Published online Mar 16, 2021. doi: 10.12998/wjcc.v9.i8.1909
Peer-review started: October 12, 2020
First decision: January 7, 2021
Revised: January 12, 2021
Accepted: January 25, 2021
Article in press: January 25, 2021
Published online: March 16, 2021
Processing time: 142 Days and 8.8 Hours
The causes of peroneal neuropathy are various, but are rarely due to weight loss. Bilateral peroneal neuropathy caused by weight loss after surgery has been reported only after bariatric surgery and there were no reports associated with other abdominal surgery. In this report, we describe a case of the bilateral peroneal neuropathy that occurred due to marked weight loss after biliary surgery.
A 58-year-old male did not receive adequate nutritional support after biliary surgery, and showed a massive weight loss over a short period of time (body mass index; 24.1 kg/m2 to 20.5 kg/m2 for 24 d). Then, foot drop occurred on both sides. Physical examination, electromyography (EMG) and magnetic resonance imaging studies were conducted and he was diagnosed as bilateral common peroneal neuropathy around the fibular head level. The patient was treated electrical stimulation therapy on both lower legs along with exercise therapy, and received sufficient oral nutritional support. The patient gradually recovered to his original weight, and the power of the dorsiflexor of bilateral ankles improved after conservative treatment. In addition, the follow-up EMG showed signs of improvement.
Any abdominal surgery that may have rapid and marked weight loss can lead to peroneal neuropathy as a complication.
Core Tip: Slimmer's paralysis is peroneal neuropathy caused by excessive weight loss such as bariatric surgery, anorexia nervosa or intentional diet, and most of them are unilateral neuropathy. Although it may appear as bilateral paralysis infrequently, there have been no reports that bilateral peroneal neuropathy occurred after abdominal surgery other than bariatric surgery. As shown in this case report, bilateral slimmer's paralysis may occur in any abdominal surgery where excessive weight loss is expected if sufficient nutritional support after surgery is not provided. Therefore, more attention should be paid to the nutritional management of the patient after any abdominal surgery.
- Citation: Oh MW, Gu MS, Kong HH. Bilateral common peroneal neuropathy due to rapid and marked weight loss after biliary surgery: A case report. World J Clin Cases 2021; 9(8): 1909-1915
- URL: https://www.wjgnet.com/2307-8960/full/v9/i8/1909.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i8.1909
Peroneal neuropathy is one of the most common form of mononeuropathy in the lower extremities, accounting for approximately 15% of all mononeuropathies in adults[1]. The known causes of damage to the peroneal nerve are trauma, external compression, or traction injuries[2]. In addition, nerve damage caused by tumors or cysts in the course of the peroneal nerve can be considered[3]. Though rare, systemic diseases such as paraneoplastic syndrome, hyperthyroidism, and diabetes mellitus (DM) can also cause peroneal neuropathy[4]. Since Schott et al[5] first reported a case of peroneal neuropathy after excessive weight loss in a patient with anorexia nervosa, peroneal neuropathy after weight loss has been often reported and called slimmer’s paralysis[6].
Most reported cases of slimmer’s paralysis were caused by weight loss after bariatric surgery, anorexia nervosa or intentional diet, and most of them are unilateral neuropathy[3,6-9]. Occasionally, bilateral peroneal neuropathy has been reported, but this was also due to the aforementioned causes[4,10]. However, no cases of bilateral peroneal neuropathy due to weight loss after abdominal surgery other than bariatric surgery have been reported[8]. In this report, we describe our experience of diagnosing and treating bilateral common peroneal neuropathy due to rapid and marked weight loss that occurred shortly after biliary surgery.
A 58-year-old male was referred to the department of rehabilitation medicine for an electromyography (EMG) study for symptoms of bilateral foot drop that appeared 25 d after the first biliary surgery.
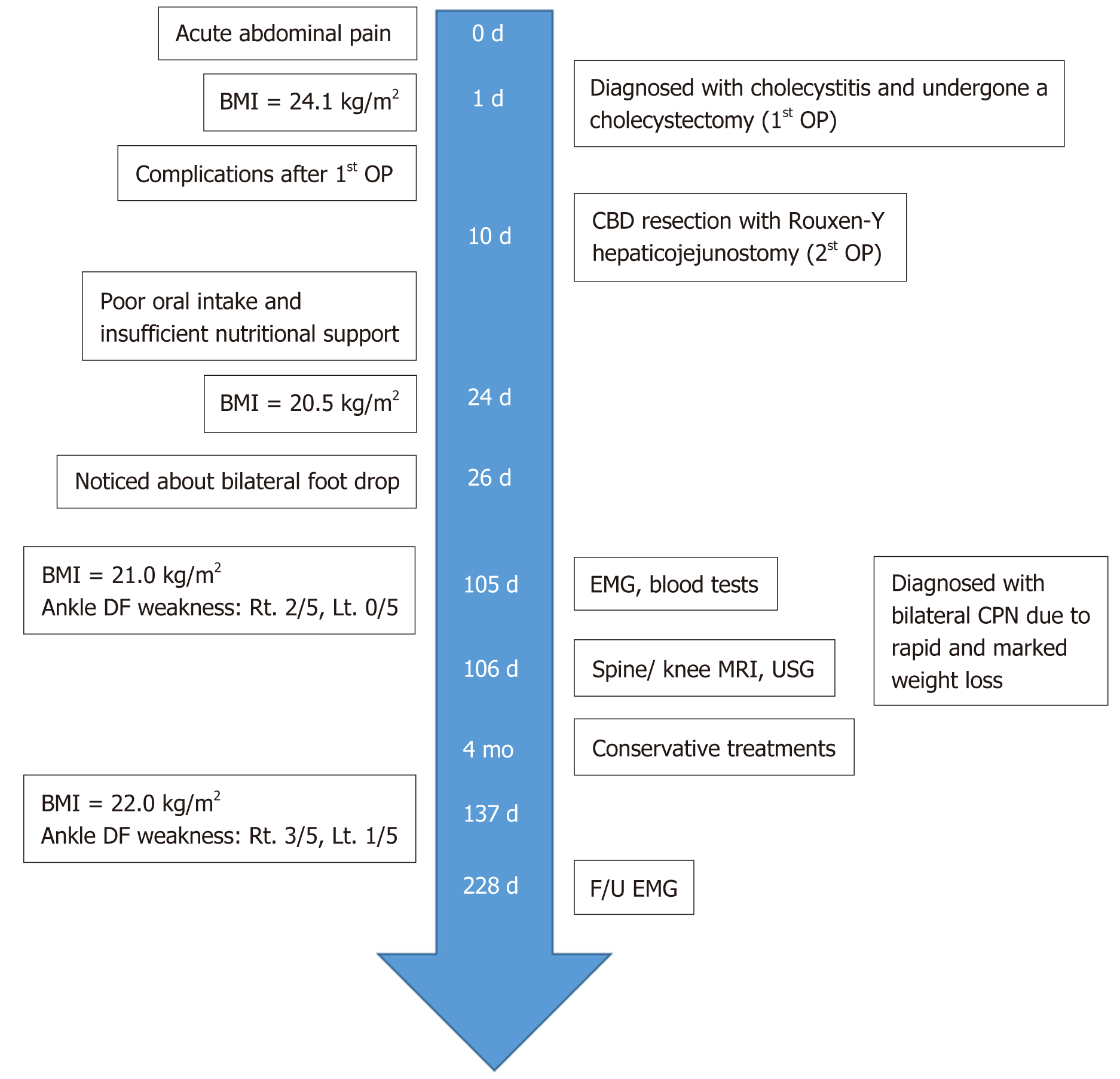
The patient was diagnosed with acute cholecystitis and then underwent a laparoscopic cholecystectomy. Nine days after the first operation, the patient developed complications and underwent second common bile duct resection with Roux-en-Y hepaticojejunostomy. During the hospitalization for the two surgeries, the patient had no unconscious time other than surgery. After the two operations, however, he rarely ate oral meals for approximately 10 d because of nausea, vomiting, and anorexia; instead, he received conservative treatment only with Hartman solution or dextrose fluid, and thus lost weight rapidly. Before the surgery, the patient was 168 cm tall and weighed 68 kg [body mass index (BMI), 24.1 kg/m2], but after the two surgeries, his body weight was reduced to 58 kg for 24 d (0.42 kg/day; BMI, 20.5 kg/m2).
After the second operation, early ambulation was recommended, but during the first postoperative week, he was unable to walk properly because of the pain of operation site and discomfort caused by the tube inserted in his body. When he tried walking in the ward 2 wk after the operation, but he noticed that both ankles, especially the left ankle, were dragged, accompanied by numbness in both feet.
There was no illness in previous medical history.
No abnormalities.
In a physical examination before the EMG study on the 105th day after the first operation, the patient showed the obvious bilateral weakness of ankle dorsiflexor (right: 2/5 and left: 0/5), big toe extensor (right: 1/5 and left: 0/5), and foot everter (right: 2/5 and left: 0/5). In addition, the sensation was decreased in the anterolateral aspect of the calf, the dorsal surface of the foot, and the first web space of foot. Tinel’s sign was positive in the area around both fibular heads.
In the motor nerve conduction study, the amplitude of the deep peroneal nerve recorded in the extensor digitorum brevis was reduced on both sides as compared with the normal lower limits, and conduction block on the area around both fibular heads was found using the “inching” technique. The amplitude of the compound motor action potential (CMAP) measured in the tibialis anterior was also significantly reduced on the left side. In the sensory nerve conduction study, no action potential was induced in the left superficial peroneal nerve (Table 1). On the needle EMG, abnormal spontaneous activity was observed in both tibialis anterior, peroneus longus, and extensor digitorum brevis. In particular, no motor unit action potential was observed in the left tibialis anterior during contraction. All the other nerve conduction studies (median, ulnar, tibial, and sural nerves) showed normal findings. The EMG study was consistent with bilateral common peroneal neuropathy around the fibular heads. In addition, blood tests were conducted to detect DM, thyroid dysfunction, vitamin (B1, B6, and B12) deficiency, or folate deficiency, which may cause non-compressive peroneal neuropathy; however, all test results were normal.
| Stimulation nerve (Stimulation site) | Recording site | Latency1 (ms) | Amplitude2 (mV or μV) | Conduction velocity3 (m/s) |
| Deep peroneal nerve (motor) | ||||
| Right ankle | EDB | 4.55 | 2.2 | 33.2 |
| Right fibular head | EDB | 14.35 | 0.6 | |
| Right fibular head | TA | 3.55 | 1.0 | - |
| Left ankle | EDB | 4.25 | 1.1 | 34.9 |
| Left fibular head | EDB | 14 | 0.1 | |
| Left fibular head | TA | 4 | 0.3 | - |
| Superficial peroneal nerve (sensory) | ||||
| Right fibular head | Ankle | 3.20 | 12.4 | - |
| Light fibular head | Ankle | NR | NR | - |
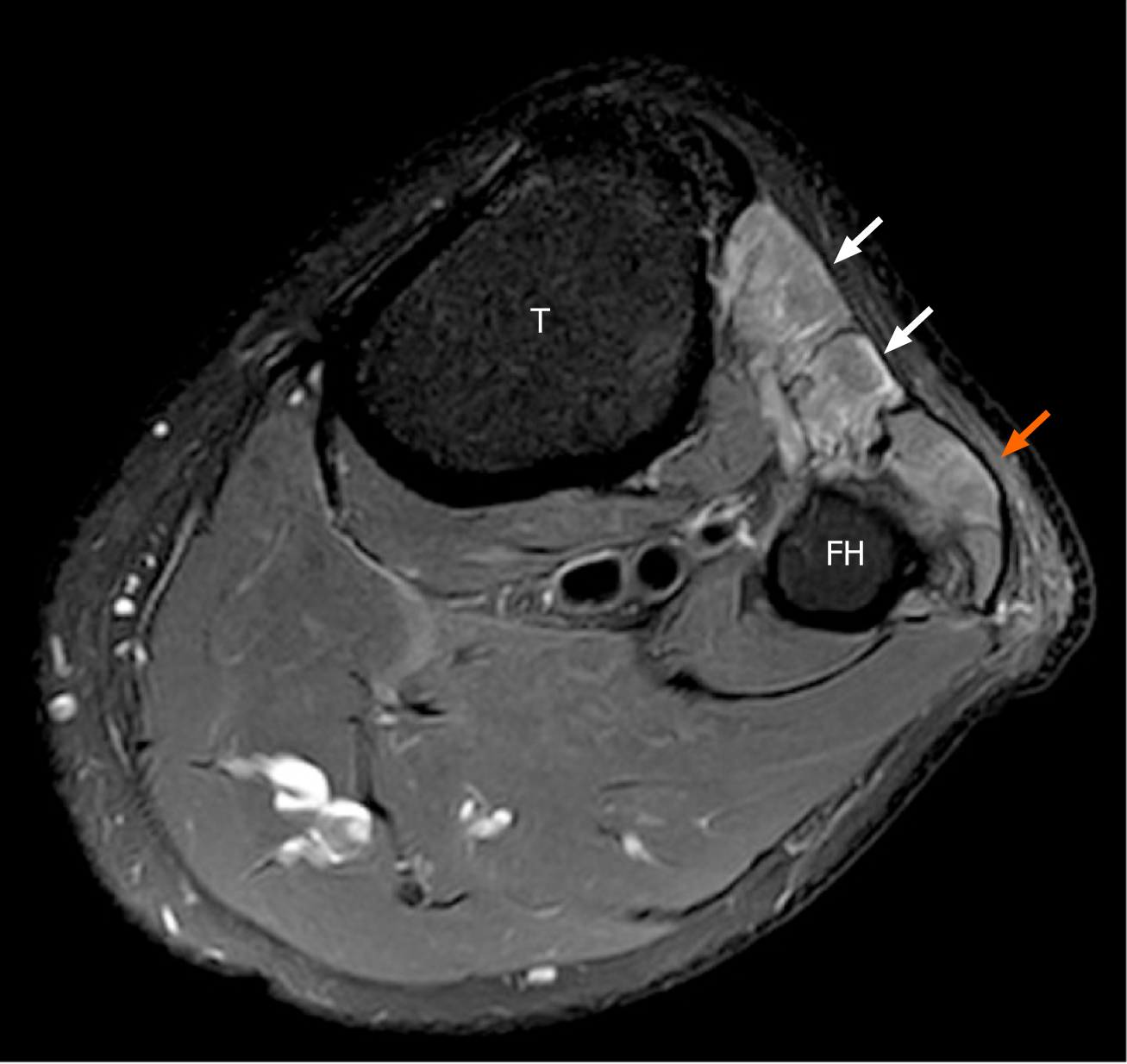
There were no abnormal findings on magnetic resonance image (MRI) study of the lumbar spine that was performed to rule out the possibility of paralysis of both lower extremities due to lumbosacral lesions. Ultrasonography revealed no tumors or cysts along the course of the sciatic nerve and peroneal nerve from the hip to the lower leg.
On left knee MRI, no structure was found around the fibular head that could cause entrapment of the peroneal nerve, and volume loss and edema were observed with the signal change by the nerve denervation in the anterior and lateral muscular compartments of the left lower leg (Figure 1).
Taking into account all medical history, physical examinations and diagnostic tests, the patient was diagnosed with bilateral common peroneal neuropathy due to rapid and marked weight loss during a short-term period.
The patient was treated with electrical stimulation on both lower legs to prevent muscle atrophy and underwent basic rehabilitation (range-of-motion and strengthening exercise). In addition, the patient received sufficient oral nutritional support through nutritional consulting.
After 4 wk of conservative treatment, his weight recovered to 62.2 kg (BMI, 22.0 kg/m2). On physical examination, dorsiflexion in both ankles had recovered (right: 3/5 and left: 1/5). At 228 d after the first operation, follow-up EMG revealed significantly increased amplitude of the CMAP measured in the extensor digitorum brevis and tibialis anterior in both legs. The overall recruit pattern was also improved in the needle EMG. The timeline of this case is shown in Figure 2.
This is the first case report of bilateral common peroneal neuropathy caused by rapid and marked weight loss after biliary surgery. Weight loss is one of various causes of peroneal neuropathy[4,11]. Since cases of peroneal neuropathy in patients with anorexia nervosa were reported[5], there have been several reports of peroneal neuropathy caused by weight loss (slimmer’s paralysis)[6]. However, most cases were peroneal neuropathy that developed after anorexia nervosa, bariatric surgery for obesity, and rapid intentional weight loss[3,5-7,9].
The common peroneal nerve emerges from the sciatic nerve and travels around the fibular neck. The area around the fibular head is not protected by muscles or soft tissue, and is very thin, which makes the peroneal nerve around this area prone to damage[12,13]. Although it is unclear what mechanisms of weight loss cause peroneal neuropathy, one hypothesis is that rapid weight loss can result in decreased adipose tissue around the fibular head, which makes the peroneal nerve vulnerable to damage by compression[14]. Another hypothesis is that rapid weight loss causes a nutritional deficit that results in neuropathy[3].
The extent of weight loss required to cause peroneal neuropathy has not been elucidated yet. Weyns et al[9] reported that peroneal nerve palsy can occur when body fat decreases by > 10%, and Shahar et al[15] showed that rapid weight loss is associated with peroneal neuropathy. The patient in this case had an average body weight (BMI, 24.1 kg/m2), but he lost 10 kg for 24 d (0.417 kg/d; BMI, 20.5 kg/m2) because of the insufficient nutritional support after two surgeries. It was not known exactly what mechanism peroneal neuropathy developed in this patient. Altogether, the results of the various tests performed for differential diagnosis suggested that the patient had bilateral compressive peroneal neuropathy around the fibular head due to the rapid and marked weight loss.
If a patient experiences foot drop symptoms, not only peroneal neuropathy but also sciatic neuropathy, lumbosacral plexopathy, L5 radiculopathy and peripheral polyneuropathy should be included in the list of differential diagnoses[2]. In particular, a deficiency of vitamins (B1, B6, B9, and B12) and minerals can cause peripheral polyneuropathy, and dietary modifications such as supplementation of insufficient nutrients can help recovery. However, it is difficult to suppose that the deficiency of micronutrients was the cause of paralysis in this patient because the blood test for micronutrients was in the normal range. And the patient also showed abnormal findings with a pattern of focal mononeuropathy in the EMG study, unlike polyneuropathy which is generally seen in nutritional neuropathy[16]. In addition, hereditary neuropathy with liability to pressure palsy, an autosomal dominant disease, should be differentiated especially in younger patients with symptoms of paralysis after trivial trauma or weight loss[17]. Although a genetic test was not performed, our patient had no relevant family history and showed normal findings in the nerve conduction study for both upper limbs.
Common peroneal neuropathy that occurs after any surgery, except bariatric surgery, is rare and usually associated with lithotomy positions such as gynecological surgery[18,19]. Prolonged lithotomy positions are known to produce peroneal nerve palsy because of compression of the peroneal nerve running behind the knee. However, because both surgeries were performed in the supine position, bilateral peroneal neuropathy was not possible in this case. Prolonged immobilization is also known to cause peroneal neuropathy[20], but our patient did not have a long immo-bilization period and attempted early ambulation immediately after surgery.
Patients with adequate nutritional support after surgery have better outcomes in terms of complications, hospitalization duration, and mortality than those who do not[21,22]. If oral or enteral feeding is not sufficient, intravenous supplementation should be considered[23]. In our patient, weight loss occurred because of the poor oral nutrition and insufficient parenteral nutrition supplement after the two surgeries.
In most cases, peroneal neuropathy caused by weight loss generally has a good prognosis after conservative management[3,24]. In other words, it is known to recover when rehabilitation treatment is performed along with nutritional support for weight gain, and the patient in this case also recovered after conservative management.
In conclusion, care should be taken to prevent peroneal neuropathy due to weight loss not only for patients undergoing bariatric surgery but also for those undergoing any surgery that can induce rapid and marked weight loss.
Manuscript source: Unsolicited manuscript
Specialty type: Rehabilitation
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kung WM S-Editor: Zhang H L-Editor: A P-Editor: Zhang YL
| 1. | Cruz-Martinez A, Arpa J, Palau F. Peroneal neuropathy after weight loss. J Peripher Nerv Syst. 2000;5:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 2. |
Bayrak İK, Oytun Bayrak A, Türker H, Akpınar ÇK, Bolat N.
Diagnostic value of ultrasonography in peroneal neuropathy |
| 3. | Martín G, Pérez Moro O, Diez-Ramos F, Fernández-Cuadros ME. Nerve Compresion Secondary to Weight Loss. Int J Neurorehabilitation. 2016;3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Margulis M, Ben Zvi L, Bernfeld B. Bilateral Common Peroneal Nerve Entrapment After Excessive Weight Loss: Case Report and Review of the Literature. J Foot Ankle Surg. 2018;57:632-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Schott GD. Anorexia nervosa presenting as foot drop. Postgrad Med J. 1979;55:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Sotaniemi KA. Slimmer's paralysis--peroneal neuropathy during weight reduction. J Neurol Neurosurg Psychiatry. 1984;47:564-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Broekx S, Weyns F. External neurolysis as a treatment for foot drop secondary to weight loss: a retrospective analysis of 200 cases. Acta Neurochir (Wien). 2018;160:1847-1856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Thaisetthawatkul P, Collazo-Clavell ML, Sarr MG, Norell JE, Dyck PJ. A controlled study of peripheral neuropathy after bariatric surgery. Neurology. 2004;63:1462-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 169] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 9. | Weyns FJ, Beckers F, Vanormelingen L, Vandersteen M, Niville E. Foot drop as a complication of weight loss after bariatric surgery: is it preventable? Obes Surg. 2007;17:1209-1212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Aguirre M, Gibson J, Lozowska D. Bilateral foot drop linked to rapid intentional weight loss and long distance walking. Marshall J Med. 2019;5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Kim DH, Kline DG. Management and results of peroneal nerve lesions. Neurosurgery. 1996;39:312-9; discussion 319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 94] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Desai SLJ. Common peroneal nerve palsy in maxillofacial surgery setting. Natl J Maxillofac Surg. 2017;8:85-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Tsukamoto H, Granata G, Coraci D, Paolasso I, Padua L. Ultrasound and neurophysiological correlation in common fibular nerve conduction block at fibular head. Clin Neurophysiol. 2014;125:1491-1495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 14. | Meylaerts L, Cardinaels E, Vandevenne J, Velghe B, Gelin G, Vanormelingen L, Weyns F. Peroneal neuropathy after weight loss: a high-resolution ultrasonographic characterization of the common peroneal nerve. Skeletal Radiol. 2011;40:1557-1562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Shahar E, Landau E, Genizi J. Adolescence peroneal neuropathy associated with rapid marked weight reduction: case report and literature review. Eur J Paediatr Neurol. 2007;11:50-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Hammond N, Wang Y, Dimachkie MM, Barohn RJ. Nutritional neuropathies. Neurol Clin. 2013;31:477-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 17. | Cruz-Martínez A, Bort S, Arpa J, Palau F. Hereditary neuropathy with liability to pressure palsies (HNPP) revealed after weight loss. Eur Neurol. 1997;37:257-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Hatano Y, Arai T, Iida H, Soneda J. Common peroneal nerve palsy. A complication of coronary artery bypass grafting surgery. Anaesthesia. 1988;43:568-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Navarro-Vicente F, García-Granero A, Frasson M, Blanco F, Flor-Lorente B, García-Botello S, García-Granero E. Prospective evaluation of intraoperative peripheral nerve injury in colorectal surgery. Colorectal Dis. 2012;14:382-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Visser LH, Hens V, Soethout M, De Deugd-Maria V, Pijnenburg J, Brekelmans GJ. Diagnostic value of high-resolution sonography in common fibular neuropathy at the fibular head. Muscle Nerve. 2013;48:171-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Fearon KC, Ljungqvist O, Von Meyenfeldt M, Revhaug A, Dejong CH, Lassen K, Nygren J, Hausel J, Soop M, Andersen J, Kehlet H. Enhanced recovery after surgery: a consensus review of clinical care for patients undergoing colonic resection. Clin Nutr. 2005;24:466-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1001] [Cited by in RCA: 1022] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 22. | Lewis SJ, Andersen HK, Thomas S. Early enteral nutrition within 24 h of intestinal surgery versus later commencement of feeding: a systematic review and meta-analysis. J Gastrointest Surg. 2009;13:569-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 279] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 23. | Braga M, Ljungqvist O, Soeters P, Fearon K, Weimann A, Bozzetti F; ESPEN. ESPEN Guidelines on Parenteral Nutrition: surgery. Clin Nutr. 2009;28:378-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 396] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 24. | Özişler Z, Akyüz M, Yalçın E. Bilateral peroneal neuropathy after bariatric surgery: A case report. Turk J Phys Med Rehabil. 2017;63:348-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |