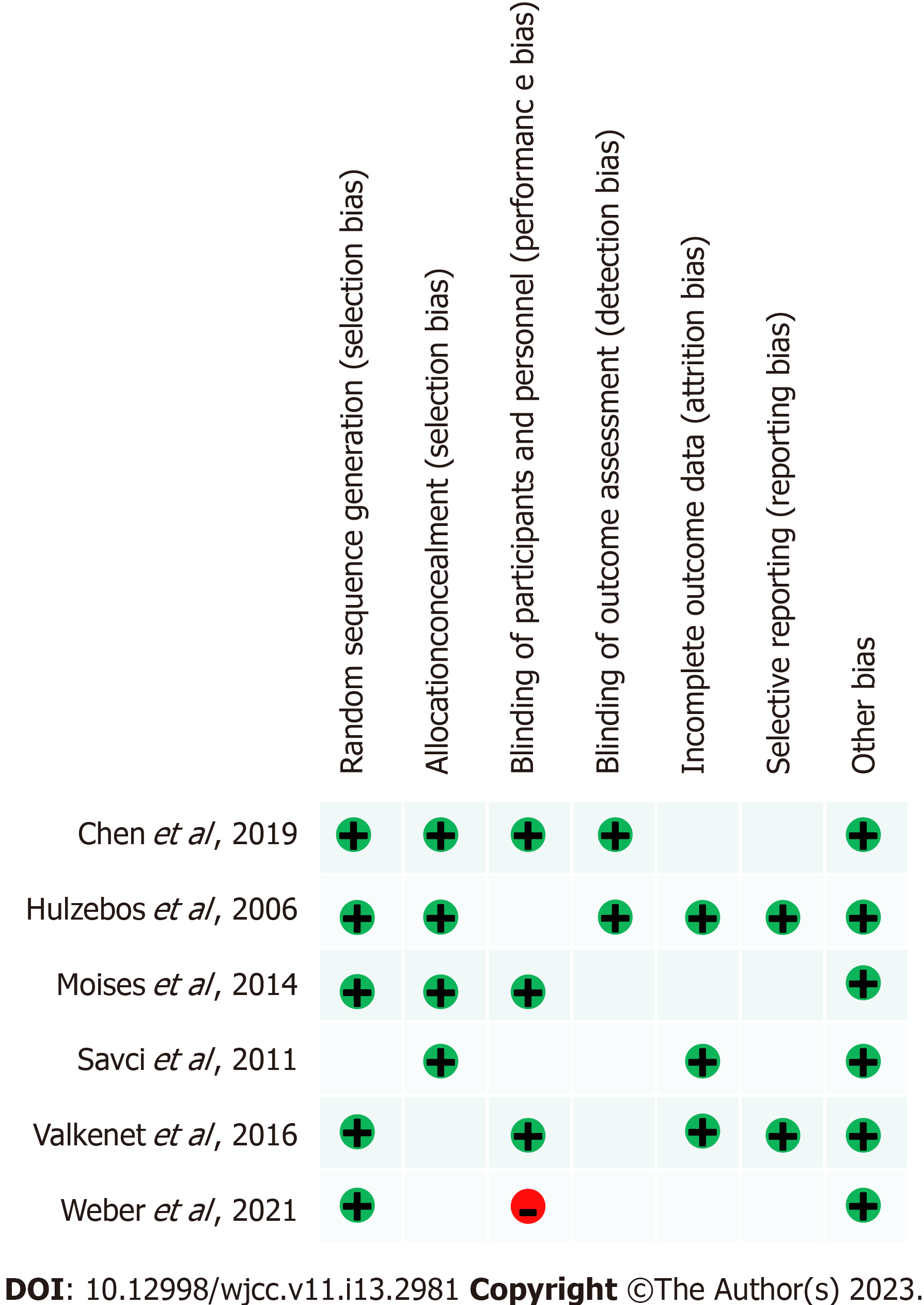
Figure 2 Risk of bias summary for each included study.
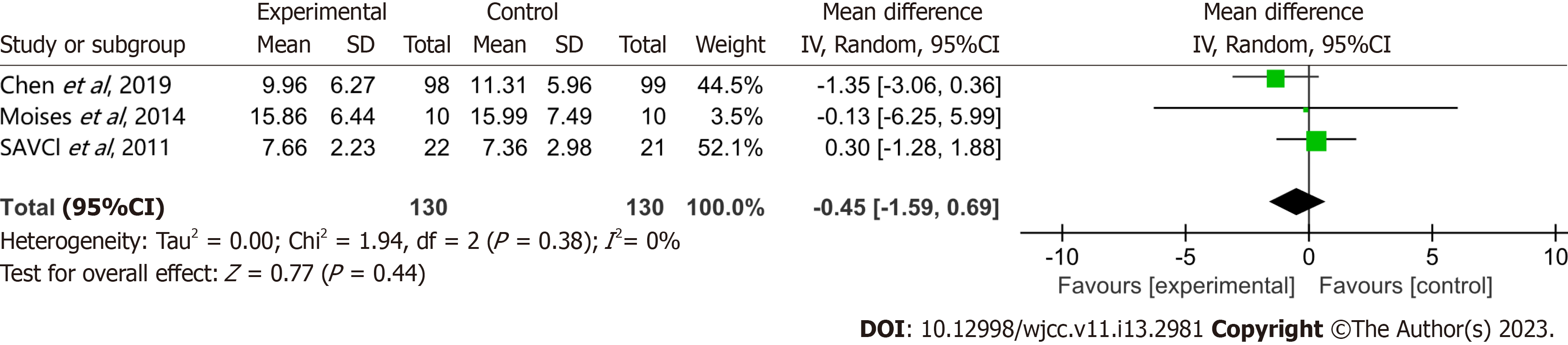
Figure 3 Effect of preoperative inspiratory muscle training on mechanical ventilation time.
The pooled mean difference of -0.45 h (95%CI: -1.59 to 0.69) and low heterogeneity (I² = 0) showed no statistically significant effect on mechanical ventilation time in patients with preoperative inspiratory muscle training after cardiac surgery. SD: Standard deviation.
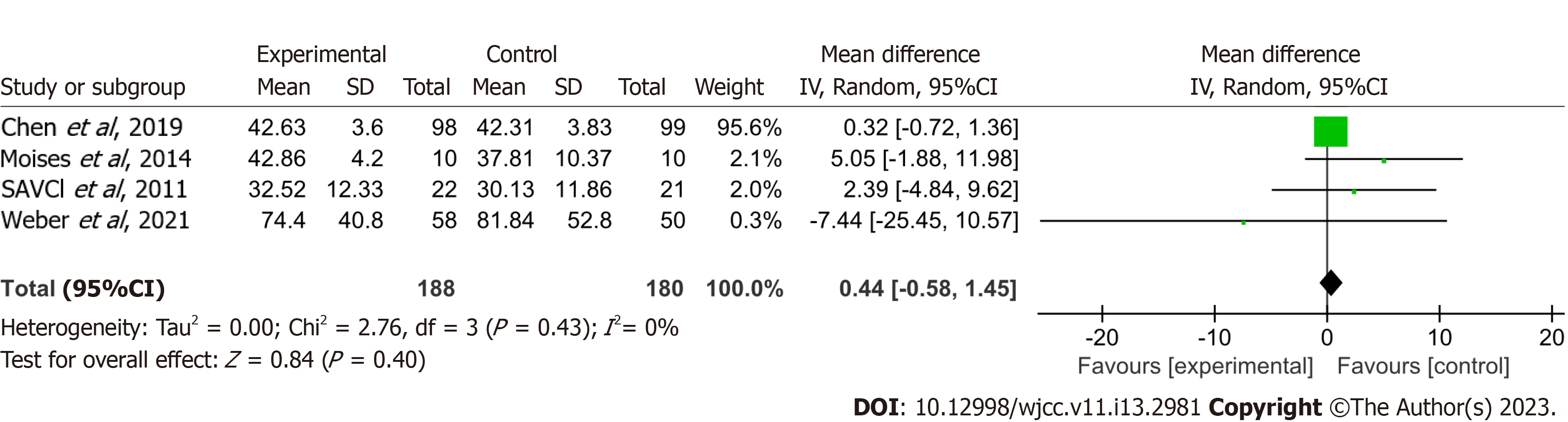
Figure 4 Effect of preoperative inspiratory muscle training on length of intensive care unit stay.
The result indicated a nonsignificant effect on the length of intensive care unit stay with a pooled mean difference of 0.44 h (95%CI: -0.58 to 1.45) and low heterogeneity (I² = 0) in cardiac surgery patients (including transcatheter aortic valve replacement) receiving preoperative inspiratory muscle training. Weight refers to the contribution of each study to the meta-analytic estimate of effect. SD: Standard deviation.
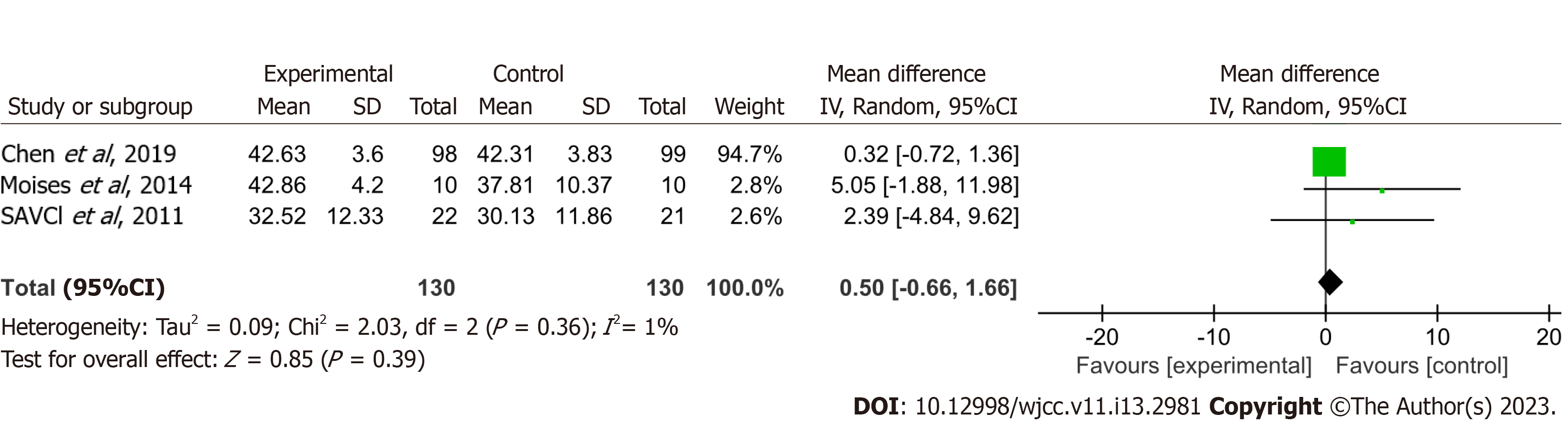
Figure 5 Effect of preoperative inspiratory muscle training on length of intensive care unit stay.
The result indicated a nonsignificant effect on the length of intensive care unit stay with a pooled mean difference of 0.50 h (95%CI: -0.66 to 1.66) and low heterogeneity (I² = 1) in cardiac surgery patients (excluding transcatheter aortic valve replacement) receiving preoperative inspiratory muscle training. SD: Standard deviation.
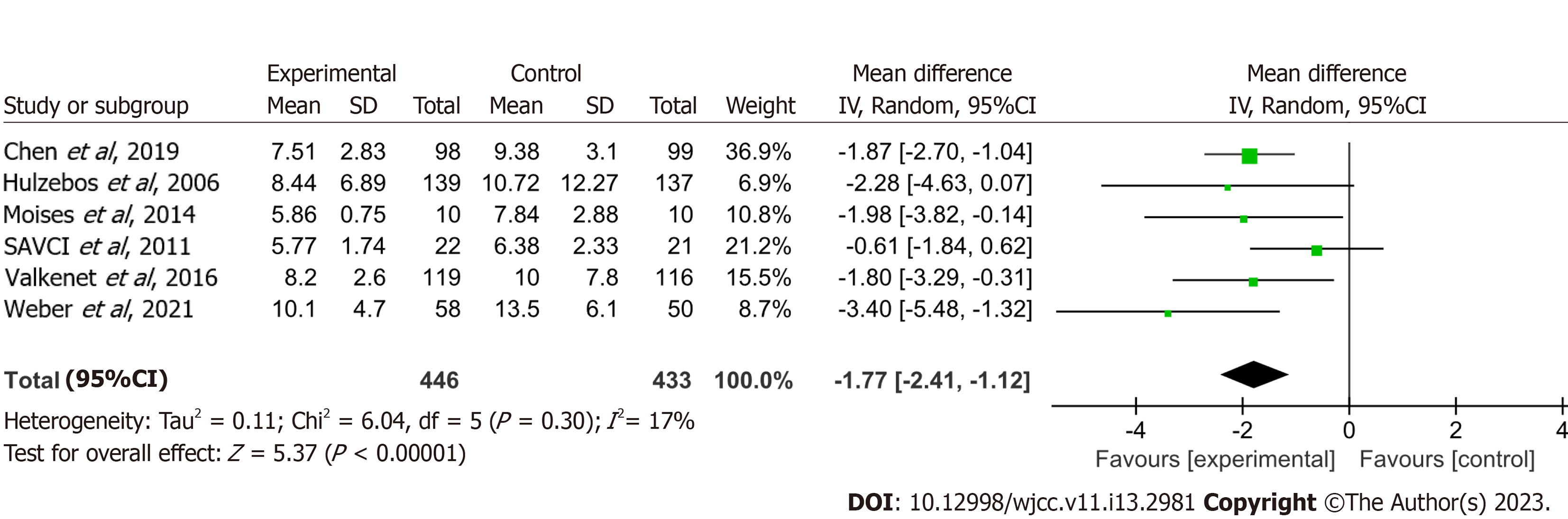
Figure 6 Impact of preoperative inspiratory muscle training on the duration of postoperative hospitalization.
The result indicated a significant positive effect on the duration of postoperative hospitalization with a pooled mean difference of -1.77 d [95%CI: -2.41-(-1.12)] in cardiac surgery patients (including transcatheter aortic valve replacement) receiving preoperative inspiratory muscle training. SD: Standard deviation.
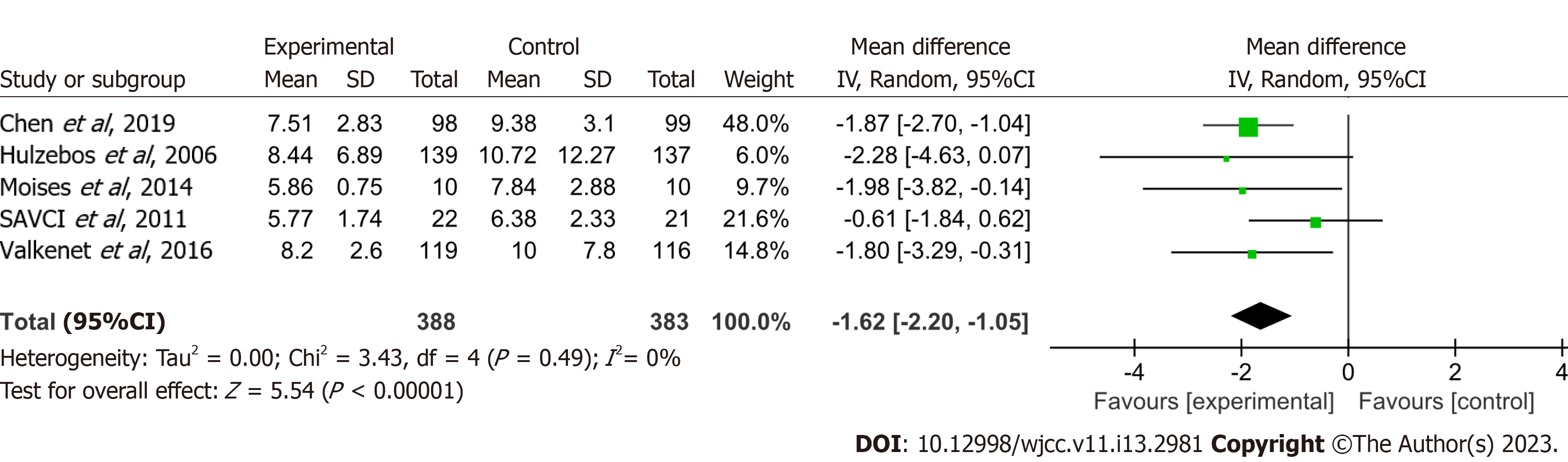
Figure 7 Impact of preoperative inspiratory muscle training on the duration of postoperative hospitalization excluding patients who received transcatheter aortic valve replacement.
The result indicated a significant positive effect on the duration of postoperative hospitalization with a pooled mean difference of -1.62 d [95%CI: -2.20-(-1.05)] in cardiac surgery patients (excluding transcatheter aortic valve replacement) receiving preoperative inspiratory muscle training. SD: Standard deviation.
- Citation: Wang J, Wang YQ, Shi J, Yu PM, Guo YQ. Effect of preoperative inspiratory muscle training on postoperative outcomes in patients undergoing cardiac surgery: A systematic review and meta-analysis. World J Clin Cases 2023; 11(13): 2981-2991
- URL: https://www.wjgnet.com/2307-8960/full/v11/i13/2981.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i13.2981