Published online Jan 15, 2022. doi: 10.4251/wjgo.v14.i1.319
Peer-review started: June 10, 2021
First decision: July 16, 2021
Revised: July 30, 2021
Accepted: September 10, 2021
Article in press: September 10, 2021
Published online: January 15, 2022
Processing time: 214 Days and 23.1 Hours
Cancer-related fatigue (CRF) is the most common concomitant symptom in the treatment of colorectal cancer (CRC). Such patients often present with subjective fatigue state accompanied by cognitive dysfunction, which seriously affects the quality of life of patients.
To explore the effects of cognitive behavior therapy (CBT) combined with Baduanjin exercise on CRF, cognitive impairment, and quality of life in patients with CRC after chemotherapy, and to provide a theoretical basis and practical reference for rehabilitation of CRC after chemotherapy.
Fifty-five patients with CRC after radical resection and chemotherapy were randomly divided into either an experimental or a control group. The experimental group received the intervention of CBT combined with exercise intervention for 6 mo, and indicators were observed and measured at baseline, 3 mo, and 6 mo to evaluate the intervention effect.
Compared with the baseline values, in the experimental group 3 mo after intervention, cognitive function, quality of life score, and P300 amplitude and latency changes were significantly better (P < 0.01). Compared with the control group, at 3 mo, the experimental group had significant differences in CRF, P300 amplitude, and quality of life score (P < 0.05), as well as significant differences in P300 latency and cognitive function (P < 0.01). Compared with the control group, at 6 mo, CRF, P300 amplitude, P300 latency, cognitive function and quality of life score were further improved in the experimental group, with significant differences (P < 0.01). The total score of CRF and the scores of each dimension were negatively correlated with quality of life (P < 0.05), while the total score of cognitive impairment and the scores of each dimension were positively correlated with quality of life (P < 0.05).
CBT combined with body-building Baduanjin exercise can improve CRF and cognitive impairment in CRC patients after chemotherapy, and improve their quality of life.
Core Tip: Cognitive behavior therapy combined with body-building Baduanjin exercise can improve cancer-induced fatigue and cognitive impairment in colorectal cancer patients after chemotherapy, and improve their quality of life. The quality of life of colorectal cancer patients may be related to cancer-induced fatigue and cognitive level. Cognitive behavior therapy combined with exercise intervention deserves to be promoted in cancer patients.
- Citation: Lin ZG, Li RD, Ai FL, Li S, Zhang XA. Effects of cognitive behavior therapy combined with Baduanjin in patients with colorectal cancer . World J Gastrointest Oncol 2022; 14(1): 319-333
- URL: https://www.wjgnet.com/1948-5204/full/v14/i1/319.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v14.i1.319
Colorectal cancer (CRC) is one of the most common malignancies. According to the 2018 global cancer statistics, the global mortality rate of CRC accounted for 9.2% of the total number of cancer deaths, and the incidence rate accounted for 10.2% of the total number of cancers, ranking second and third, respectively[1]. CRC is mainly treated by surgical resection, combined with perioperative radiotherapy and chemotherapy and other comprehensive treatment methods. Cancer-related fatigue (CRF) is a subjective fatigue state caused by the adverse effects of cancer itself and chemotherapy, and is also affected by social objective factors and individual factors[2]. Cancer-related cognitive impairment (CRCI) is caused by chemotherapy in cancer patients, often referred to as chemotherapy brain or chemotherapy fog[3]. Due to chronic inactivity and the effects of CRF, cancer patients often develop cognitive impairments that ultimately affect their quality of life.
Cognitive behavioral therapy is concerned about the relationship between thought, feeling, and behavior; the main purpose is to reduce stress, in a rational way to solve the patients’ severe psychological stress response, so that it can adapt to the changes brought by psychological stress[4]. Exercise therapy as a nondrug method has been pursued by clinicians in recent years. Aerobic exercise can improve the physical status of cancer patients, negative emotions such as anxiety and depression, and cognitive impairment and reduce the level of CRF[5]. Baduanjin is a medium-intensity aerobic exercise that has a good promoting effect on human digestion, respiration, circulation, and motor function[6]. So far, there have been few studies on the effect of cognitive behavior therapy (CBT) combined with exercise on cognitive function in patient with CRC. The present study used CBT combined with Baduanjin as the intervention for 6 mo in patients with CRC chemotherapy to explore the value of the combination therapy in the rehabilitation of CRC during chemotherapy.
We recruited patients undergoing chemotherapy for CRC who were admitted to Liaoning Tumor Hospital between March and October 2018. The inclusion criteria were: (1) Subjects met the guidelines for diagnosis, staging, and treatment of CRC[7], and underwent surgery for CRC; (2) In the stable period after surgery (clinical stages I–III); (3) The score of the simple mini-mental state examination scale was 22–27 points; and (4) All patients with CRC successfully completed standardized chemotherapy regimen. The exclusion criteria were: (1) Complicated with serious cardiovascular and cerebrovascular diseases and mental diseases; (2) Presence of limb dysfunction; (3) Accompanied by pneumonia, asthma, and other respiratory diseases; and (4) Had participated in regular exercise during the past 6 mo. This study was approved by the Ethics Committee of Liaoning Tumor Hospital. All subjects participated voluntarily and gave signed informed consent.
Using a random number table method, 60 patients were randomly divided into either an experimental or a control group, with 30 cases in each group. During the study, a total of five patients withdrew from the study, including three in the experimental group who did not complete the treatment on time (n = 2) or whose condition deteriorated (n = 1), and two in the control group who were readmitted to the hospital for chemotherapy and withdrew from the study. Finally, 27 patients in the experimental group and 28 in the control group completed the study. There was no significant difference in patients’ general baseline data or disease-related data between the two groups (P > 0.05; Table 1).
| Experimental group (n = 27) | Control group (n = 28) | P value | |
| Mean age (range, yr) | 52 (44-60) | 51 (40-62) | 0.516 |
| Gender | |||
| Male | 19 (70.4) | 21 (75) | 0.70 |
| Female | 8 (29.6) | 7 (25) | |
| Years of education | |||
| < 9 | 8 (29.6) | 9 (32.2) | 0.747 |
| 9-12 | 15 (55.6) | 13 (46.4) | |
| > 12 | 4 (14.8) | 6 (21.4) | |
| Marital status | |||
| Married | 20 (74.1) | 24 (85.7) | 0.555 |
| Unmarried | 2 (7.4) | 1 (3.6) | |
| Divorced | 5 (18.5) | 3 (10.7) | |
| Clinical stage | |||
| I | 3 (11.1) | 2 (7.2) | 0.763 |
| II | 11 (40.8) | 10 (35.7) | |
| III | 13 (48.1) | 16 (57.1) | |
| Chemotherapy | |||
| XELOX | 12 (44.4) | 10 (35.7) | 0.509 |
| FOLOX | 15 (55.6) | 18 (64.3) | |
| Mean BMI (kg/m2) | 22.56 (20.38-24.05) | 22.71 (21.22-24.19) | 0.561 |
| Mean MMSE score | 24 (22-27) | 24 (22-27) | 0.765 |
The experimental group received CBT from psychotherapists. The patients provided details of their symptoms and illness for 1 h, three times a week. Doctors provided immediate monitoring and cognitive correction, stress management, cognitive restructuring, and relaxation counseling, and encouraged patients to adopt positive behavioral strategies. After discharge, doctors conducted home visits or telephone communication once a week and completed CBT for 6 mo.
During hospitalization, the experimental group received comprehensive and systematic guidance from professional coaches on the skills and exercise load of Baduanjin, until they could all regulate and master the exercise movements. The videos of Baduanjin were released upon discharge. After discharge, the patients were given weekly telephone supervision and follow-up visits. The patients were asked to write a daily exercise diary. The mean duration of exercise was ≥ 4 d/wk, ≥ 20 d/mo, 45–60 min/session, twice daily (once in the morning and once in the afternoon) for 6 mo. There was no exercise intervention in the control group.
The cognitive potential P300 test and scale were evaluated at baseline, and 3 mo and 6 mo after intervention. The changes in cognitive function, CRF, and quality of life of subjects before and after intervention were compared and analyzed, and the effect of intervention was evaluated.
Functional assessment of cancer therapy-cognitive function (FACT-Cog)[8] comprises 37 items in four dimensions, including correction of cognitive impairment, cognitive ability, evaluation by others, and impact on quality of life; each item has a score of 0–4, with 5 grades. The lower the score, the worse the cognitive function, and the test has good reliability and validity[9].
The Cancer Fatigue Scale (CFS) compiled by Okuyama et al[10] was designed for evaluating fatigue symptoms of cancer patients, consisting of 15 items and three dimensions of physical fatigue, emotional fatigue, and cognitive fatigue. Each item was rated on a scale of 1–5, with higher scores indicating more fatigue[11]. Studies have shown that the coefficient of Cronbach’s (a) in the total table is 0.84–0.88, and the sub-half reliability coefficient (r) is 0.32–0.67[12].
Functional assessment of cancer therapy-colorectal (FACT-C) is specifically used in the assessment of CRC patients. It consists of generic and CRC-specific modules with five dimensions: Physiological status, social/family status, emotional status, functional status, and additional concern for CRC. The internal consistency coefficient of additional concern was 0.56, the retest correlation coefficient of other fields was ≥ 0.76, and the α coefficient of all fields and general modules was ≥ 0.80[13].
The amplitudes and latency of P300 were recorded using the 32-channel electroencephalography acquisition system produced by Neuroscan Corporation (Charlotte, NC, United States), and the position of electrode was recorded at CZ point, which is located in the central midline of the brain and is the most commonly used electrode placement for recording cognitive-related potentials in the International Electroencephalogram Society 10-20 standard. The test was completed in the Department of Neurology in hospital.
SPSS 20.0 was used for data analyses. Quantitative data are expressed as the mean ± SD. Repeatability measurement analysis of variance was used between groups and within groups, and Pearson correlation analysis was conducted between variables. Stepwise multiple linear regression was conducted for the variables with high correlation, and P < 0.05 was considered significant, and P < 0.01 was considered highly significant.
The quality of life, cognitive function, and CRF status of all subjects at baseline are shown in Table 2. Among all the quality of life dimensions, social/family status score was the highest, followed by emotional status, additional concern, physiological status, and functional status (Table 2). Among the cognitive status dimensions, others’ evaluation score was the highest, followed by corrected cognitive impairment, cognitive ability, and impact on quality of life. The scores for CRF showed that the scores of each dimension from high to low were physical fatigue, emotional fatigue, and cognitive fatigue.
| Item | Scale score range | Actual score range | Actual score | Score percentage (%) |
| Quality of life | ||||
| FACT-C total score | 0-144 | 36-131 | 81.65 ± 23.27 | 56.72 |
| Physiological status | 0-28 | 6-25 | 15.38 ± 4.47 | 54.93 |
| Social/family status | 0-28 | 9-28 | 19.05 ± 4.57 | 68.04 |
| Emotional status | 0-24 | 6-24 | 14.93 ± 4.08 | 62.21 |
| Functional status | 0-28 | 5-26 | 12.69 ± 4.46 | 45.32 |
| Additional attention score | 0-36 | 10-30 | 19.84 ± 4.87 | 55.11 |
| Cognitive function | ||||
| FACT-Cog total score | 38-132 | 47-108 | 80.15 ± 10.97 | 60.72 |
| Corrected cognitive impairment | 18-72 | 26-57 | 46.62 ± 4.98 | 64.75 |
| Cognitive ability | 0-28 | 7-22 | 14.76 ± 3.21 | 52.14 |
| Other’s evaluation | 4-16 | 5-16 | 10.51 ± 2.28 | 65.69 |
| Impact on quality of life | 4-16 | 4-13 | 8.25 ± 2.08 | 51.75 |
| CRF | ||||
| CFS total score | 0-60 | 22-46 | 34.47 ± 6.59 | 57.45 |
| Physical fatigue | 0-28 | 11-28 | 18.09 ± 3.23 | 64.61 |
| Emotional fatigue | 0-16 | 6-15 | 8.85 ± 1.82 | 55.31 |
| Cognitive fatigue | 0-16 | 3-12 | 7.53 ± 2.05 | 47.06 |
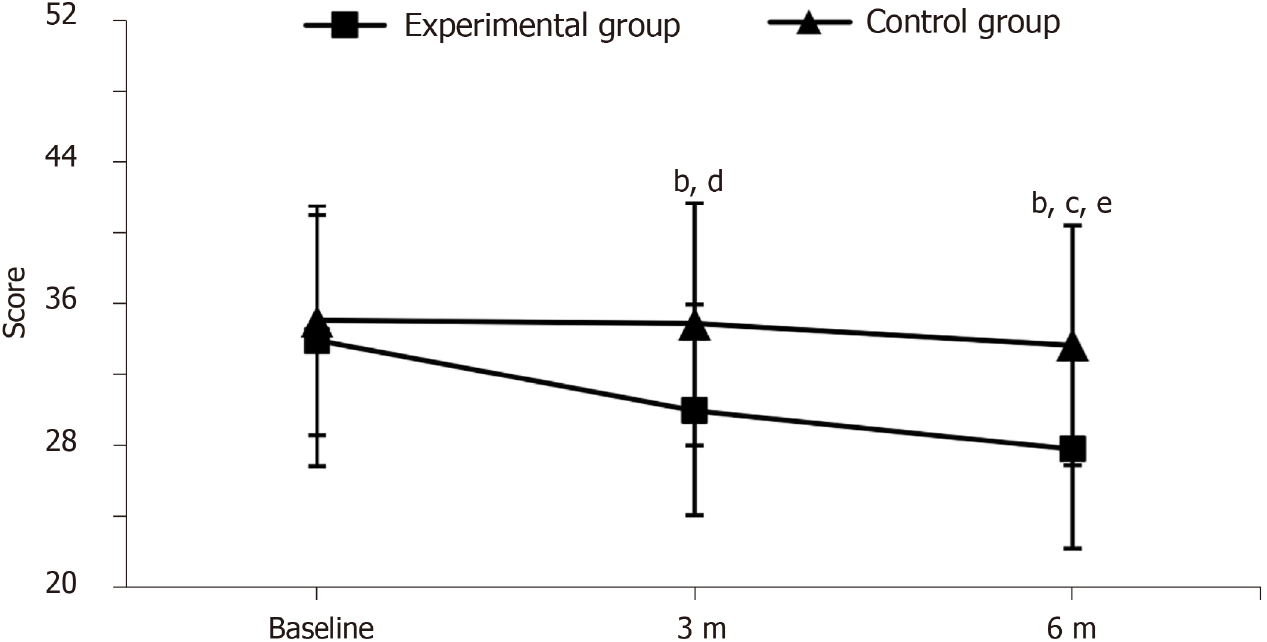
The total score for the CRF test and the scores of each dimension in each group before and after exercise intervention are shown in Figure 1 and Table 3. At baseline, there were no significant differences between the two groups in terms of overall fatigue and each dimension (P > 0.05). Compared with baseline values, there were significant differences in the total score (P < 0.001), body fatigue score (P < 0.001), emotional fatigue score (P < 0.001), and cognitive fatigue (P = 0.013) in the experimental group at 3 mo and 6 mo after intervention. Compared with the control group, there were significant differences in the total score (P = 0.018), body fatigue score (P = 0.003), emotional fatigue score (P = 0.029), and cognitive fatigue (P = 0.022) at 3 mo and 6 mo after exercise intervention in the experimental group (P < 0.001).
| Group | Physical fatigue | Emotional fatigue | Cognitive fatigue |
| Experimental group (n = 27) | |||
| Baseline | 17.56 ± 3.53 | 8.67 ± 1.78 | 7.37 ± 2.09 |
| 3 mo | 15.78 ± 2.85b,e | 7.59 ± 1.67b,d | 6.59 ± 1.65a,d |
| 6 mo | 15.19 ± 2.66b,e | 6.59 ± 1.47b,c,e | 6.33 ± 1.66b,e |
| Control group (n = 28) | |||
| Baseline | 18.61 ± 2.82 | 9.04 ± 1.80 | 7.57 ± 2.06 |
| 3 mo | 18.43 ± 3.71 | 8.61 ± 1.69 | 7.79 ± 2.08 |
| 6 mo | 18.46 ± 3.31 | 8.68 ± 1.91 | 7.68 ± 1.83 |
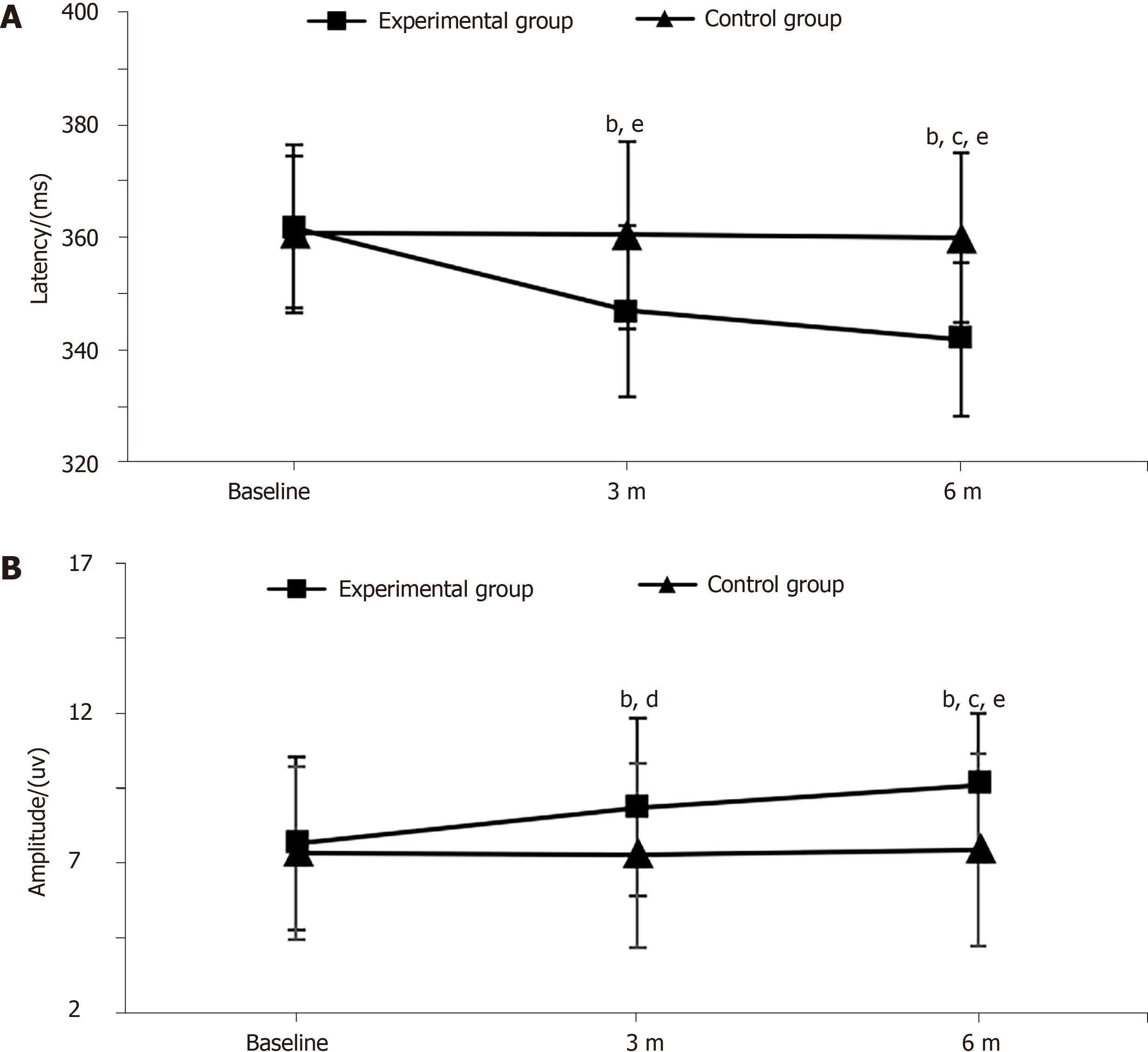
Status of electrophysiological tests: Figure 2 shows the cognitive potential P300 test of each group before and after exercise intervention. At baseline, there was no significant difference in the latency or amplitude of P300 between the two groups (P > 0.05). Compared with baseline values, there were significant differences in latent period (P < 0.001) and amplitude of P300 (P = 0.008) in the experimental group at 3 mo; furthermore, after 6 mo of intervention, there were highly significant differences in latency and amplitude of P300 (P < 0.001). Compared with the control group, there were significant differences in latent period (P = 0.002) and amplitude of P300 (P = 0.041) at 3 mo; and after 6 mo of intervention, the latency of P300 in the experimental group was shortened and the amplitude of P300 increased, with highly significant differences (P < 0.001).
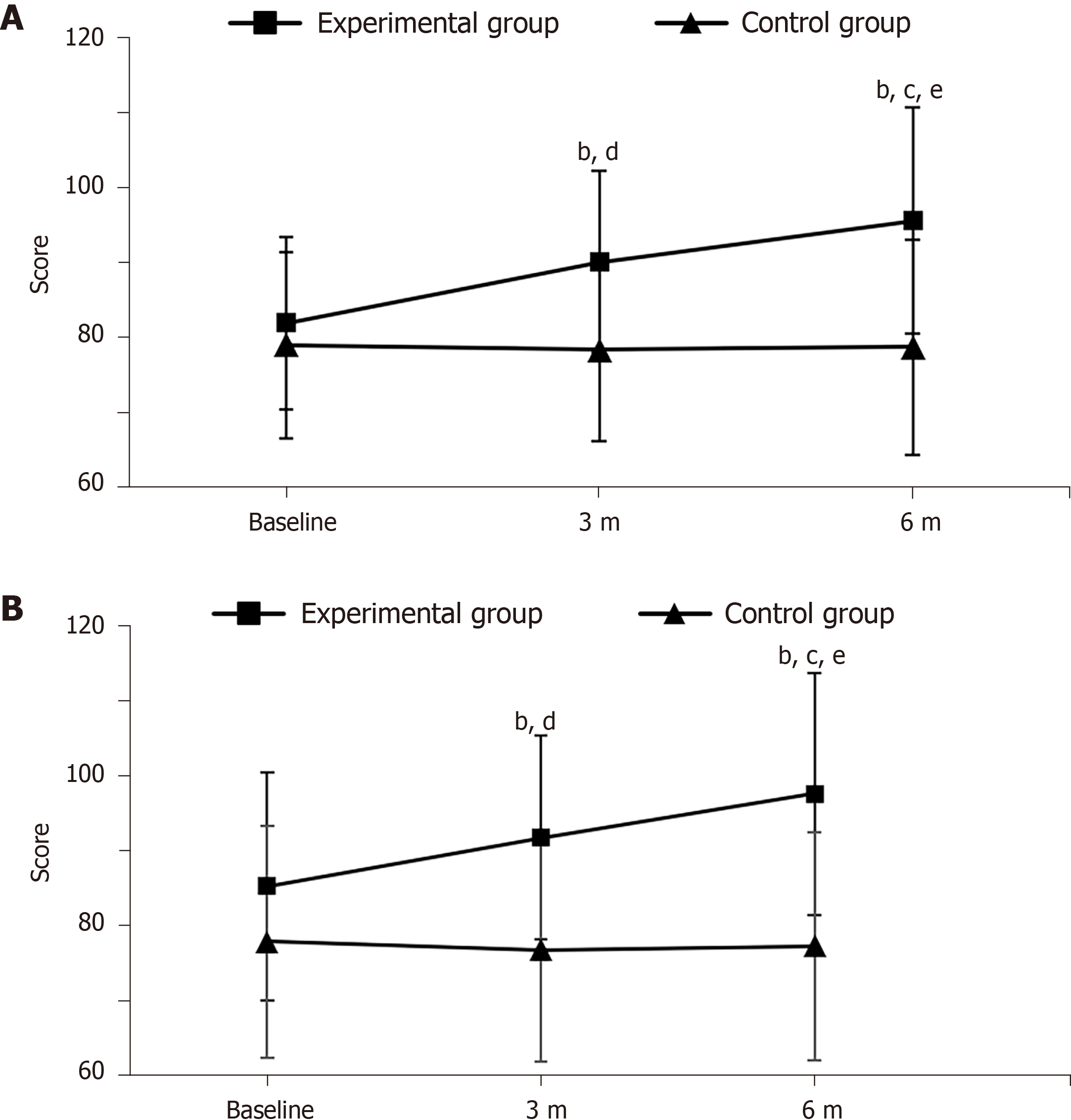
Cognitive scale scores: Figure 3A and Table 4 show the total score of cognitive function and scores of each dimension in each group before and after exercise intervention. At baseline, there were no significant differences between the two groups in FACT-Cog total score or the scores of the four dimensions (P > 0.05). Compared with baseline values, 3 mo after intervention, except for impact on quality of life (P = 0.526) and other’s evaluation (P = 0.013), the P values of total FACT-Cog score and the scores of other two dimensions were all less than 0. 001; 6 mo after intervention, the P values of total FACT-Cog score and the scores of the four dimensions were all less than 0. 001. Compared with the control group, after 3 mo of intervention, there were significant differences in the total score (P = 0.016) and scores of corrected cognitive impairment (P = 0.003), cognitive ability (P = 0.011), and impact on quality of life (P = 0.002); after 6 mo of intervention, there were highly significant differences in the total score (P = 0.002) and scores of corrected cognitive impairment (P < 0.001), cognitive ability (P = 0.002), other’s evaluation (P = 0.002), and impact on quality of life (P < 0.001).
| Group | Corrected cognitive impairment | Cognitive ability | Others’ evaluation | Impact on quality of life |
| Experimental group (n = 27) | ||||
| Baseline | 47.19 ± 4.14 | 14.96 ± 3.47 | 10.93 ± 2.24 | 8.81 ± 2.08 |
| 3 mo | 50.26 ± 3.96b,e | 17.11 ± 3.64b,d | 11.26 ± 2.33a | 9.37 ± 2.66e |
| 6 mo | 54.22 ± 6.80b,c,e | 18.30 ± 4.26b,c,e | 12.22 ± 2.28b,c,e | 10.81 ± 2.73b,c,e |
| Control group (n = 28) | ||||
| Baseline | 46.07 ± 5.73 | 14.57 ± 2.87 | 10.11 ± 2.25 | 7.71 ± 1.94 |
| 3 mo | 46.21 ± 5.37 | 14.68 ± 3.22 | 10.14 ± 2.17 | 7.32 ± 2.02 |
| 6 mo | 46.25 ± 6.92 | 14.86 ± 3.50 | 10.21 ± 2.35 | 7.43 ± 2.01 |
The total score of quality of life and the scores of the five dimensions in each group before and after exercise intervention are shown in Figure 3B and Table 5. At baseline, there were no significant differences between the two groups in the total score of quality of life or the scores of the five dimensions (P > 0.05). Compared with baseline values, 3 mo after intervention, there were significant differences in total score (P < 0.001), and scores of physiological status (P < 0.001), emotional status (P < 0.001), and additional attention (P = 0.044), while there were no significant differences in the score of social/family status (P = 0.455) or functional status (P = 0.059); 6 mo after intervention, there were significant differences in total score and the scores of the five dimensions (P < 0.001). Compared with the control group, after 3 mo of intervention, there were significant differences in total score (P = 0.016) and the scores of physiological status (P = 0.039), social/family status (P = 0.025), emotional status (P = 0.012), functional status (P = 0.007), and additional attention (P = 0.023); after 6 mo of intervention, there were highly significant differences in total score (P = 0.002) and the scores of physiological status (P = 0.001), social/family status (P = 0.009), emotional status (P = 0.010), functional status (P = 0.001), and additional attention (P = 0.001).
| Group | Physiological status | Social/family status | Emotional status | Functional status | Additional attention score |
| Experimental group (n = 27) | |||||
| Baseline | 16.19 ± 3.48 | 19.85 ± 4.92 | 15.41 ± 4.41 | 13.78 ± 4.29 | 11.54 ± 4.36 |
| 3 mo | 17.67 ± 3.96b,d | 20.59 ± 4.73d | 17.11 ± 4.47b,d | 14.74 ± 4.78e | 22.41 ± 6.08a,d |
| 6 mo | 18.70 ± 4.15b,e | 21.48 ± 4.57b,c,e | 17.48 ± 4.64b,d | 16.00 ± 4.84b,c,e | 24.85 ± 6.56b,c,e |
| Control group (n = 28) | |||||
| Baseline | 14.61 ± 5.18 | 18.29 ± 4.14 | 14.46 ± 3.76 | 11.64 ± 4.44 | 19.14 ± 4.28 |
| 3 mo | 14.89 ± 5.72 | 17.75 ± 4.40 | 14.32 ± 3.49 | 11.32 ± 4.28 | 18.71 ± 5.61 |
| 6 mo | 14.25 ± 5.29 | 18.14 ± 4.61 | 14.46 ± 3.75 | 11.54 ± 4.36 | 19.11 ± 5.63 |
Correlation between quality of life and CRF and cognitive function in the experimental group: Pearson correlation analysis was performed between the total scores of FACT-C and CFS and its three dimensions, and the total score of FACT-Cog and its four dimensions. As shown in Table 6, the total score of quality of life was negatively correlated with the total score of fatigue and the scores of the three dimensions, and the total score of quality of life and cognitive function was positively correlated with the four dimensions.
| Item | FACT-C total score | |
| r | P value | |
| CFS total score | -0.733 | < 0.000 |
| Physical fatigue | -0.439 | 0.023 |
| Emotional fatigue | -0.487 | 0.011 |
| Cognitive fatigue | -0.642 | < 0.000 |
| FACT-Cog total score | 0.753 | < 0.000 |
| Corrected cognitive impairment | 0.663 | < 0.000 |
| Cognitive ability | 0.624 | 0.001 |
| Other’s evaluation | 0.186 | 0.342 |
| Impact on quality of life | 0.40 | 0.023 |
Multivariate stepwise regression analysis of quality of life, CRF, and cognitive function in the experimental group: To analyze the relationship between quality of life and CRF and cognitive function, the difference between the total score of quality of life of patients undergoing CRC chemotherapy in the experimental group at 6 mo and the baseline data was used as the dependent variable. Five significant factors in the correlation analysis were taken as independent variables, and the five factors in the multivariate stepwise regression analysis were as follows: CRF total score, cognitive fatigue, FACT-Cog total score, corrected cognitive impairment, and cognitive ability.
The complex correlation coefficient r = 0.80 and the adjusted R2 = 0.603 indicated that the dependent variable (total score of quality of life) of the stepwise fitting multiple linear regression equation could be explained by the independent variables (fatigue and cognition) by 60.3%. According to the standard regression coefficient, Table 7 shows that the factors affecting the quality of life of patients with CRC chemotherapy included total score of CRF and total score of FACT-Cog. Linear regression equation can be established according to the following model, with X1 representing the total score of CRF and X2 representing the total score of FACT-Cog: Y = 4.923 - 0.585 X1 + 0.375 X2, the results showed that the CRF score has a greater impact on quality of life than FACT-Cog score. The collinearity diagnosis results showed that all variables had a variance inflation factor (VIF) < 10, and there was no collinearity; therefore, it is of practical significance to establish the corresponding linear regression model. VIF is a common measure for judging the severity of multicollinearity in multiple linear regression models. Usually, 10 is taken as the judgment boundary. When VIF < 10, there is no multicollinearity.
| Variable | Regression coefficient | SE | Standard regression coefficient | t | P value | Collinearity Statistics | |
| Tolerance | VIF | ||||||
| Constant | 4.923 | 1.429 | 3.209 | 0.004 | |||
| FACT-Cog Total score | 0.375 | 0.149 | 0.464 | 2.512 | 0.019 | 0.447 | 2.235 |
| CRF total score | -0.585 | 0.278 | -0.388 | -2.103 | 0.046 | 0.651 | 1.535 |
CRC has high clinical morbidity. With improvement in medical understanding, its fatality rate has decreased year by year. In recent years, people’s health awareness has been gradually enhanced, but due to the neglect of early screening of CRC, often the best time for diagnosis and treatment is missed, resulting in adverse effects on recovery[14]. Patients with CRC generally need chemotherapy to inhibit the growth of cancer cells, and most patients with chemotherapy are accompanied by CRF. In addition to less exercise, bed rest, chemotherapy, and other internal and external factors, patients often appear with anxiety, depression, and other negative emotions and varying degrees of cognitive impairment. If the above factors are not effectively resolved or controlled, the cognitive level and quality of life of patients continue to decline, and even aggravate the condition of the patients, forming a vicious cycle. Studies have shown that exercise and psychological intervention could promote the improvement of quality of life in cancer patients[15], and exercise combined with psychotherapy may be an effective intervention to improve CRF in patients with CRC undergoing chemotherapy.
CBT focuses on the relationships between thought, feeling, and behavior, with the goal of reducing stress and fatigue, thereby improving the quality of life of patients. Fitness Qigong Baduanjin, a Chinese traditional Qigong exercise that focuses on a mind-body integration, is considered to be an effective exercise in promoting health. Numerous studies have shown that Baduanjin exercise could effectively relieve physical pain, improve physical function, relieve negative emotions such as anxiety and depression, and have a very good effect on the improvement of cognitive function. It is an effective adjunctive rehabilitation method for cognitive and psychological diseases, and is widely used in clinical practice[16]. A randomized controlled trial has shown that CBT combined with exercise can improve fatigue, sleep disturbance, anxiety, and depression in breast cancer patients[17].
Studies have shown that CRF is a common symptom in about 70% of cancer patients[18]. Fatigue in patients is often more serious than that in healthy groups, and is difficult to alleviate through sleep and rest, causing a major economic burden and mental pressure on patients and their families[19]. At present, there are many studies on the pathogenesis of CRF, among which, the explanation of CRF by 5-hydroxytryptamine (5-HT) disorder has been accepted by most researchers. This mechanism can be divided into two types of CRF: Peripheral and central fatigue[20]. Peripheral fatigue mainly refers to physical fatigue. After cancer patients receive chemotherapy, peripheral nerves can be stimulated to release neuroactive substances, and the vagus afferent nerve can be activated, thus inhibiting skeletal muscle activity. Decrease of skeletal muscle activity leads to physical fatigue. Central fatigue, including emotional and cognitive fatigue, is mainly related to neural bundles and disorders in the brain, especially the increased concentration of 5-HT in the brain[21]. In the present study, the CFS was used to evaluate the degree of CRF, and it was found that body fatigue was most severe in patients undergoing chemotherapy for CRC, and this conclusion is consistent with the research of Jong et al[22]. Studies have confirmed that moderate physical activity has a good effect in improving CRF in patients with CRC, but most of the aerobic exercises used in existing studies are jogging, swimming, cycling, etc., and the efficacy evaluation also focuses on a single time point and lacks periodic efficacy observation. In this study, Chinese traditional healthy Qigong Baduanjin was used to intervene patients with CRC for 6 mo, and the CFS was evaluated at 3 and 6 mo. The results showed that exercise intervention for 3 mo could improve the CRF of CRC patients significantly, among which the improvement of body fatigue was the most obvious, and still had a certain curative effect with the extension of intervention time. Therefore, Baduanjin is a good exercise intervention method for CRF, which is worthy of long-term adherence.
Cancer patients often have cognitive impairment, mainly for memory, attention, and event processing speed[23]. This may be caused by effects of chemotherapeutic drugs on the CNS and nerve cell damage directly, resulting in oxidative stress, inflammatory reaction, and changes in hormone levels, blood supply, and metabolism[24]. However, it should be noted that mild cognitive impairment is not easily detected by the patients themselves, and their families often focus on the recovery of disease symptoms, while the symptoms of CRCI, such as decline in memory and attention, are easily ignored. In this study, the FACT-Cog scale was used to evaluate the cognitive function of CRC patients from multiple dimensions, which showed that, there are different degrees of cognitive impairment in CRC patients; among the dimensions of the scale, the lowest score was for impact on quality of life and cognitive ability, while the highest score was for other people’s evaluation. The reason may be that the cognitive impairment caused by chemotherapy for CRC makes the patients unable to have normal work and social skills, and affect the quality of life ultimately. Studies have shown that physical activities can improve cognitive function in patients, which may be because exercise stimulates the cranial nerves, activates the CNS, prevents brain atrophy, and increases the hippocampal volume, thereby promoting the remodeling of nerve cells and synapses[25]. Furthermore, Ferguson et al[26] found that CBT therapy could improve cognitive dysfunction and the quality of life effectively in breast cancer survivors following chemotherapy. In the present study, after 6 mo of Baduanjin and CBT intervention, the five main dimensions of FACT-Cog scale were improved significantly, and the results are consistent with those of previous studies. To further analyze the effect on the cognitive function of CRC patients, we used P300, which provides objective evidence for the theory that CBT combined with exercise intervention can improve related cognitive dysfunction in patients with CRC chemotherapy. P300 is an effective electrophysiological indicator reflecting cognitive function status. The latency of P300 is often used to reflect short-term memory, selective attention, and reaction speed, the ability to process events, and cognitive processing[27], and the amplitude of P300 reflects the resources invested in the brain when it senses incoming stimulus information, namely, the active control of attention and the ability of information processing. The decrease of P300 amplitude and the prolongation of latency indicate the decline of cognitive ability, and P300 latency is more sensitive to the occurrence of early CRCI than P300 amplitude response, so P300 amplitude and latency can be used as biological markers of cognitive physiological mechanism[28,29]. The present study was completed by auditory stimulation under the oddball paradigm, and the latency of P300 was significantly shortened and the amplitude of P300 was significantly increased in CRC patients receiving 3 mo of CBT combined with exercise intervention, and the difference became more significant with the duration of the intervention. In addition, the above changes were not observed in the control group, which was consistent with the scale evaluation results, confirming the effectiveness of combined intervention for CRCI in this type of disease.
In recent years, the quality of life of patients with CRC during chemotherapy has attracted much attention. Different from the traditional biomedical models, modern medical models do not take tumor elimination as the only goal, and their evaluation of survival rate of cancer patients is more systematic, especially paying attention to the quality of life of patients after surgery and chemotherapy[30]. The concept of quality of life is extremely complex, including physical, psychological, social function, mental state, etc. It reflects the gap between personal expectations and actual living conditions. Research has shown that CRC surgery and chemotherapy cause changes in normal defecation patterns and disorder of self-image, and lead to negative emotions such as anxiety and depression, and then affect the quality of life of patients seriously[31]. In this study, the FACT-C scale was used valuate the quality of life of patients with CRC after chemotherapy, and then we found a general decline in quality of life. For the FACT-C scale, the decline of functional status is the most obvious, followed by physiological status and additional attention score, and the decline of social/family status is relatively small. The reason may be that after cancer chemotherapy, patients get the support and encouragement from family and friends, and get a great emotional release. Physical activities are closely related to the quality of life of CRC patients. A large number of studies have shown that the overall quality of life of patients who participate in physical activities for a long time is significantly higher than that of patients who do not[32]. Baduanjin exercise has been found effective in improving the quality of life and mental health, and reducing stress[33]. Ferguson et al[26] also found that 2 mo of brief cognitive-behavioral therapy intervention could improve the quality of life and verbal memory performance of breast cancer survivors effectively. In this study, we found that the scores of the four dimensions of the FACT-C scale were improved after 3 mo of Baduanjin combined CBT intervention in patients with CRC after chemotherapy, and the quality of life was further improved by 6 mo of intervention. Baduanjin exercise could improve the physical function and CBT could relieve the negative emotion effectively, and they cooperate with each other and play a benign promoting role together.
In this study, we analyzed the correlation between quality of life and CRF and cognitive function in patients undergoing chemotherapy for CRC, and found that patients with more severe CRF had lower quality of life. CRF causes many problems for cancer patients, including daily diet, daily life, leisure and entertainment, normal working ability, etc. The total score of cognitive function and the scores of each dimension are closely related to the total score of quality of life. The reason may be that chemotherapy and other factors lead to the cognitive decline. Cancer patients are often unable to concentrate and their memory declines, which seriously affects their normal social activities. Therefore, it will also have an impact on the quality of life of patients. In our study, the decrease in quality of life of subjects was mainly related to CRF, followed by CRCI. CRF and CRCI caused by cancer chemotherapy have varying impacts on the daily life of patients, leading to a decline in their quality of life. In the rehabilitation of patients with CRC chemotherapy, we should strengthen evaluation of their degree of fatigue, carry out health education in advance, and use CBT combined with Baduanjin as auxiliary rehabilitation therapy, which can prevent and slow down the decline of cognitive function, and ultimately improve quality of life.
Patients with CRC generally have obvious CRF (mainly body fatigue), cognitive impairment, and serious decline in quality of life, which affects their prognosis. CBT combined with Baduanjin exercise can improve fatigue and cognitive impairment of CRC patients undergoing chemotherapy, and improve their quality of life. The quality of life of CRC patients is closely related to their CRF and cognitive level. CBT combined with exercise intervention is worth promoting in the postoperative rehabilitation of cancer patients.
Patients with colorectal cancer (CRC) after chemotherapy are often accompanied with cancer-related fatigue (CRF) and cancer-related cognitive dysfunction, which seriously affects the quality of life and recovery during chemotherapy, but there is no effective treatment.
This study sought to find an effective treatment for cognitive impairment and cancer-related fatigue after chemotherapy for CRC, and to provide a theoretical basis and practical reference for rehabilitation of CRC patients.
This study aimed to explore the effects cognitive behavior therapy (CBT) combined with Baduanjin exercise on CRF, cognitive impairment, and quality of life in patients with CRC after chemotherapy.
Patients with CRC were treated with CBT combined with Baduanjin (experimental group, n = 27) or usual care (control group, n = 28), and then the changes of cancer-related fatigue, cognitive function, quality of life, and P300 amplitude and latency were compared at baseline, 3 mo, and 6 mo.
Compared with the baseline values, the cancer-related fatigue, cognitive function, quality of life, and P300 amplitude and latency were significantly better in the experimental group at 3 mo (P < 0.01). The cancer-related fatigue, cognitive function, quality of life, and P300 amplitude and latency were significantly better in the experimental group than in the control group (experimental group vs control group at 3/6 mo; P < 0.05 or P < 0.01). The quality of life was negatively correlated with cancer-related fatigue and positively correlated with cognitive function.
CBT combined with Baduanjin exercise can improve fatigue and cognitive impairment of CRC patients undergoing chemotherapy, and improve their quality of life. The quality of life of CRC patients is closely related to their CRF and cognitive level. CBT combined with exercise intervention is worth promoting in the postoperative rehabilitation of cancer patients.
This study contributes to the rehabilitation of cognitive impairment and cancer-related fatigue in patients with colorectal cancer after chemotherapy. To confirm and validate the results of this study, a larger scale prospective study would be helpful.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Sport Sciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Eglinton TW, Liebig-Hoerl G S-Editor: Wang JL L-Editor: Wang TQ P-Editor: Yu HG
| 1. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55806] [Article Influence: 7972.3] [Reference Citation Analysis (132)] |
| 2. | Vogelzang NJ, Breitbart W, Cella D, Curt GA, Groopman JE, Horning SJ, Itri LM, Johnson DH, Scherr SL, Portenoy RK. Patient, caregiver, and oncologist perceptions of cancer-related fatigue: results of a tripart assessment survey. The Fatigue Coalition. Semin Hematol. 1997;34:4-12. [PubMed] |
| 3. | Wefel JS, Vardy J, Ahles T, Schagen SB. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 2011;12:703-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 555] [Cited by in RCA: 728] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 4. | Duijts SF, Oldenburg HS, van Beurden M, Aaronson NK. Cognitive behavioral therapy and physical exercise for climacteric symptoms in breast cancer patients experiencing treatment-induced menopause: design of a multicenter trial. BMC Womens Health. 2009;9:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Hu B. Application of Wearable Technology in Clinical Walking and Dual Task Testing. J Transl Int Med. 2019;7:87-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Zhou J, Yu Y, Cao B, Li X, Wu M, Wen T, Xiong Y, Jia J, Zhao Y. Characteristic of Clinical Studies on Baduanjin during 2000-2019: A Comprehensive Review. Evid Based Complement Alternat Med. 2020;2020:4783915. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Lansdorp-Vogelaar I, von Karsa L; International Agency for Research on Cancer. European guidelines for quality assurance in colorectal cancer screening and diagnosis. First Edition--Introduction. Endoscopy. 2012;44 Suppl 3:SE15-SE30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Cheung YT, Lim SR, Shwe M, Tan YP, Chan A. Psychometric properties and measurement equivalence of the English and Chinese versions of the functional assessment of cancer therapy-cognitive in Asian patients with breast cancer. Value Health. 2013;16:1001-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Cheung YT, Shwe M, Chui WK, Chay WY, Ang SF, Dent RA, Yap YS, Lo SK, Ng RC, Chan A. Effects of chemotherapy and psychosocial distress on perceived cognitive disturbances in Asian breast cancer patients. Ann Pharmacother. 2012;46:1645-1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Okuyama T, Akechi T, Kugaya A, Okamura H, Imoto S, Nakano T, Mikami I, Hosaka T, Uchitomi Y. Factors correlated with fatigue in disease-free breast cancer patients: application of the Cancer Fatigue Scale. Support Care Cancer. 2000;8:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 148] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Finnegan-John J, Molassiotis A, Richardson A, Ream E. A systematic review of complementary and alternative medicine interventions for the management of cancer-related fatigue. Integr Cancer Ther. 2013;12:276-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 102] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 12. | Okuyama T, Akechi T, Kugaya A, Okamura H, Shima Y, Maruguchi M, Hosaka T, Uchitomi Y. Development and validation of the cancer fatigue scale: a brief, three-dimensional, self-rating scale for assessment of fatigue in cancer patients. J Pain Symptom Manage. 2000;19:5-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 233] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 13. | Ward WL, Hahn EA, Mo F, Hernandez L, Tulsky DS, Cella D. Reliability and validity of the Functional Assessment of Cancer Therapy-Colorectal (FACT-C) quality of life instrument. Qual Life Res. 1999;8:181-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 350] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 14. | Cruzado J, Sánchez FI, Abellán JM, Pérez-Riquelme F, Carballo F. Economic evaluation of colorectal cancer (CRC) screening. Best Pract Res Clin Gastroenterol. 2013;27:867-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Zhang P, Mo L, Torres J, Huang X. Effects of cognitive behavioral therapy on psychological adjustment in Chinese pediatric cancer patients receiving chemotherapy: A randomized trial. Medicine (Baltimore). 2019;98:e16319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Chan JS, Ho RT, Chung KF, Wang CW, Yao TJ, Ng SM, Chan CL. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evid Based Complement Alternat Med. 2014;2014:106048. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 86] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 17. | Zhang Q, Li F, Zhang H, Yu X, Cong Y. Effects of nurse-led home-based exercise & cognitive behavioral therapy on reducing cancer-related fatigue in patients with ovarian cancer during and after chemotherapy: A randomized controlled trial. Int J Nurs Stud. 2018;78:52-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 18. | Ahlberg K, Ekman T, Gaston-Johansson F, Mock V. Assessment and management of cancer-related fatigue in adults. Lancet. 2003;362:640-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 372] [Cited by in RCA: 364] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 19. | Mohandas H, Jaganathan SK, Mani MP, Ayyar M, Rohini Thevi GV. Cancer-related fatigue treatment: An overview. J Cancer Res Ther. 2017;13:916-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 20. | Ryan JL, Carroll JK, Ryan EP, Mustian KM, Fiscella K, Morrow GR. Mechanisms of cancer-related fatigue. Oncologist. 2007;12 Suppl 1:22-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 362] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 21. | Scott K, Posmontier B. Exercise Interventions to Reduce Cancer-Related Fatigue and Improve Health-Related Quality of Life in Cancer Patients. Holist Nurs Pract. 2017;31:66-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 22. | Jong MC, Boers I, Schouten van der Velden AP, Meij SV, Göker E, Timmer-Bonte ANJH, van Wietmarschen HA. A Randomized Study of Yoga for Fatigue and Quality of Life in Women with Breast Cancer Undergoing (Neo) Adjuvant Chemotherapy. J Altern Complement Med. 2018;24:942-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 56] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 23. | Cruzado JA, López-Santiago S, Martínez-Marín V, José-Moreno G, Custodio AB, Feliu J. Longitudinal study of cognitive dysfunctions induced by adjuvant chemotherapy in colon cancer patients. Support Care Cancer. 2014;22:1815-1823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 24. | Gottschalk LA, Holcombe RF, Jackson D, Bechtel RJ. The effects of anticancer chemotherapeutic drugs on cognitive function and other neuropsychiatric dimensions in breast cancer patients. Methods Find Exp Clin Pharmacol. 2003;25:117-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Cox EP, O'Dwyer N, Cook R, Vetter M, Cheng HL, Rooney K, O'Connor H. Relationship between physical activity and cognitive function in apparently healthy young to middle-aged adults: A systematic review. J Sci Med Sport. 2016;19:616-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 97] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 26. | Ferguson RJ, McDonald BC, Rocque MA, Furstenberg CT, Horrigan S, Ahles TA, Saykin AJ. Development of CBT for chemotherapy-related cognitive change: results of a waitlist control trial. Psychooncology. 2012;21:176-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 152] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 27. | Higuchi Y, Sumiyoshi T, Tateno T, Nakajima S, Sasabayashi D, Nishiyama S, Mizukami Y, Takahashi T, Suzuki M. Prolonged P300 Latency in Antipsychotic-Free Subjects with At-Risk Mental States Who Later Developed Schizophrenia. J Pers Med. 2021;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Hong JS, Lee JH, Yoon YH, Choi JH, Shin JE, Kim SM, Park YG. The assessment of reliability of cognitive evoked potential in normal person. Ann Rehabil Med. 2013;37:263-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Delle-Vigne D, Kornreich C, Verbanck P, Campanella S. The P300 component wave reveals differences in subclinical anxious-depressive states during bimodal oddball tasks: An effect of stimulus congruence. Clin Neurophysiol. 2015;126:2108-2123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Liu M, Sun W, Cai YY, Wu HZ. Validation of Quality of Life Instruments for Cancer Patients - Colorectal Cancer (QLICP-CR) in patients with colorectal cancer in Northeast China. BMC Cancer. 2018;18:1228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, Jemal A, Yu XQ, He J. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66:115-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11444] [Cited by in RCA: 13210] [Article Influence: 1467.8] [Reference Citation Analysis (3)] |
| 32. | Eyl RE, Xie K, Koch-Gallenkamp L, Brenner H, Arndt V. Quality of life and physical activity in long-term (≥5 years post-diagnosis) colorectal cancer survivors - systematic review. Health Qual Life Outcomes. 2018;16:112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 33. | Ho RTH, Wan AHY, Chan JSM, Ng SM, Chung KF, Chan CLW. Study protocol on comparative effectiveness of mindfulness meditation and qigong on psychophysiological outcomes for patients with colorectal cancer: a randomized controlled trial. BMC Complement Altern Med. 2017;17:390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |