Copyright
©The Author(s) 2022.
World J Clin Cases. Aug 26, 2022; 10(24): 8742-8748
Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8742
Published online Aug 26, 2022. doi: 10.12998/wjcc.v10.i24.8742
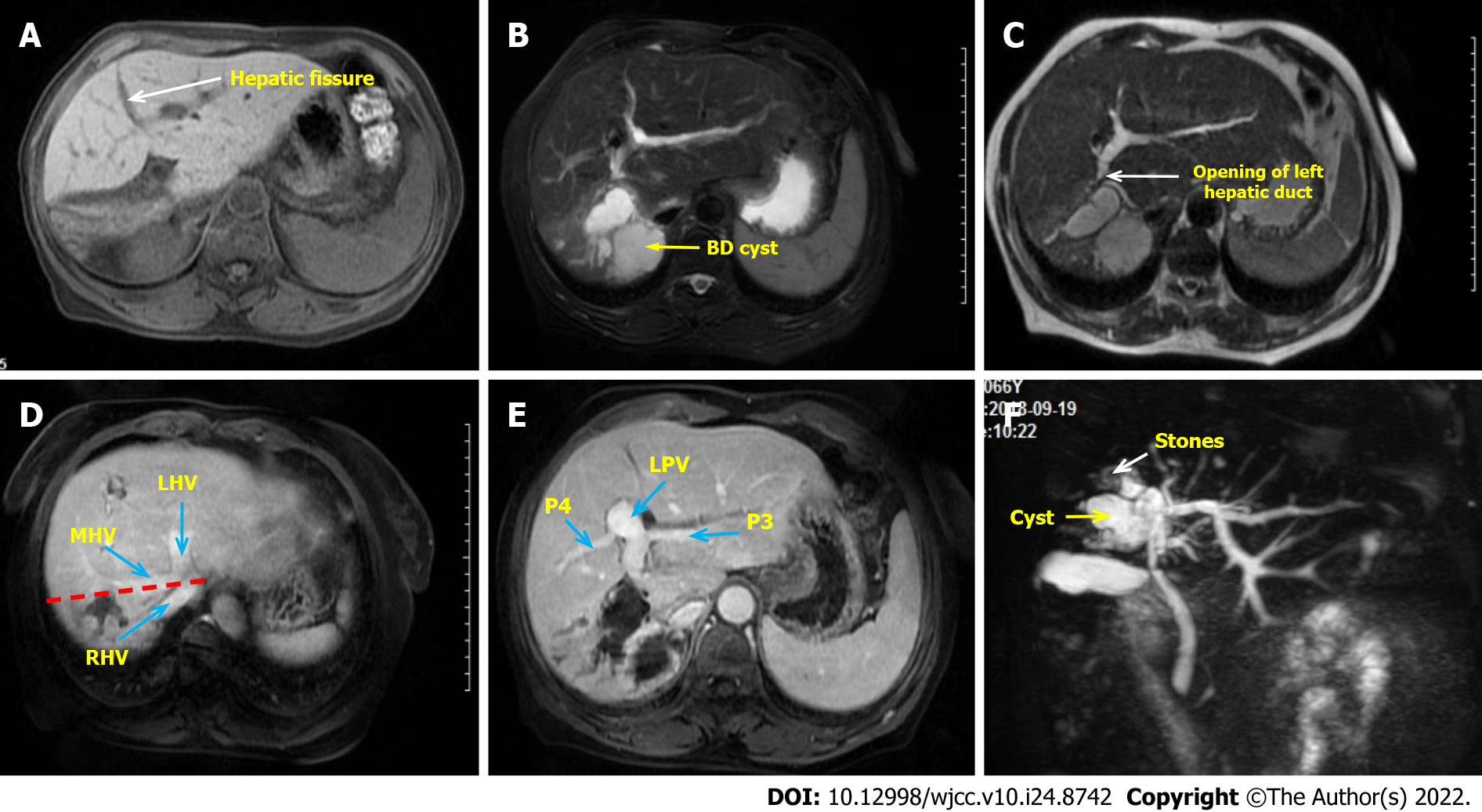
Figure 1 Preoperative clinical image of the abdomen.
A: The right liver atrophy and compensatory hypertrophy of the left liver were seen, with the hepatic fissure (the white arrow) transposed to the right; B: Right hepatic duct cystic dilatation; C: The opening of left hepatic duct (the white arrow) is very close to the cyst; D: The red line shows the expected excision line and the blue arrows show the three major hepatic veins; E: No vascular variation was found and the left portal veins were also transposed to the right; F: Magnetic resonance cholangiopancreatography was used to evaluate intrahepatic and extrahepatic bile ducts. The end of the right hepatic duct is full of stones (the white arrow). LHV: Left hepatic vein; MHV: Middle hepatic vein; P3: Portal vein of Segment 3; P5: Portal vein of Segment 5; RHV: Right hepatic vein.
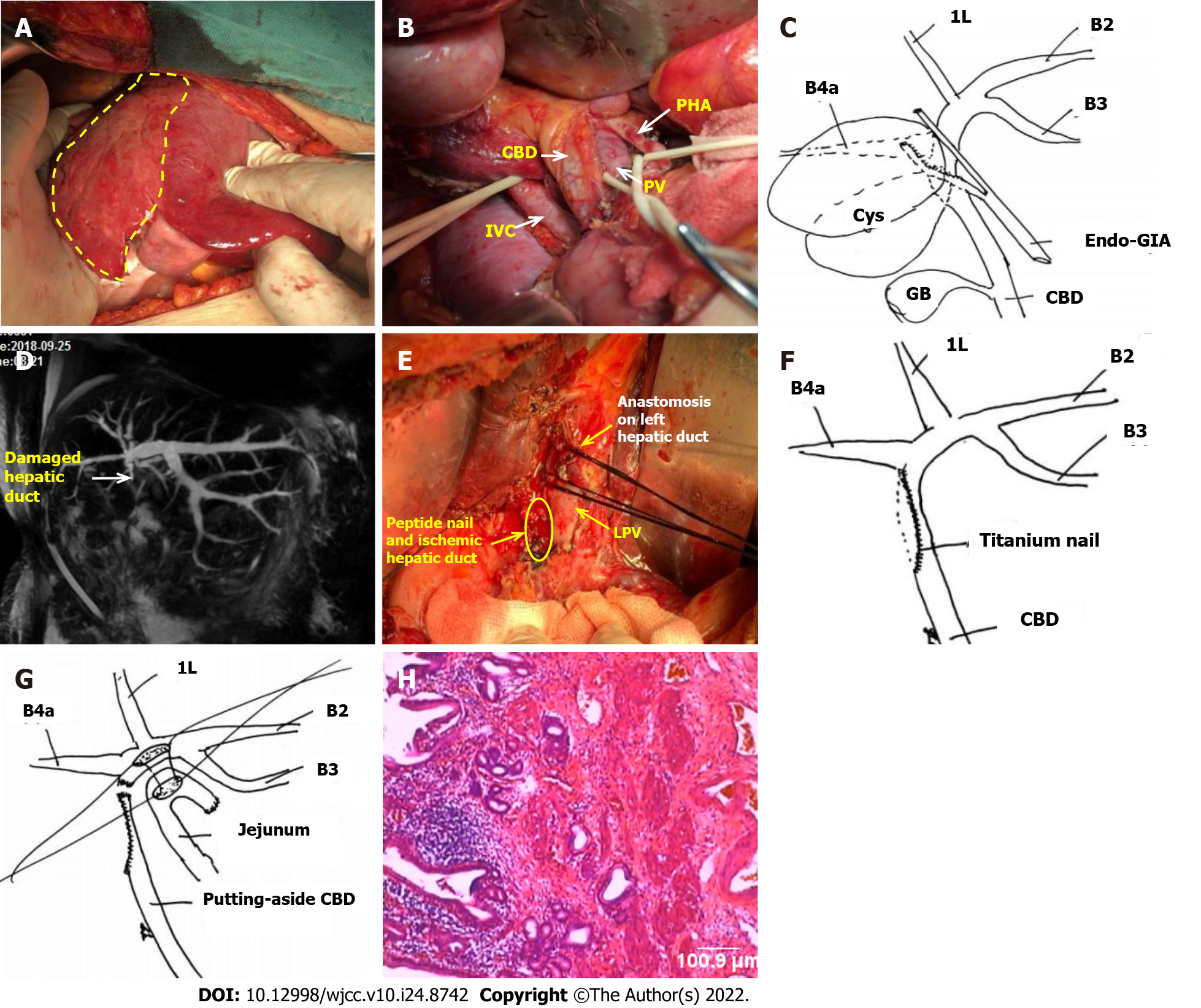
Figure 2 Postoperative clinical images and surgical schematic diagram.
A: The right liver atrophy and left liver hyperplasia were confirmed intraoperatively. The area within the yellow line is the right liver with fibrosis and atrophy; B: The portal vessels were dissected, and there was no variation in extrahepatic vessels; C: The right hepatic duct was transected by endovascular gastrointestinal anastomosis from its origin; D: Postoperative magnetic resonance cholangiopancreatography reexamination showed that the extrahepatic bile duct was not shown; E: Severe ischemia (the yellow area) was found due to titanium nail damage to the lateral wall of the hepatic duct during the reoperation exploration. The anastomosis of the left hepatic duct (the white arrow) was suspended by silk thread; F: Schematic diagram of the causes of bile duct injurie; G: Schematic diagram of the side-by-side anastomosis of the hepatic duct and jejunum; H: Postoperative pathology (× 100) showed chronic inflammation of the bile duct wall, and no malignant cells were found. 1L: Bile duct of Segment 1L; B2: Bile duct of Segment 2; B3: Bile duct of Segment 3; B4a: Bile duct of Segment 4a; CBD: Common bile duct; GB: Gall bladder; IVC: Inferior vena cava; LPV: Left portal vein; PV: Portal vein.
- Citation: Zhao J, Dang YL. When should endovascular gastrointestinal anastomosis transection Glissonean pedicle not be used in hepatectomy? A case report. World J Clin Cases 2022; 10(24): 8742-8748
- URL: https://www.wjgnet.com/2307-8960/full/v10/i24/8742.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i24.8742