Published online Mar 16, 2021. doi: 10.12998/wjcc.v9.i8.2001
Peer-review started: November 26, 2020
First decision: December 24, 2020
Revised: January 2, 2021
Accepted: January 21, 2021
Article in press: January 21, 2021
Published online: March 16, 2021
Processing time: 100 Days and 3.2 Hours
To report the possible reasons for needle perforation and complications related to perforation, as well as the clinical management of subretinal hemorrhage (SRH) during retrobulbar injection.
A 65-year-old female was scheduled to undergo pars plana vitrectomy (PPV) in her left eye for rhegmatogenous retinal detachment (RRD). During retrobulbar anesthesia, needle perforation of the globe occurred. Massive SRH in the inferotemporal quadrant together with vitreous hemorrhage were observed. The patient underwent PPV combined with retinotomy for removal of the massive SRH. After earlier surgical intervention, successful reattachment of the retina was achieved.
Inadvertent globe penetration during retrobulbar anesthesia is associated with a poor prognosis and may result in blindness. Timely detection and earlier intervention may be beneficial.
Core Tip: Inadvertent globe penetration during retrobulbar anesthesia is an uncommon and serious complication. We present a case of needle perforation of the globe during retrobulbar injection. We discuss the results of our literature search for evidence related to reasons for needle perforation and complications related to perforation, as well as the clinical management of subretinal hemorrhage, in an effort to encourage ophthalmologists to pay more attention to this sight-threatening complication. If iatrogenic perforations occur, timely detection and earlier intervention may be beneficial for prognosis.
- Citation: Dai Y, Sun T, Gong JF. Inadvertent globe penetration during retrobulbar anesthesia: A case report . World J Clin Cases 2021; 9(8): 2001-2007
- URL: https://www.wjgnet.com/2307-8960/full/v9/i8/2001.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i8.2001
As a common procedure in ophthalmic practice, retrobulbar injection is performed to deliver agents to the muscle pyramid for anesthesia or treatment. It is generally used for pain relief caused by glaucoma, surgical anesthesia, and postoperative treatment to reduce inflammation and prevent infection. As an invasive practice, retrobulbar injection carries risk for globe perforation, retrobulbar hemorrhage, temporary amaurosis, and life-threatening respiratory arrest[1]. The complications related to globe perforation include retinal toxicity, choroidal hemorrhage, vitreous hemorrhage (VH), retinal tear, retinal detachment (RD), proliferative vitreoretinopathy (PVR)[1,2]. We present a case of subretinal hemorrhage (SRH) due to inadvertent globe perforation during retrobulbar injection. We discuss the results of our literature search for evidence related to reasons for needle perforation and complications related to perforation and the clinical management of SRH in an effort to encourage ophthalmologists to pay more attention to this sight-threatening complication.
A 65-year-old female came to our department with a complaint of severe vision impairment in her left eye for 10 d.
At 10 d before admission, the patient complained of severe vision impairment and dark shadows in the visual field. No symptoms of pain, soreness, or redness in the left eye were described. No history of trauma was reported. During these 10 d, the patient did not receive any treatment.
The patient had a history of hypertension for 2 years, which was controlled by oral antihypertensive agents. She had no history of eye surgery or high myopia.
The patient had no significant personal or family history.
At the time of her admission, the patient underwent a detailed ophthalmic examination that included measurements of preoperative visual acuity and intraocular pressure (IOP), as well as anterior segment evaluation with a slit-lamp microscope and a dilated fundus examination. (Table 1). The axial length of the globe was 22.97 mm.
| Clinical characteristics | Right eye | Left eye |
| Preoperative visual acuity | 20/400 | FC/BE |
| IOP (mmHg) | 13 mmHg | 12 mmHg |
| Anterior segment evaluation | Cataract | Cataract |
| Fundus examination | Macular hole, retinal break | RRD with two quadrants, macula off detachment, two retinal breaks |
Serum laboratory testing, electrocardiography, and chest X-ray were normal.
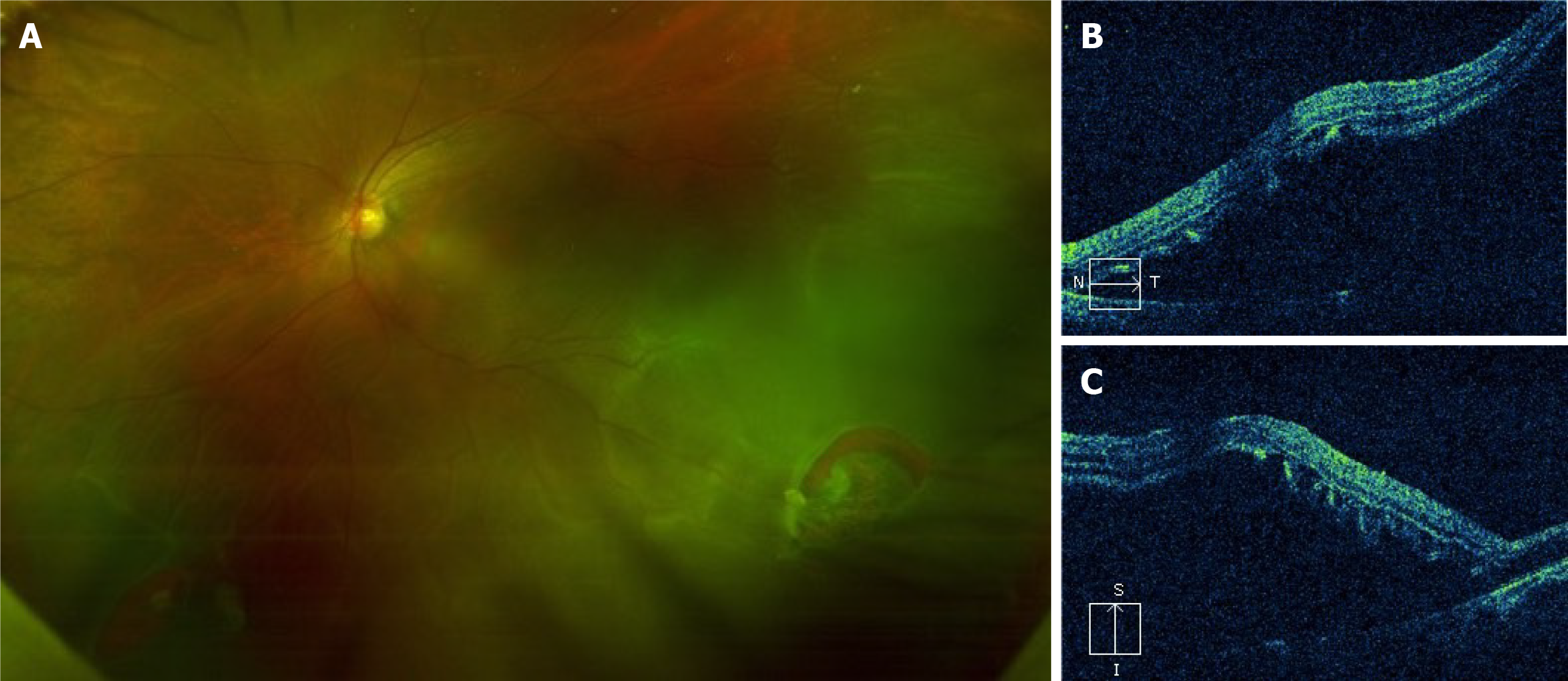
Fundus photography (Figure 1A) and optical coherence tomography (OCT) (Figure 1B and C) revealed this patient had rhegmatogenous retinal detachment (RRD) that extended over two quadrants and included the macula, with retinal breaks at 4 and 7 o’clock on the globe’s equator.
RRD was diagnosed.
This patient was scheduled to undergo pars plana vitrectomy (PPV) on her left eye due to RRD. The treating ophthalmologist noticed some resistance during retrobulbar anesthesia, at the time of needle insertion. Before the injection of ropivacaine, the patient felt severe pain. Subsequently, we observed subconjunctival hemorrhage and an altered red reflex. We considered the possibility of inadvertent globe penetration during retrobulbar injection. An experienced senior ophthalmologist re-administered retrobulbar anesthesia. Three cannulas for PPV were established at 4.0 mm from the corneoscleral limbus in the inferotemporal, superotemporal, and superonasal quadrants. With the help of a noncontact wide-angle viewing system, massive SRH and VH were observed in the inferotemporal quadrant. Needle perforation of the globe during retrobulbar injection was confirmed.
During PPV, we found it was difficult to remove the SRH from the site of retinal break. Thus, it was appropriate to enlarge the retinal break and perform retinotomy for removal of the massive SRH. This procedure involves the use of heavy liquids to flatten the retina and laser photocoagulation in the areas surrounding the retinal breaks and tear. The position of needle entry was approximately 4 disc diameters temporal to the optic disc. After air/fluid exchange and laser photocoagulation, 4.5 mL of silicone oil was injected into the left eye. This patient underwent phacoemulsifi-cation, implantation of an intraocular lens, PPV, retinotomy, removal of the SRH, air/fluid exchange, laser photocoagulation, and silicone oil injection.
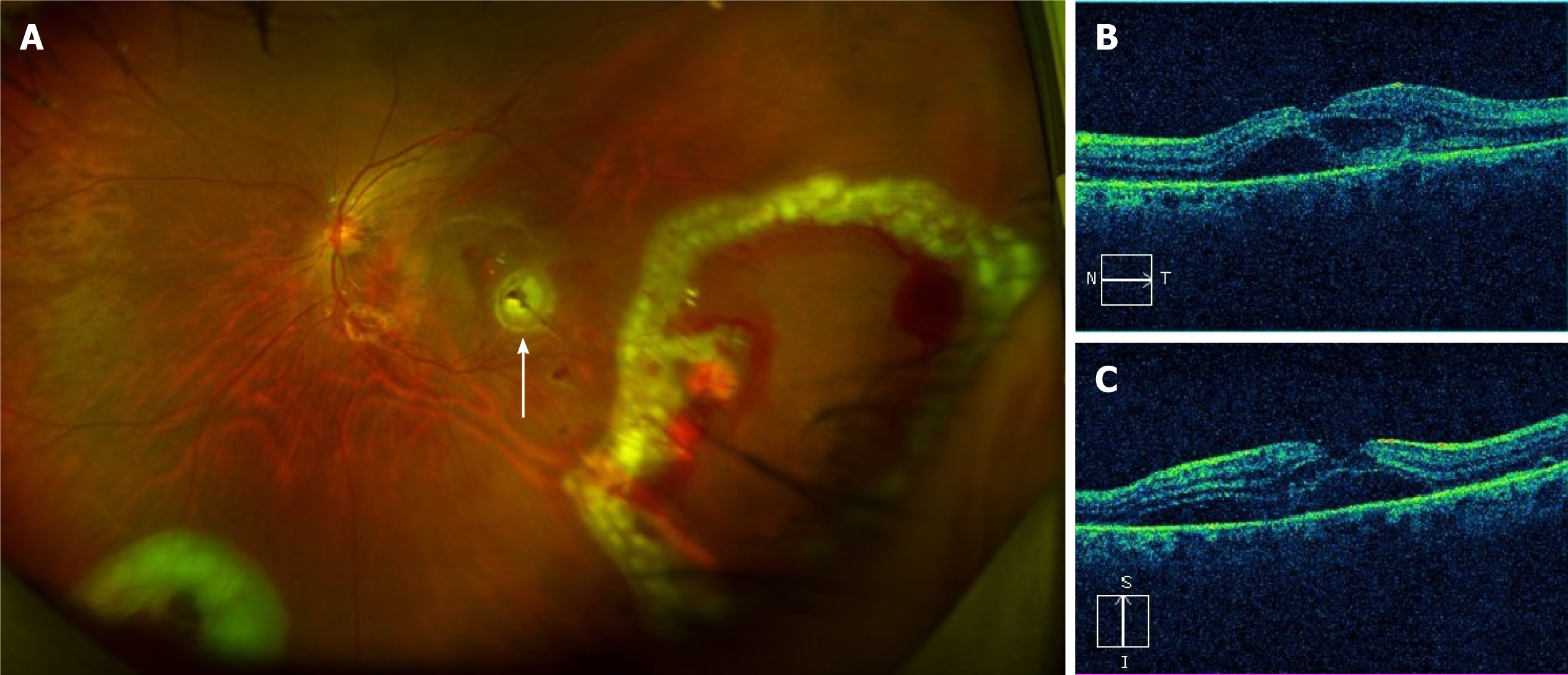
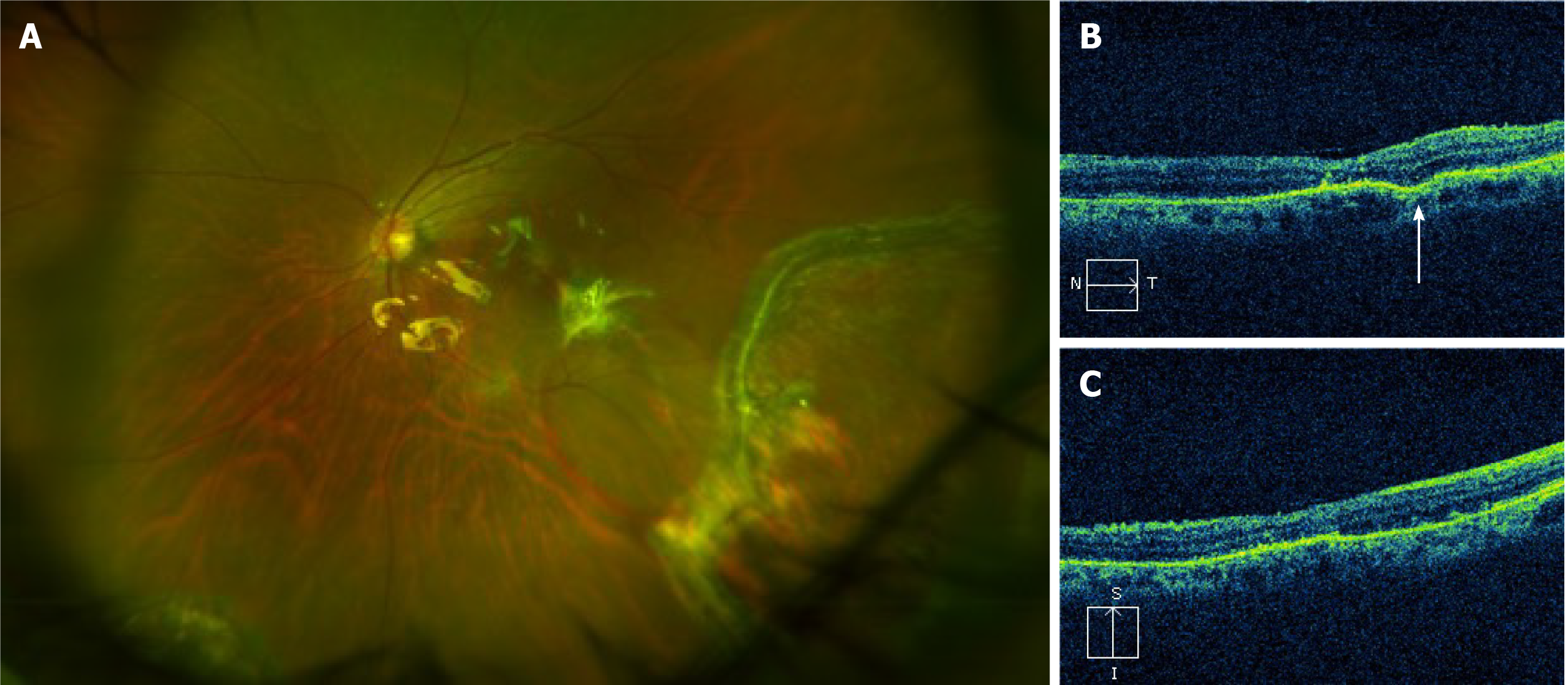
After earlier surgical intervention, successful reattachment of the retina was achieved. On the third postoperative day, fundus photography revealed an attached retina, the position of needle entry, endo-laser spots and minor hemorrhage (Figure 2). At 4 wk postoperatively, the patient’s best-corrected visual acuity (BCVA) improved to 20/250. Further fundus examination showed that the retina remained flat and that the minor hemorrhage had disappeared (Figure 3). At 3 mo, the patient’s BCVA recovered to 20/200. At 5 mo after PPV, the patient underwent silicone oil removal. During the subsequent 6 mo follow-up, the retina remained flat.
Inadvertent globe penetration during retrobulbar injection is an uncommon and serious complication of ophthalmic surgery that is associated with a poor prognosis and, sometimes, blindness. The complications associated with globe penetration include retinal tear, retinal toxicity, choroidal hemorrhage, SRH, VH, RD, and PVR[1,2].
The reported incidence of ocular perforation during retrobulbar anesthesia is approximately 0.075%[3,4]. Scleral perforation associated with retrobulbar anesthesia is more common than scleral perforation associated with peribulbar anesthesia[2]. The perforation rate of peribulbar anesthesia is 0.0062%, so the technique is considered safer, but peribulbar anesthesia is less effective than retrobulbar anesthesia[2,3]. When this complication is recognized, the patient may feel a sharp pain, accompanied by a sudden loss of vision[5]. Early signs of this serious complication include increased IOP and an abnormal red reflex[5]. Usually, needle perforation of the globe requires surgical intervention, such as laser photocoagulation or vitreoretinal surgery.
The causes of inadvertent globe penetration during retrobulbar injection include: The use of long and sharp disposable needles; incorrect angle of needle insertion; poor patient cooperation during surgery; previous history of a scleral buckling operation; high myopia[3]. In order to avoid ocular perforation, general anesthesia is a better alternative for uncooperative patients, such as children or those with neurosis or psychosis. Previous research indicates that highly myopic eyes with longer axial length have higher risk of globe perforation during local anesthesia[2]. The risk of perforation is 10- to 30-fold higher in highly myopic eyes with axial length ≥ 26.0 mm that are otherwise normal[2]. To reduce the risk of globe penetration in highly myopic eyes, it is advisable to use B-ultrasound examination to exclude staphyloma at the injection site preoperatively. Recently, Foad et al[6] explored the accuracy and safety of real-time ultrasound-guided retrobulbar regional anesthesia, as compared with blind technique, for cataract surgery. Foad et al[6] used the Siemens® ACUSON X600™ Ultrasound System. Ultrasound-guided retrobulbar regional anesthesia allows for real-time visualization as the needle advances and as local anesthetic spreads[6]. Foad et al[6] reported that ultrasound-guided retrobulbar injection may decrease risk for sight-threatening or life-threatening complications. However, our patients had no high-risk factors, and in this case, one possible explanation was that the younger surgeon lacked experience, resulting in an incorrect angle of needle insertion.
Iatrogenic perforations may result in iatrogenic retinal tears. In cases of iatrogenic retinal tears without RD or VH, treatment should include laser photocoagulation or cryotherapy. Iatrogenic retinal tears are mostly located in the posterior part of the equator, and inferotemporal breaks are more common[7]. The iatrogenic tear in this case was consistent with this pattern of localization. In cases of the inadvertent intravitreal injection of local anesthetic agents, IOP may suddenly increase, sometimes resulting in central retinal artery occlusion[7]. Medications vary in terms of their retinal toxicity. Liang et al[8] previously investigated the toxicity of various concentrations of intravitreal lidocaine, bupivacaine, and a combination of both in animal models. Reversible changes were observed on electroretinography. No permanent histologic abnormalities were observed[8]. In line with this result, after intravitreally injecting lidocaine (concentration < 0.2%), no obvious functional or histological changes were noted in the cornea or retina of rabbits[9]. Olmez et al[10] explored the effect of intravitreal ropivacaine on retinal thickness and integrity in animal models. More extensive retinal thinning was observed in eyes injected with 0.1 mL of 1% ropivacaine, compared with eyes injected with 0.1 mL of 0.75% or 0.5% ropivacaine[10]. The mean total retinal thickness was lower in the ropivacaine group than in controls. Histopathological analysis revealed structural abnormalities in the retinas of eyes that received 0.1 mL of 0.75% or 1% ropivacaine[10]. The authors hypothesized that the toxic effects of intravitreal ropivacaine on animal retinas were concentration dependent[10]. In this situation, surgical options, such as PPV, should be considered to minimize the retinal toxicity caused by medication.
Perforation signs, such as VH, SRH, and RD were noted. In our case, massive SRH in the inferotemporal quadrant and VH were observed. We sought to determine whether the SRH required surgical intervention. SRH may contribute to photoreceptor damage and vision loss through the following three mechanisms: Toxicity, traction effects, and barrier effects[11]. During the absorption of SRH, the engulfed erythrocytes are metabolized, and hemosiderin is converted to ferritin[11]. The released iron has toxic effects on retinal and choriocapillaris circulation, resulting in photoreceptor and retinal pigment epithelium (RPE) apoptosis[11]. The second mechanism of retinal damage is traction caused by the SRH[11]. During clot retraction, fibrin may contribute to retinal traction[11]. To the best of our knowledge, the RPE is responsible for the transfer of nutrients and metabolites[11]. Furthermore, retinal damage secondary to SRH and the final visual prognosis are time dependent[11]. In addition to SRH duration, SRH thickness is associated with the final visual outcome[11]. In this case, earlier surgical drainage of the SRH appeared to be necessary and was performed to minimize toxin- and barrier-mediated damage.
Currently, various techniques are available for the surgical drainage of SRH, such as pneumatic displacement and PPV combined with retinotomy and tissue plasminogen activator (tPA)-assisted PPV[12]. Retinotomy for clot extraction may result in mechanical damage to the retina and aggravate proliferation. For large and massive SRH, tPA treatment alone is usually insufficient for dissolving the clot[11]. Although tremendous advances in vitreoretinal surgical techniques for the management of SRH have been made over recent decades, there is still no consensus on the optimal approach. In terms of treatment, the preferred approach depends on the duration, size, thickness, and location of the SRH, as well as surgeon preference. For small SRH, the risk-benefit profile suggests that the conservative approach may achieve a satisfactory prognosis[12]. For massive SRH, vitreoretinal specialists are in favor of surgical drainage[12]. Given the massive SRH in this RRD patient, PPV combined with retinotomy was carried out. Because there was enough space between the neurosensory retina and the RPE in this case of RRD, there was less risk for mechanical damage to the retina during the retinotomy for clot extraction. In the future, large randomized controlled trials should be conducted to better evaluate the safety and efficacy of various options for the removal of SRH.
To avoid iatrogenic perforations during local anesthesia, it may be advisable for surgeons to use blunt needles with length of less than 35.0 mm[2]. For retrobulbar anesthesia, 3-4 mL of anesthetic agents should be enough for vitreoretinal surgery. During injection, patients should gaze straight ahead or in the superonasal direction[2]. Of course, before any ophthalmic procedure, the surgeon must consider the patient’s detailed information, such as axial length, to select the appropriate anesthetic approach. Moreover, the risks of retrobulbar anesthesia must be explained to the patient. If iatrogenic perforations occur, timely detection and earlier intervention may be beneficial for prognosis.
Manuscript source: Unsolicited manuscript
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Morya AK S-Editor: Zhang H L-Editor: Filipodia P-Editor: Li JH
| 1. | Han Y, Lam HH, Stewart JM. Endophthalmitis due to inadvertent globe penetration during retrobulbar injection of saline solution for laser in situ keratomileusis. J Cataract Refract Surg. 2009;35:1132-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Schrader WF, Schargus M, Schneider E, Josifova T. Risks and sequelae of scleral perforation during peribulbar or retrobulbar anesthesia. J Cataract Refract Surg. 2010;36:885-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Wadood AC, Dhillon B, Singh J. Inadvertent ocular perforation and intravitreal injection of an anesthetic agent during retrobulbar injection. J Cataract Refract Surg. 2002;28:562-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Ramsay RC, Knobloch WH. Ocular perforation following retrobulbar anesthesia for retinal detachment surgery. Am J Ophthalmol. 1978;86:61-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 132] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Tran KD, Crane AM, Flynn HW Jr. Management of inadvertent needle penetration resulting in subretinal triamcinolone acetonide and retinal detachment. Am J Ophthalmol Case Rep. 2018;10:288-289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Foad AZ, Mansour MA, Ahmed MB, Elgamal HR, Ibrahim HEE, Elawamy A. Real-time ultrasound-guided retrobulbar block vs blind technique for cataract surgery (pilot study). Local Reg Anesth. 2018;11:123-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Gadkari SS. Evaluation of 19 cases of inadvertent globe perforation due to periocular injections. Indian J Ophthalmol. 2007;55:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Liang C, Peyman GA, Sun G. Toxicity of intraocular lidocaine and bupivacaine. Am J Ophthalmol. 1998;125:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Nishide T, Kadonosono K, Itoh N, Yazama F, Endoh Y, Sawada H, Ohno S. The Effect of Intraocular Lidocaine in White Rabbit Eyes. Jpn J Ophthalmol. 2000;44:569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Olmez G, Soker Cakmak S, Ipek Soker S, Nergiz Y, Yildiz F. Effects of intravitreal ropivacaine on retinal thickness and integrity in the guinea pig. Curr Ther Res Clin Exp. 2005;66:394-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Hochman MA, Seery CM, Zarbin MA. Pathophysiology and management of subretinal hemorrhage. Surv Ophthalmol. 1997;42:195-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 128] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Yiu G, Mahmoud TH. Subretinal hemorrhage. Dev Ophthalmol. 2014;54:213-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |