Published online Feb 15, 2023. doi: 10.4251/wjgo.v15.i2.225
Peer-review started: September 19, 2022
First decision: December 1, 2022
Revised: December 15, 2022
Accepted: January 9, 2023
Article in press: January 9, 2023
Published online: February 15, 2023
Processing time: 148 Days and 15.7 Hours
Colorectal cancer (CRC) is the second deadliest cancer and the third-most common malignancy in the world. Surgery, chemotherapy, and targeted therapy have been widely used to treat CRC, but some patients still develop resistance to these treatments. Ferroptosis is a novel non-apoptotic form of cell death. It is an iron-dependent non-apoptotic cell death characterized by the accumulation of lipid reactive oxygen species and has been suggested to play a role in reversing resistance to anticancer drugs. This review summarizes recent advances in the prognostic role of ferroptosis in CRC and the mechanism of action in CRC.
Core Tip: The prognosis of patients with advanced colorectal cancer is still poor, largely due to resistance to anticancer drugs. Ferroptosis is a novel form of non-apoptotic cell death, mainly characterized by abnormal iron metabolism and the excessive accumulation of lipid peroxidation. Studies have shown that ferroptosis can participate in the process of colorectal cancer (CRC) through the accumulation of lipid peroxides, inhibition of the System Xc−, disruption of the glutathione/glutathione peroxidase 4 balance, imbalance of iron homeostasis, and mediation of the P53 pathway. Induction of ferroptosis can reverse the resistance of anticancer drugs and improve the prognosis of CRC patients.
- Citation: Song YQ, Yan XD, Wang Y, Wang ZZ, Mao XL, Ye LP, Li SW. Role of ferroptosis in colorectal cancer. World J Gastrointest Oncol 2023; 15(2): 225-239
- URL: https://www.wjgnet.com/1948-5204/full/v15/i2/225.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v15.i2.225
Colorectal cancer (CRC) is a common gastrointestinal malignancy and the second-most common cause of cancer death. During the last decade (2010-2019), CRC mortality declined by about 2% per year but increased among those under 50 years old[1]. The oncogenesis and development of CRC involve multiple genes and steps, which is an extremely complex process.
Studies have shown that CRC cells have characteristics of strong proliferation, easy recurrence and easy metastasis[2], but there are few effective therapeutic targets for CRC patients[3]. At present, the comprehensive treatment of CRC includes surgical resection, neoadjuvant chemoradiotherapy, postoperative chemoradiotherapy, targeted therapy, immunotherapy and other methods, but the prognosis of patients with advanced CRC is still poor.
Cell death is a basic life process and can be divided into accidental cell death and regulated cell death (RCD). RCD can be further divided into the category of apoptosis, pyroptosis, necroptosis and ferroptosis[4]. Ferroptosis, first reported in 2012, is a newly defined form of RCD involving iron-dependent, non-apoptotic cell death. The characterization methods included free iron and lipid reactive oxygen species (ROS), particularly lipid hydroperoxides[5], and by cytoplasmic and organelle swelling, chromatin condensation and mitochondrial disorder[6,7]. Studies have shown that the tumor cell survival is highly dependent on an abnormally activated antioxidant system.
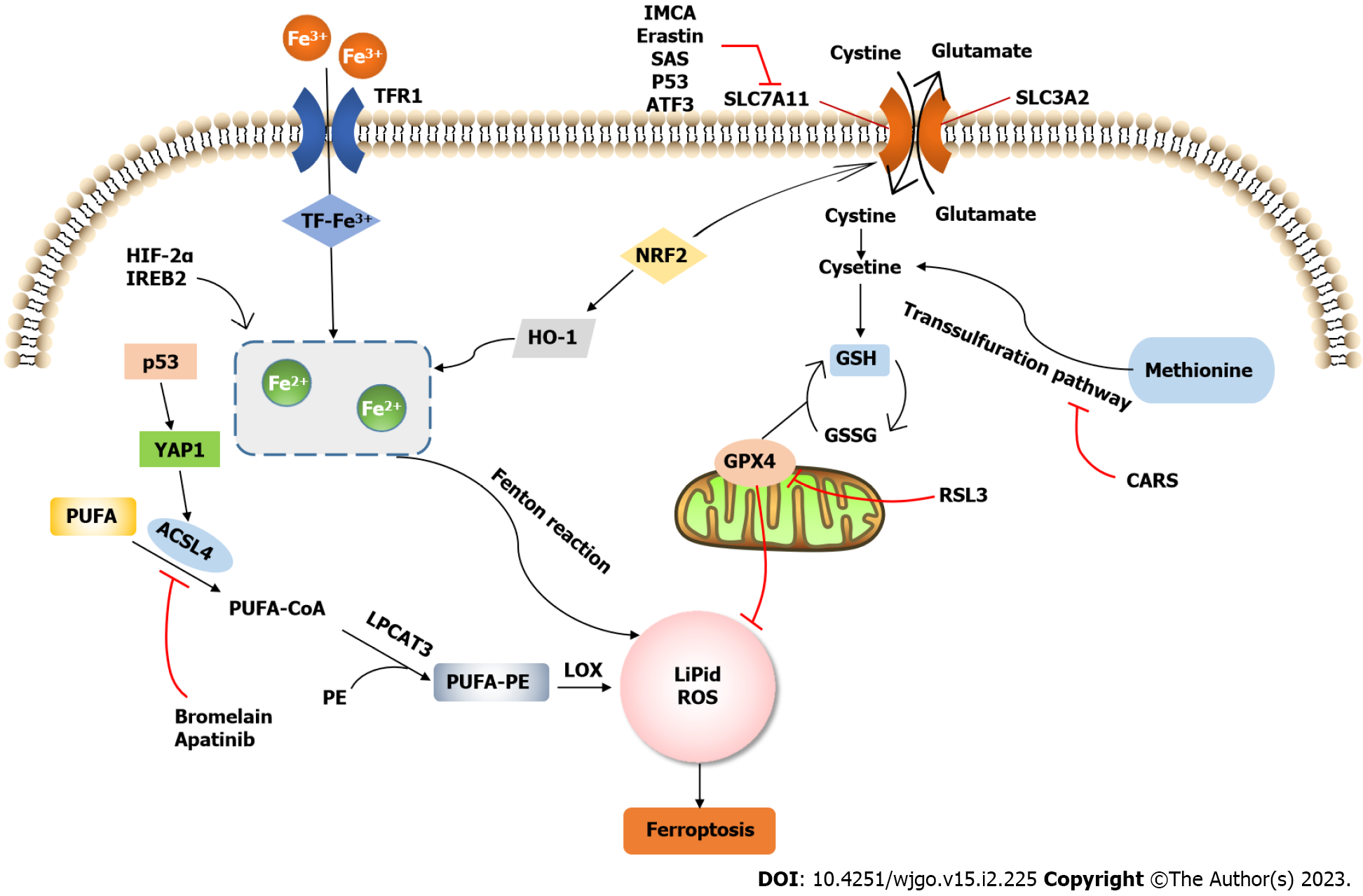
Several therapeutic targets associated with ferroptosis have been identified in CRC (Figure 1). The induction of ferroptosis is also considered a promising research direction in cancer resistance.
Recently, a growing number of studies have shown that genes involved in ferroptosis are associated with the prognosis of CRC patients. CRC has a high recurrence rate and individual heterogeneity, so it is desirable to have good prognostic biomarkers that can be used to predict high-risk patients in order to help patients obtain appropriate treatment.
In an analytical study combining samples from eight CRC patients with the TCGA public database, changes in ferroptosis in CRC patients at various molecular levels, ranging from DNA, RNA and proteins to epigenetic modifications, were described, and four ferroptosis-related genes associated with the prognosis were identified: Cyclin-dependent kinase inhibitor 2A (CDKN2A), glutathione peroxidase 4 (GPX4), arachidonic acid lipoxygenase 3 (ALOXE3) and LINC00336[8]. Another study constructed a clinical prediction model including GPX4, NOX1 and Acyl-CoA synthetase long-chain family member 4 (ACSL4) that effectively reflected the prognosis, tumor progression and asthma control test responsiveness of CRC patients. It is also worth noting that tumors with low ferroptosis scores may infiltrate more CD4+ and CD8+ T cells and fewer M1 macrophages[9]. ALOX5 is considered a key ferroptosis-related gene associated with a poor prognosis in CRC patients, and it regulates ferroptosis in cancer cells through lipid peroxidation[10,11]. CRC patients with an increased NOX1 expression and decreased BRAF status have a higher survival rate than others, and genes positively correlated with NOX1 are also significantly correlated with the CRC survival rate. The mechanism underlying NOX1 and BRAF mutations needs to be further explored[12]. A prognostic model combining genes related to oxidative stress and ferroptosis can distinguish CRC as hot and cold tumors. Patients in the low-risk group responded better to fluorouracil chemotherapy and immune checkpoint blocking therapy than those in the high-risk group[13].
Long non-coding RNA (lncRNA) is non-coding RNA longer than 200 nucleotides and refers to the major class of transcripts encoded by the genome but mostly not translated into proteins[14]. LncRNA plays a key role in regulating cancer proliferation, the cell cycle, metastasis and programmed death[15,16]. The abnormal expression of lncRNA is associated with the risk of CRC, imbuing it with clinical potential as a stratification marker, diagnostic index and therapeutic target of CRC[17-20]. A model containing only four lncRNAs was able to well predict the prognosis, vein invasion and lymphatic metastasis in CRC patients, and it was proven that AP003555.1 and AC005841.1 induced ferroptosis by regulating Erastin[21]. The lncRNA model including AC016027.1, AC099850.3, ELFN1-AS1 and VPS9D1-AS1 was able to accurately predict the prognosis of CRC patients and showed great potential to guide individualized treatment[22]. Cai et al[23] summarized the details of seven ferroptosis-related lncRNAs to predict the prognosis of CRC patients and found that these lncRNAs were mainly enriched in the mitogen-activated protein kinase (MAPK) signaling pathway, mammalian target of rapamycin (mTOR) signaling pathway and glutathione (GSH) metabolism pathway[23]. LINC00239 increased Nrf2 protein stability by inhibiting Nrf2 ubiquitination and decreased the antitumor activity of erastin and Ras-selective lethal 3 (RSL3)[24]. Circular RNA also plays an important role in ferroptosis. CircABCB10 serves as a sponge of Mir-326 and eventually regulates ferroptosis of CRC by regulating CCL5[25].
In addition to being an independent clinical prognostic factor for CRC patients, genes associated with ferroptosis can also accurately predict the clinical status, including tumor occurrence and progression, drug resistance, somatic mutations and the immune function[26,27], which provides a new research direction for targeted therapy or immunotherapy.
The process of lipid peroxide accumulation in cells is the crucial section of ferroptosis. Polyunsaturated fatty acids (PUFAs) containing diallyl matrigel are prone to hydrogen deprivation, causing the formation of lipid peroxides and inducing ferroptosis[28]. When PUFAs are replaced by monounsaturated fatty acids (MUFAs) in the plasma membrane, lipid ROS accumulation is hindered, and ferroptosis is prevented[29]. With the process of esterification into membrane phospholipids and oxidation into ferroptosis signals, free PUFAs then can be joined into the lipid signaling mediator syntheses[30]. Several studies have shown that phosphatidylethanolamines, a key phospholipid containing arachidonic acid (AA) or its derivative epinephrine (AdA), are oxidized to oxophosphatidylethanolamines to induce ferroptosis[31]. Elongation of very-long-chain fatty acid protein 5 (ELOVL5) and fatty acid desaturase 1 are can participate in AA and AdA synthesis, which can effectively inhibit ferroptosis[32]. Furthermore, regulatory enzymes involved in membrane phospholipid biosynthesis of PUFAs, such as ACSL4[33] and lysophosphatidylcholine acyltransferase 3 (LPCAT3)[34], can also trigger or prevent ferroptosis. However, the effect of LPCAT3 on ferroptosis was mild compared to that of ASCL4[34].
Bromelain, a pineapple stem extract, potently induces cell ferroptosis and inhibits the proliferation of Kras mutant CRC in Kras mutant cell lines by regulating ACSL-4 Levels compared to Kras wild-type cells[35]. The behavers of Emodin, inhibiting ACSL4 expression, which can inhibit the proliferation and invasion of CRC, bring new research directions for CRC[36].
Apatinib, also known as YN968D1, as a third-line therapy can effectively improve the prognosis of patients with metastatic CRC[37]. ELOVL6 is a target of apatinib. By orienting the ELOVL6, Apatinib can promote ferroptosis with result of ACSL4 regulation, which has been verified by a co-IP assay. This suggests that apatinib inhibits CRC cell viability, at least in part, by targeting ELOVL6/ACSL4 signaling, thus providing novel mechanistic support for the use of apatinib in the clinical treatment of CRC patients[38].
GSH has been known as a crucial antioxidant. It can bind toxic molecules, such as free radicals and heavy metals, and convert them into harmless substances that are excreted[39]. GSH is also the first line of defense in the body to scavenge free radicals, which can effectively inhibit ferroptosis, and has a strong protective effect on the body[40]. System Xc− is a heterodimer, which was constructed by a heavy-chain subunit and a light-chain subunit (SLC7A11) that assists in the transmembrane transport of cystine and glutamate. Upon entry into the cell, cystine is reduced to cysteine[41], and together with cysteine and glycine, GSH is synthesized intracellularly. Therefore, System Xc− plays an important role in maintaining GSH homeostasis.
Studies have suggested that System Xc− may mediate ferroptosis by affecting the glutamate uptake and GSH synthesis[42,43]. Erastin and sulfasalazine are inhibitors of System Xc- that can lead to intracellular GSH deficiency and ferroptosis by affecting intracellular GSH homeostasis[44,45]. By regulating the expression of SLC7A11, a functional subunit of Xc−, it can affect the activity of System Xc− and the susceptibility to ferroptosis in cancer cells[46-48].
Knockdown of SLC7A11 attenuates the viability of CRC stem cells by increasing ROS levels and decreasing cysteine and GSH levels[49]. Talaroconvolutin A is a natural product, and studies have shown that, in addition to inducing ferroptosis by increasing ROS levels in cancer cells, this compound can also promote ferroptosis by down-regulating the SLC7A11 expression and up-regulating the ALOXE3 expression, becoming a new potentially powerful drug candidate for CRC therapy[50]. Copper overload mediated by the copper chelator elesclomol inhibits CRC both in vitro and in vivo, and one of its pathways may induce ferroptosis by promoting the degradation of SLC7A11[51].
The benzopyran derivative 2-imino-6-methoxy-2H-chromene-3-carbothioamide (IMCA) is considered to significantly inhibit the viability of CRC cells. IMCA can downregulate the expression of SLC7A11 and reduce cysteine and GSH glycine content, which leads to the accumulation of ROS and ferroptosis. In contrast, the overexpression of SLC7A11 was shown to attenuate ferroptosis induced by IMCA, which was confirmed to be involved in the activated protein kinase/mTOR/p70S6k signaling pathway[52].
Petunidin 3-O-[rhamnopyranosyl-(trans-p-coumaroyl)]-5-O-(β-D-glucopyranoside) is a flavonoid compound. CRC cell proliferation can be inhibited by down-regulating SLC7A11 to reduce ferroptosis[53].
Resveratrol (RSV) has been shown to promote ferroptosis by down-regulating the expression of SLC7A11 and GPX4. Combined with bionic nanocarriers, RSV's therapeutic potential as ferroptosis inducing anticancer agent has been developed. The bionic nanomaterial coated the RSV-supported poly (ε-caprolactone) poly (ethylene glycol) nanoparticles on the erythrocyte membrane to improve the transmission efficiency of RSV[54].
Several ferroptosis-related genes are concentrated on System Xc−. Activating transcription factor 3 (ATF3) promotes ferroptosis by inhibiting System Xc−[55]. Deficiency of CDKN2A and growth differentiation factor 15 downregulates SLC7A11 expression, thereby sensitizing cells to ferroptosis[56,57].
Radiotherapy and poly-ADP-ribose polymerase inhibitors have been used in clinical trials in the treatment of CRC, the mechanism of which may be ionizing radiation activation of dsDNA that modulates ferroptosis through activation of the ATF3-SLC7A11 pathway. Triggers cGAS signaling mediated tumor control in cancer cell lines and mouse xenograft models[58].
More than 40% of the source of cysteine came from diet, and transfer to GSH via a biochemical process in body, which can combat the excessive deposition of peroxide. In addition to being transported into cells by System Xc−, cysteine can also be converted intracellularly by methionine via the transsulfuration pathway[59].
Cystathionine-β-synthase (CBS), an enzymatic component of the transsulfuration pathway, is significantly increased in cells resistant to Erastin-induced ferroptosis[60]. CBS has also been shown to be an independent regulator of ferroptosis[61,62]. Endogenous H2S, a by-product of the transsulfuration pathway, is closely related to tumor cell physiology and is finely regulated in a variety of cancers[63,64]. Xc(-) transporter-related protein (xCT), a functional subunit of system Xc−, was shown to interfere with xCT in colon cancer cells, resulting in an increased expression of cystathionine-γ-lyase and CBS, which are majority of the transsulfuration pathway. Additionally, the endogenous H2S levels can be significantly decreased by interfering with xCT. The correlation of xCT and transsulfuration pathway has been investigated that is a makeable metabolic vulnerability.
Cysteinyl-tRNA synthetase, a genetic suppressor of ferroptosis, upturns the sulfur pathway and re-sensitizes cells to erastin, demonstrating a new mechanism for resistance to ferroptosis[65]. This implies that the transsulfuration pathway is a regulator of ferroptosis resistance.
Zinc oxide has outstanding desulfurization ability, and VZnO can effectively reduce the content of H2S in CRC, effectively deplete GSH in tumor cells and ultimately lead to ferroptosis in CRC cells, providing an effective strategy for CRC treatment[66].
ROS levels in the body are regulated by the antioxidant defense system, and oxidant/antioxidant imbalance may also contribute to ferroptosis[67]. GPX4 is an important selenoprotein that belongs to the GPX antioxidant defense system and is a considerable enzyme to balance the concentration of GSH and GS-SG. GPX4 protects membrane lipid bilayers by transferring toxic lipid hydroperoxides to nontoxic lipid alcohols[68]. GPX4 has been literately proved as a factor of ferroptosis promotor and can be trigger by ferroptosis inducers, such as Erastin and RSL3. Likewise, direct knockdown of GPX4 Leading to the excessive accumulation of intracellular lipid peroxidation and cell death[69]. Thus, GPX4 is consider as a crucial target to trigger ferroptosis[70,71].
In experiments with three different CRC cells (HCT116, LoVo and HT29), RSL3 was found to trigger cellular ferroptosis in a dose- and time-dependent manner due to increased ROS levels and destabilization of the intracellular iron pool. In a further analysis, GPX4 inhibition was proven to be a key determinant of RSL3-induced ferroptosis, and overexpression of GPX4 rescued RSL3-induced ferroptosis[72]. Aspirin has been reported to have therapeutic benefits for CRC carrying carcinogenic PIK3CA. The mechanism may be that aspirin inhibits protein kinase B/mTOR signaling. The expression of downstream sterol regulatory elm-binding protein 1 was inhibited, and the production of MUFA fat by stearoyl-CoA desaturase-1 was reduced. Thus promoting RSL3-induced ferroptosis in CRC cells[73].
Serine- and arginine-rich splicing factor 9 (SRSF9) is frequently overexpressed in multiple tumor types and manifests as a proto-oncogene[74-76]. SFRS9 upregulates GPX4 protein, which is an obstacle to ferroptosis[77]. Knockdown of SFRS9 may be an effective treatment for CRC. In CRC tissues, the expression of SFRS9 mRNA and protein was significantly higher than that in adjacent tissues. Experiments in mice demonstrate that regulation of GPX4 by SRSF9 is an important mechanism driving CRC tumorigenesis and resistance to Erastin-induced ferroptosis. This molecular mechanism may provide a novel approach to improving the sensitivity of CRC to Erastin[78].
ACADSB is a member of the Acyl-CoA dehydrogenase family, and its overexpression inhibits the migration, invasion and proliferation of CRC cells. Studies have shown that ACADSB negatively regulates the expression of GSH reductase and GPX4 while increasing the concentrations of malondialdehyde, Fe ions and superoxide dismutase. This suggests that ACADSB may affect CRC cell migration, invasion and proliferation by regulating CRC cell ferroptosis[79].
Antioxidant proteins, such as Nrf2, are major antioxidant transcription factors that help prevent the accumulation of excess ROS and maintain redox homeostasis. Downregulation of Nrf2 enhances the sensitivity of cancer cells to ferroptosis promoters[80].
The Warburg effect is thought to be a characteristic of cancer cells, that is, cancer cells will undergo glycolysis beyond very high levels under aerobic conditions[81]. Inhibition of the Warburg effect reduces the ability of cells to proliferate. Therefore, inhibiting the Warburg effect may be a therapeutic strategy for cancer. In vivo and in vitro experiments in CRC showed that iron-induced ROS activated the expression of Nrf2 in the nucleus has the positive correlation with Warbury enzymes expression and CRC cell proliferation by enhancing the Warburg effect.
Heme oxygenase 1 (HO-1) is a downstream gene of Nrf2, and NGF2 protects against lipid peroxidation[80] and ferroptosis through the transcription of enzymes such as HO-1[82]. Ferroptosis can be effectively alleviated by the elimination of lipid oxidation through the Nrf2/HO-1 axis activation[83,84].
Tagitin C, a sesquiterpene lactone[85], can induce ferroptosis in HCT116 cells and inhibit the growth of CRC cells. Mechanistically, Tagitinin C induces endoplasmic reticulum stress and oxidative stress as well as nuclear translocation of Nrf2. As a downstream gene of Nrf2, HO-1 was significantly increased with Tagitinin C treatment[86].
Tagitinin C-induced ferroptosis was accompanied by a decrease in GSH levels and an increase in lipid peroxidation. Cetuximab combined with chemotherapy has made great progress in the treatment of metastatic CRC[87], but cetuximab is not effective in CRC patients with KRAS mutations[88,89].
Lysionotin (Lys), a flavonoid, has been demonstrated to successfully inhibit cell proliferation, migration and invasion of HCT116 and SW480 CRC cells in vitro. Lys treatment worked by increasing Nrf2 cells’ degradation rate to reduce the concentration of Nrf2 protein, inducing ferroptosis and ROS accumulation in CRC cells[90].
P38 MAPK has been investigated that participate in the regulation of Nrf2/HO-1[91,92]. It has been shown that cetuximab can significantly inhibit Nrf2/HO-1 signaling through p38 MAPK activation in KRAS-mutant CRC cell lines, thereby promoting RSL3-induced ferroptosis. This provides a research direction for cetuximab in the treatment of KRAS-mutant CRC[93].
Oxaliplatin is the first-line chemotherapy drug for CRC. By inhibiting the Nrf2 signaling pathway, the sensitivity of CRC cells to oxaliplatin can be enhanced[94,95]. Furthermore, the study found that oxaliplatin significantly inhibited the protein expression of Nrf2, HO-1 and NQ in the Nrf2 signaling pathway in a dose-dependent manner. Therefore, the anticancer effect of oxaliplatin may be enhanced by inhibiting the Nrf2 signaling pathway, leading to ferroptosis and oxidative stress in CRC cells[96].
The primary condition for the initiation of ferroptosis pathway is the need of iron ion. Dietary iron is absorbed primarily in the gut as ferric ion and delivered to the blood by transferrin (TF). In general, extracellular iron transport into the cell through the sequence of complexing with circulating TF, then binds to membrane TF receptor proten-1 (TFR1), finally to the cytoplasmic unstable iron pool. Excess cellular iron is stored as ferritin or transported extracellularly by ferritin[97,98]. Maintenance of cellular iron homeostasis prevents oxidative damage, cytotoxicity and death.
Lipid reactions can be divided into enzymatic and non-enzymatic reactions. Iron can promote the production of ROS through the Fenton reaction, leading to enzymatic lipid peroxidation[99,100], and also acts in a non-enzymatic manner as a cofactor for lipid-oxidizing lipoxygenase. Supplementation of exogenous iron ions can accelerate erastin-induced ferroptosis[5]. Knockout the gene encoding the TFR or upregulate the expression of iron storage proteins can inhibit iron overload and ferroptosis. Iron metabolism can be regulated by inhibition of the major transcription factors, like iron regulatory protein 2, significantly upregulates the expression of iron metabolism-related genes, such as FTH1 and FTL, thereby inhibiting erastin-induced ferroptosis[101]. Iron chelators can prevent the transfer of electrons from iron to oxides, thus inhibiting the production of oxygen free radicals and inhibiting lipid peroxidation to prevent ferroptosis. Therefore, the regulation of iron metabolism and ferritin phagocytosis may become new targets and new pathways for regulating ferroptosis.
Hypoxia-inducible factor-2α (HIF-2α) is a master transcriptional regulator of cellular iron levels[102]. Activation of HIF-2α increases cellular iron in CRC, leading to an increase in lipid ROS and a decrease in GSH production, thus enhancing cellular sensitivity to ferroptosis[103].
There is a conserved miR-545 binding site in the 3' untranslated region of TF, and the overexpression of TF in CRC cells was found to induce increased levels of ROS, MDA and Fe2+, thereby promoting CRC cell death. This suggests that miR-545 may play an oncogenic role in CRC by regulating the iron accumulation in cells[104].
Dichloroacetate attenuates the stemness of CRC cells by chelating iron in lysosomes, leading to the up-regulation of iron concentrations and lipid peroxide levels, thus triggering ferroptosis[105].
OTUD1 is a deubiquitinase of iron-responsive element-binding protein 2 (IREB2), which is mainly expressed in intestinal epithelial cells. OTUD1 promotes TFR1-mediated iron transport through deubiquitination and stabilization of IREB2, leading to increased ROS production and ferroptosis, which is highly associated with a poor prognosis in CRC[106].
The tumor suppressor gene p53 plays a dual role in mediating ferroptosis in a variety of cancers[99]. Studies have found that p53 can enhance ROS-mediated ferroptosis by inhibiting SLC7A11 protein expression, resulting in decreased cystine import and thus reduced GSH production[46,107]. However, unlike in CRC, p53 can protect CRC cells from ferroptosis by stirring SLC7A11[108]. In addition, p53 can also inhibit CRC cell ferroptosis by blocking dipeptidyl peptidase 4 activity[97,109].
Cytoglobin (CYGB) is a regulator of ROS that plays an important role in oxygen homeostasis and acts as a tumor suppressor[110]. Yes-associated protein 1 (YAP1) is a key downstream target of CYGB. CYGB modulates cellular ferroptosis through p53-YAP1 signaling in CRC cells[111]. A novel antitumor compound optimized from the natural saponin biocide A has also been shown to trigger ferroptosis by activating p53[112].
Ginsenoside Rh4 can increase ROS accumulation, lead to the activation of ROS/p53 signaling pathway, and induce ferroptosis to inhibit the proliferation of cancer cells[113]. Cullin-9 can bind p53 to ubiquitinized heteroribo nucleoprotein C for degradation through whole genome sequencing and external differential expression analysis. Cullin-9 overexpression increases resistance to erastin-induced ferroptosis and is a novel and important regulator of CRC ferroptosis[114].
Oxaliplatin prolongs the median disease-free survival and overall survival in patients with advanced CRC, but clinical data suggest that < 40% of patients with advanced CRC benefit from it[115,116]. This may be related to oxaliplatin resistance, and recent studies have shown that induction of ferroptosis can significantly reverse oxaliplatin resistance in CRC cells.
Ferroptosis in CRC cells may be inhibited through the KIF20A/NUAK1/PP1β/GPX4 pathway, which may underlie CRC resistance to oxaliplatin[117]. Deletion of cysteine desulfurase (NFS1) can significantly enhance the sensitivity of CRC cells to oxaliplatin. The mechanism may involve NFS1 deficiency synergizing with oxaliplatin to induce PANoptosis (apoptosis, necroptosis, pyroptosis and ferroptosis), thus increasing the intracellular ROS levels. This also demonstrated that ferroptosis is involved in the oxaliplatin resistance pathway[118]. Obesity is strongly associated with a poor prognosis in patients with advanced CRC, and adipose-derived exosomes reduce susceptibility to ferroptosis in CRC, thereby promoting chemoresistance to oxaliplatin[119].
Combination with chemotherapy with monoclonal antibodies against anti-epidermal growth factor receptor or vascular endothelial growth factor has advanced in the treatment of metastatic CRC. However, inherent resistance to downstream KRAS mutations, so the effect of combination chemotherapy is often less optimistic. β-elemene has broad-spectrum anticancer effects, and it has been demonstrated that combined treatment of β-elemene and cetuximab can induce ferroptosis and inhibit epithelial-mesenchymal transition, thereby improving resistance to KRAS-mutated CRC cells[120].
FAM98A is a microtubule-associated protein involved in cell proliferation and migration. Increased expression of FAM98A can inhibit ferroptosis and promote CRC resistance to 5-fluorouracil (5-FU)[121]. Similarly, PYCR is an oncogene that desensitizes CRC cells to 5-FU cytotoxicity by promoting ferroptosis in CRC cells[122].
In addition, Andrographis Paniculata may also exert a sensitizing effect on CRC treatment by activating ferroptosis[123,124]. Andrographis Paniculata-mediated sensitivity to 5-FU-based chemotherapy in CRC is primarily mediated through activation of ferroptosis and inhibition of the β-catenin/Wnt signaling pathway[123].
Although increasing iron concentration promotes ferroptosis in tumor cells has been demonstrated experimentally, direct administration of Fe2+ is not feasible in the clinic due to the protective effect of cell membranes and the defense mechanism of the tumor immune microenvironment (TME). Nano-drug delivery system (nano-DDSs) has unique physical and chemical properties of nanomaterials, which can not only enhance drug solubility and improve drug circulation time in the body, but also achieve targeted delivery and controlled release of drugs[125]. Therefore, the use of novel nanodelivery systems to improve the efficiency of iron release has great prospects in CRC targeted therapy.
Nano DDS can directly drive the death of iron in tumor cells, and iron-based nanoparticles can be catabolized by acid lysosomes of tumor cells to release Fe2+ and iron 3+[126]. Iron-based nanoparticles induce ferroptosis by catalyzing the Fenton reaction, but because of their low reactive oxygen production, they are often used in conjunction with other treatments. Liang et al[127] synthesized ultra-small single crystal Fe nanoparticles (bcc-USINPs) that are highly active in the tumor microenvironment and can effectively induce tumor cell ferroptosis and immunogenetic cell death at very low concentrations[127].
In addition to acting directly on cancer cells, nanotechnology also works by acting on key components of TME. Due to TME's weak acidity, abundant angiogenesis and hypoxia conditions, the effectiveness of conventional cytotoxic therapy delivery is limited, while active targeting of nanoparticles may be more useful[128].
Sodium persulfate (NaSO) is a novel chemodynamic therapy (CDT) that can produce •SO and Na, which can cause ferroptosis in cells. Ir780-iodide (IR780) is a phototherapy agent that produces ROS in conjunction with NaSO's CDT to overcome CRC chemotherapeutic resistance. Co-assembly of NaSO and IR780 on the nano platform improved the stability of NaSO and solubility of IR780, significantly enhancing the anti-tumor effect on CRC cell lines[129]. A novel composite nanomaterial PPy@Fe3O4 has been demonstrated to regulate the nuclear factor-kappaB signaling pathway and then then inhibit the proliferation, migration and invasion of CRC cells in vitro. Interestingly, Fer-1, an ferroptosis inhibitor, reversed changes in transfer-related proteins induced by nanoparticle therapy[130].
Ferroptosis, a newly discovered type of RCD mediated by iron-dependent lipid ROS accumulation, plays a role in a variety of diseases of the gastrointestinal tract. Many ferroptosis-related genes have been confirmed to be associated with the prognosis of CRC, and various models have been confirmed to be able to stratify CRC patients well and facilitate the early identification of high-risk patients. Iron metabolism and the accumulation of lipid peroxides are the core processes in ferroptosis. As mentioned above, GPX4, SLC7A11, ACSL4 and p53 act as key regulators in ferroptosis-related CRC mediation (Table 1). Induction of ferroptosis can reverse the resistance of anticancer drugs or exert a synergistic effect with other anticancer drugs to enhance the sensitivity of antitumor drugs and improve the prognosis of CRC patients. Furthermore, in colon cancer, copper chelators have also been shown to facilitate CRC cell death by promoting the degradation of SLC7A11. The mechanism underlying ferroptosis and the relationship between key regulators and other RCDs, such as autophagy and apoptosis, should be explored in future research.
| Target | Ferroptosis inducers | Ref. |
| ACSL4 | Bromelain | [35] |
| Apatinib | [37] | |
| Emodin | [36] | |
| SLC7A11 | Erastin | [42] |
| SAS | [44,45] | |
| Talaroconvolutin A | [50] | |
| Copper chelator elesclomol | [51] | |
| IMCA | [52] | |
| Pt3R5G | [53] | |
| RSV | [54] | |
| Transsulfuration pathway | CARS | [65] |
| VZnO | [66] | |
| GPX4 | Erastin | [67] |
| RSL3 | [67] | |
| ACADSB | [79] | |
| Nrf2/HO-1 | Cetuximab | [87] |
| Lys | [90] | |
| Oxaliplatin | [94,95] | |
| Cellular iron homeostasis | HIF-2α | [102] |
| miR-545 | [104] | |
| Dichloroacetate | [105] | |
| IREB2 | [106] | |
| P53 | Ginsenoside Rh4 | [113] |
| Cullin-9 | [114] |
In animal studies, the underlying mechanism of ferroptosis is complex, involving multiple targeted enzyme systems and metabolic networks. However, the actual clinical situation is more complicated, which requires the combination of gene mutation, epigenetic modification, metabolomics, etc. The absorption, transport, storage and metabolism of iron in the body is a very complex process, and how to define the therapeutic iron concentration needs to be carefully considered. In practice, increasing iron concentration to promote ferroptosis in tumor cells seems difficult to achieve due to the presence of defense mechanisms in the TME. At present, many studies have mentioned the promotion of ferroptosis in CRC cells through nanotechnology, and nano-DDSs seems to be able to effectively help solve this problem due to the advantages of targeted delivery and controlled release. In fact, ferroptosis seems to be a double-edged sword in the treatment of gastrointestinal diseases. The role of ferroptosis in different gastrointestinal diseases is different, and the pros and cons of ferroptosis treatment need to be evaluated more carefully.
At present, research on the mechanism underlying ferroptosis in the colorectum is still in its infancy, and other ferroptosis pathways or related targets, such as the ferroptosis suppressor protein 1/CoQ/nicotinamide adenine dinucleotide phosphate pathway, still need to be further explored. In the future, ferroptosis genes related to the prognosis of CRC also need to be verified. The mechanism underlying ferroptosis and tumor escape in CRC is also worth further in-depth study in order to promote the development of new and effective therapeutic strategies.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lamballe F, France; Sato T, Japan S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4235] [Cited by in RCA: 11369] [Article Influence: 3789.7] [Reference Citation Analysis (4)] |
| 2. | Kleppe A, Albregtsen F, Vlatkovic L, Pradhan M, Nielsen B, Hveem TS, Askautrud HA, Kristensen GB, Nesbakken A, Trovik J, Wæhre H, Tomlinson I, Shepherd NA, Novelli M, Kerr DJ, Danielsen HE. Chromatin organisation and cancer prognosis: a pan-cancer study. Lancet Oncol. 2018;19:356-369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (1)] |
| 3. | Wang X, Ward PA. Opportunities and challenges of disease biomarkers: a new section in the Journal of Translational Medicine. J Transl Med. 2012;10:240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Galluzzi L, Vitale I, Aaronson SA, Abrams JM, Adam D, Agostinis P, Alnemri ES, Altucci L, Amelio I, Andrews DW, Annicchiarico-Petruzzelli M, Antonov AV, Arama E, Baehrecke EH, Barlev NA, Bazan NG, Bernassola F, Bertrand MJM, Bianchi K, Blagosklonny MV, Blomgren K, Borner C, Boya P, Brenner C, Campanella M, Candi E, Carmona-Gutierrez D, Cecconi F, Chan FK, Chandel NS, Cheng EH, Chipuk JE, Cidlowski JA, Ciechanover A, Cohen GM, Conrad M, Cubillos-Ruiz JR, Czabotar PE, D'Angiolella V, Dawson TM, Dawson VL, De Laurenzi V, De Maria R, Debatin KM, DeBerardinis RJ, Deshmukh M, Di Daniele N, Di Virgilio F, Dixit VM, Dixon SJ, Duckett CS, Dynlacht BD, El-Deiry WS, Elrod JW, Fimia GM, Fulda S, García-Sáez AJ, Garg AD, Garrido C, Gavathiotis E, Golstein P, Gottlieb E, Green DR, Greene LA, Gronemeyer H, Gross A, Hajnoczky G, Hardwick JM, Harris IS, Hengartner MO, Hetz C, Ichijo H, Jäättelä M, Joseph B, Jost PJ, Juin PP, Kaiser WJ, Karin M, Kaufmann T, Kepp O, Kimchi A, Kitsis RN, Klionsky DJ, Knight RA, Kumar S, Lee SW, Lemasters JJ, Levine B, Linkermann A, Lipton SA, Lockshin RA, López-Otín C, Lowe SW, Luedde T, Lugli E, MacFarlane M, Madeo F, Malewicz M, Malorni W, Manic G, Marine JC, Martin SJ, Martinou JC, Medema JP, Mehlen P, Meier P, Melino S, Miao EA, Molkentin JD, Moll UM, Muñoz-Pinedo C, Nagata S, Nuñez G, Oberst A, Oren M, Overholtzer M, Pagano M, Panaretakis T, Pasparakis M, Penninger JM, Pereira DM, Pervaiz S, Peter ME, Piacentini M, Pinton P, Prehn JHM, Puthalakath H, Rabinovich GA, Rehm M, Rizzuto R, Rodrigues CMP, Rubinsztein DC, Rudel T, Ryan KM, Sayan E, Scorrano L, Shao F, Shi Y, Silke J, Simon HU, Sistigu A, Stockwell BR, Strasser A, Szabadkai G, Tait SWG, Tang D, Tavernarakis N, Thorburn A, Tsujimoto Y, Turk B, Vanden Berghe T, Vandenabeele P, Vander Heiden MG, Villunger A, Virgin HW, Vousden KH, Vucic D, Wagner EF, Walczak H, Wallach D, Wang Y, Wells JA, Wood W, Yuan J, Zakeri Z, Zhivotovsky B, Zitvogel L, Melino G, Kroemer G. Molecular mechanisms of cell death: recommendations of the Nomenclature Committee on Cell Death 2018. Cell Death Differ. 2018;25:486-541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3672] [Cited by in RCA: 4477] [Article Influence: 639.6] [Reference Citation Analysis (0)] |
| 5. | Dixon SJ, Lemberg KM, Lamprecht MR, Skouta R, Zaitsev EM, Gleason CE, Patel DN, Bauer AJ, Cantley AM, Yang WS, Morrison B 3rd, Stockwell BR. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149:1060-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4711] [Cited by in RCA: 11544] [Article Influence: 888.0] [Reference Citation Analysis (1)] |
| 6. | Tang D, Chen X, Kang R, Kroemer G. Ferroptosis: molecular mechanisms and health implications. Cell Res. 2021;31:107-125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1891] [Cited by in RCA: 2384] [Article Influence: 596.0] [Reference Citation Analysis (0)] |
| 7. | Vabulas RM. Ferroptosis-Related Flavoproteins: Their Function and Stability. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Zhong Y, Zhang W, Yu H, Lin L, Gao X, He J, Li D, Chen Y, Zeng Z, Xu Y, Tang D, Dai Y. Multi-platform-based characterization of ferroptosis in human colorectal cancer. iScience. 2022;25:104750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Lv Y, Feng QY, Zhang ZY, Zheng P, Zhu DX, Lin Q, Chen SM, Mao YH, Xu YQ, Ji ML, Xu JM, He GD. Low ferroptosis score predicts chemotherapy responsiveness and immune-activation in colorectal cancer. Cancer Med. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 10. | Zhu L, Yang F, Wang L, Dong L, Huang Z, Wang G, Chen G, Li Q. Identification the ferroptosis-related gene signature in patients with esophageal adenocarcinoma. Cancer Cell Int. 2021;21:124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 76] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 11. | Li C, Zhang Y, Liu J, Kang R, Klionsky DJ, Tang D. Mitochondrial DNA stress triggers autophagy-dependent ferroptotic death. Autophagy. 2021;17:948-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 302] [Article Influence: 75.5] [Reference Citation Analysis (0)] |
| 12. | Zhu J, Kong W, Xie Z. Expression and Prognostic Characteristics of Ferroptosis-Related Genes in Colon Cancer. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Wang X, Xu Y, Dai L, Yu Z, Wang M, Chan S, Sun R, Han Q, Chen J, Zuo X, Wang Z, Hu X, Yang Y, Zhao H, Hu K, Zhang H, Chen W. A novel oxidative stress- and ferroptosis-related gene prognostic signature for distinguishing cold and hot tumors in colorectal cancer. Front Immunol. 2022;13:1043738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 14. | Bhan A, Soleimani M, Mandal SS. Long Noncoding RNA and Cancer: A New Paradigm. Cancer Res. 2017;77:3965-3981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2088] [Cited by in RCA: 2150] [Article Influence: 268.8] [Reference Citation Analysis (0)] |
| 15. | Li J, Meng H, Bai Y, Wang K. Regulation of lncRNA and Its Role in Cancer Metastasis. Oncol Res. 2016;23:205-217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 234] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 16. | Peng WX, Koirala P, Mo YY. LncRNA-mediated regulation of cell signaling in cancer. Oncogene. 2017;36:5661-5667. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 757] [Cited by in RCA: 1264] [Article Influence: 158.0] [Reference Citation Analysis (0)] |
| 17. | Ni W, Yao S, Zhou Y, Liu Y, Huang P, Zhou A, Liu J, Che L, Li J. Long noncoding RNA GAS5 inhibits progression of colorectal cancer by interacting with and triggering YAP phosphorylation and degradation and is negatively regulated by the m(6)A reader YTHDF3. Mol Cancer. 2019;18:143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 220] [Cited by in RCA: 453] [Article Influence: 75.5] [Reference Citation Analysis (0)] |
| 18. | Wang Y, Lu JH, Wu QN, Jin Y, Wang DS, Chen YX, Liu J, Luo XJ, Meng Q, Pu HY, Wang YN, Hu PS, Liu ZX, Zeng ZL, Zhao Q, Deng R, Zhu XF, Ju HQ, Xu RH. LncRNA LINRIS stabilizes IGF2BP2 and promotes the aerobic glycolysis in colorectal cancer. Mol Cancer. 2019;18:174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 337] [Cited by in RCA: 365] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 19. | Yuan H, Tu S, Ma Y, Sun Y. Downregulation of lncRNA RPLP0P2 inhibits cell proliferation, invasion and migration, and promotes apoptosis in colorectal cancer. Mol Med Rep. 2021;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Lin C, Yang L. Long Noncoding RNA in Cancer: Wiring Signaling Circuitry. Trends Cell Biol. 2018;28:287-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 380] [Cited by in RCA: 399] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 21. | Wu Z, Lu Z, Li L, Ma M, Long F, Wu R, Huang L, Chou J, Yang K, Zhang Y, Li X, Hu G, Lin C. Identification and Validation of Ferroptosis-Related LncRNA Signatures as a Novel Prognostic Model for Colon Cancer. Front Immunol. 2021;12:783362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 97] [Article Influence: 32.3] [Reference Citation Analysis (0)] |
| 22. | Zhang W, Fang D, Li S, Bao X, Jiang L, Sun X. Construction and Validation of a Novel Ferroptosis-Related lncRNA Signature to Predict Prognosis in Colorectal Cancer Patients. Front Genet. 2021;12:709329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 23. | Cai HJ, Zhuang ZC, Wu Y, Zhang YY, Liu X, Zhuang JF, Yang YF, Gao Y, Chen B, Guan GX. Development and validation of a ferroptosis-related lncRNAs prognosis signature in colon cancer. Bosn J Basic Med Sci. 2021;21:569-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 24. | Han Y, Gao X, Wu N, Jin Y, Zhou H, Wang W, Liu H, Chu Y, Cao J, Jiang M, Yang S, Shi Y, Xie X, Chen F, Han Y, Qin W, Xu B, Liang J. Long noncoding RNA LINC00239 inhibits ferroptosis in colorectal cancer by binding to Keap1 to stabilize Nrf2. Cell Death Dis. 2022;13:742. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 50] [Reference Citation Analysis (0)] |
| 25. | Xian ZY, Hu B, Wang T, Cai JL, Zeng JY, Zou Q, Zhu PX. CircABCB10 silencing inhibits the cell ferroptosis and apoptosis by regulating the miR-326/CCL5 axis in rectal cancer. Neoplasma. 2020;67:1063-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 26. | Shao Y, Jia H, Huang L, Li S, Wang C, Aikemu B, Yang G, Hong H, Yang X, Zhang S, Sun J, Zheng M. An Original Ferroptosis-Related Gene Signature Effectively Predicts the Prognosis and Clinical Status for Colorectal Cancer Patients. Front Oncol. 2021;11:711776. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 66] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 27. | Yang YB, Zhou JX, Qiu SH, He JS, Pan JH, Pan YL. Identification of a Novel Ferroptosis-Related Gene Prediction Model for Clinical Prognosis and Immunotherapy of Colorectal Cancer. Dis Markers. 2021;2021:4846683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Yang WS, Kim KJ, Gaschler MM, Patel M, Shchepinov MS, Stockwell BR. Peroxidation of polyunsaturated fatty acids by lipoxygenases drives ferroptosis. Proc Natl Acad Sci U S A. 2016;113:E4966-E4975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 699] [Cited by in RCA: 1599] [Article Influence: 177.7] [Reference Citation Analysis (0)] |
| 29. | Magtanong L, Ko PJ, To M, Cao JY, Forcina GC, Tarangelo A, Ward CC, Cho K, Patti GJ, Nomura DK, Olzmann JA, Dixon SJ. Exogenous Monounsaturated Fatty Acids Promote a Ferroptosis-Resistant Cell State. Cell Chem Biol. 2019;26:420-432.e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 249] [Cited by in RCA: 720] [Article Influence: 120.0] [Reference Citation Analysis (0)] |
| 30. | Cao JY, Dixon SJ. Mechanisms of ferroptosis. Cell Mol Life Sci. 2016;73:2195-2209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1001] [Cited by in RCA: 1112] [Article Influence: 123.6] [Reference Citation Analysis (0)] |
| 31. | Conrad M, Kagan VE, Bayir H, Pagnussat GC, Head B, Traber MG, Stockwell BR. Regulation of lipid peroxidation and ferroptosis in diverse species. Genes Dev. 2018;32:602-619. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 211] [Cited by in RCA: 365] [Article Influence: 52.1] [Reference Citation Analysis (0)] |
| 32. | Lee JY, Nam M, Son HY, Hyun K, Jang SY, Kim JW, Kim MW, Jung Y, Jang E, Yoon SJ, Kim J, Seo J, Min JK, Oh KJ, Han BS, Kim WK, Bae KH, Song J, Huh YM, Hwang GS, Lee EW, Lee SC. Polyunsaturated fatty acid biosynthesis pathway determines ferroptosis sensitivity in gastric cancer. Proc Natl Acad Sci U S A. 2020;117:32433-32442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 320] [Article Influence: 64.0] [Reference Citation Analysis (0)] |
| 33. | Anthonymuthu TS, Kenny EM, Shrivastava I, Tyurina YY, Hier ZE, Ting HC, Dar HH, Tyurin VA, Nesterova A, Amoscato AA, Mikulska-Ruminska K, Rosenbaum JC, Mao G, Zhao J, Conrad M, Kellum JA, Wenzel SE, VanDemark AP, Bahar I, Kagan VE, Bayır H. Empowerment of 15-Lipoxygenase Catalytic Competence in Selective Oxidation of Membrane ETE-PE to Ferroptotic Death Signals, HpETE-PE. J Am Chem Soc. 2018;140:17835-17839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 34. | Dixon SJ, Winter GE, Musavi LS, Lee ED, Snijder B, Rebsamen M, Superti-Furga G, Stockwell BR. Human Haploid Cell Genetics Reveals Roles for Lipid Metabolism Genes in Nonapoptotic Cell Death. ACS Chem Biol. 2015;10:1604-1609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 654] [Cited by in RCA: 757] [Article Influence: 75.7] [Reference Citation Analysis (0)] |
| 35. | Park S, Oh J, Kim M, Jin EJ. Bromelain effectively suppresses Kras-mutant colorectal cancer by stimulating ferroptosis. Anim Cells Syst (Seoul). 2018;22:334-340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 36. | Dai G, Wang D, Ma S, Hong S, Ding K, Tan X, Ju W. ACSL4 promotes colorectal cancer and is a potential therapeutic target of emodin. Phytomedicine. 2022;102:154149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 37. | Liang L, Wang L, Zhu P, Xia Y, Qiao Y, Wu J, Zhuang W, Fei J, Wen Y, Jiang X. A Pilot Study of Apatinib as Third-Line Treatment in Patients With Heavily Treated Metastatic Colorectal Cancer. Clin Colorectal Cancer. 2018;17:e443-e449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 38. | Tian X, Li S, Ge G. Apatinib Promotes Ferroptosis in Colorectal Cancer Cells by Targeting ELOVL6/ACSL4 Signaling. Cancer Manag Res. 2021;13:1333-1342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 39. | Forman HJ, Zhang H, Rinna A. Glutathione: overview of its protective roles, measurement, and biosynthesis. Mol Aspects Med. 2009;30:1-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1947] [Cited by in RCA: 1650] [Article Influence: 103.1] [Reference Citation Analysis (0)] |
| 40. | Lv H, Zhen C, Liu J, Yang P, Hu L, Shang P. Unraveling the Potential Role of Glutathione in Multiple Forms of Cell Death in Cancer Therapy. Oxid Med Cell Longev. 2019;2019:3150145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 143] [Cited by in RCA: 214] [Article Influence: 35.7] [Reference Citation Analysis (0)] |
| 41. | Liu J, Xia X, Huang P. xCT: A Critical Molecule That Links Cancer Metabolism to Redox Signaling. Mol Ther. 2020;28:2358-2366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 219] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 42. | Ottestad-Hansen S, Hu QX, Follin-Arbelet VV, Bentea E, Sato H, Massie A, Zhou Y, Danbolt NC. The cystine-glutamate exchanger (xCT, Slc7a11) is expressed in significant concentrations in a subpopulation of astrocytes in the mouse brain. Glia. 2018;66:951-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 43. | Miyamoto K, Watanabe M, Boku S, Sukeno M, Morita M, Kondo H, Sakaguchi K, Taguchi T, Sakai T. xCT Inhibition Increases Sensitivity to Vorinostat in a ROS-Dependent Manner. Cancers (Basel). 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 44. | Conrad M, Sato H. The oxidative stress-inducible cystine/glutamate antiporter, system x (c) (-) : cystine supplier and beyond. Amino Acids. 2012;42:231-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 458] [Article Influence: 32.7] [Reference Citation Analysis (0)] |
| 45. | Ahmed I, Manno FAM, Manno SHC, Liu Y, Zhang Y, Lau C. Detection of lithium in breast milk and in situ elemental analysis of the mammary gland. Biomed Opt Express. 2018;9:4184-4195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 46. | Jiang L, Kon N, Li T, Wang SJ, Su T, Hibshoosh H, Baer R, Gu W. Ferroptosis as a p53-mediated activity during tumour suppression. Nature. 2015;520:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1173] [Cited by in RCA: 2377] [Article Influence: 237.7] [Reference Citation Analysis (0)] |
| 47. | Sun X, Ou Z, Chen R, Niu X, Chen D, Kang R, Tang D. Activation of the p62-Keap1-NRF2 pathway protects against ferroptosis in hepatocellular carcinoma cells. Hepatology. 2016;63:173-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 872] [Cited by in RCA: 1482] [Article Influence: 164.7] [Reference Citation Analysis (0)] |
| 48. | Bridges RJ, Natale NR, Patel SA. System xc⁻ cystine/glutamate antiporter: an update on molecular pharmacology and roles within the CNS. Br J Pharmacol. 2012;165:20-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 419] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 49. | Xu X, Zhang X, Wei C, Zheng D, Lu X, Yang Y, Luo A, Zhang K, Duan X, Wang Y. Targeting SLC7A11 specifically suppresses the progression of colorectal cancer stem cells via inducing ferroptosis. Eur J Pharm Sci. 2020;152:105450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 50. | Xia Y, Liu S, Li C, Ai Z, Shen W, Ren W, Yang X. Discovery of a novel ferroptosis inducer-talaroconvolutin A-killing colorectal cancer cells in vitro and in vivo. Cell Death Dis. 2020;11:988. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 96] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 51. | Gao W, Huang Z, Duan J, Nice EC, Lin J, Huang C. Elesclomol induces copper-dependent ferroptosis in colorectal cancer cells via degradation of ATP7A. Mol Oncol. 2021;15:3527-3544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 197] [Article Influence: 49.3] [Reference Citation Analysis (0)] |
| 52. | Zhang L, Liu W, Liu F, Wang Q, Song M, Yu Q, Tang K, Teng T, Wu D, Wang X, Han W, Li Y. IMCA Induces Ferroptosis Mediated by SLC7A11 through the AMPK/mTOR Pathway in Colorectal Cancer. Oxid Med Cell Longev. 2020;2020:1675613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 71] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 53. | Han L, Yan Y, Fan M, Gao S, Zhang L, Xiong X, Li R, Xiao X, Wang X, Ni L, Tong D, Huang C, Cao Y, Yang J. Pt3R5G inhibits colon cancer cell proliferation through inducing ferroptosis by down-regulating SLC7A11. Life Sci. 2022;306:120859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 54. | Zhang Z, Ji Y, Hu N, Yu Q, Zhang X, Li J, Wu F, Xu H, Tang Q, Li X. Ferroptosis-induced anticancer effect of resveratrol with a biomimetic nano-delivery system in colorectal cancer treatment. Asian J Pharm Sci. 2022;17:751-766. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 78] [Reference Citation Analysis (0)] |
| 55. | Wang L, Liu Y, Du T, Yang H, Lei L, Guo M, Ding HF, Zhang J, Wang H, Chen X, Yan C. ATF3 promotes erastin-induced ferroptosis by suppressing system Xc(). Cell Death Differ. 2020;27:662-675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 535] [Article Influence: 89.2] [Reference Citation Analysis (0)] |
| 56. | Chen D, Tavana O, Chu B, Erber L, Chen Y, Baer R, Gu W. NRF2 Is a Major Target of ARF in p53-Independent Tumor Suppression. Mol Cell. 2017;68:224-232.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 245] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 57. | Chen L, Qiao L, Bian Y, Sun X. GDF15 knockdown promotes erastin-induced ferroptosis by decreasing SLC7A11 expression. Biochem Biophys Res Commun. 2020;526:293-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 58. | Shen D, Luo J, Chen L, Ma W, Mao X, Zhang Y, Zheng J, Wang Y, Wan J, Wang S, Ouyang J, Yi H, Liu D, Huang W, Zhang W, Liu Z, McLeod HL, He Y. PARPi treatment enhances radiotherapy-induced ferroptosis and antitumor immune responses via the cGAS signaling pathway in colorectal cancer. Cancer Lett. 2022;550:215919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 45] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 59. | Hao S, Liang B, Huang Q, Dong S, Wu Z, He W, Shi M. Metabolic networks in ferroptosis. Oncol Lett. 2018;15:5405-5411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 60. | Liu N, Lin X, Huang C. Activation of the reverse transsulfuration pathway through NRF2/CBS confers erastin-induced ferroptosis resistance. Br J Cancer. 2020;122:279-292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 154] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 61. | Wang L, Cai H, Hu Y, Liu F, Huang S, Zhou Y, Yu J, Xu J, Wu F. A pharmacological probe identifies cystathionine β-synthase as a new negative regulator for ferroptosis. Cell Death Dis. 2018;9:1005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 99] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 62. | Wang M, Mao C, Ouyang L, Liu Y, Lai W, Liu N, Shi Y, Chen L, Xiao D, Yu F, Wang X, Zhou H, Cao Y, Liu S, Yan Q, Tao Y, Zhang B. Long noncoding RNA LINC00336 inhibits ferroptosis in lung cancer by functioning as a competing endogenous RNA. Cell Death Differ. 2019;26:2329-2343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 225] [Cited by in RCA: 394] [Article Influence: 65.7] [Reference Citation Analysis (0)] |
| 63. | Szabo C, Coletta C, Chao C, Módis K, Szczesny B, Papapetropoulos A, Hellmich MR. Tumor-derived hydrogen sulfide, produced by cystathionine-β-synthase, stimulates bioenergetics, cell proliferation, and angiogenesis in colon cancer. Proc Natl Acad Sci U S A. 2013;110:12474-12479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 568] [Article Influence: 47.3] [Reference Citation Analysis (0)] |
| 64. | Szabo C. Gasotransmitters in cancer: from pathophysiology to experimental therapy. Nat Rev Drug Discov. 2016;15:185-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 507] [Article Influence: 50.7] [Reference Citation Analysis (0)] |
| 65. | Hayano M, Yang WS, Corn CK, Pagano NC, Stockwell BR. Loss of cysteinyl-tRNA synthetase (CARS) induces the transsulfuration pathway and inhibits ferroptosis induced by cystine deprivation. Cell Death Differ. 2016;23:270-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 311] [Cited by in RCA: 361] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 66. | Pan X, Qi Y, Du Z, He J, Yao S, Lu W, Ding K, Zhou M. Zinc oxide nanosphere for hydrogen sulfide scavenging and ferroptosis of colorectal cancer. J Nanobiotechnology. 2021;19:392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 67. | Stockwell BR, Friedmann Angeli JP, Bayir H, Bush AI, Conrad M, Dixon SJ, Fulda S, Gascón S, Hatzios SK, Kagan VE, Noel K, Jiang X, Linkermann A, Murphy ME, Overholtzer M, Oyagi A, Pagnussat GC, Park J, Ran Q, Rosenfeld CS, Salnikow K, Tang D, Torti FM, Torti SV, Toyokuni S, Woerpel KA, Zhang DD. Ferroptosis: A Regulated Cell Death Nexus Linking Metabolism, Redox Biology, and Disease. Cell. 2017;171:273-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4608] [Cited by in RCA: 4906] [Article Influence: 613.3] [Reference Citation Analysis (0)] |
| 68. | Maiorino M, Conrad M, Ursini F. GPx4, Lipid Peroxidation, and Cell Death: Discoveries, Rediscoveries, and Open Issues. Antioxid Redox Signal. 2018;29:61-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 467] [Article Influence: 66.7] [Reference Citation Analysis (0)] |
| 69. | Gong Y, Wang N, Liu N, Dong H. Lipid Peroxidation and GPX4 Inhibition Are Common Causes for Myofibroblast Differentiation and Ferroptosis. DNA Cell Biol. 2019;38:725-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 70. | Bösl MR, Takaku K, Oshima M, Nishimura S, Taketo MM. Early embryonic lethality caused by targeted disruption of the mouse selenocysteine tRNA gene (Trsp). Proc Natl Acad Sci U S A. 1997;94:5531-5534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 246] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 71. | Ingold I, Berndt C, Schmitt S, Doll S, Poschmann G, Buday K, Roveri A, Peng X, Porto Freitas F, Seibt T, Mehr L, Aichler M, Walch A, Lamp D, Jastroch M, Miyamoto S, Wurst W, Ursini F, Arnér ESJ, Fradejas-Villar N, Schweizer U, Zischka H, Friedmann Angeli JP, Conrad M. Selenium Utilization by GPX4 Is Required to Prevent Hydroperoxide-Induced Ferroptosis. Cell. 2018;172:409-422.e21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 537] [Cited by in RCA: 1112] [Article Influence: 158.9] [Reference Citation Analysis (0)] |
| 72. | Sui X, Zhang R, Liu S, Duan T, Zhai L, Zhang M, Han X, Xiang Y, Huang X, Lin H, Xie T. RSL3 Drives Ferroptosis Through GPX4 Inactivation and ROS Production in Colorectal Cancer. Front Pharmacol. 2018;9:1371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 171] [Cited by in RCA: 488] [Article Influence: 69.7] [Reference Citation Analysis (0)] |
| 73. | Chen H, Qi Q, Wu N, Wang Y, Feng Q, Jin R, Jiang L. Aspirin promotes RSL3-induced ferroptosis by suppressing mTOR/SREBP-1/SCD1-mediated lipogenesis in PIK3CA-mutatnt colorectal cancer. Redox Biol. 2022;55:102426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 108] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 74. | Fu Y, Huang B, Shi Z, Han J, Wang Y, Huangfu J, Wu W. SRSF1 and SRSF9 RNA binding proteins promote Wnt signalling-mediated tumorigenesis by enhancing β-catenin biosynthesis. EMBO Mol Med. 2013;5:737-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 75. | Yoshino H, Enokida H, Chiyomaru T, Tatarano S, Hidaka H, Yamasaki T, Gotannda T, Tachiwada T, Nohata N, Yamane T, Seki N, Nakagawa M. Tumor suppressive microRNA-1 mediated novel apoptosis pathways through direct inhibition of splicing factor serine/arginine-rich 9 (SRSF9/SRp30c) in bladder cancer. Biochem Biophys Res Commun. 2012;417:588-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 76. | Zhang Q, Lv R, Guo W, Li X. microRNA-802 inhibits cell proliferation and induces apoptosis in human cervical cancer by targeting serine/arginine-rich splicing factor 9. J Cell Biochem. 2019;120:10370-10379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 77. | Wang R, Xing R, Su Q, Yin H, Wu D, Lv C, Yan Z. Knockdown of SFRS9 Inhibits Progression of Colorectal Cancer Through Triggering Ferroptosis Mediated by GPX4 Reduction. Front Oncol. 2021;11:683589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 78. | Wang R, Su Q, Yin H, Wu D, Lv C, Yan Z. Inhibition of SRSF9 enhances the sensitivity of colorectal cancer to erastin-induced ferroptosis by reducing glutathione peroxidase 4 expression. Int J Biochem Cell Biol. 2021;134:105948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 79. | Lu D, Yang Z, Xia Q, Gao S, Sun S, Luo X, Li Z, Zhang X, Li X. ACADSB regulates ferroptosis and affects the migration, invasion, and proliferation of colorectal cancer cells. Cell Biol Int. 2020;44:2334-2343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 80. | Dodson M, Castro-Portuguez R, Zhang DD. NRF2 plays a critical role in mitigating lipid peroxidation and ferroptosis. Redox Biol. 2019;23:101107. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1085] [Cited by in RCA: 1502] [Article Influence: 250.3] [Reference Citation Analysis (0)] |
| 81. | . Homeostasis of redox status derived from glucose metabolic pathway could be the key to understanding the Warburg effect [Retraction]. Am J Cancer Res. 2016;6:2387. [PubMed] |
| 82. | Liu X, Yuan X, Liang G, Zhang S, Zhang G, Qin Y, Zhu Q, Xiao Q, Hou N, Luo JD. BRG1 protects the heart from acute myocardial infarction by reducing oxidative damage through the activation of the NRF2/HO1 signaling pathway. Free Radic Biol Med. 2020;160:820-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 83. | Sun J, Zhou C, Zhao Y, Zhang X, Chen W, Zhou Q, Hu B, Gao D, Raatz L, Wang Z, Nelson PJ, Jiang Y, Ren N, Bruns CJ, Zhou H. Quiescin sulfhydryl oxidase 1 promotes sorafenib-induced ferroptosis in hepatocellular carcinoma by driving EGFR endosomal trafficking and inhibiting NRF2 activation. Redox Biol. 2021;41:101942. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 129] [Cited by in RCA: 126] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 84. | Qiu YB, Wan BB, Liu G, Wu YX, Chen D, Lu MD, Chen JL, Yu RQ, Chen DZ, Pang QF. Nrf2 protects against seawater drowning-induced acute lung injury via inhibiting ferroptosis. Respir Res. 2020;21:232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 118] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 85. | Ranti I, Wahyuningsih MSH, Wirohadidjojo YW. The antifibrotic effect of isolate tagitinin C from tithonia diversifolia (Hemsley) A. Gray on keloid fibroblast cell. Pan Afr Med J. 2018;30:264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 86. | Wei R, Zhao Y, Wang J, Yang X, Li S, Wang Y, Fei J, Hao X, Gui L, Ding X. Tagitinin C induces ferroptosis through PERK-Nrf2-HO-1 signaling pathway in colorectal cancer cells. Int J Biol Sci. 2021;17:2703-2717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 270] [Article Influence: 67.5] [Reference Citation Analysis (1)] |
| 87. | Jensen BV, Schou JV, Yilmaz M, Johannesen HH, Skougaard K, Linnemann D, Hogdall EV, Larsen FO, Johansen JS, Pfeiffer P, Nielsen DL. Cetuximab plus irinotecan administered biweekly with reduced infusion time to heavily pretreated patients with metastatic colorectal cancer and related RAS and BRAF mutation status. Int J Cancer. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 88. | Wadlow RC, Hezel AF, Abrams TA, Blaszkowsky LS, Fuchs CS, Kulke MH, Kwak EL, Meyerhardt JA, Ryan DP, Szymonifka J, Wolpin BM, Zhu AX, Clark JW. Panitumumab in patients with KRAS wild-type colorectal cancer after progression on cetuximab. Oncologist. 2012;17:14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 89. | Amado RG, Wolf M, Peeters M, Van Cutsem E, Siena S, Freeman DJ, Juan T, Sikorski R, Suggs S, Radinsky R, Patterson SD, Chang DD. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26:1626-1634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2504] [Cited by in RCA: 2402] [Article Influence: 141.3] [Reference Citation Analysis (0)] |
| 90. | Gao Z, Jiang J, Hou L, Ji F. Lysionotin Induces Ferroptosis to Suppress Development of Colorectal Cancer via Promoting Nrf2 Degradation. Oxid Med Cell Longev. 2022;2022:1366957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 91. | Yang CC, Hsiao LD, Lin HH, Tseng HC, Situmorang JH, Leu YL, Yang CM. Induction of HO-1 by 5, 8-Dihydroxy-4',7-Dimethoxyflavone via Activation of ROS/p38 MAPK/Nrf2 Attenuates Thrombin-Induced Connective Tissue Growth Factor Expression in Human Cardiac Fibroblasts. Oxid Med Cell Longev. 2020;2020:1080168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 92. | Chen Q, Shen L, Chen C, He H, Fu Y, Xu L, Wang Y. Cetuximab combined with cisplatin improves the prognosis of gastric cancer patients and its effect on P38 MAPK expression. J BUON. 2019;24:2490-2498. [PubMed] |
| 93. | Yang J, Mo J, Dai J, Ye C, Cen W, Zheng X, Jiang L, Ye L. Cetuximab promotes RSL3-induced ferroptosis by suppressing the Nrf2/HO-1 signalling pathway in KRAS mutant colorectal cancer. Cell Death Dis. 2021;12:1079. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 199] [Cited by in RCA: 198] [Article Influence: 49.5] [Reference Citation Analysis (0)] |
| 94. | Lu Y, Wu S, Xiang B, Li L, Lin Y. Curcumin Attenuates Oxaliplatin-Induced Liver Injury and Oxidative Stress by Activating the Nrf2 Pathway. Drug Des Devel Ther. 2020;14:73-85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 95. | Chian S, Li YY, Wang XJ, Tang XW. Luteolin sensitizes two oxaliplatin-resistant colorectal cancer cell lines to chemotherapeutic drugs via inhibition of the Nrf2 pathway. Asian Pac J Cancer Prev. 2014;15:2911-2916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 84] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 96. | Liu B, Wang H. Oxaliplatin induces ferroptosis and oxidative stress in HT29 colorectal cancer cells by inhibiting the Nrf2 signaling pathway. Exp Ther Med. 2022;23:394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 97. | Lane DJ, Merlot AM, Huang ML, Bae DH, Jansson PJ, Sahni S, Kalinowski DS, Richardson DR. Cellular iron uptake, trafficking and metabolism: Key molecules and mechanisms and their roles in disease. Biochim Biophys Acta. 2015;1853:1130-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 282] [Article Influence: 28.2] [Reference Citation Analysis (0)] |
| 98. | Coffey R, Ganz T. Iron homeostasis: An anthropocentric perspective. J Biol Chem. 2017;292:12727-12734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 145] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 99. | Dixon SJ, Stockwell BR. The role of iron and reactive oxygen species in cell death. Nat Chem Biol. 2014;10:9-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1155] [Cited by in RCA: 1698] [Article Influence: 154.4] [Reference Citation Analysis (1)] |
| 100. | Stoyanovsky DA, Tyurina YY, Shrivastava I, Bahar I, Tyurin VA, Protchenko O, Jadhav S, Bolevich SB, Kozlov AV, Vladimirov YA, Shvedova AA, Philpott CC, Bayir H, Kagan VE. Iron catalysis of lipid peroxidation in ferroptosis: Regulated enzymatic or random free radical reaction? Free Radic Biol Med. 2019;133:153-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 252] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 101. | Kindrat I, Tryndyak V, de Conti A, Shpyleva S, Mudalige TK, Kobets T, Erstenyuk AM, Beland FA, Pogribny IP. MicroRNA-152-mediated dysregulation of hepatic transferrin receptor 1 in liver carcinogenesis. Oncotarget. 2016;7:1276-1287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 102. | Shah YM, Matsubara T, Ito S, Yim SH, Gonzalez FJ. Intestinal hypoxia-inducible transcription factors are essential for iron absorption following iron deficiency. Cell Metab. 2009;9:152-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 350] [Cited by in RCA: 337] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 103. | Singhal R, Mitta SR, Das NK, Kerk SA, Sajjakulnukit P, Solanki S, Andren A, Kumar R, Olive KP, Banerjee R, Lyssiotis CA, Shah YM. HIF-2α activation potentiates oxidative cell death in colorectal cancers by increasing cellular iron. J Clin Invest. 2021;131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 138] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 104. | Zheng S, Hu L, Song Q, Shan Y, Yin G, Zhu H, Kong W, Zhou C. miR-545 promotes colorectal cancer by inhibiting transferring in the non-normal ferroptosis signaling. Aging (Albany NY). 2021;13:26137-26147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 105. | Sun J, Cheng X, Pan S, Wang L, Dou W, Liu J, Shi X. Dichloroacetate attenuates the stemness of colorectal cancer cells via trigerring ferroptosis through sequestering iron in lysosomes. Environ Toxicol. 2021;36:520-529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 106. | Song J, Liu T, Yin Y, Zhao W, Lin Z, Lu D, You F. The deubiquitinase OTUD1 enhances iron transport and potentiates host antitumor immunity. EMBO Rep. 2021;22:e51162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 104] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 107. | Zhang W, Gai C, Ding D, Wang F, Li W. Targeted p53 on Small-Molecules-Induced Ferroptosis in Cancers. Front Oncol. 2018;8:507. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 108. | Xie Y, Zhu S, Song X, Sun X, Fan Y, Liu J, Zhong M, Yuan H, Zhang L, Billiar TR, Lotze MT, Zeh HJ 3rd, Kang R, Kroemer G, Tang D. The Tumor Suppressor p53 Limits Ferroptosis by Blocking DPP4 Activity. Cell Rep. 2017;20:1692-1704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 681] [Article Influence: 97.3] [Reference Citation Analysis (0)] |
| 109. | Mao L, Zhao T, Song Y, Lin L, Fan X, Cui B, Feng H, Wang X, Yu Q, Zhang J, Jiang K, Wang B, Sun C. The emerging role of ferroptosis in non-cancer liver diseases: hype or increasing hope? Cell Death Dis. 2020;11:518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 98] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 110. | Yoshizato K, Thuy le TT, Shiota G, Kawada N. Discovery of cytoglobin and its roles in physiology and pathology of hepatic stellate cells. Proc Jpn Acad Ser B Phys Biol Sci. 2016;92:77-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 111. | Ye S, Xu M, Zhu T, Chen J, Shi S, Jiang H, Zheng Q, Liao Q, Ding X, Xi Y. Cytoglobin promotes sensitivity to ferroptosis by regulating p53-YAP1 axis in colon cancer cells. J Cell Mol Med. 2021;25:3300-3311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 112. | Wei G, Sun J, Hou Z, Luan W, Wang S, Cui S, Cheng M, Liu Y. Novel antitumor compound optimized from natural saponin Albiziabioside A induced caspase-dependent apoptosis and ferroptosis as a p53 activator through the mitochondrial pathway. Eur J Med Chem. 2018;157:759-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 113. | Wu Y, Pi D, Chen Y, Zuo Q, Zhou S, Ouyang M. Ginsenoside Rh4 Inhibits Colorectal Cancer Cell Proliferation by Inducing Ferroptosis via Autophagy Activation. Evid Based Complement Alternat Med. 2022;2022:6177553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 114. | Yang L, WenTao T, ZhiYuan Z, Qi L, YuXiang L, Peng Z, Ke L, XiaoNa J, YuZhi P, MeiLing J, QingYang F, GuoDong H, YueXiang W, JianMin X. Cullin-9/p53 mediates HNRNPC degradation to inhibit erastin-induced ferroptosis and is blocked by MDM2 inhibition in colorectal cancer. Oncogene. 2022;41:3210-3221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 115. | Sun X, Wang X, Feng W, Guo H, Tang C, Lu Y, Xiang X, Bao Y. Gene signatures associated with drug resistance to irinotecan and oxaliplatin predict a poor prognosis in patients with colorectal cancer. Oncol Lett. 2017;13:2089-2096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 116. | Sun F, Liang W, Qian J. The identification of CRNDE, H19, UCA1 and HOTAIR as the key lncRNAs involved in oxaliplatin or irinotecan resistance in the chemotherapy of colorectal cancer based on integrative bioinformatics analysis. Mol Med Rep. 2019;20:3583-3596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 117. | Yang C, Zhang Y, Lin S, Liu Y, Li W. Suppressing the KIF20A/NUAK1/Nrf2/GPX4 signaling pathway induces ferroptosis and enhances the sensitivity of colorectal cancer to oxaliplatin. Aging (Albany NY). 2021;13:13515-13534. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 107] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 118. | Lin JF, Hu PS, Wang YY, Tan YT, Yu K, Liao K, Wu QN, Li T, Meng Q, Lin JZ, Liu ZX, Pu HY, Ju HQ, Xu RH, Qiu MZ. Phosphorylated NFS1 weakens oxaliplatin-based chemosensitivity of colorectal cancer by preventing PANoptosis. Signal Transduct Target Ther. 2022;7:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 187] [Article Influence: 62.3] [Reference Citation Analysis (0)] |
| 119. | Zhang Q, Deng T, Zhang H, Zuo D, Zhu Q, Bai M, Liu R, Ning T, Zhang L, Yu Z, Ba Y. Adipocyte-Derived Exosomal MTTP Suppresses Ferroptosis and Promotes Chemoresistance in Colorectal Cancer. Adv Sci (Weinh). 2022;9:e2203357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 115] [Article Influence: 38.3] [Reference Citation Analysis (0)] |
| 120. | Chen P, Li X, Zhang R, Liu S, Xiang Y, Zhang M, Chen X, Pan T, Yan L, Feng J, Duan T, Wang D, Chen B, Jin T, Wang W, Chen L, Huang X, Zhang W, Sun Y, Li G, Kong L, Li Y, Yang Z, Zhang Q, Zhuo L, Sui X, Xie T. Combinative treatment of β-elemene and cetuximab is sensitive to KRAS mutant colorectal cancer cells by inducing ferroptosis and inhibiting epithelial-mesenchymal transformation. Theranostics. 2020;10:5107-5119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 280] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 121. | He Z, Yang J, Sui C, Zhang P, Wang T, Mou T, Sun K, Wang Y, Xu Z, Li G, Deng H, Shi J, Zhuang B. FAM98A promotes resistance to 5-fluorouracil in colorectal cancer by suppressing ferroptosis. Arch Biochem Biophys. 2022;722:109216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 122. | Zhou B, Mai Z, Ye Y, Song Y, Zhang M, Yang X, Xia W, Qiu X. The role of PYCR1 in inhibiting 5-fluorouracil-induced ferroptosis and apoptosis through SLC25A10 in colorectal cancer. Hum Cell. 2022;35:1900-1911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 123. | Sharma P, Shimura T, Banwait JK, Goel A. Andrographis-mediated chemosensitization through activation of ferroptosis and suppression of β-catenin/Wnt-signaling pathways in colorectal cancer. Carcinogenesis. 2020;41:1385-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 124. | Shimura T, Sharma P, Sharma GG, Banwait JK, Goel A. Enhanced anti-cancer activity of andrographis with oligomeric proanthocyanidins through activation of metabolic and ferroptosis pathways in colorectal cancer. Sci Rep. 2021;11:7548. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 125. | Zheng H, Jiang J, Xu S, Liu W, Xie Q, Cai X, Zhang J, Liu S, Li R. Nanoparticle-induced ferroptosis: detection methods, mechanisms and applications. Nanoscale. 2021;13:2266-2285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 99] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 126. | Qian X, Zhang J, Gu Z, Chen Y. Nanocatalysts-augmented Fenton chemical reaction for nanocatalytic tumor therapy. Biomaterials. 2019;211:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 213] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 127. | Liang H, Wu X, Zhao G, Feng K, Ni K, Sun X. Renal Clearable Ultrasmall Single-Crystal Fe Nanoparticles for Highly Selective and Effective Ferroptosis Therapy and Immunotherapy. J Am Chem Soc. 2021;143:15812-15823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 155] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 128. | Giraldo NA, Sanchez-Salas R, Peske JD, Vano Y, Becht E, Petitprez F, Validire P, Ingels A, Cathelineau X, Fridman WH, Sautès-Fridman C. The clinical role of the TME in solid cancer. Br J Cancer. 2019;120:45-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 469] [Article Influence: 67.0] [Reference Citation Analysis (0)] |
| 129. | Shi J, Tian H, Peng L, Huang C, Nice EC, Zou B, Zhang H. A nanoplatform reshaping intracellular osmolarity and redox homeostasis against colorectal cancer. J Control Release. 2022;352:766-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 130. | Yu Z, Tong S, Wang C, Wu Z, Ye Y, Wang S, Jiang K. PPy@Fe(3)O(4) nanoparticles inhibit the proliferation and metastasis of CRC via suppressing the NF-κB signaling pathway and promoting ferroptosis. Front Bioeng Biotechnol. 2022;10:1001994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |