Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.11071
Peer-review started: June 29, 2021
First decision: July 26, 2021
Revised: July 28, 2021
Accepted: October 25, 2021
Article in press: October 25, 2021
Published online: December 16, 2021
Processing time: 163 Days and 15.9 Hours
Large pedunculated colorectal polyps are not frequent among colonic polyps. We present a clinical case of a large pedunculated colorectal polyp with signet ring cell cancer infiltrating the submucosa and lymph node invasion in a patient who ultimately underwent additional surgery. Clinicians should attach importance to pedunculated colorectal polyps and choose the most appropriate therapy.
A 52-year-old female farmer underwent routine screening colonoscopy and denied constipation, diarrhea, hematochezia, or other gastrointestinal symptoms. Her past medical history and general biochemical examination results were unremarkable. During the colonoscopy, a 25-mm pedunculated polyp in the sigmoid colon was identified. The superficial epithelium was macroscopically congestive, rough, and granular, showing characteristic features of adenoma. We first ligated the root of the pedunculated polyp using nylon loops as well as a titanium clip. Histopathological examination revealed high-grade intraepithelial neoplasia of the tumor surface and a negative margin with signet ring cell adenocarcinoma infiltrating the submucosal layer. The deepest infiltration was approximately 0.9 cm from the tumor surface and 0.55 cm from the stratum basale. We performed radical resection of the left colon with lymph node dissection after two weeks. The lesion was completely resected, and pathological assessment revealed signet ring cell adenocarcinoma infiltrating the submucosal layer as well as lymph node invasion (stage PT1N1M0 and grade IIIA in pathological grading, NRAS-, BRAF V600E-, KRAS-).
This case highlights the importance of paying attention to the malignancy of large pedunculated polyps. Polyps or adenomas removed via endoscopy must be evaluated histologically. Even if adenomas may be fragile, endoscopy doctors should still remove polyps as completely as possible and choose perpendicular sections through the stalk and base to fix by formaldehyde solution.
Core Tip: Pedunculated polyp itself is considered to have a low degree of malignancy. Herein, we present a rare case of a large pedunculated polyp that contains signet ring cells and infiltrates the submucosal layer. This case highlights the malignancy of pedunculated polyps, and even if adenomas may be fragile, endoscopy doctors should still remove polyps as completely as possible and choose perpendicular sections through the stalk and base for fixation.
- Citation: Yan JN, Shao YF, Ye GL, Ding Y. Signet ring cell carcinoma hidden beneath large pedunculated colorectal polyp: A case report. World J Clin Cases 2021; 9(35): 11071-11077
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/11071.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.11071
Colorectal cancer (CRC) is the third most common malignant tumor worldwide, most of which develop from polyps, and the transition of polyps to carcinoma is a vital process in CRC development[1]. Large pedunculated polyps are polyps ≥ 10 mm in head diameter, and the degree of malignancy is always low[2]. Herein, we present a clinical report of a patient with signet ring cell colorectal adenocarcinoma in a long pedunculated colorectal polyp that is easily confused with benign polyps.
A 52-year-old female farmer underwent routine screening colonoscopy at our hospital.
She denied constipation, diarrhea, hematochezia, or other gastrointestinal symptoms.
The patient’s previous medical history was uneventful.
The patient and her family members had no previous episodes of similar diseases.
Her pulse rate, blood pressure, and respiratory rhythm were normal. No scleroma was observed on anal finger examination, and no positive nervous system signs were observed on physical examination.
The general biochemical examinations were unremarkable.
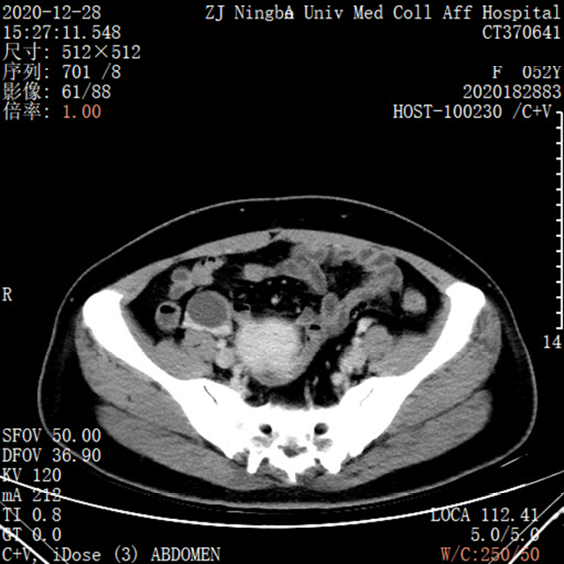
Contrast-enhanced CT scans of the abdomen showed no specific abnormalities in the left colon in Figure 1. During colonoscopy, a 25-mm pedunculated polyp was identified in the sigmoid colon. The superficial epithelium was macroscopically congestive, rough, and granular, showing characteristic features of adenoma (Figure 2).
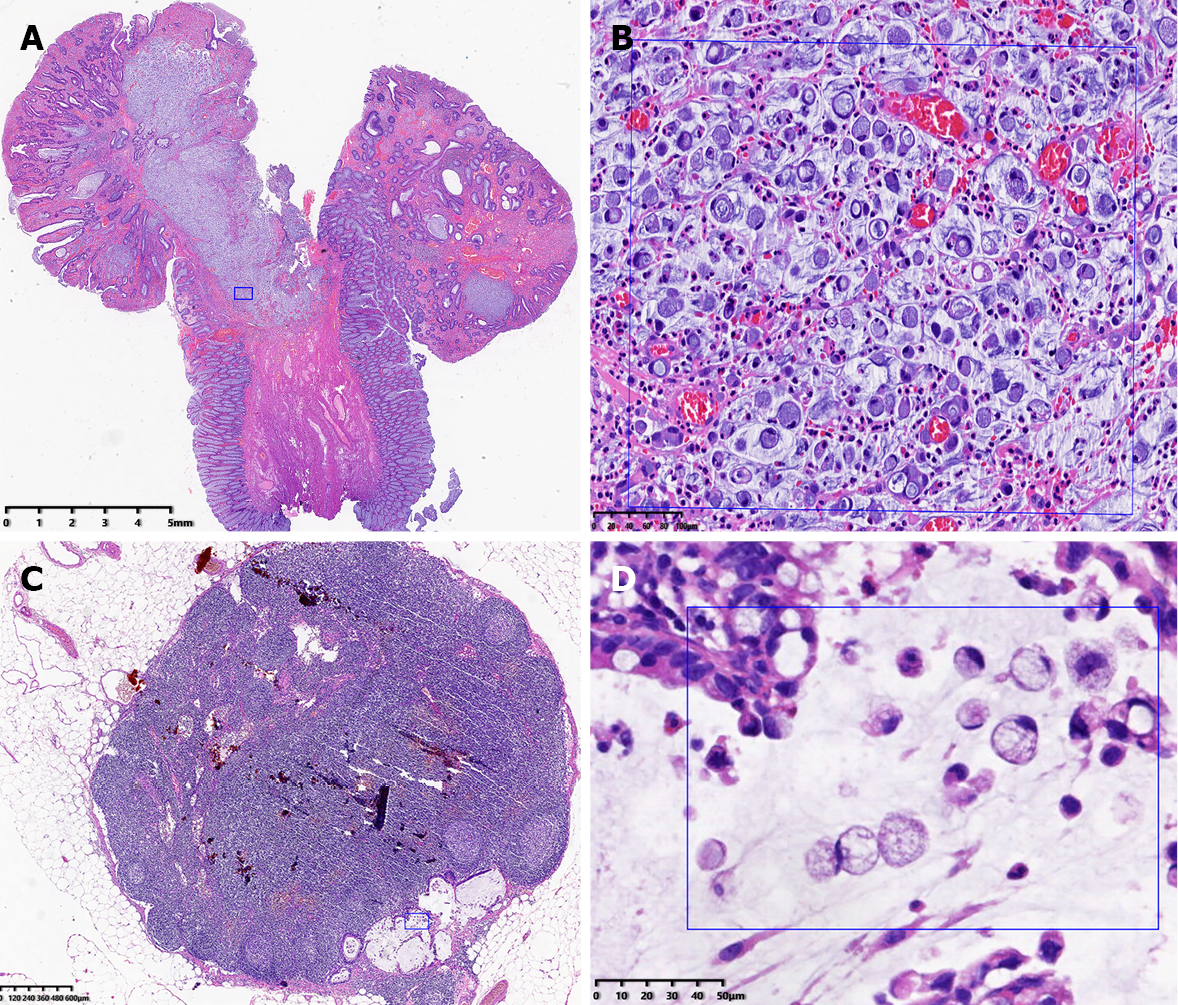
Histopathological examination showed high-grade intraepithelial neoplasia of the tumor surface and a negative margin, but a signet ring cell adenocarcinoma was found to infiltrate the submucosal layer of the first biopsy during colonoscopy. The deepest infiltration was approximately 0.9 cm from the tumor surface and 0.55 cm from the stratum basale (Figure 3A and B).
The second histopathological examination after operation showed signet ring cell adenocarcinoma infiltrating the submucosal layer as well as lymph node invasion (stage PT1N1M0 and grade IIIA in pathological grading, NRAS-, BRAF V600E-, KRAS-) (Figure 3C and D).
The final diagnosis was signet ring cell adenocarcinoma (stage PT1N1M0 and grade IIIA in pathological grading, NRAS-, BRAF V600E-, KRAS-).
We first ligated the root of the pedunculated polyp using nylon loops as well as a titanium clip and then performed polypectomy using a snare and fixed it at once (Figure 2D). The patient had a definite surgical indication and required additional surgery. We performed radical resection of the left colon with lymph node dissection after two weeks. This patient subsequently received a chemotherapy regimen with XELOX.
The patient was referred to the oncology department for the assessment of chemotherapy. The xelox chemotherapy regimen was well tolerated and established 8 times.
The incidence of signet ring cell carcinoma in the colon and rectum is low; most cases are usually detected only at an advanced stage[3]. Meanwhile, it is difficult to identify the pit pattern because signet ring cell carcinoma produces a large amount of mucus, and the structure of the pits is always destroyed[4]. Recent studies have shown that signet ring cell adenocarcinoma is more frequently found in men in the left-sided colon with a more advanced tumor–node–metastasis stage and worse outcomes than in women; the median overall survival in patients with stage IV disease was found to be 14 mo, which was much shorter than the 23.4 mo at the same stage[5]. To the best of our knowledge, this is the first report of signet ring cell carcinoma with such a large pedunculated polyp.
It has been revealed that the incidence of carcinoma in flat and depressed lesions is higher than that in pedunculated polyps, and few studies have focused on the strategy for pedunculated polyps[6]. Although pedunculated polyps are generally considered to pose a lower risk of lymph node metastases, it is necessary to ascertain the distinction between the head and stalk in pedunculated polyps. The depth of invasion of the stalk is critical for estimating lymph node invasion, formulating therapeutic schemes, and determining distal prognosis. Factors such as the depth of submucosal invasion (SM invasion depth) and histological type (differentiated adenocarcinoma, signetring cell carcinoma) have been reported to be risk factors for regional lymph node metastasis in pT1 (SM) carcinoma[7]. It has been suggested that the long stalk may play a protective role and suppress the invasive progression of malignant cells because sessile polyps are closer, hence facilitating infiltration, but this has not been proven[2]. Haggitt et al[8] proposed a new method to distinguish the level of invasion in a pedunculated malignant polyp and summarized the methods as follows: Level 1, invasive adenocarcinoma limited to the polyp head; Level 2, neck involvement; Level 3, carcinoma cells in the stalk; and Level 4, carcinoma cells infiltrating the submucosa at the level of the adjacent bowel wall, in which levels less than 4 indicate a low risk of metastasis. The European Society of Gastrointestinal Endoscopy 2015 guidelines advocate using the Haggitt classification for pedunculated polyps, and the Japanese Society for Cancer of the Colon and Rectum 2016 guidelines suggest measuring from the Haggitt line only in pedunculated lesions[9,10]. The Japanese Society for Cancer of the Colon and Rectum 2019 indicates that the lymph node metastasis rate in patients with a depth of invasion of 1000 μm or greater is 12.5%[11]. Emerging cases have revealed associations among the Haggitt level, lymph node invasion risk, and long-term prognosis[12,13]. However, we could not define the Haggitt line clearly because in this case, the stem base and long, large stalk were smooth, lacking the typical characteristics of adenoma, such as swelling mucous and an unstructured or excavated surface according to Kudo’s pit pattern classification[14]. Finally, we ensured that the Haggitt level was 4; this theory still deserves further study in larger patient cohorts for validation.
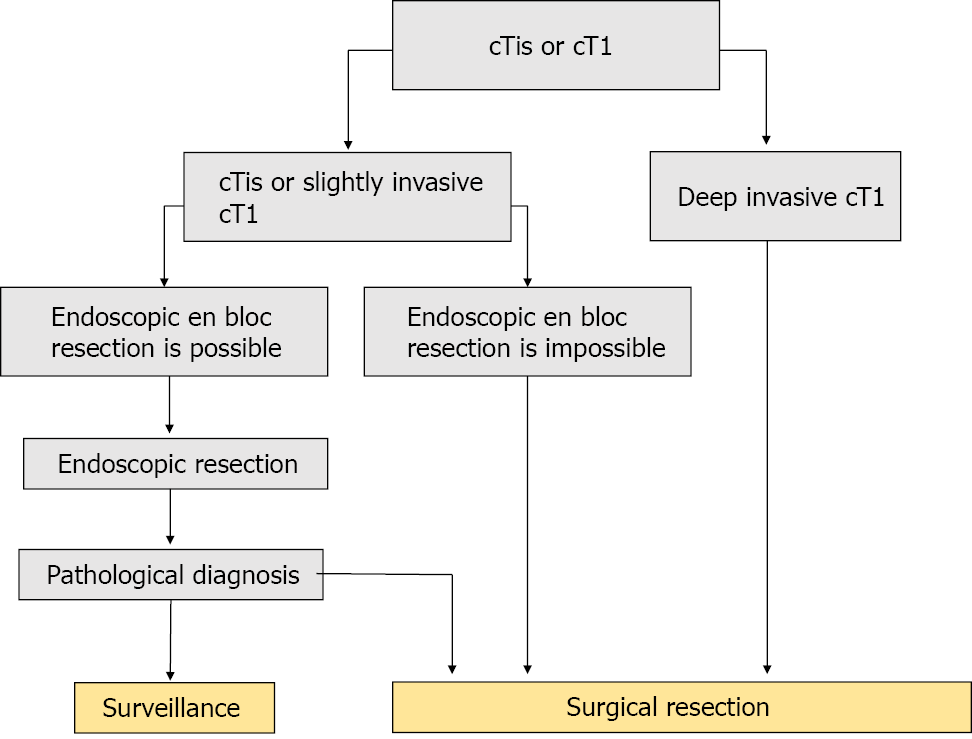
The principle of pT1 carcinoma treatment is intestinal resection with lymph node dissection. We refer to the treatment strategies for cTis and cT1 colorectal cancer from the Japanese Society for Cancer of the Colon and Rectum Guidelines shown in Figure 4[11]. In the present case, the lesion was obscure, hidden, and easy to overlook. Fortunately, our ligation position and polypectomy were thorough, and the deep lesion was suitable for surgery (depth of SM invasion ≥ 1000 µm and signet ring cell carcinoma)[11].
Polyps or adenomas removed via endoscopy must be sent for histopathology examination to be carefully evaluated by the pathologists keeping in their minds the possibility of underlying malignancy in a benign looking lesion, they should examine the lesion from the muscularis mucosae to the submucosa and describe the position precisely as well[15,16].
This case highlights the importance of paying attention to malignancy of large pedunculated polyps. Polyps or adenomas removed via endoscopy must be evaluated histologically. Even if adenomas may be fragile, endoscopy doctors should still remove polyps as completely as possible and choose perpendicular sections through the stalk and base to fix by formaldehyde solution.
We are grateful to our colleagues from the Department of Imaging, Laboratory, Pathology, and Infection for providing diagnostic and therapeutic assistance.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hasan A, Tadros M S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64721] [Article Influence: 16180.3] [Reference Citation Analysis (177)] |
| 2. | Ciocalteu A, Gheonea DI, Saftoiu A, Streba L, Dragoescu NA, Tenea-Cojan TS. Current strategies for malignant pedunculated colorectal polyps. World J Gastrointest Oncol. 2018;10:465-475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Ohnita K, Isomoto H, Akashi T, Hashiguchi K, Matsushima K, Minami H, Akazawa Y, Yamaguchi N, Takeshima F, To K, Takeshita H, Yasui H, Abe K, Nakao K. Early stage signet ring cell carcinoma of the colon examined by magnifying endoscopy with narrow-band imaging: a case report. BMC Gastroenterol. 2015;15:86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Fu KI, Sano Y, Kato S, Saito H, Ochiai A, Fujimori T, Saito Y, Matsuda T, Fujii T, Yoshida S. Primary signet-ring cell carcinoma of the colon at early stage: a case report and a review of the literature. World J Gastroenterol. 2006;12:3446-3449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Wei Q, Wang X, Gao J, Li J, Qi C, Li Y, Li Z, Shen L. Clinicopathologic and Molecular Features of Colorectal Adenocarcinoma with Signet-Ring Cell Component. PLoS One. 2016;11:e0156659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Kudo S. Endoscopic mucosal resection of flat and depressed types of early colorectal cancer. Endoscopy. 1993;25:455-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 594] [Cited by in RCA: 557] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 7. | Ueno H, Mochizuki H, Hashiguchi Y, Shimazaki H, Aida S, Hase K, Matsukuma S, Kanai T, Kurihara H, Ozawa K, Yoshimura K, Bekku S. Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology. 2004;127:385-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 501] [Cited by in RCA: 529] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 8. | Haggitt RC, Glotzbach RE, Soffer EE, Wruble LD. Prognostic factors in colorectal carcinomas arising in adenomas: implications for lesions removed by endoscopic polypectomy. Gastroenterology. 1985;89:328-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 515] [Cited by in RCA: 438] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 9. | Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 817] [Cited by in RCA: 929] [Article Influence: 92.9] [Reference Citation Analysis (0)] |
| 10. | Watanabe T, Muro K, Ajioka Y, Hashiguchi Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kawano H, Kinugasa Y, Kokudo N, Murofushi K, Nakajima T, Oka S, Sakai Y, Tsuji A, Uehara K, Ueno H, Yamazaki K, Yoshida M, Yoshino T, Boku N, Fujimori T, Itabashi M, Koinuma N, Morita T, Nishimura G, Sakata Y, Shimada Y, Takahashi K, Tanaka S, Tsuruta O, Yamaguchi T, Yamaguchi N, Tanaka T, Kotake K, Sugihara K; Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 2018;23:1-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 576] [Cited by in RCA: 603] [Article Influence: 86.1] [Reference Citation Analysis (0)] |
| 11. | Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, Ishihara S, Kanemitsu Y, Kinugasa Y, Murofushi K, Nakajima TE, Oka S, Tanaka T, Taniguchi H, Tsuji A, Uehara K, Ueno H, Yamanaka T, Yamazaki K, Yoshida M, Yoshino T, Itabashi M, Sakamaki K, Sano K, Shimada Y, Tanaka S, Uetake H, Yamaguchi S, Yamaguchi N, Kobayashi H, Matsuda K, Kotake K, Sugihara K; Japanese Society for Cancer of the Colon and Rectum. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1024] [Cited by in RCA: 1313] [Article Influence: 262.6] [Reference Citation Analysis (1)] |
| 12. | Matsuda T, Fukuzawa M, Uraoka T, Nishi M, Yamaguchi Y, Kobayashi N, Ikematsu H, Saito Y, Nakajima T, Fujii T, Murakami Y, Shimoda T, Kushima R, Fujimori T. Risk of lymph node metastasis in patients with pedunculated type early invasive colorectal cancer: a retrospective multicenter study. Cancer Sci. 2011;102:1693-1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | de Freitas Pinheiro N Junior, da Silva NDF. Diverging Ways of Determining Depth of Invasion in Pedunculated pT1 Colon Carcinomas. Arch Pathol Lab Med. 2020;144:671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Park W, Kim B, Park SJ, Cheon JH, Kim TI, Kim WH, Hong SP. Conventional endoscopic features are not sufficient to differentiate small, early colorectal cancer. World J Gastroenterol. 2014;20:6586-6593. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Kang SH, Chung WS, Hyun CL, Moon HS, Lee ES, Kim SH, Sung JK, Lee BS, Jeong HY. A rare case of a signet ring cell carcinoma of the colon mimicking a juvenile polyp. Gut Liver. 2012;6:129-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Hasan A, Nafie K, Aldossary MY, Ismail A, Monazea K, Baheeg M, Rady K, Elhawary R, Ibrahim AA. Unexpected histopathology results following routine examination of cholecystectomy specimens: How big and how significant? Ann Med Surg (Lond). 2020;60:425-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |