Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10362
Peer-review started: July 9, 2021
First decision: August 18, 2021
Revised: August 29, 2021
Accepted: September 19, 2021
Article in press: September 19, 2021
Published online: November 26, 2021
Processing time: 135 Days and 21.4 Hours
Iodophor (povidone-iodine) is widely used clinically because of its broad-spectrum antibacterial effects. Although extremely rare, it may cause anaphylactic shock, which itself carries the life-threatening risk of cardiac arrest.
We present a case in which a patient with postoperative infection went into anaphylactic shock and cardiac arrest caused by povidone-iodine during secondary surgery. The patient was successfully resuscitated by 2 h of cardiopulmonary resuscitation.
This is the first known case of cardiac arrest caused by povidone-iodine allergy.
Core Tip: We report a rare case of cardiac arrest caused by povidone-iodine allergy, representing a life-threatening complication never reported before. The patient was successfully resuscitated by 2 h of cardiopulmonary resuscitation, which suggests that a favorable outcome of prolonged cardiopulmonary resuscitation is possible.
- Citation: Xiang BB, Yao YT, Jiao SL. Successful prolonged cardiopulmonary resuscitation after intraoperative cardiac arrest due to povidone-iodine allergy: A case report. World J Clin Cases 2021; 9(33): 10362-10368
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10362.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10362
Iodophor (povidone-iodine) is an iodine complex formed by molecular iodine and polyvinylpyrrolidone (also called "povidone") in combination with surfactants[1]. Povidone-iodine is widely used clinically because of its broad-spectrum antibacterial effect[2]. Several cases of skin allergies caused by povidone-iodine have been reported, but cases of the drug-induced anaphylactic shock are extremely rare. Here, we present the first case of cardiac arrest caused by a povidone-iodine allergy. The American Heart Association recommends stopping resuscitation for patients who do not respond to at least 20 min of advanced cardiovascular life support[3]. Our pediatric patient had a postoperative infection and went into anaphylactic shock with cardiac arrest due to povidone-iodine administration during secondary surgery. She was successfully resuscitated after 2 h of cardiopulmonary resuscitation (CPR).
A 9-year-old girl was admitted to our hospital for treatment of postoperative infection after orthopedic surgery for a spinal deformity.
The patient was found to have spinal malformation four years ago, and then she underwent spinal orthopaedic surgery in our hospital one year ago. The patient developed wound infection a week ago and came to our hospital for further treatment.
The patient had no history of hypertension, coronary disease, or diabetes mellitus. The patient was allergic to penicillin and cephalosporins.
Personal and family history of the patient was normal.
Findings from physical examination on admission were normal, except for presence of a slight scoliosis.
Routine preoperative evaluations did not show any pre-existing abnormalities.
Routine preoperative evaluations did not show any pre-existing abnormalities.
We conducted a skin sensitivity test on the patient during the postoperative follow-up and found that she was indeed allergic to povidone-iodine. By reviewing the experience of the previous surgery and anesthesia, we ruled out the possibility that this patient was allergic to the anesthetic and ancillary drugs (i.e., sevoflurane, dexmedetomidine, propofol, remifentanil, sufentanil, rocuronium, crystal liquid, hydroxyethyl starch solution, succinyl gelatin solution). In addition, when the patient underwent re-operation 1 year later, we avoided the use of povidone-iodine and the patient did not develop allergies during operation.
Postoperative infection debridement and unilateral internal fixation removal were performed under general anesthesia with tracheal intubation on March 29, 2019. After entering the operating room at 08:00, pulse oxygen saturation (SpO2), electrocardiogram (ECG) and body temperature were monitored. Before general anesthesia, the patient’s blood pressure was 84/54 mmHg, heart rate was 98 beats/min, oxygen saturation was 100%, and body temperature was 36.5 °C. Anesthesia induction was performed at 08:30, with intravenous injection of sufentanil (15 µg), propofol (50 mg), and rocuronium (20 mg), followed by tracheal intubation and end-tidal CO2 (ETCO2) monitoring. At that time, the ETCO2 was 38 mmHg and the airway peak pressure was 14 cm H2O. Then, radial artery puncture and deep vein catheterization were performed for continuous invasive arterial intra-arterial blood pressure and central venous pressure (CVP) monitoring. Continuously-pumped remifentanil (at 10 µg/kg/h), dexmedetomidine (at 0.4 µg/kg/h), and sevoflurane (2%) were administered to maintain anesthesia.
At 09:40 during the initial operation, the surgeon disinfected the skin with dilute povidone-iodine (Batch No. 20200703S; Shanghai Likang Disinfection High-tech Co., Ltd., Shanghai, China), during which transient hypotension occurred at 56/37 mmHg and then the blood pressure returned to normal at 86/53 mmHg after treatment with 3 mg ephedrine. Subsequently, the operation was started and the blood pressure was stable. At 11:15, the surgical wound was rinsed with dilute povidone-iodine, during which the blood pressure dropped to 65/37 mmHg and the heart rate rose to 112 beats/min. The blood pressure returned to normal at 81/47 mmHg after intravenous administration of 3 mg ephedrine. At 11:42, the surgical wound was irrigated with a large amount of povidone-iodine. Suddenly, the blood pressure waveform became low and flat and the arterial pulsation became weak, with the airway pressure soaring to 30 cm H2O. Suspecting anaphylactic shock caused by povidone-iodine, which would have infiltrated the blood system through the surgical wound, antiallergic treatment was given immediately by injecting 100 µg epinephrine and 40 mg methylprednisolone intravenously. Due to the non-exclusivity of anesthetic allergies, the anesthesia maintenance medications (i.e., dexmedetomidine, intravenous remifentanil and sevoflurane) were discontinued immediately, and then 2 mg midazolam was given intravenously. Even so, the patient’s condition worsened. The ECG waveform and blood pressure waveform disappeared, and the carotid pulse could not be felt. The surgeon immediately stopped the operation and closed the incision with a sterile surgical towel.
CPR was performed after the patient was turned over and an injection of 1 mg epinephrine was given intravenously six times. Spontaneous circulation returned at 11:49, but cardiac arrest occurred again at 11:58. Immediately, CPR was performed again and intravenous injection of 1 mg epinephrine was given a total of 30 times. The epinephrine was pumped at 0.1-0.2 µg/kg/min, norepinephrine was pumped at 0.1-0.3 µg/kg/min and dopamine was pumped at 5-10 µg/kg/min continuously. At 12:30, the depth of anesthesia was enhanced by administering sufentanil (10 µg), midazolam (2 mg), and vecuronium (4 mg). At 13:42, spontaneous circulation returned, but was followed by cardiac arrest reoccurrence; at 13:47, spontaneous circulation returned. At that time, the patient’s blood pressure was 136/87 mmHg, heart rate was 121 beats/min, and ETCO2 was 42 mmHg.
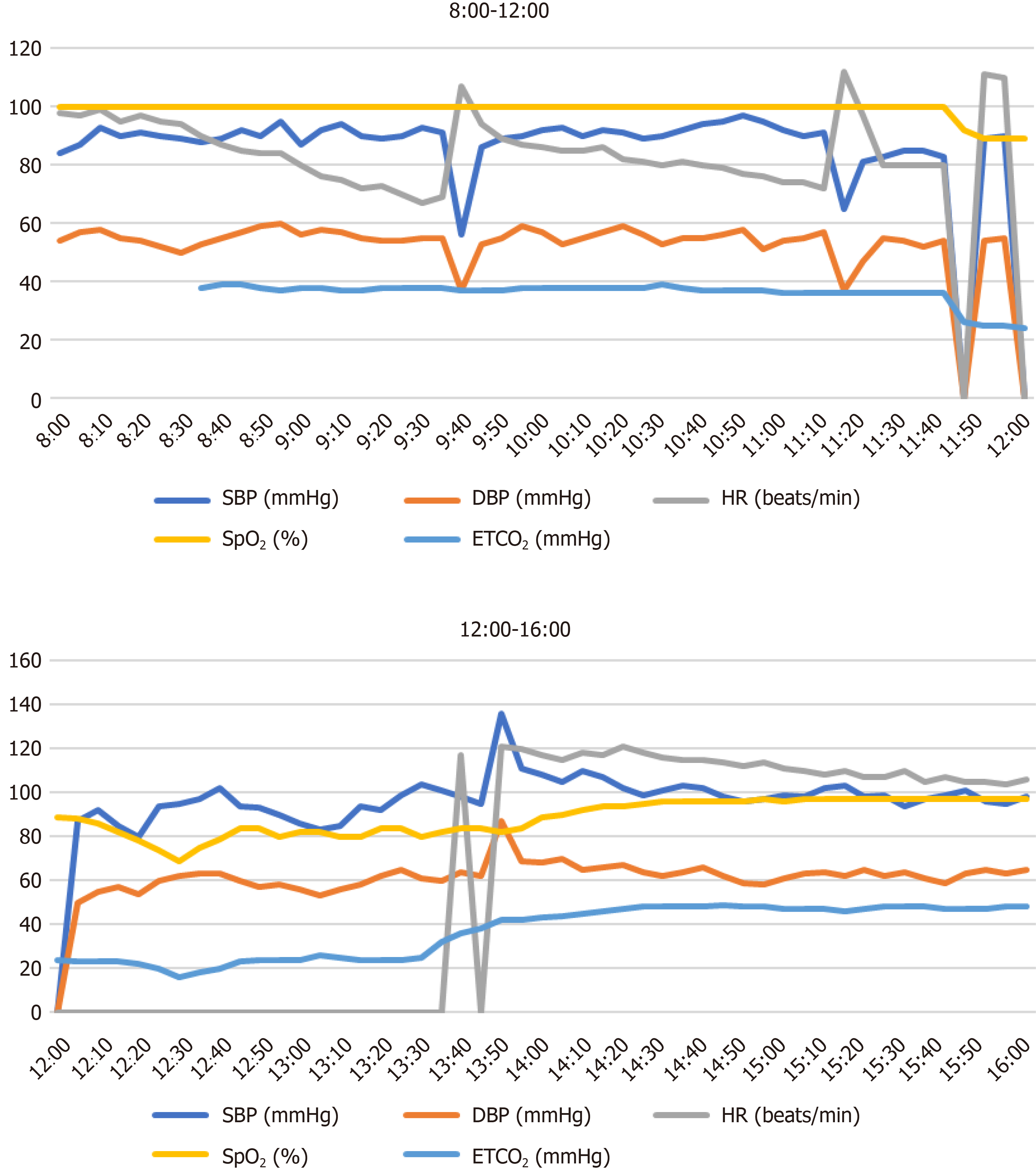
After observation for about 1 h, the patient's vital signs were stable under the maintenance of vasoactive drugs. At 14:45, the patient was turned over into the lateral position and the operation was continued, with intravenous injection of midazolam (5 mg), continuous remifentanil pumping (at 10 µg/kg/h) and inhalation of sevoflurane (2%). The surgical incision was sutured at 17:00, and the operation was completed. At 17:20, the patient was sent to the intensive care unit under endotracheal intubation for postoperative intensive care, with continuous norepinephrine pumping (at 0.3 µg/kg/min) and epinephrine (at 0.15 µg/kg/min) intravenously. When she left the operating room, her blood pressure was 106/62 mmHg, heart rate was 98 beats/min, SpO2 was 97%, CVP was 12 mmHg, and body temperature was 35 °C. Both pupils were equally large and round, with a diameter of approximately 3 mm. Figure 1 demonstrates the intraoperative vital signs.
The patient's vital signs and general condition were stable after 4 h follow-up. The tracheal tube was removed on March 31, 2019 and the patient was discharged from the hospital on May 16, 2019. No related neurological complications were found during the 1 year of follow-up.
Povidone-iodine is an unshaped binding compound composed of iodine, povidone and surfactant that is widely used in the clinic due to its broad-spectrum antibacterial effect[2]. So far, there have been no reports on the resistance of bacteria to povidone-iodine. Rinsing or soaking with dilute povidone-iodine solution in spinal surgery is routinely used for debridement of patients with postoperative infection or trauma. Since 1998, approximately 8 cases of immunoglobulin E-mediated allergy to povidone-iodine after disinfecting skin or mucosa have been reported (Table 1). Hypersensitivity reactions to povidone are immediate[1,4]. Since the early 1980s, however, approximately 40 cases of delayed allergic reaction to povidone-iodine have been reported, for an estimated incidence of 0.4%. Nonoxynol, a surfactant, is the allergen of povidone-iodine implicated as the cause of delayed hypersensitivity reactions. Since 2010, unlike povidone-iodine (Mylan), povidone-iodine (Betadine) no longer contains nonoxynol. Delayed hypersensitivity to povidone-iodine usually manifests as contact dermatitis, and does not lead to anaphylactic shock.
| Ref. | Age in year | Sex | Site | Onset delay | Clinical features | Skin testing |
| López Sáez et al[9], 1998 | 27 | M | Skin wound | Immediately | Pruritus of the soles, generalized urticaria, facial angioedema | + |
| Adachi et al[10], 2003 | 59 | F | Mucosa | 10 min | Pruritus in the genital area, erythema, generalized urticaria, SAP: 40 mmHg, dyspnea | + |
| Le Pabic et al[11], 2003 | 32 | M | Surgical wound | A few minutes | Anaphylactic shock and acute respiratory distress syndrome | + |
| Pedrosa et al[12], 2005 | 9 | M | Skin | 10 min | Urticaria, facial angioedema, dyspnea | + |
| Komericki et al[13], 2014 | 42 | M | Surgical wound | 15 min | generalized urticaria, tongue swelling, SAP: 94 mmHg, moderate bronchospasm | + |
| Gray et al[14], 2013 | 12 | F | Skin wound | Not mentioned | Not detailed, one previous allergy include generalized urticaria, facial angioedema and shortness of breath | + |
| Castelain et al[15], 2016 | 56 | M | Knee wound | Immediately | Pruritus on the knee spreading to the whole body, generalized erythema, sweating, SAP: 70 mmHg | + |
| Moreno-Escobosa[16], 2017 | 4 | M | Skin wound | 20 min | Eyelids angioedema, generalized urticaria, SAP: 80 mmHg | + |
From a pathophysiological point of view, anaphylactic shock is an extreme manifestation of immediate hypersensitivity. In our case, the patient suffered from anaphylactic shock due to povidone-iodine, which is considered to be an immediate allergic reaction caused by povidone. Dewachter et al[1] have shown that iodine never participates in the allergic reaction of povidone-iodine, which contrasts with our previous impression of an "iodine allergy". Krohne et al[5] also observed this phenomenon, and confirmed that there is no cross-reaction between different classes of iodine-containing drugs. Therefore, people allergic to iodized contrast agents are not prohibited from using povidone-iodine, and there is no evidence supporting the avoidance of iodized drugs in patients allergic to seafood. Therefore, pre-existing allergic diseases should be carefully considered during preoperative evaluation. If a patient is identified as allergic to povidone-iodine, then if povidone-iodine is necessary to irrigate the wound to avoid or treat surgical site infection, it may be replaced with vancomycin powder.
The "2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care"[6] pointed out that when ETCO2 is less than 10 mmHg after 20 min of CPR that is, when the patient does not respond to at least 20 min of advanced life support termination of resuscitation should be considered. However, in recent years, many cases of successful CPR exceeding the traditional 20 min have been reported. Although the majority have had a poor outcome, certain successful cases with complete neurological recovery have been reported. Relevant studies have confirmed that when CPR lasts more than 20 min, the resuscitation success rate falls to 25.5% and the survival rate falls to 5.6%[7]. Considering that the patient in this case was relatively young with no underlying diseases, and the cause of cardiac arrest, anaphylactic shock, was clear and reversible, the whole rescue team chose to continue the rescue even though the CPR had lasted more than 20 min, which involved timely communication with the patient's family and their signing of an informed consent form. The patient was finally resuscitated after continuing CPR for 2 h. This case proves that the duration of CPR can be extended under appropriate circumstances.
Cardiac arrest due to complications related to surgery or anesthesia has been found to be inversely correlated with intraoperative immediate death and postoperative 3-mo mortality[8]. High-quality CPR is also considered to be one of the important factors influencing whether to prolong the duration[6]. Continuous invasive blood pressure and ETCO2 monitoring can better guide CPR, so as to ensure the quality of CPR. During CPR in this case, ETCO2 was mostly maintained above 20 mmHg and mean blood pressure was above 70 mmHg. In addition, blood gas analysis provides important objective evidence, and prompted our team to continue with the CPR, which can often provide a basis for predicting the outcome of patients with cardiac arrest.
In general, anaphylactic shock caused by povidone-iodine is extremely rare. Obviously, early detection of povidone-iodine allergy is very important. For patients allergic to povidone-iodine, the drug should be avoided and switched to another disinfectant agent. Constant vigilance is needed when using large amounts of povidone-iodine to irrigate a wound during operation. In this case, the ultimate success of the rescue after a 2-h CPR was due to many factors, such as timely and rapid treatment, high-quality CPR, good preoperative basic conditions, and a reversible cause of cardiac arrest. Determining when to appropriately halt the rescue remains a major challenge. The decision to try prolonged and active CPR may be a difficult one, but this case highlights some factors, such as the high ETCO2 levels and good blood gas analysis results, that favor such a decision and shows that a favorable outcome is possible.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Elpek GO, Nyamuryekung'e M S-Editor: Yan JP L-Editor: A P-Editor: Xing YX
| 1. | Dewachter P, Mouton-Faivre C. [Allergy to iodinated drugs and to foods rich in iodine: Iodine is not the allergenic determinant]. Presse Med. 2015;44:1136-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Lemans JVC, Wijdicks SPJ, Boot W, Govaert GAM, Houwert RM, Öner FC, Kruyt MC. Intrawound Treatment for Prevention of Surgical Site Infections in Instrumented Spinal Surgery: A Systematic Comparative Effectiveness Review and Meta-Analysis. Global Spine J. 2019;9:219-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL Jr, Lasa JJ, Lavonas EJ, Levy A, Mahgoub M, Meckler GD, Roberts KE, Sutton RM, Schexnayder SM; Pediatric Basic and Advanced Life Support Collaborators. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S469-S523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 285] [Article Influence: 57.0] [Reference Citation Analysis (0)] |
| 4. | Dewachter P, Kopac P, Laguna JJ, Mertes PM, Sabato V, Volcheck GW, Cooke PJ. Anaesthetic management of patients with pre-existing allergic conditions: a narrative review. Br J Anaesth. 2019;123:e65-e81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 5. | Krohne TU, Allam JP, Novak N, Holz FG. ["Iodine allergy" : A medical myth with risks for the ophthalmological patient]. Ophthalmologe. 2016;113:1023-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Panchal AR, Berg KM, Hirsch KG, Kudenchuk PJ, Del Rios M, Cabañas JG, Link MS, Kurz MC, Chan PS, Morley PT, Hazinski MF, Donnino MW. 2019 American Heart Association Focused Update on Advanced Cardiovascular Life Support: Use of Advanced Airways, Vasopressors, and Extracorporeal Cardiopulmonary Resuscitation During Cardiac Arrest: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2019;140:e881-e894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 94] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 7. | Youness H, Al Halabi T, Hussein H, Awab A, Jones K, Keddissi J. Review and Outcome of Prolonged Cardiopulmonary Resuscitation. Crit Care Res Pract. 2016;2016:7384649. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Bell D, Gluer R, Murdoch D. Factors Promoting Survival After Prolonged Resuscitation Attempts: A Case of Survival With Good Neurological Outcome Following 60 Minutes of Downtime After Out-of-Hospital Cardiac Arrest. Heart Lung Circ. 2018;27:e1-e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | López Sáez MP, de Barrio M, Zubeldia JM, Prieto A, Olalde S, Baeza ML. Acute IgE-mediated generalized urticaria-angioedema after topical application of povidone-iodine. Allergol Immunopathol (Madr). 1998;26:23-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 10. | Adachi A, Fukunaga A, Hayashi K, Kunisada M, Horikawa T. Anaphylaxis to polyvinylpyrrolidone after vaginal application of povidone-iodine. Contact Dermatitis. 2003;48:133-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Le Pabic F, Sainte-Laudy J, Blanchard N, Moneret-Vautrin DA. First case of anaphylaxis to iodinated povidone. Allergy. 2003;58:826-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Pedrosa C, Costa H, Oliveira G, Romariz J, Praça F. Anaphylaxis to povidone in a child. Pediatr Allergy Immunol. 2005;16:361-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Komericki P, Grims RH, Aberer W, Kränke B. Near-fatal anaphylaxis caused by human serum albumin in fibrinogen and erythrocyte concentrates. Anaesthesia. 2014;69:176-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Gray PE, Katelaris CH, Lipson D. Recurrent anaphylaxis caused by topical povidone-iodine (Betadine). J Paediatr Child Health. 2013;49:506-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Castelain F, Girardin P, Moumane L, Aubin F, Pelletier F. Anaphylactic reaction to povidone in a skin antiseptic. Contact Dermatitis. 2016;74:55-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Moreno-Escobosa MC. Aanaphylactic shock due to povidone. J Paediatr Child Health. 2017;53:517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |