Published online Mar 16, 2021. doi: 10.12998/wjcc.v9.i8.1877
Peer-review started: September 20, 2020
First decision: December 14, 2020
Revised: December 23, 2020
Accepted: January 6, 2021
Article in press: January 6, 2021
Published online: March 16, 2021
Processing time: 166 Days and 2.8 Hours
Typically, right coronary artery (RCA) occlusion causes ST-segment elevation in inferior leads. However, it is rarely observed that RCA occlusion causes ST-segment elevation only in precordial leads. In general, an electrocardiogram is considered to be the most important method for determining the infarct-related artery, and recognizing this is helpful for timely discrimination of the culprit artery for reperfusion therapy. In this case, an elderly woman presented with chest pain showing dynamic changes in precordial ST-segment elevation with RCA occlusion.
A 96-year-old woman presented with acute chest pain showing precordial ST-segment elevation with dynamic changes. Myocardial injury markers became positive. Coronary angiography indicated acute total occlusion of the proximal nondominant RCA, mild atherosclerosis of left anterior descending artery and 75% stenosis in the left circumflex coronary artery. Percutaneous coronary intervention was conducted for the RCA. Repeated manual thrombus aspiration was performed, and fresh thrombus was aspirated. A 2 mm × 15 mm balloon was used to dilate the RCA with an acceptable angiographic result. The patient’s chest pain was relieved immediately. A postprocedural electrocardiogram showed alleviation of precordial ST-segment elevation. The diagnosis of acute isolated right ventricular infarction caused by proximal nondominant RCA occlusion was confirmed. Echocardiography indicated normal motion of the left ventricular anterior wall and interventricular septum (ejection fraction of 54%), and the right ventricle was slightly dilated. The patient was asymptomatic during the 9-mo follow-up period.
Cardiologists should be conscious that precordial ST-segment elevation may be caused by occlusion of the nondominant RCA.
Core Tip: It is rarely observed that right coronary artery occlusion causes ST-segment elevation only in precordial leads without inferior lead elevation. Electrocardiograms are often used by cardiologists to identify the infarct-related artery. This case emphasizes the importance for cardiologists to be conscious that occlusion of the nondominant right coronary artery can cause precordial ST-segment elevation. Recognizing this is helpful for discriminating the culprit artery for timely reperfusion therapy.
- Citation: Wu HY, Cheng G, Cao YW. Chest pain showing precordial ST-segment elevation in a 96-year-old woman with right coronary artery occlusion: A case report. World J Clin Cases 2021; 9(8): 1877-1884
- URL: https://www.wjgnet.com/2307-8960/full/v9/i8/1877.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i8.1877
Precordial ST-segment elevation usually indicates occlusion of the left anterior descending (LAD) artery[1-3]. However, ST-segment elevation in V1-V4 on a 12-lead electrocardiogram (ECG) may occur in acute isolated right ventricular infarction caused by right coronary artery (RCA) occlusion, which is a very rare event in clinical practice and accounts for no more than 3% of myocardial infarctions[4-6].
Here, we report a case in which precordial ST-segment elevation occurred in an elderly woman with acute total occlusion of the proximal nondominant RCA. ECG is considered to be the most important method for identifying the infarct-related artery. Therefore, a comprehensive ECG evaluation can improve the accuracy of diagnosis, shorten the time from door to balloon and improve the prognosis of patients.
A 96-year-old woman presented with a 4 h history of substernal chest pain along with diaphoresis.
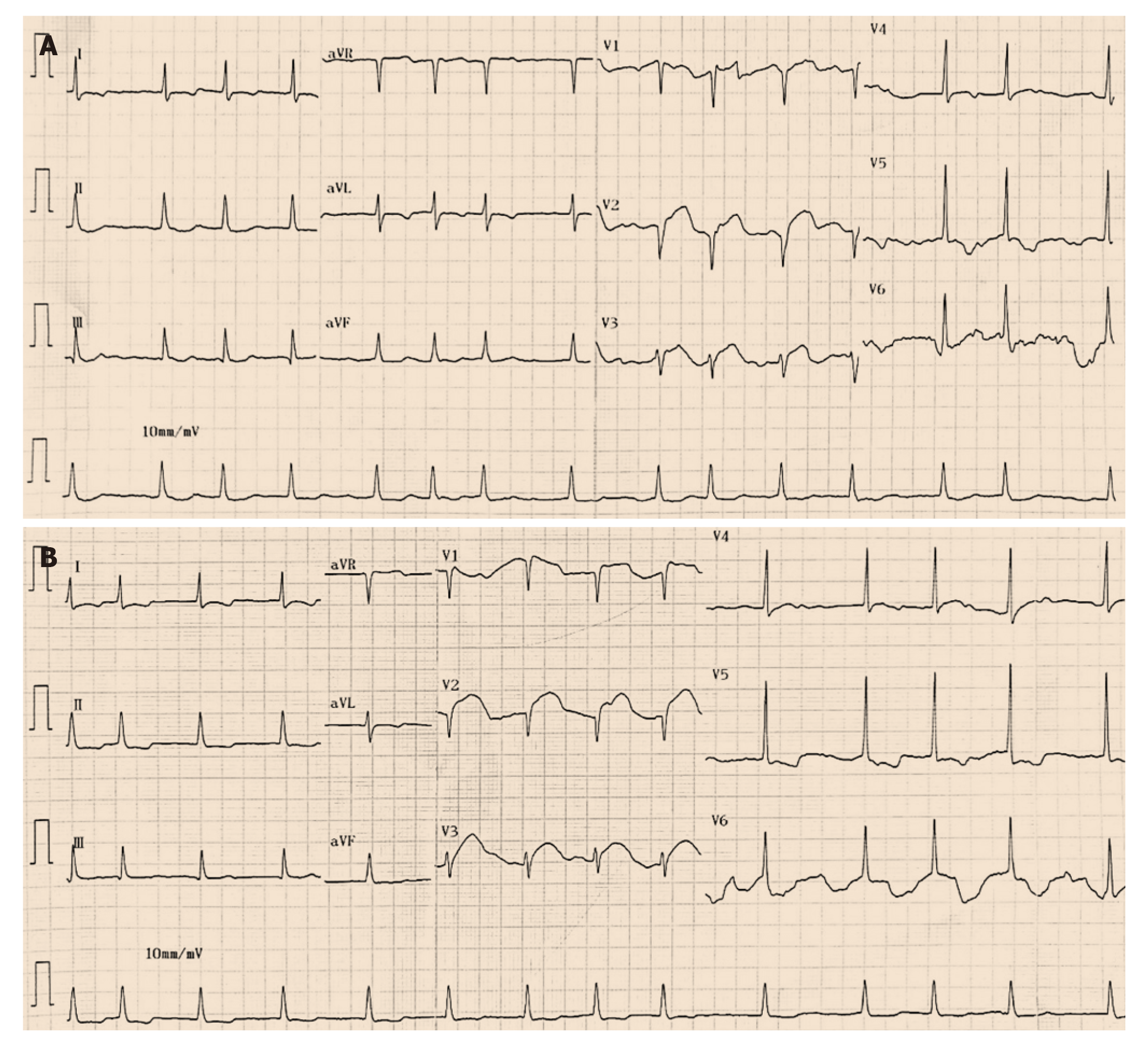
The patient had substernal chest pain along with diaphoresis four hours before admission to the emergency department. On the way to the emergency department, the patient was free of symptoms after sublingual administration of nitroglycerin. A standard 12-lead ECG obtained on admission indicated an ectopic atrial fibrillation rhythm and convex ST-segment elevation in V1-V4 (Figure 1A). No previous ECG was available for comparison. Assessment of initial myocardial injury markers showed that the troponin T level was less than 40 ng/L (0-40), the troponin I level was 0.007 ng/mL (0-0.030), the myoglobin level was 57.4 ng/mL (14.3-65.8), and the creatine kinase MB level was 5.0 ng/mL (0.6-6.3). The patient was transferred to the cardiovascular intensive care unit for further monitoring and evaluation after treatment with 300 mg of aspirin and 300 mg of clopidogrel. Intermittent chest pain was relieved with sublingual nitroglycerin. Approximately two hours after admission, the patient progressed to severe recurrent chest pain.
The patient had a history of hypertension for 30 years and type 2 diabetes for 20 years.
The patient had no relevant personal history. The patient had no family history of inherited diseases or premature coronary heart disease.
Vital signs were stable. A pulmonary examination showed clear lung auscultation. A cardiac examination showed an irregular rate and rhythm without rubs, murmurs or gallops. No jugular vein engorgement or peripheral edema was found.
The troponin T level increased to 167 ng/L. The peak troponin T level was more than 2000 ng/L, and the peak troponin I level was 15.107 ng/mL.
Echocardiography showed normal motion of the left ventricular anterior wall and interventricular septum (ejection fraction of 54%). The right ventricle was slightly dilated.
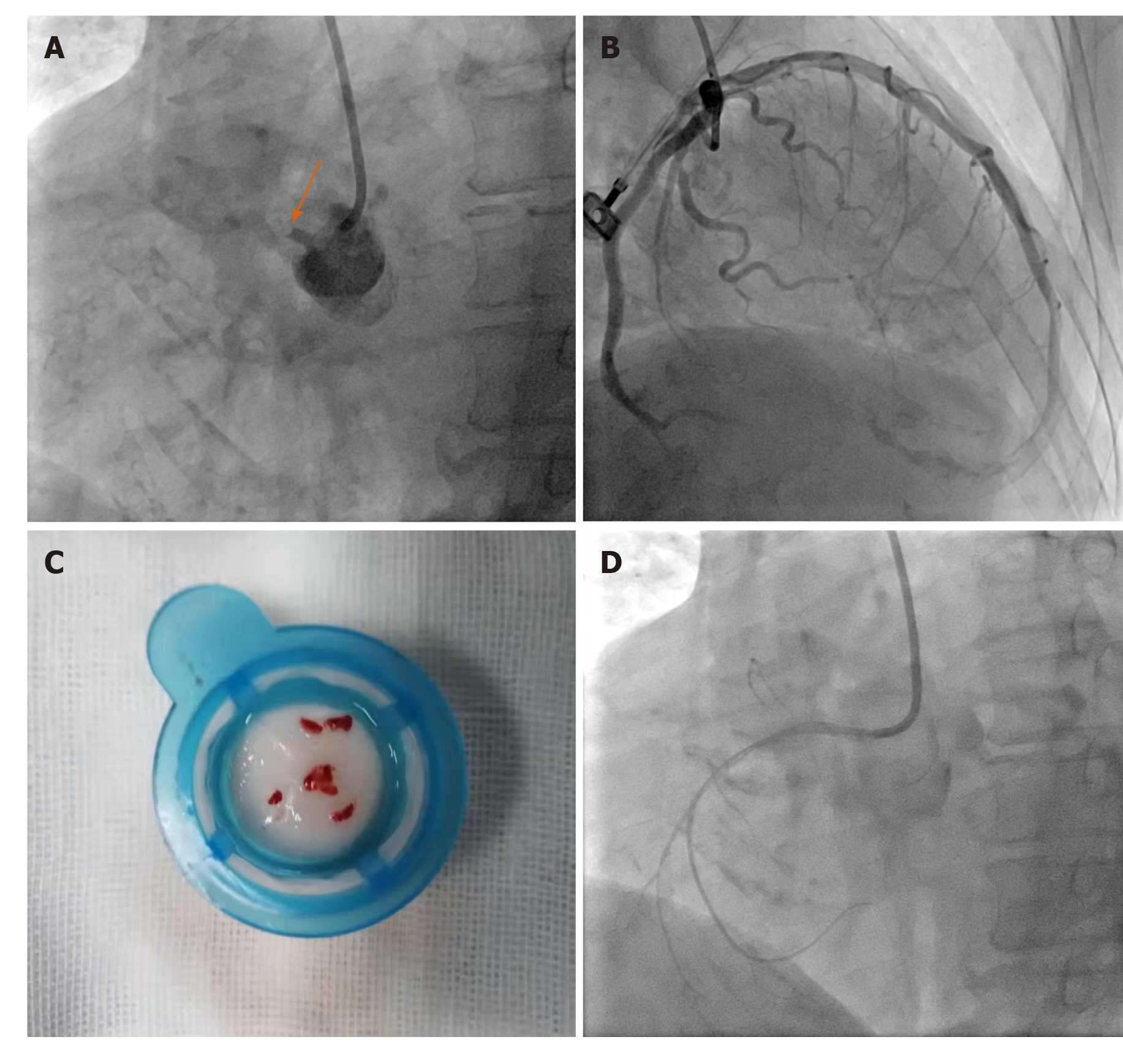
A twelve-lead ECG indicated ST-segment elevation in V1-V4 with dynamic changes compared with the former results (Figure 1B). A suspected anterior wall myocardial infarction caused by LAD artery occlusion was first considered. Emergent coronary angiography demonstrated complete occlusion of the proximal nondominant RCA with thrombus without reverse perfusion and collateral circulation at the distal end (Figure 2A). The left coronary artery showed 75% stenosis in the left circumflex artery and mild atherosclerosis of the LAD artery (Figure 2B). We realized that the infarct-related artery was the RCA.
The diagnosis of acute isolated right ventricular infarction caused by proximal nondominant RCA occlusion was confirmed.
Primary percutaneous coronary intervention (PCI) was conducted with a JR4.0 (6 French) guiding catheter in the RCA. Repeated manual thrombus aspiration was performed, and fresh thrombus was aspirated (Figure 2C). Intracoronary tirofiban 10 μg/kg was also administered during the procedure. A 2 mm × 15 mm balloon was used for dilatation. Restoration of Thrombolysis in Myocardial Infarction blood flow to grade 2 was achieved with an acceptable angiographic result (Figure 2D). Because of the small RCA, heavy thrombus load and acceptable angiographic results, coronary stent implantation was not attempted.
The patient was administered 100 mg aspirin, 75 mg clopidogrel, 20 mg atorvastatin, 47.5 mg metoprolol and 2.5 mg rivaroxaban bid to treat atrial fibrillation.
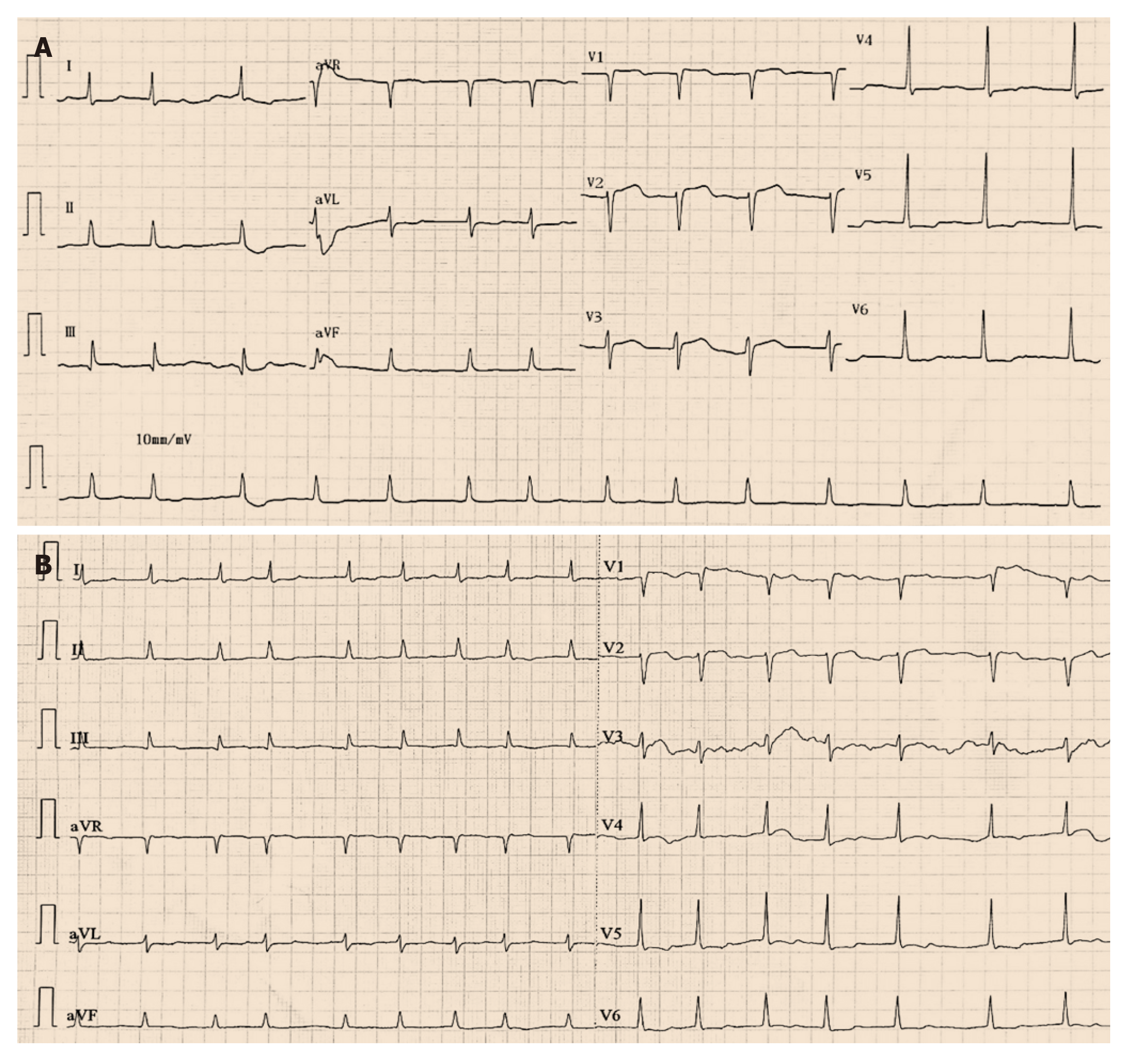
The patient’s chest pain was relieved immediately by PCI. A postprocedural ECG showed alleviation of precordial ST-segment elevation (Figure 3A). An ECG indicated complete resolution of precordial ST-segment elevation 4 d after PCI (Figure 3B).
No complications occurred during the patient’s hospitalization. The patient was asymptomatic at the 1, 3, 6 and 9 mo follow-up visits.
In this case, the RCA had a short total length. Due to the decreased RCA territory, the left coronary artery supplied the inferior wall. Therefore, the typical inferior lead ST-segment elevation was not clearly presented, while isolated precordial ST-segment elevation was presented for this acute total occlusion of the proximal nondominant RCA causing an isolated right ventricular infarction.
ECG is essential to identify the infarct-related artery in acute coronary syndrome and is necessary for clinical decisions, such as correct distinction of the acute myocardial infarction type, treatment strategy (proper fluid infusion for right ventricular infarction and limited fluid infusion for left ventricular infarction) and prognosis as well as for timely initiation of reperfusion therapy[7-11]. Although some algorithms are used to identify the culprit artery with excellent results, the accuracy is insufficient under certain conditions, including old myocardial infarction, coronary artery anomaly, left bundle block and pacing on an ECG[12]. Typically, an elevated ST-segment across the precordial leads is caused by acute occlusion of the LAD artery. For dominant RCA occlusion, the forces of inferior infarction hide the anterior forces of right ventricular infarction, causing typical inferior ST-segment elevation without precordial ST-segment elevation. Because nondominant RCA supplies the isolated right ventricle, occlusion of the artery does not cause inferior wall infarction, and precordial ST-segment elevation may emerge[13-16]. Similarly, right ventricular expansion caused by isolated right ventricular infarction leading to counterclockwise cardiac rotation was also discussed[17].
However, precordial ST-segment elevation alone due to isolated right ventricular infarction is very rare and can occur under certain conditions except for acute occlusion of the nondominant RCA, including acute occlusion of the branch from the RCA (right ventricular marginal branch, right ventricular branch or conus branch)[6,13,18-20], acute occlusion of a proximal RCA with the inferior wall protecting collaterals from the left coronary artery[15,21,22] or anomalous origination of the coronary artery with occlusion[12,16]. Although it is a very rare phenomenon, isolated right ventricular infarction may cause serious adverse cardiac events, including right ventricular dysfunction, severe tricuspid regurgitation, rupture of the right ventricular free wall, malignant ventricular arrhythmias, severe bradycardia, cardiogenic shock and sudden death[23,24]. Because the patient’s symptoms disappeared on admission, the initial myocardial injury markers were negative, and the patient was a 96-year-old woman, the family members of the patient asked for drug treatment first. Approximately two hours after admission, the patient progressed to severe recurrent chest pain and underwent emergent PCI. Notably, however, ST-segment elevation myocardial infarction is a clinical diagnosis. If within the indicated time frames and without contraindication, PCI for ST-segment elevation myocardial infarction should be performed as soon as possible, and there is no need to wait for positive cardiac enzymes. The infarct-related artery should be systematically treated during the initial intervention. Full revascularization can benefit patients with multivessel disease undergoing primary PCI, but the optimal timing of treatment of the nonculprit lesion is unclear. Patients with multivessel disease should undergo routine revascularization of nonculprit artery lesions before hospital discharge. However, for patients with cardiogenic shock, routine revascularization of nonculprit artery lesions is not recommended during primary PCI[25].
Although not common in proximal nondominant RCA occlusion, the ECG changes observed in our case may cause erroneous infarct-related artery definition and delayed treatment in serious situations. Isolated right ventricular infarction may be difficult to identify, thus requiring a high degree of clinical suspicion and careful evaluation of ECG characteristics[26]. Even with the ideal setting of choosing the appropriate diagnostic and guiding catheters in emergent PCI, only a few minutes would be required to change catheters. Therefore, overemphasizing the importance of identifying the potential culprit artery by ECG before PCI is not warranted.
Occlusion of a nondominant RCA may be followed by ST-segment elevation in precordial leads. Internists, especially interventional cardiologists, should be aware of this scenario to discriminate the infarct-related artery for timely reperfusion therapy.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dai X S-Editor: Gao CC L-Editor: Filipodia P-Editor: Wang LYT
| 1. | Eskola MJ, Nikus KC, Sclarovsky S. Persistent precordial "hyperacute" T waves signify proximal left anterior descending artery occlusion. Heart. 2009;95:1951-1952; author reply 1952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | de Winter RW, Adams R, Verouden NJ, de Winter RJ. Precordial junctional ST-segment depression with tall symmetric T-waves signifying proximal LAD occlusion, case reports of STEMI equivalence. J Electrocardiol. 2016;49:76-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Driver BE, Khalil A, Henry T, Kazmi F, Adil A, Smith SW. A new 4-variable formula to differentiate normal variant ST segment elevation in V2-V4 (early repolarization) from subtle left anterior descending coronary occlusion - Adding QRS amplitude of V2 improves the model. J Electrocardiol. 2017;50:561-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Yip HK, Chen MC, Wu CJ, Chang HW, Yu TH, Yeh KH, Fu M. Acute myocardial infarction with simultaneous ST-segment elevation in the precordial and inferior leads: evaluation of anatomic lesions and clinical implications. Chest. 2003;123:1170-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Nikus KC, Eskola MJ. Electrocardiogram patterns in acute left main coronary artery occlusion. J Electrocardiol. 2008;41:626-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Zhong WW, Blue M, Michaels AD. Acute Isolated Right Ventricular Infarction: Unusual Presentation of Anterior ST-Segment-Elevation Myocardial Infarction. Tex Heart Inst J. 2019;46:151-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Lin YY, Wen YD, Wu GL, Xu XD. De Winter syndrome and ST-segment elevation myocardial infarction can evolve into one another: Report of two cases. World J Clin Cases. 2019;7:3296-3302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Quinn T, Johnsen S, Gale CP, Snooks H, McLean S, Woollard M, Weston C; Myocardial Ischaemia National Audit Project (MINAP) Steering Group. Effects of prehospital 12-lead ECG on processes of care and mortality in acute coronary syndrome: a linked cohort study from the Myocardial Ischaemia National Audit Project. Heart. 2014;100:944-950. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 9. | Lindow T, Pahlm O, Khoshnood A, Nyman I, Manna D, Engblom H, Lassen AT, Ekelund U. Electrocardiographic changes in the differentiation of ischemic and non-ischemic ST elevation. Scand Cardiovasc J. 2020;54:100-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Frangieh AH, Obeid S, Ghadri JR, Imori Y, D’Ascenzo F, Kovac M, Ruschitzka F, Lüscher TF, Duru F, Templin C; InterTAK Collaborators. ECG Criteria to Differentiate Between Takotsubo (Stress) Cardiomyopathy and Myocardial Infarction. J Am Heart Assoc. 2016;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 11. | Zanuttini D, Armellini I, Nucifora G, Grillo MT, Morocutti G, Carchietti E, Trillò G, Spedicato L, Bernardi G, Proclemer A. Predictive value of electrocardiogram in diagnosing acute coronary artery lesions among patients with out-of-hospital-cardiac-arrest. Resuscitation. 2013;84:1250-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 12. | Matte BDS, Azmus AD. Acute Myocardial Infarction Caused by an Anomalous Right Coronary Artery Occlusion Presenting with Precordial ST Elevation. Case Rep Cardiol. 2017;2017:3972830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Marinakis A, Lampropoulos K. Precordial ST elevation due to isolated ventricular branch occlusion after stent implantation in the right coronary artery. Rev Esp Cardiol. 2009;62:1338-1340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Franco JJ, Brown M, Bashir R, O’Murchu B. Acute anterior ST-elevation myocardial infarction and electrical storm secondary to nondominant right coronary artery occlusion. Tex Heart Inst J. 2014;41:335-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Kim SE, Lee JH, Park DG, Han KR, Oh DJ. Acute Myocardial Infarction by Right Coronary Artery Occlusion Presenting as Precordial ST Elevation on Electrocardiography. Korean Circ J. 2010;40:536-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Liu CJ, Cheng ST, Ko YL. Acute Anterior ST-Segment Elevation Myocardial Infarction Caused by Occlusion of Right Coronary Artery. Am J Med Sci. 2016;351:200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Iannetta L, Puddu PE, Missiroli B, Morabito G, Grillo P, De Gregorio C, Schiariti M. Pathophysiology and ECG patterns of isolated right ventricular infarction with nondominant right coronary artery. J Cardiovasc Med (Hagerstown). 2013;14:740-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Eichhöfer J, Curzen N. Images in cardiovascular medicine. Unexpected profound transient anterior ST elevation after occlusion of the conus branch of the right coronary artery during angioplasty. Circulation. 2005;111:e113-e114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Acikel M, Yilmaz M, Bozkurt E, Gürlertop Y, Köse N. ST segment elevation in leads V1 to V3 due to isolated right ventricular branch occlusion during primary right coronary angioplasty. Catheter Cardiovasc Interv. 2003;60:32-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Koh TW, Coghlan JG, Lipkin DP. Anterior ST segment elevation due to isolated right ventricular infarction during right coronary angioplasty. Int J Cardiol. 1996;54:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Muhammad KI, Kapadia SR. Anterior ST-segment elevation with right coronary artery occlusion: a unique case of isolated right ventricular infarction. Angiology. 2008;59:622-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Cafri C, Orlov G, Weinstein JM, Kobal S, Ilia R. ST elevation in the anterior precordial leads during right ventricular infarction: lessons learned during primary coronary angioplasty--a case report. Angiology. 2001;52:417-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Karim MA, Wong C, Armbruster R, Windle J, Deligonul U. Importance of a non-dominant right coronary artery occlusion presenting as sudden cardiac death with prolonged right ventricular dysfunction and malignant arrhythmias. Cathet Cardiovasc Diagn. 1995;35:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Vural M, Uslu A, Bülbül S. An isolated right ventricular myocardial infarction and severe tricuspid regurgitation due to occlusion of a non-dominant right coronary artery: role of delayed revascularization. Anadolu Kardiyol Derg. 2010;10:376-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferović PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO. 2018 ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention. 2019;14:1435-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 382] [Article Influence: 63.7] [Reference Citation Analysis (0)] |
| 26. | Carroll R, Sharma N, Butt A, Hussain KM. Unusual electrocardiographic presentation of an isolated right ventricular myocardial infarction secondary to thrombotic occlusion of a non-dominant right coronary artery--a case report and brief review of literature. Angiology. 2003;54:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |