Published online Mar 16, 2021. doi: 10.12998/wjcc.v9.i8.1940
Peer-review started: November 5, 2020
First decision: December 28, 2020
Revised: January 8, 2021
Accepted: January 22, 2021
Article in press: January 22, 2021
Published online: March 16, 2021
Processing time: 120 Days and 1.4 Hours
Nasolacrimal duct obstruction leading to epiphora is a common ophthalmologic complaint, and it may derive from amyloidosis in rare cases. There are a few reports about localized amyloidosis, and amyloidosis with involvement and obstruction of the nasolacrimal duct is exceedingly rare.
A 54-year-old male presented with a 2-year history of a lump overlying the left lacrimal sac that had grown rapidly for nearly half a year. Physical examination touched a firm lump in the left lacrimal sac. Nasal endoscopy discovered lesions in appearance of sediments with easy bleeding at the entry of the nasolacrimal duct of the left inferior nasal meatus. Computerized tomography scan revealed speckle high density in the left lacrimal sac and the dilated nasolacrimal duct. During an endoscopic exploration and excision, a large number of dacryoliths were exposed. Pathology indicated amorphous pink material and multinucleated giant cell reaction in the fibrous tissue.
This case showed amyloidosis in localized form mimicking dacryolith with nasolacrimal duct obstruction. In clinical practice, we should be aware of the possibility of localized amyloidosis in the nasolacrimal excretory system.
Core Tip: Localized amyloidosis is a very rare cause of nasolacrimal duct obstruction and dacryocystitis. It has been reported that amyloidosis in nasolacrimal excretory system may be invasive or present as a pseudo-dacryolith with clear boundary in liquid or colloidal forms. However, massive dacryolithiasis can also be formed and obstruct the nasolacrimal excretory system as a consequence. Computed tomography examination can be a noninvasive tool for preoperative evaluation in case of incapability of dacryocystorhinostomy and nasal endoscopy of fully displaying deeper structures of nasolacrimal excretory system.
- Citation: Che ZG, Ni T, Wang ZC, Wang DW. Computed tomography imaging features for amyloid dacryolith in the nasolacrimal excretory system: A case report. World J Clin Cases 2021; 9(8): 1940-1945
- URL: https://www.wjgnet.com/2307-8960/full/v9/i8/1940.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i8.1940
Amyloidosis can present in either localized or systemic forms. The former form is relatively rare and may involve the head and neck[1,2] without systemic manifestations. Amyloidosis involving the nasolacrimal excretory system is an exceedingly rare condition. Only a few related case reports have been published[3-5] and partly differ from this case. Marcet et al[3] described amyloidosis localized to a lacrimal sac and duct with nasolacrimal duct obstruction (NLDO) but causing bony erosion. Levine et al[4] found a dacryolith-mimicking lesion occupying the lacrimal duct without NLDO. The case described here presents partially mutual features of the previous cases.
The patient was a 54-year-old male who came to our hospital with a chief complaint of a 2-year history of a lump overlying the left lacrimal sac. The patient was admitted to the Ophthalmology Department on September 18, 2018.
Patient’s symptoms started 2 years ago with a lump overlying the left lacrimal sac, which had grown rapidly for nearly half a year.
The patient had a free previous medical history.
The patient had no family history.
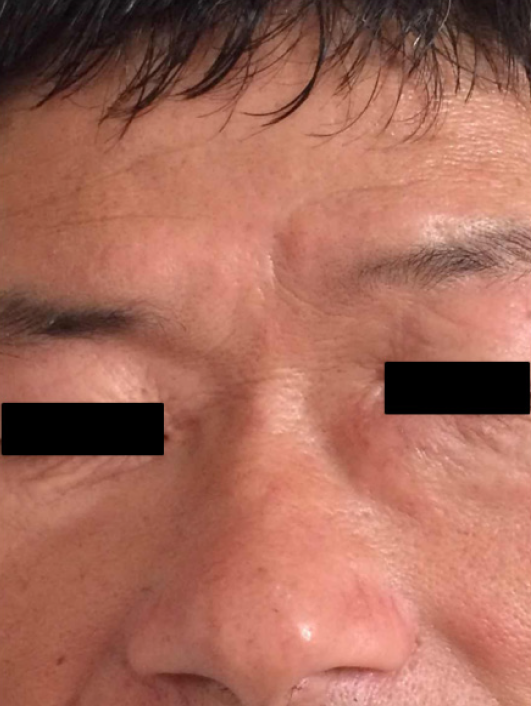
A 1.5 cm × 1.5 cm firm lump in the left lacrimal sac was touched with no secretion or swelling (Figure 1). The left upper and lower lacrimal duct had a smooth irrigation of 100% reflux. Nasal endoscopy discovered lesions in appearance of sediments with easy bleeding at the entry of the nasolacrimal duct of the left inferior nasal meatus.
Total proteins were slightly lower, and no other abnormalities were found.
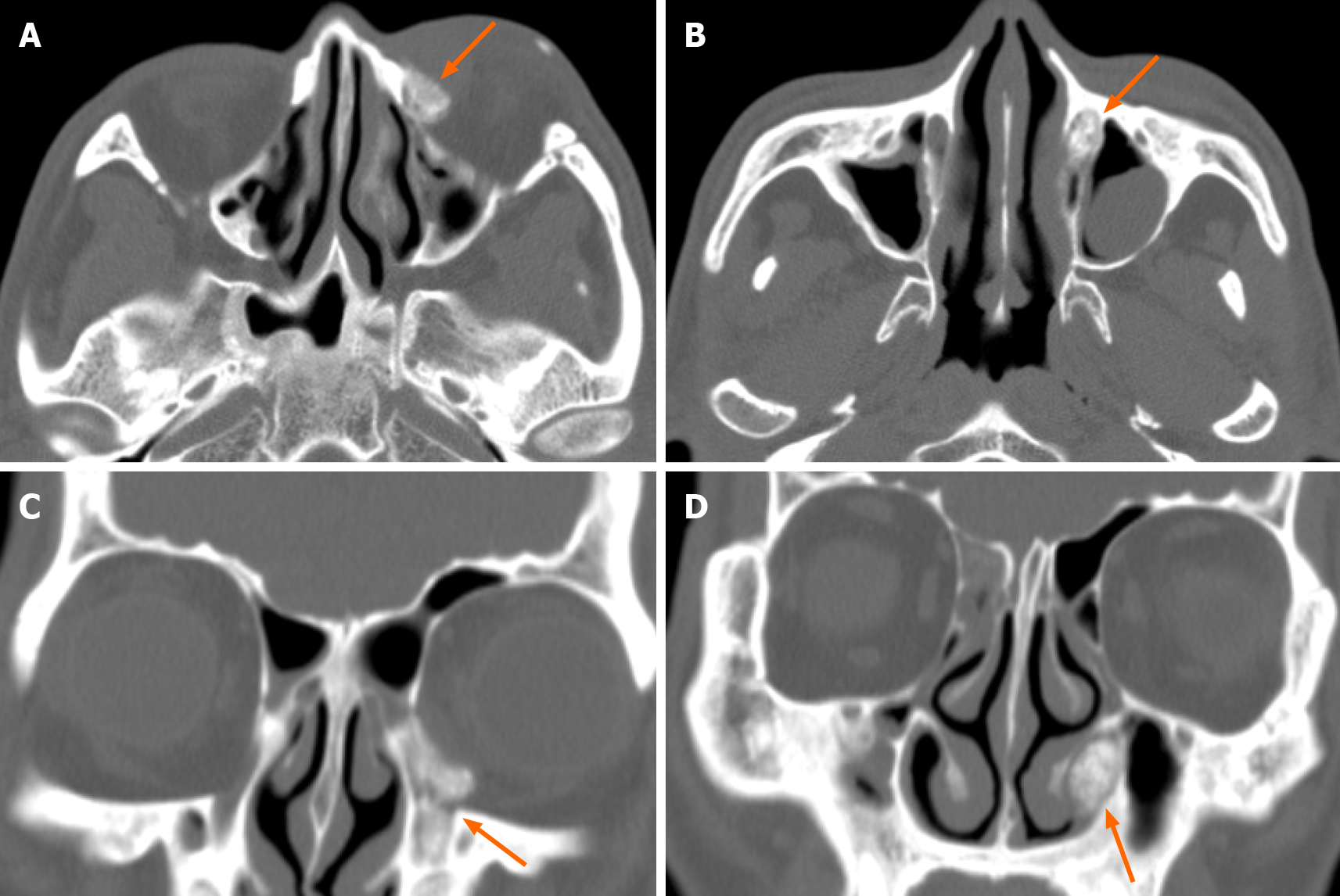
The non-contrast enhanced computed tomography (CT) imaging of paranasal sinuses showed that the left lacrimal duct blocked. The maximum cross section of the soft tissue density observed in the left lacrimal sac was about 1.6 cm × 1.4 cm, which extended downward to the obviously dilated nasolacrimal duct (Figure 2).
An endoscopic exploration and excision was performed for the left lacrimal sac under general anesthesia, with nasolacrimal duct dredging.
The final diagnosis of the presented case is amyloidosis in the nasolacrimal excretory system.
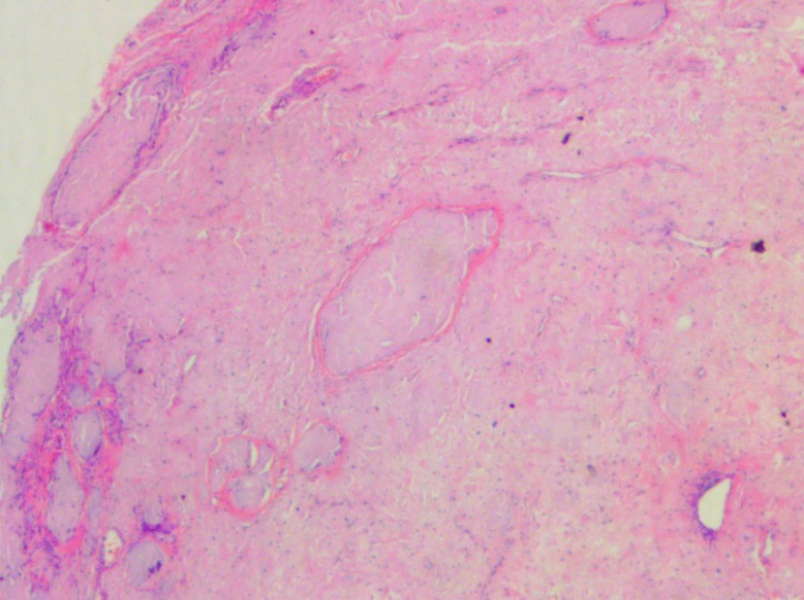
On September 20, 2018, an endoscopic exploration and excision was performed for the left lacrimal sac under general anesthesia, with nasolacrimal duct dredging. The mucoperiosteal flap and window were made on the lateral wall of the nasal cavity. A large number of dacryoliths were exposed and scraped out by curette, with a larger one about 1.5 cm in size (Figure 3). Cleaning up the lower meatus and dredging the nasolacrimal duct were conducted under nasal endoscopy. Then the hemostatic sponge filled the left nasal cavity. Surrounding tissues were separated layer by layer under subcutaneous infiltration anesthesia. The lesion had an intact capsule and smooth surface indicating it was noninvasive. After completely removed and dissected, the lesion had a yellow solid component.
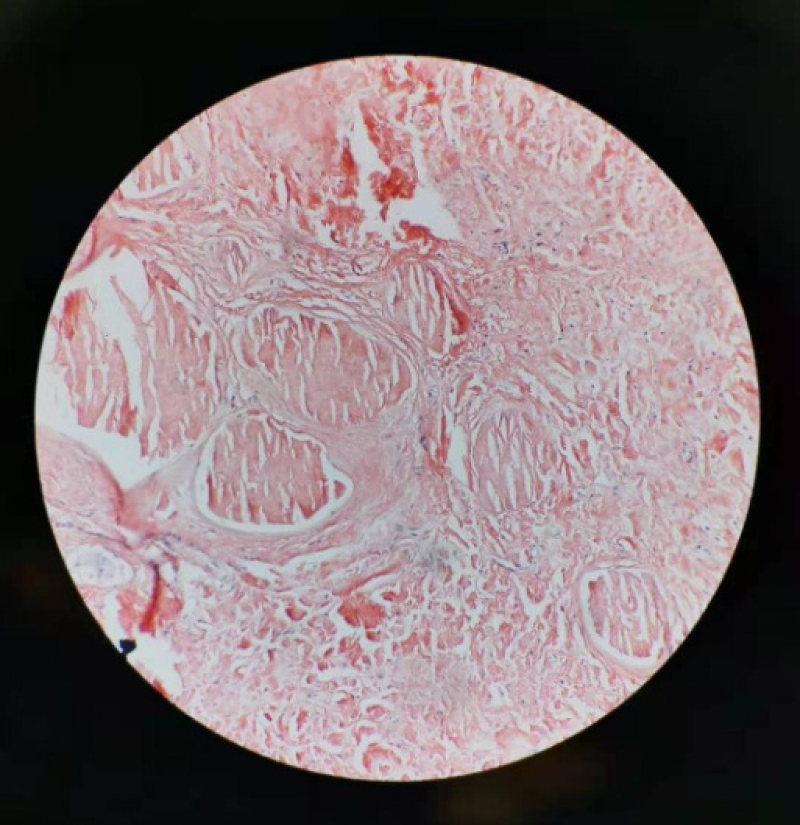
Pathological results showed (orbital) nodular amyloidosis with giant cell foreign body reaction, calcification and ossification (Figure 4). Congo red staining was further conducted, showing that homogeneous orange material without structure in coarse granular, massive, nodular forms on Congo red staining (Figure 5). The patient was followed up through telephone interview. No new lesions appeared, and the current condition of the patient is good.
Amyloid is a pathologic fibrillar aggregation of polypeptides in a cross-β-sheet conformation. Amyloidosis is caused by the deposition of amyloid and may represent either localized or systemic disease. The etiology of amyloidosis is still unknown. The possible mechanisms that have been reported are as follows: (1) Immune disorders and chronic inflammatory stimuli lead to protein metabolism disorders associated with accumulation of insoluble amyloid protein fibers in submucosa, vascular wall and connective tissue, resulting in dysfunction of structures; (2) Degeneration. Amyloid deposits as local internal component of neoplasm (such as polyps) degenerate; (3) Family genetic correlation; (4) Systemic immunodeficiency; and (5) Amyloidosis associated with multiple myeloma; etc[6,7].
Although uncommon, amyloidosis may affect almost any anatomic structure. Periocular and orbital amyloidosis have all been reported[1,2]. Amyloid localized to the nasolacrimal excretory system is exceedingly rare. In 2006, a case reported localized amyloidosis causing NLDO[3]. Another case published in 2016 was associated with amyloidosis mimicking a dacryolith and involving the lacrimal duct[4]. In this case, amyloidosis involved the whole nasolacrimal excretory system and formed large dacryoliths. CT scan showed soft tissue density and speckle high density with a wide range from lacrimal sac and nasolacrimal duct to the inferior nasal meatus. Pathological results indicate (orbital) nodular amyloidosis with giant cell foreign body reaction, calcification and ossification. Because of the wide range of occupation, as mentioned previously, neither dacryocystorhinostomy nor endoscopic approach could thoroughly and completely remove the lesions. Thus, a combination was adopted with nasolacrimal duct dredging. The patient had a 2-year disease course and a rapid development within 6 mo. This demands differentiation of common chronic inflammation such as granulomatous lesions and awareness of potential possibility of lacrimal sac tumor[8]. Rare diseases such as sarcoidosis[9] could not be completely excluded; neither could amyloidosis be proven in this case. Massive calcification on CT imaging is not typical of granulomatous lesions, while the feathers of clear border, the way of a fit-in growth and dilation of nasolacrimal duct without bone erosion do not correspond with malignancy.
Localized amyloidosis is a very rare cause of NLDO and dacryocystitis. It has been reported that amyloidosis in nasolacrimal excretory system may be invasive or present as a pseudo-dacryolith with clear bounder in liquid or colloidal forms. However, massive dacryolithiasis can also be formed and obstruct the nasolacrimal excretory system as a consequence. CT examination can be a noninvasive tool for preoperative evaluation in case of incapability of dacryocystorhinostomy and nasal endoscopy of fully displaying deeper structures of nasolacrimal excretory system. Once found, the whole course nasolacrimal involvement can be managed by the combination of traditional surgical operation and endoscopy.
This case described amyloidosis in localized form mimicking dacryolith with NLDO. In clinical practice, we should be aware of the possibility of localized amyloidosis in the nasolacrimal excretory system.
Manuscript source: Unsolicited manuscript
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ge Y S-Editor: Zhang H L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Leibovitch I, Selva D, Goldberg RA, Sullivan TJ, Saeed P, Davis G, McCann JD, McNab A, Rootman J. Periocular and orbital amyloidosis: clinical characteristics, management, and outcome. Ophthalmology. 2006;113:1657-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 102] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 2. | Medel Jiménez R, Sánchez España JC, Vasquez LM, Tapia Bahamondes A, Rondón M, Francesc T, Barroso EA. Orbital and peri-orbital amyloidosis: a report of four cases. Orbit. 2019;38:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Marcet MM, Roh JH, Mandeville JT, Woog JJ. Localized orbital amyloidosis involving the lacrimal sac and nasolacrimal duct. Ophthalmology. 2006;113:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Levine MR, Seipel SB, Plesec TP, Costin BR. Amyloid Pseudo-Dacryolith and Nasolacrimal Obstruction in a 67-Year-Old Male. Ophthalmic Plast Reconstr Surg. 2017;33:e86-e88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Geller E, Freitag SK, Laver NV. Localized nasopharyngeal amyloidosis causing bilateral nasolacrimal duct obstruction. Ophthalmic Plast Reconstr Surg. 2011;27:e64-e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Kumar B, Pant B, Kumar V, Negi M. Sinonasal Globular Amyloidosis Simulating Malignancy: A Rare Presentation. Head Neck Pathol. 2016;10:379-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Hazenberg BP. Amyloidosis: a clinical overview. Rheum Dis Clin North Am. 2013;39:323-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 8. | Koturović Z, Knežević M, Rašić DM. Clinical significance of routine lacrimal sac biopsy during dacryocystorhinostomy: A comprehensive review of literature. Bosn J Basic Med Sci. 2017;17:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Nassif SJ, Ruiz D, Callahan A, Rebeiz EE. Nasolacrimal Duct Obstruction: An Unusual Presentation of Sarcoidosis. Ear Nose Throat J. 2020: 145561320950494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |