Published online Feb 16, 2021. doi: 10.12998/wjcc.v9.i5.1103
Peer-review started: August 12, 2020
First decision: December 3, 2020
Revised: December 11, 2020
Accepted: December 23, 2020
Article in press: December 23, 2020
Published online: February 16, 2021
Processing time: 171 Days and 0.8 Hours
Large intracranial dissecting aneurysm (IDA) in the anterior cerebral circulation is rare in children. There has been no consensus on the diagnosis and treatment for IDA in children.
We report a 3-year-old boy with a large ruptured IDA in the right middle cerebral artery (16 mm × 14 mm). The IDA was successfully managed with clipping and angioplasty. Next-generation sequencing of the blood sample followed by bioinformatics analysis suggested that the rs78977446 variant of the ADAMTS13 gene is a risk for pediatric IDA. Three years after surgery, the boy was develop-mentally normal.
Clipping and angioplasty are effective treatments for ruptured IDA in the anterior cerebral circulation. ADAMTS13 rs78977446 is a risk factor for pediatric IDA.
Core Tip: The index case was a 3-year-old boy with a large ruptured intracranial dissecting aneurysm in the right middle cerebral artery (16 mm × 14 mm). He was successfully treated by clipping and angioplasty. Whole-genome high-throughput sequencing identified the rs78977446 variant of the ADAMTS13 gene. Bioinformatics analysis using the American College of Medical Genetics guidelines and literature search suggested that this variant is a risk factor for pediatric intracranial dissecting aneurysm.
- Citation: Sun N, Yang XY, Zhao Y, Zhang QJ, Ma X, Wei ZN, Li MQ. Treatment of pediatric intracranial dissecting aneurysm with clipping and angioplasty, and next-generation sequencing analysis: A case report and literature review . World J Clin Cases 2021; 9(5): 1103-1110
- URL: https://www.wjgnet.com/2307-8960/full/v9/i5/1103.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i5.1103
Rupture of intracranial dissecting aneurysms (IDA) is a cause of subarachnoid hemorrhage (SAH) in children[1]. The incidence of IDA is estimated to be no more than that for cervical dissecting artery (2.6–3.0 per 100000 people per year)[2,3]. Both genetic and environmental factors contribute to the development of pediatric IDA[4]. At the level of pathology, ultimate formation of intramural hematoma between the intima and media consists of tear of artery and rupture of vasa vasorum[5]. IDA is associated with syphilis[6], connective tissue diseases[7], atherosclerosis[8], infection[9], migraine[10], hyperhomocysteinemia[10], and alpha-1 antitrypsin deficiency[11]. A key event in dissec-ting aneurysms is the sudden widespread disruption of the internal elastic lamina and media[12,13].
IDA in children, and particularly in the anterior cerebral circulation, has rarely been reported and represents a formidable challenge in both the diagnosis and treatment[14].
We report a case of SAH caused by ruptured IDA in the anterior cerebral circul-ation. The patient was successfully treated with clipping and angioplasty. We also performed whole-genome sequencing to identify potential pathogenic gene polymorphisms.
A 3-year-old boy presented with intermittent non-projectile vomiting after a brief episode of syncope.
There was no clear triggering events for the emergence of symptoms. There was no blood in the gastric contents. Upon admission, the boy was lethargic but able to respond to command.
He had no history of trauma or surgery and no family history of cardiovascular diseases.
The Glasgow Coma Scale score was 14. Hunt-Hess grade was III. Pupil reflex was normal. The muscle strength was grade III in the left leg.
With the exception of increased white blood cell count (8.58 × 109/L), the laboratory test results were normal.
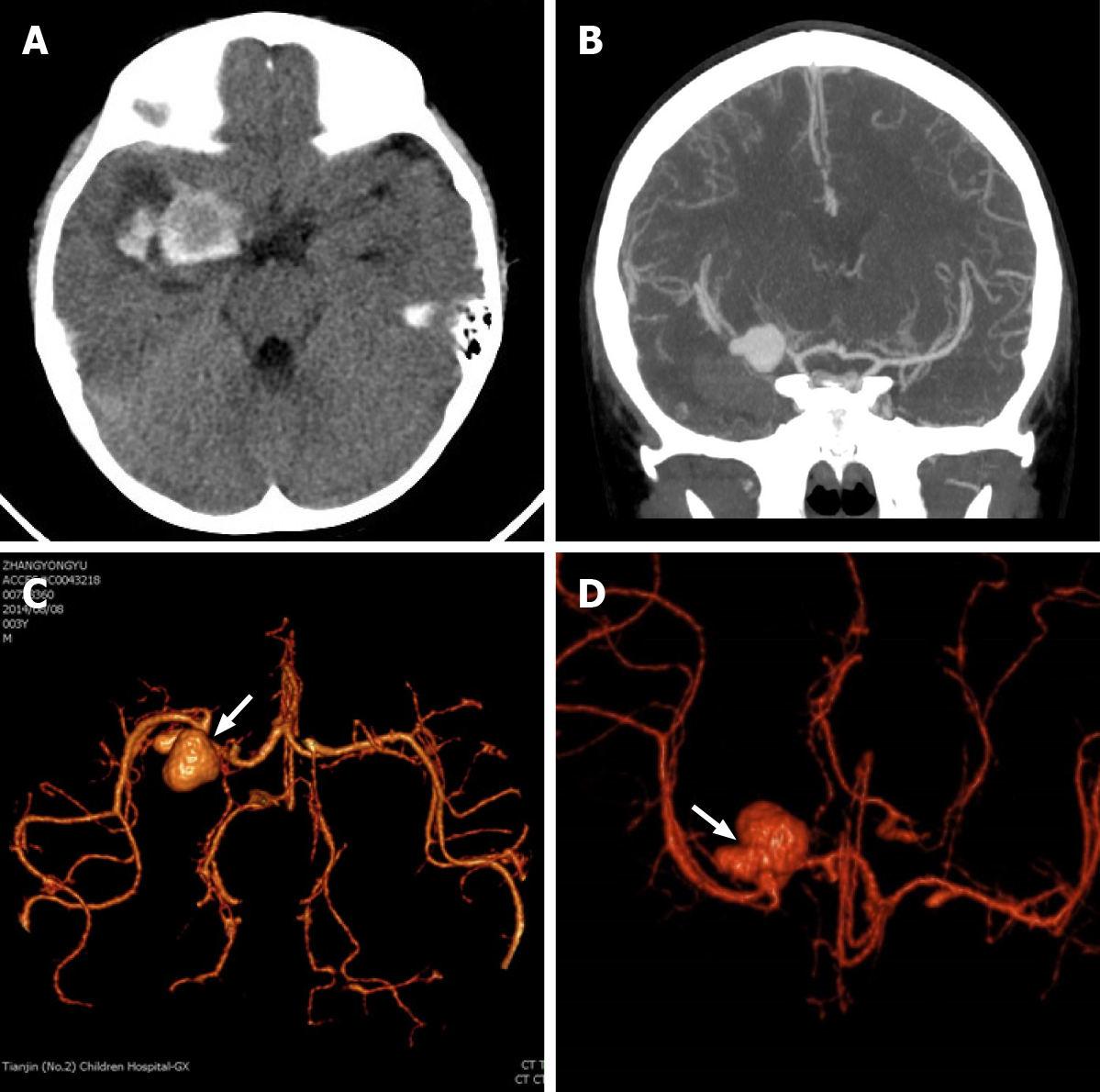
Computed tomography (CT) scan showed subarachnoid hemorrhage in the lateral fissure cistern and a small amount of blood in the right lateral ventricle (Figure 1A). CT angiography showed ruptured aneurysm in the right middle cerebral artery (Figure 1B-D). The intracranial aneurysm (IA) was 16 mm × 14 mm, with a wide neck. The pearl-and-string sign (proximal stenosis and distal stenosis in the intracranial aneurysm) was consistent with dissecting aneurysm (Figure 1C and D), as previously reported[15].
Based on these features, a diagnosis of IDA was established.
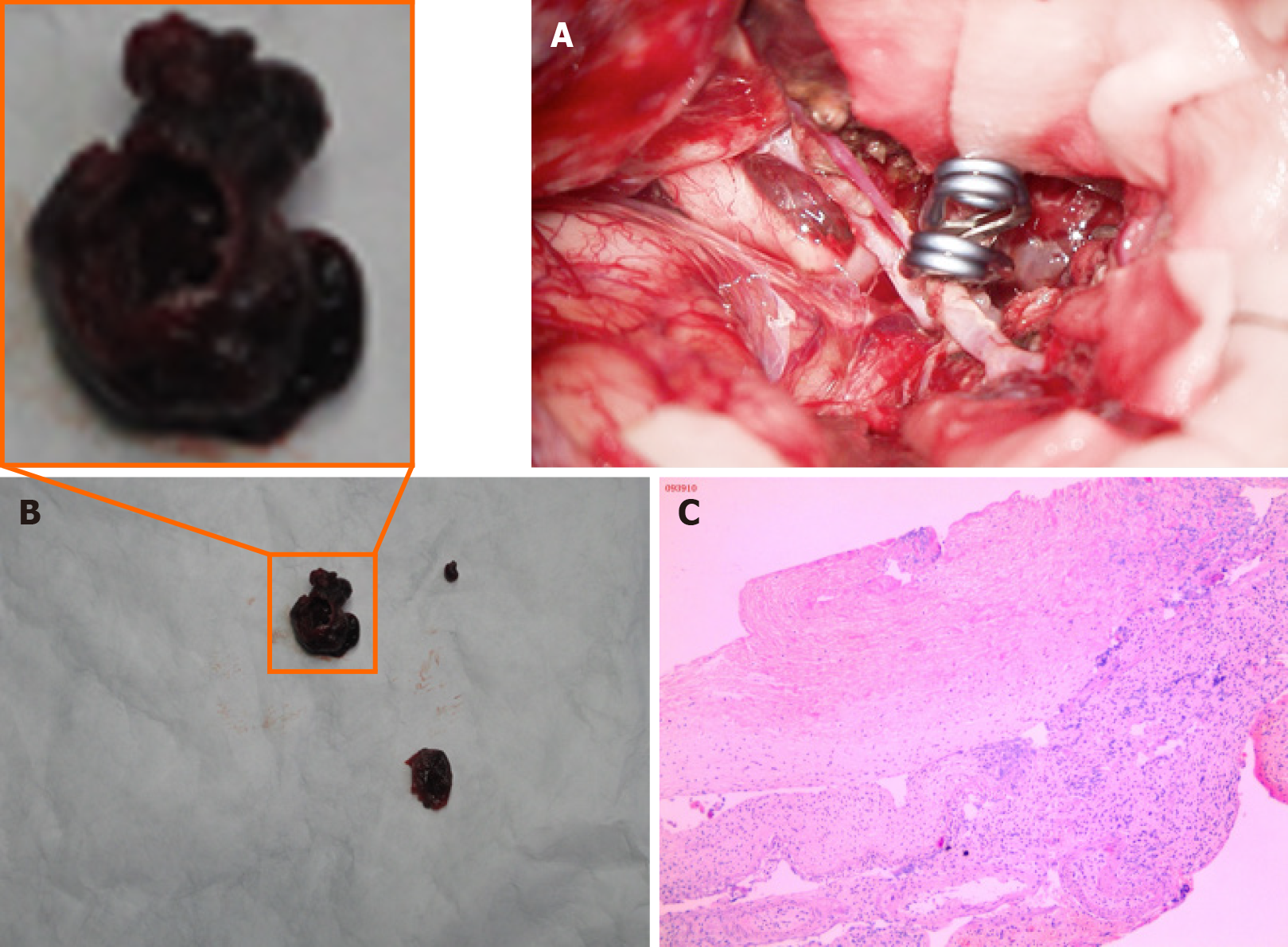
Surgery was conducted using a pterional approach under general anesthesia. After adequate exposure of the parent artery, an IA was apparent at the junction between M1 and M2. There was severe stenosis in the proximal part of the aneurysm. The aneurysm wall was extremely thin. The normal anatomical structure of the parent artery has been apparently destroyed. The aneurysm was opened, and the blood clot within the aneurysm and the patent artery was removed. Then the IA was clipped (Figure 2A and B). The normal anatomical structure of the parent artery was restored and the parent vessel remained patent. IDA lesion was resected and tissue specimen was sent to pathologic examination (Figure 2B and C).
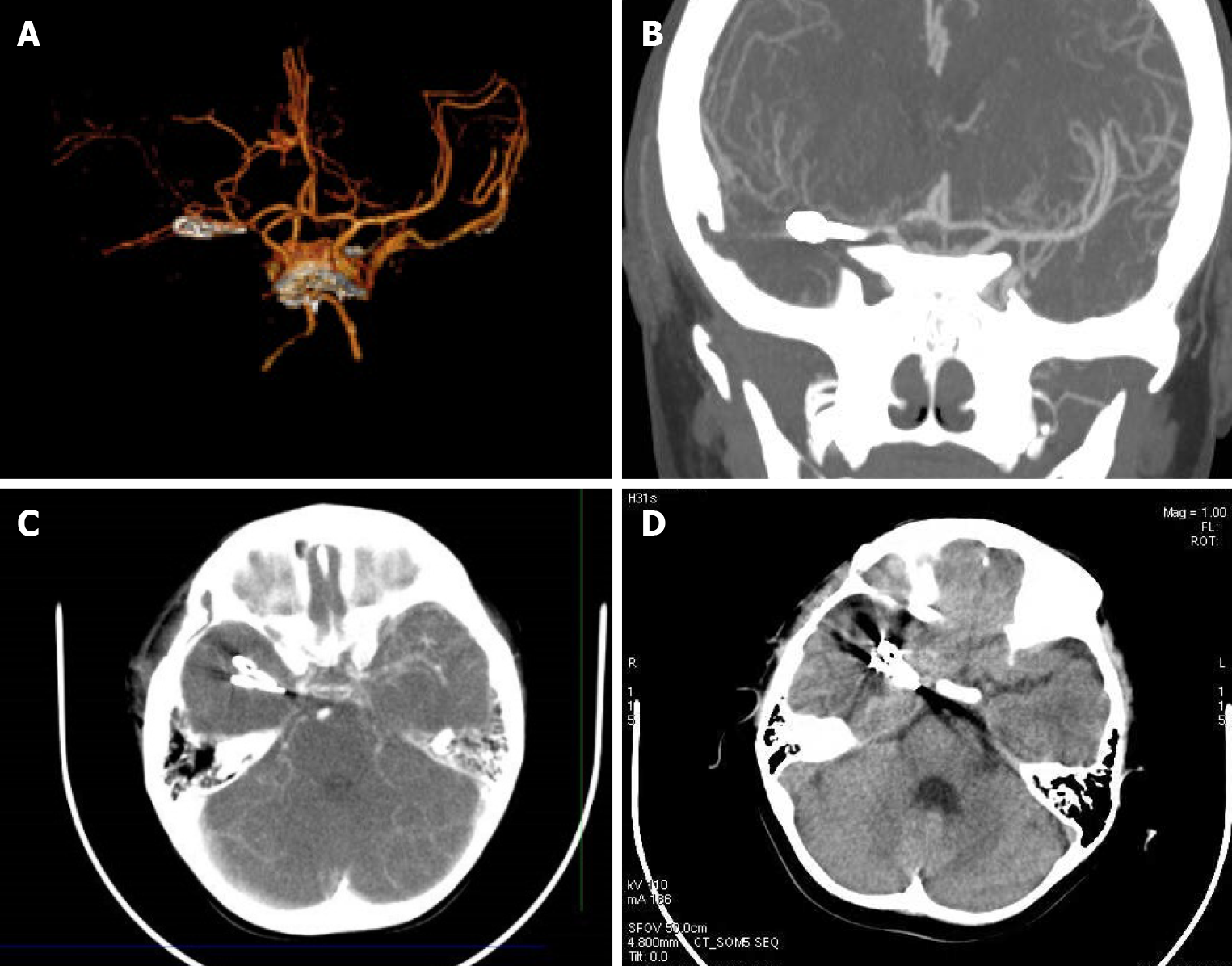
CT angiography was conducted 2 wk later, and showed no aneurysm; the parent artery was patent (Figure 3A-C). Neurologic symptoms and signs gradually improved. At the 1 mo follow-up visit, the boy was healthy, with the exception of slight muscle weakness in the left leg (grade IV). At 3 years later, the patient had completely recovered. CT angiography revealed normal blood supply to the brain (Figure 3D).
Whole-genome sequencing (Novogene, Beijing, China) of the blood sample followed by bioinformatics analysis according to the American College of Medical Genetics guidelines[16] revealed 13 candidate genes (Table 1). Next, we searched the PubMed database using the keyword “intracranial aneurysm” or “dissecting,” and “genes including pathogenic variation.” The literature review suggested an association between the rs78977446 variant of the ADAMTS13 gene and pediatric IDA. Briefly, ADAMTS13 participates in the inflammatory processes and vascular remodeling in IA[17,18]. Genetic variants, transcription abnormality, and methylation changes in the ADAMTS genes may be an important factor for IA[19]. In addition to IA, an autopsy study of 31 cases of aortic dissections revealed much higher frequency (0.1613) of the rs11575933 variant of the ADAMTS13 gene in aortic dissections[20] vs healthy control subjects (https://www.ncbi.nlm.nih.gov/snp/?term=rs11575933).
| Chromosome | Position | Variation | REF | ALT | Function | Gene | SIFT | Mutation taster | CADD |
| 1 | 47610522 | rs570554271 | C | T | Stopgain | CYP4A22 | - | 1, A | 10.070978, 36 |
| 2 | 234637905 | rs45625338 | C | T | Missense | UGT1A3 | 0.0, D | 1, D | 2.458692, 19.20 |
| 8 | 145699712 | - | G | A | Missense | FOXH1 | 0.0, D | 1, D | 6.334943, 29.3 |
| 9 | 136310917 | rs78977446 | C | T | Missense | ADAMTS13 | 0.081, T | 1, N | 0.962795, 10.45 |
| 11 | 17482222 | rs185040406 | C | T | Missense | ABCC8 | 0.07, T | 0.777604, N | 3.415216, 23.0 |
| 12 | 85266484 | rs12424429 | G | A | Missense | SLC6A15 | 0.295, T | 0.975276, N | - |
| 13 | 100518634 | rs41281112 | C | T | Stopgain | CLYBL | - | 1, A | 8.514350, 35 |
| 14 | 75514138 | rs28756990 | C | A | Missense | MLH3 | 0.034, D | 1, N | 2.798595, 21.4 |
| 16 | 3705465 | rs77254040 | C | G | Missense | DNASE1 | 0.007, D | 1, D | 3.289682, 22.8 |
| 18 | 29867688 | rs3744921 | T | C | Missense | GAREM1 | 0.22, T | 0.999954, D | 1.071666, 11.06 |
| 19 | 4157148 | rs77002741 | G | A | Missense | CREB3L3 | 0.169, T | 1, N | 1.858481, 15.34 |
| 19 | 39898667 | rs3746083 | C | T | Synonymous | ZFP36 | - | - | - |
| 22 | 50523267 | rs184241759 | C | T | Missense | MLC1 | 0.007, D | 1, N | 3.434483, 23.0 |
IDA can be classified into two types. In type 1 IDA, the dissection is located between the elastic layer and media layer, and causes ischemic stroke. In type 2 IDA, the dissection occurs between the media and adventitia, and causes SAH[21].
Treatment options for type 2 IDA include microsurgical clipping, coiling embolization, triple stent, trapping[22], bypass[23], wrapping, and complete exclusion[24]. The choice of these treatment modalities remains controversial[25].
As an endovascular interventional therapy, clipping has been frequently used in pediatric IDA of the posterior circulation[26-28]. It does not require craniotomy and thus is associated with minimal surgical trauma. The IDA in the index case was relatively large, and was ruptured. Thus, controlling bleeding and preventing rebleeding were the primary aims of the treatment[29]. For this rare ruptured large dissecting aneurysm, microsurgery clipping and patent vessel remodeling may have a lower probability of long-term recurrence. More importantly, the lesions can be visualized during the microsurgery. Blood clot in the parent artery was cleared to establish the normal anatomy of the parent artery. IDA, which is similar to the saccular aneurysm in the same location, has the risk of rebleeding during the acute stage[30]. Also, recurrence after several years has been reported[31]. As a result, long-term monitoring is required.
Sequencing analysis followed by bioinformatics analysis and literature review suggested that the rs78977446 variant of the ADAMTS13 gene is a risk for pediatric IDA. IDA is more common in children than in adults, indicating a genetic contribution, but genetic studies for pediatric IDA are rare. In a previous study, the mutational rate was significantly higher in intracranial vertebral–basilar artery dissection cases than in controls[32]. RNF213 rs112735431 (c.14576G>A) frequency is significantly lower in patients with intracranial vertebral artery dissection. The genetic predisposition to IDA in the index case may form the basis of future recurrence, and physicians should be aware of the unique circumstance of each patient[33].
In summary, clipping and angioplasty are appropriate treatments for ruptured IDA in the anterior cerebral circulation. The rs78977446 variant of the ADAMTS13 gene is a risk factor for pediatric IDA.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kheiralla OAM S-Editor: Fan JR L-Editor: Filipodia P-Editor: Yuan YY
| 1. | Friedman AH, Drake CG. Subarachnoid hemorrhage from intracranial dissecting aneurysm. J Neurosurg. 1984;60:325-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 251] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 2. | Béjot Y, Daubail B, Debette S, Durier J, Giroud M. Incidence and outcome of cerebrovascular events related to cervical artery dissection: the Dijon Stroke Registry. Int J Stroke. 2014;9:879-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 3. | Lee VH, Brown RD Jr, Mandrekar JN, Mokri B. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006;67:1809-1812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 374] [Cited by in RCA: 378] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 4. | Rabinov JD, Hellinger FR, Morris PP, Ogilvy CS, Putman CM. Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2003;24:1421-1428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Kim YK, Schulman S. Cervical artery dissection: pathology, epidemiology and management. Thromb Res. 2009;123:810-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Kellett MW, Young GR, Fletcher NA. Paraparesis due to syphilitic aortic dissection. Neurology. 1997;48:221-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Brandt T, Orberk E, Weber R, Werner I, Busse O, Müller BT, Wigger F, Grau A, Grond-Ginsbach C, Hausser I. Pathogenesis of cervical artery dissections: association with connective tissue abnormalities. Neurology. 2001;57:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 189] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 8. | Larson EW, Edwards WD. Risk factors for aortic dissection: a necropsy study of 161 cases. Am J Cardiol. 1984;53:849-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 630] [Cited by in RCA: 544] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 9. | Guillon B, Bousser MG. [Epidemiology and pathophysiology of spontaneous cervical artery dissection]. J Neuroradiol. 2002;29:241-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Rubinstein SM, Peerdeman SM, van Tulder MW, Riphagen I, Haldeman S. A systematic review of the risk factors for cervical artery dissection. Stroke. 2005;36:1575-1580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 221] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 11. | Schievink WI, Prakash UB, Piepgras DG, Mokri B. Alpha 1-antitrypsin deficiency in intracranial aneurysms and cervical artery dissection. Lancet. 1994;343:452-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 114] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Mizutani T, Kojima H, Asamoto S. Healing process for cerebral dissecting aneurysms presenting with subarachnoid hemorrhage. Neurosurgery. 2004;54:342-7; discussion 347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Mizutani T, Kojima H, Asamoto S, Miki Y. Pathological mechanism and three-dimensional structure of cerebral dissecting aneurysms. J Neurosurg. 2001;94:712-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 130] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, Goeggel-Simonetti B, Engelter ST, Pezzini A, Bijlenga P, Southerland AM, Naggara O, Béjot Y, Cole JW, Ducros A, Giacalone G, Schilling S, Reiner P, Sarikaya H, Welleweerd JC, Kappelle LJ, de Borst GJ, Bonati LH, Jung S, Thijs V, Martin JJ, Brandt T, Grond-Ginsbach C, Kloss M, Mizutani T, Minematsu K, Meschia JF, Pereira VM, Bersano A, Touzé E, Lyrer PA, Leys D, Chabriat H, Markus HS, Worrall BB, Chabrier S, Baumgartner R, Stapf C, Tatlisumak T, Arnold M, Bousser MG. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015;14:640-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 305] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 15. | Hermes J, Lakshmanan R, Watkins L, Davagnanam I. Teaching NeuroImages: Intracranial arterial dissection. Neurology. 2017;88:e111-e112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL; ACMG Laboratory Quality Assurance Committee. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405-424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19696] [Cited by in RCA: 22540] [Article Influence: 2254.0] [Reference Citation Analysis (0)] |
| 17. | Arning A, Jeibmann A, Köhnemann S, Brokinkel B, Ewelt C, Berger K, Wellmann J, Nowak-Göttl U, Stummer W, Stoll M, Holling M. ADAMTS genes and the risk of cerebral aneurysm. J Neurosurg. 2016;125:269-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Hanson E, Jood K, Nilsson S, Blomstrand C, Jern C. Association between genetic variation at the ADAMTS13 locus and ischemic stroke. J Thromb Haemost. 2009;7:2147-2148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Chen S, Li M, Xin W, Liu S, Zheng L, Li Y, Li M, Zhan M, Yang X. Intracranial aneurysm's association with genetic variants, transcription abnormality, and methylation changes in ADAMTS genes. PeerJ. 2020;8:e8596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Nakagawa M, Matsusue A, Umetsu K, Iino M, Ishikawa T, Yuasa I. Genotyping of the c.1423C>T (p.P475S) polymorphism in the ADAMTS13 gene by APLP and HRM assays: Northeastern Asian origin of the mutant. Leg Med (Tokyo). 2016;21:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Sasaki O, Koike T, Tanaka R, Ogawa H. Subarachnoid hemorrhage from a dissecting aneurysm of the middle cerebral artery. Case report. J Neurosurg. 1991;74:504-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Araki S, Oda K, Fujita T, Kawakami M. Internal trapping of a ruptured vertebral artery dissecting aneurysm followed by recanalization of the trapped vertebral artery without aneurysm recurrence: case report. Neurol Med Chir (Tokyo). 2010;50:914-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Starke RM, Ding D, Durst CR, Crowley RW, Liu KC. Combined microsurgical PICA-PICA bypass and endovascular parent artery occlusion for a ruptured dissecting vertebral artery aneurysm. Neurosurg Focus. 2015;38:Video3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Narata AP, Yilmaz H, Schaller K, Lovblad KO, Pereira VM. Flow-diverting stent for ruptured intracranial dissecting aneurysm of vertebral artery. Neurosurgery. 2012;70:982-988; discussion 988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 82] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 25. | de Divitiis O, Di Somma A, Somma T, Cavallo LM, Marseglia M, Briganti F, Cappabianca P. Surgical clipping of a dissecting aneurysm of the precommunicating segment of the anterior cerebral artery: a case report and review of the literature. J Med Case Rep. 2015;9:117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Shin YS, Kim BM, Kim SH, Suh SH, Ryu CW, Koh JS, Kim DI, Kim DJ. Endovascular treatment of bilateral intracranial vertebral artery dissecting aneurysms presenting with subarachnoid hemorrhage. Neurosurgery. 2012;70:75-81; discussion 81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Briganti F, Cicala D, Tortora F, Leone G, Napoli M, Maiuri F. Endovascular treatment of a giant dissecting aneurysm of the posterior cerebral artery. A case report and literature review. Neuroradiol J. 2012;25:695-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Li H, Zhang X, Li XF, He XY, Zhu GH, Fang QR, Wang ZQ, Duan CZ. Predictors of Favorable Outcome of Intracranial Basilar Dissecting Aneurysm. J Stroke Cerebrovasc Dis. 2015;24:1951-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Massimi L, Moret J, Tamburrini G, Di Rocco C. Dissecting giant vertebro-basilar aneurysms. Childs Nerv Syst. 2003;19:204-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Aoki N, Sakai T. Rebleeding from intracranial dissecting aneurysm in the vertebral artery. Stroke. 1990;21:1628-1631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 138] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 31. | Ikeda T, Kurita H, Konishi Y, Fujitsuka M, Hino K, Shiokawa Y, Saito I. De novo dissecting aneurysm in a patient with a ruptured saccular lesion. Case report. J Neurosurg. 2002;97:701-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Wang K, Zhao S, Zhang Q, Yuan J, Liu J, Ding X, Song X, Lin J, Du R, Zhou Y, Sugimoto M, Chen W, Yuan B, Liu J, Yan Z, Liu B, Zhang Y, Li X, Niu Y, Long B, Shen Y, Zhang S, Abe K, Su J, Wu Z, Wu N, Liu P, Yang X; Deciphering Disorders Involving Scoliosis & Comorbidities (DISCO) study. Whole-exome sequencing reveals known and novel variants in a cohort of intracranial vertebral-basilar artery dissection (IVAD). J Hum Genet. 2018;63:1119-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Schork NJ. Personalized medicine: Time for one-person trials. Nature. 2015;520:609-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 693] [Cited by in RCA: 702] [Article Influence: 70.2] [Reference Citation Analysis (0)] |