Copyright
©The Author(s) 2022.
World J Clin Cases. Aug 6, 2022; 10(22): 8045-8053
Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.8045
Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.8045
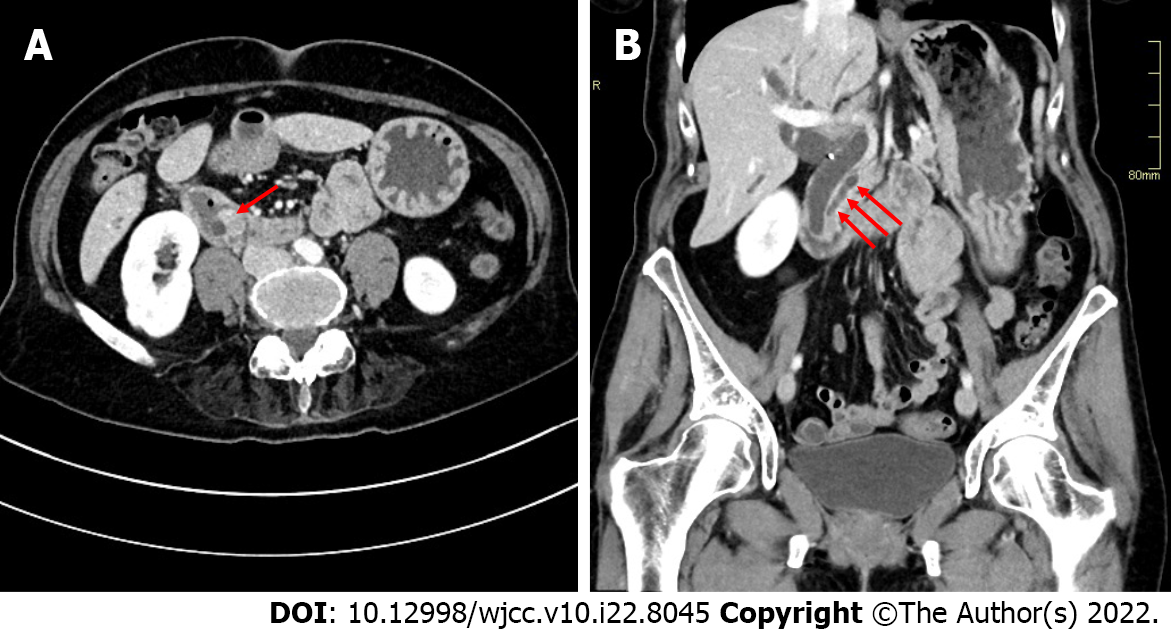
Figure 1 Abdominal computed tomography images.
A: A 1.5 cm contrast enhancing mass was seen in the ampullary region (arrow) together with a dilated main pancreatic duct; B: The mass led to obstruction and upstream dilatation of intra- and extra-hepatic bile ducts and the main pancreatic duct (arrows).
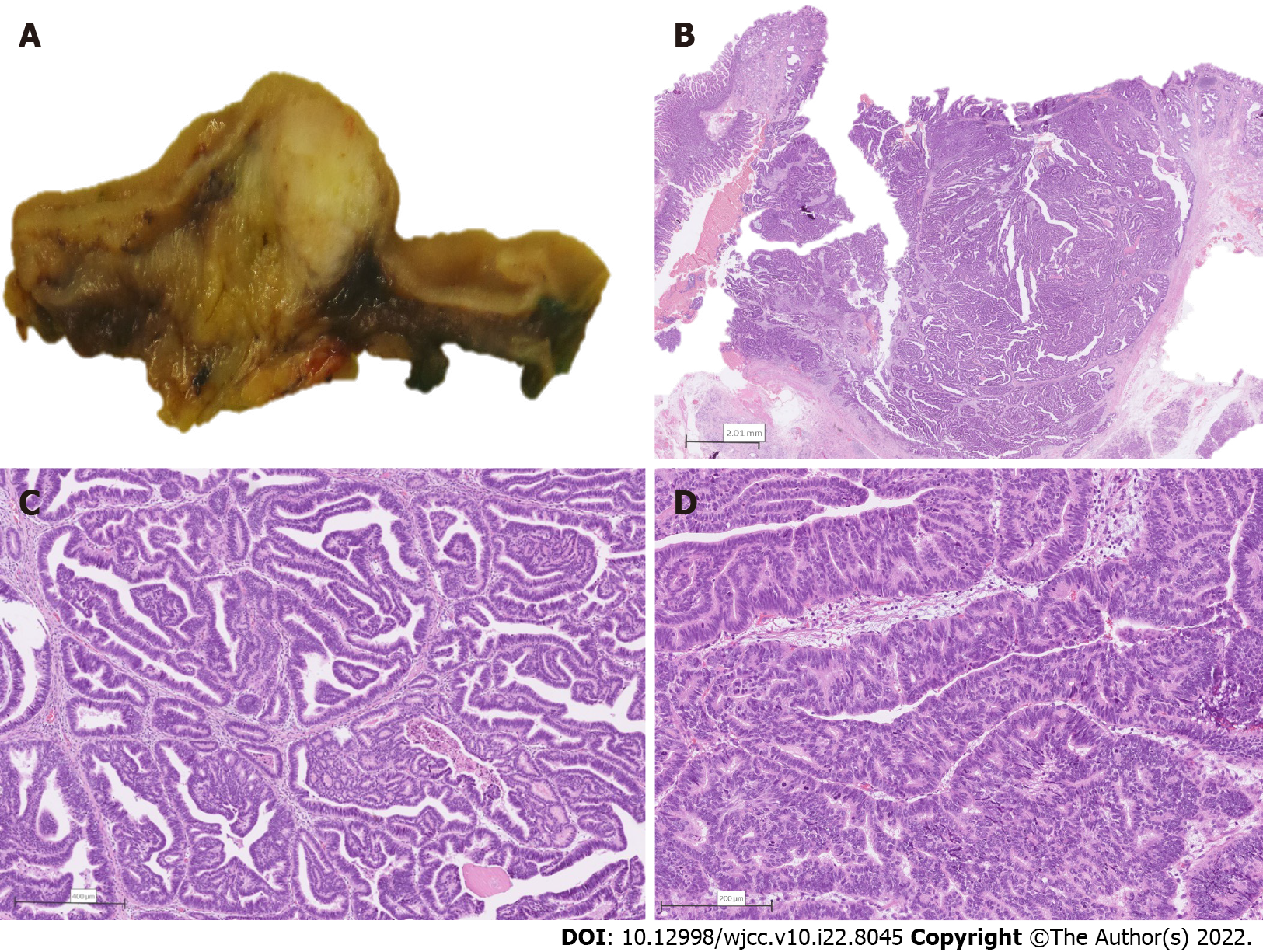
Figure 2 Combined intra-ampullary papillary-tubular neoplasm and neuroendocrine carcinoma.
A: Section through the ampulla of Vater revealing a well-demarcated tumor localized to the area; B: Low power magnification depicting a well-delineated non-invasive tumor composed predominantly of papillary structures; C: Papillary structures are lined by a pseudostratified mildly atypical epithelium; D: Higher magnification revealing areas of high-grade dysplasia.
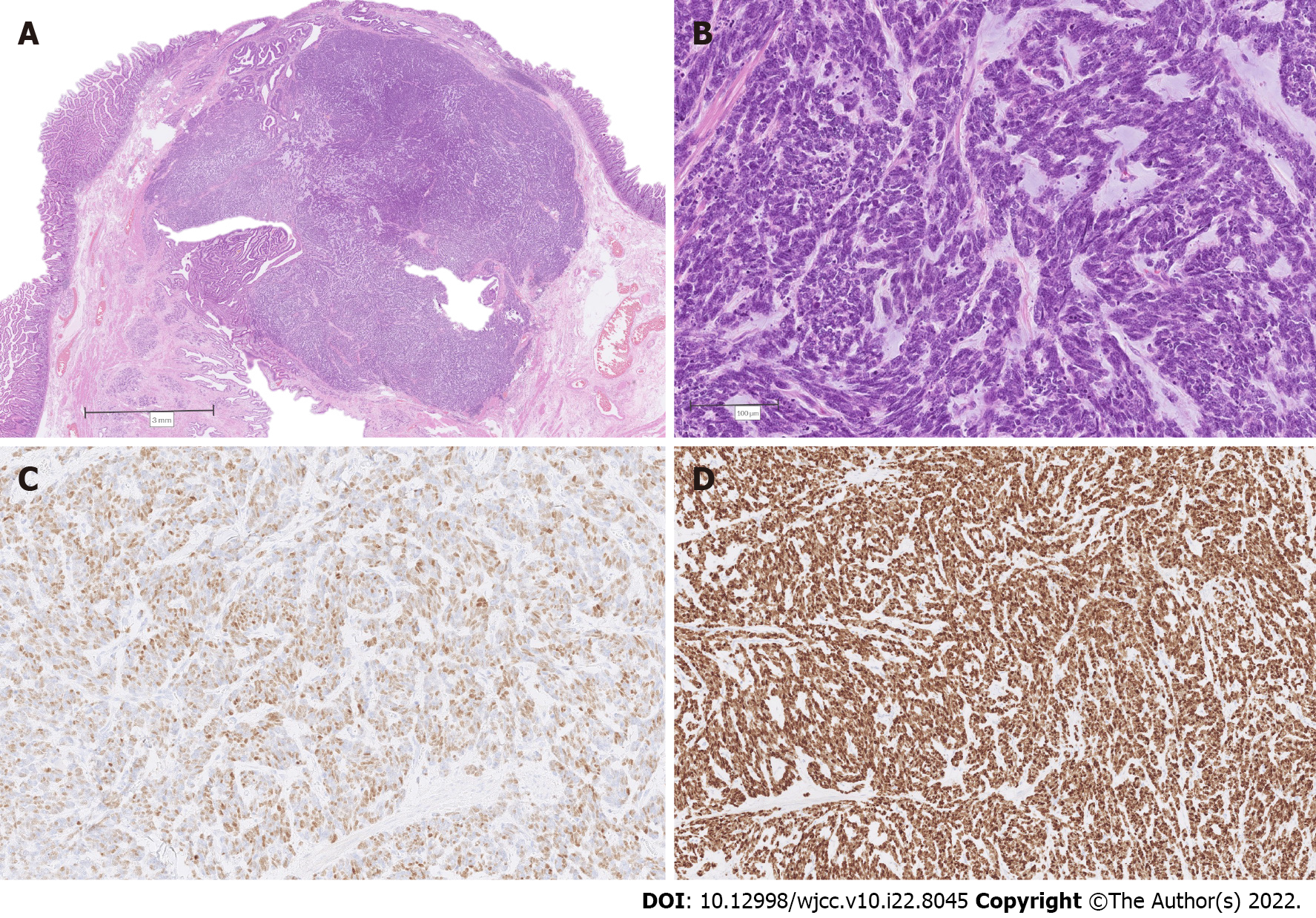
Figure 3 Combined intra-ampullary papillary-tubular neoplasm and neuroendocrine carcinoma.
A: Low power magnification depicting abrupt transition from the papillary tumor (upper and middle left) to solid nodular proliferation (middle and right); B: Higher magnification of the solid component, consistent with poorly differentiated neuroendocrine carcinoma; C: Immunohistochemistry for insulinoma-associated protein 1 depicting diffuse nuclear positivity; D: Immunohistochemistry revealing a 100% Ki-67 index in tumor cells.
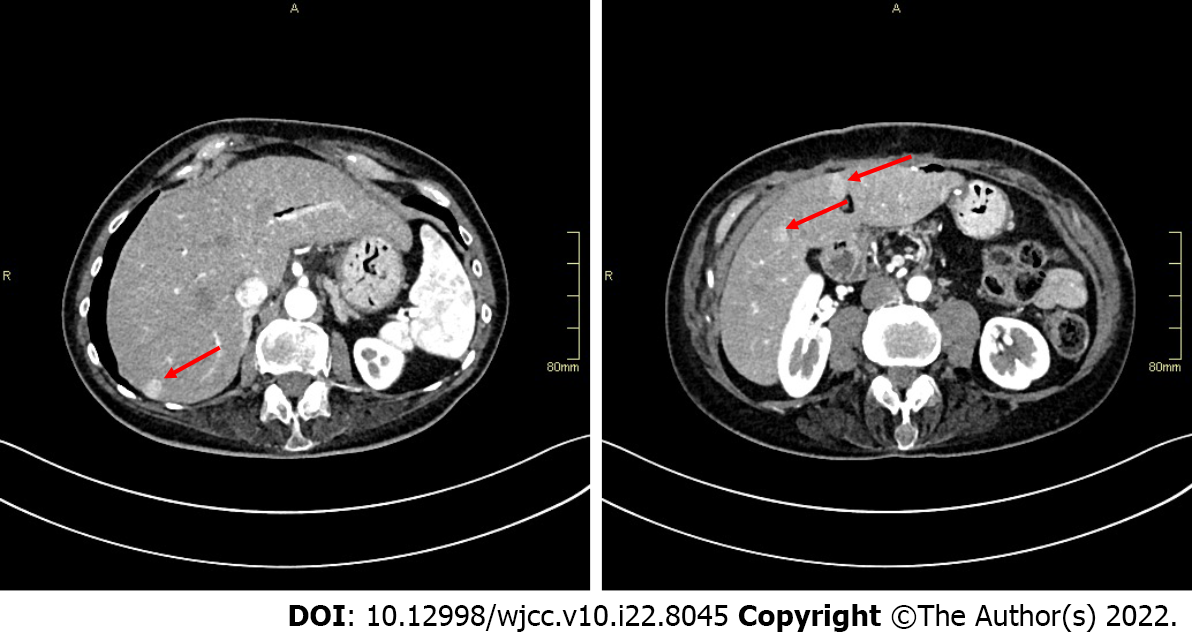
Figure 4 Abdominal computed tomography images revealing several hypervascular liver metastases (arrows).
- Citation: Zavrtanik H, Luzar B, Tomažič A. Intra-ampullary papillary-tubular neoplasm combined with ampullary neuroendocrine carcinoma: A case report. World J Clin Cases 2022; 10(22): 8045-8053
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/8045.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.8045