Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10328
Peer-review started: July 10, 2021
First decision: July 26, 2021
Revised: August 8, 2021
Accepted: September 10, 2021
Article in press: September 10, 2021
Published online: November 26, 2021
Processing time: 134 Days and 21 Hours
Total pharyngo-laryngo-esophagectomy with a reconstruction of gastric pull-up is the most common treatment method for patients with multiple primary upper digestive tract carcinomas, such as hypopharyngeal carcinoma with thoracic esophageal carcinoma. However, neck circumferential defect and tracheoesophageal fistula after gastric necrosis are still challenging problems for surgeons and patients.
This case report presents 2 patients who underwent reconstructive surgeries using 4 local random flaps with a split thickness skin graft in the first case, and 6 local random flaps in the second case to close the circumferential defect and tracheoesophageal fistula after failed gastric pull-up. Both patients achieved good swallowing function and could take solid diet without dysphagia postoperatively.
For selected patients, local random flaps (with a split thickness skin graft) can be a simple and reliable solution for reconstructing tracheoesophageal fistula or cervical circumferential defect after gastric necrosis, especially when the necrosis extends below the thoracic inlet.
Core Tip: In this paper, we report 2 patients who suffered from cervical circumferential defect and tracheoesophageal fistula, reconstructed with local random flaps (with a split thickness skin graft in the first case), after failed gastric pull-up. Both patients achieved good swallowing function without dysphagia postoperatively. Local random flaps and split thickness skin graft have the advantages of easy to harvest with abundant and flexible donor sites. Herein, local random flaps (with a split thickness skin graft) can be a simple and reliable solution for reconstructing tracheoesophageal fistula or cervical circumferential defect after gastric necrosis.
- Citation: Zhang Y, Liu Y, Sun Y, Xu M, Wang XL. Local random flaps for cervical circumferential defect or tracheoesophageal fistula reconstruction after failed gastric pull-up: Two case reports. World J Clin Cases 2021; 9(33): 10328-10336
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10328.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10328
Hypopharyngeal carcinoma is one of the most common head and neck squamous cell carcinomas. It is usually diagnosed at an advanced stage and results in substantial morbidities and mortalities. In addition, through routine esophagoscope examination, hypopharyngeal carcinoma patients are often diagnosed with second primary esophageal squamous cell carcinoma, with the incidence rate ranging from 10% to 51.5%[1-3]. Total pharyngo-laryngo-esophagectomy is the most common treatment method for patients with multiple primary upper digestive tract carcinomas such as hypopharyngeal carcinoma with thoracic esophageal carcinoma. It is worth noting that gastric pull-up is usually used as a reconstruction method after pharyngo-laryngo-esophagectomy. However, postoperative complications associated with gastric pull-up, especially circumferential necrosis at the anastomotic site and tracheoesophageal fistula, poses a significant challenge for surgeons and patients and it may result in high mortality rates. Therefore, the reconstruction in neck and the upper mediastinum after circumferential necrosis of the gastric conduit or tracheoesophageal fistula is essential. It can help patients achieve better quality of life and prognosis. Previous studies have reported use of pedicled flaps such as the pectoralis major musculocutaneous flap, trapezius myocutaneous flap, and latissimus dorsi myocutaneous flap to reconstruct circumferential hypopharyngeal defects[4-6]. Moreover, improvement of microvascular techniques has led to widespread use of free flaps including the anterolateral thigh flap and the jejunal free flap[7,8]. Colonic interposition has also been used to deal with gastric pull-up failure[9]. In this paper, we present 2 cases of circumferential reconstruction and tracheoesophageal fistula, after failed gastric pull-up, using local random flaps (and split thickness skin graft).
Case 1: A 58-year-old man, presented the complaint of circumferential necrosis at the cervical part of the gastric conduit. It was 12 d after a total pharyngo-laryngo-esophagectomy with gastric pull-up for his hypopharyngeal squamous cell carcinoma with multiple primary esophageal cancer.
Case 2: A 70-year-old man, presented a pharyngeal fistula and tracheoesophageal fistula for 10 mo after a total pharyngo-laryngo-esophagectomy with gastric pull-up.
Case 1: The patient presented with the complaint of hoarseness for half a year and odynophagia for 3 mo. He did not complain about dysphasia and could eat solid foods without weight loss. Initial evaluation using laryngoscopy and esophagoscopy showed a lesion occupying the right pyriform sinus and extending to the inferior postcricoid, right ary-epiglottic fold, right pharyngo-epiglottic fold, both arytenoids, the lingual surface of epiglottis, and the entrance of cervical esophagus. Several small focuses were found in the left pyriform sinus and the posterior hypopharyngeal wall. Moreover, flat lesions were found in thoracic esophagus, 36-38 cm from incisors. A biopsy confirmed all lesions to be squamous cell carcinoma. Thus, the patient underwent total pharyngo-laryngo-esophagectomy with gastric pull-up, and also bilateral neck dissection (level II-IV and VI). Furthermore, tracheostoma was made between the fourth and the fifth tracheal ring. Next, a nasogastric tube and a jejunal feeding tube were routinely placed for postoperative gastrointestinal decompression and enteral nutrition. On the 7th postoperative day, the patient started to drink water through his mouth but it was hard to swallow it down. He started taking a liquid diet on the 12th postoperative day. However, the cervix drainage fluid turned turbid and black. On the next day, a circumferential necrosis at the cervical part of the gastric conduit was found using video laryngoscopy. The patient presented with sepsis and toxemia symptoms.
Case 2: The patient underwent a total pharyngo-laryngo-esophagectomy with gastric pull-up and bilateral neck dissection (level II-IV and VI) 10 mo earlier in order to cure his hypopharyngeal carcinoma in another hospital. The immediate postoperative recovery was normal. On the 7th postoperative day, the drainage fluid of anastomotic stoma unexpectedly increased to 70 mL/24 h, and turned stink and black. Exploration and debridement were performed, however, no evidence of fistula or necrosis was found. So, the exploration did not enter the pharyngeal cavity. Iodoform gauze was used to pack the wound left by the exploration. Upper gastrointestinal roentgenography was performed on the 15th postoperative day. No obvious contrast medium extravasation was detected. Therefore, the patient started a liquid diet and the drainage tube was removed on the 21st postoperative day without drainage. Three days later, a fistula was found on the posterior wall of the tracheostoma, with a lot of purulent secretion. Thus, the patient underwent an emergency surgery through the original incision for a second-time exploration and debridement. Intraoperatively, extensive necrosis of the anterior wall of the gastric conduit was found which also led to a defect on the upper and posterior wall of the tracheostoma, thereby resulting in a pharyngeal fistula with tracheoesophageal fistula. The dressing was regularly changed for 9 mo in order to avoid aspiration and provide a bed of fresh granulation tissue. The patient was then sent to our center for reconstruction.
Cases 1 and 2: The patient had a free previous medical history.
Case 1: The patient is a known alcoholic and smoker. He had no other special personal and family history.
Case 2: The patient was an alcoholic and smoker, who quit after diagnosis of hypopharyngeal carcinoma. He had no other special personal and family history.
Case 1: Physical examination revealed turbid and black cervix drainage with redness and swelling around the surgical site. Body temperature raised to 39 ℃.
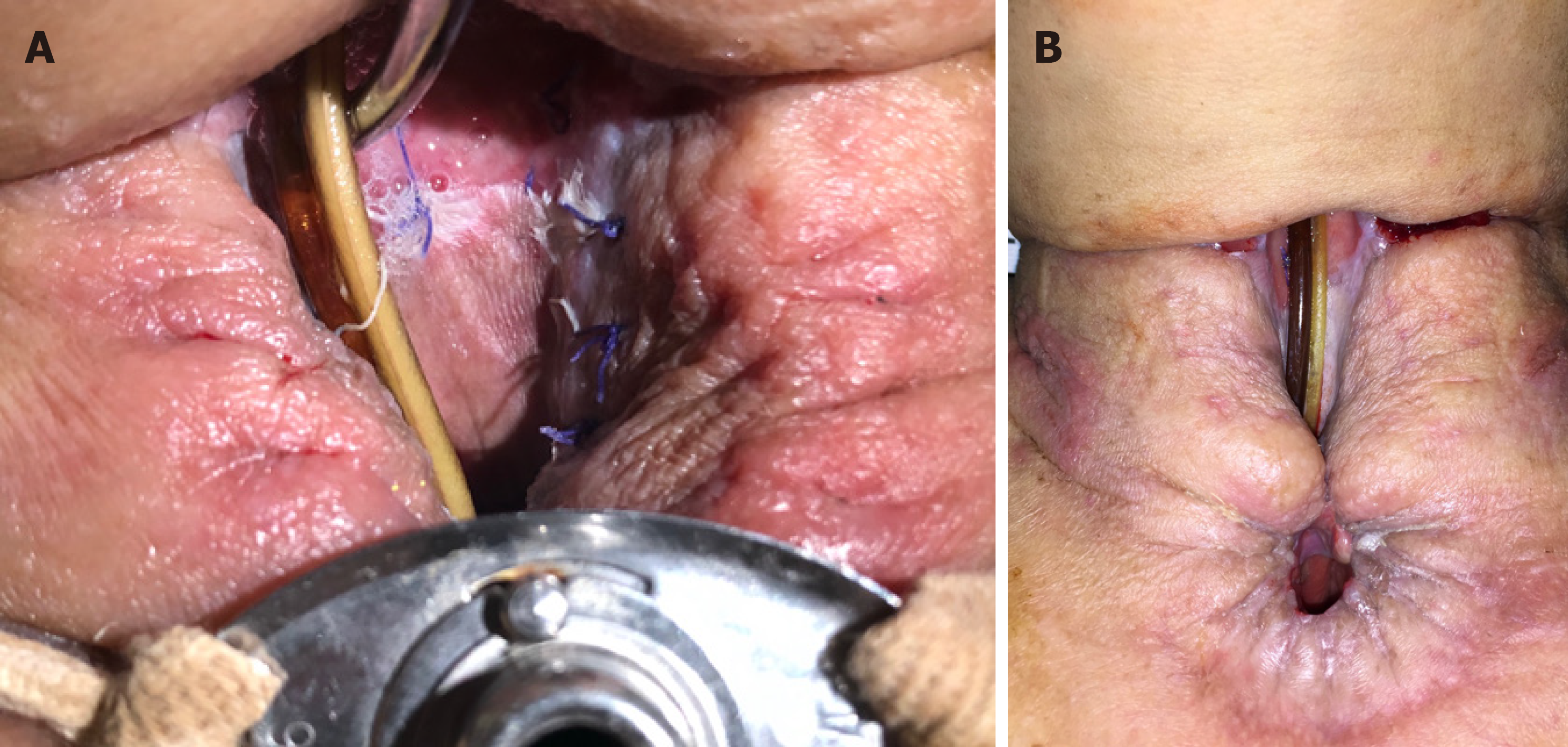
Case 2: Physical examination revealed a defect on the patient’s neck with missing anterior wall of the pharyngeal and the upper wall of the tracheostoma (Figure 1).
Case 1: Leukocyte cell count (13.78 × 109/L), neutrophil count (12.16 × 109/L), neutrophilic granulocyte percentage (88.2%) and C-reactive protein (10.9 mg/dL) were all elevated.
Case 2: Laboratory examinations had normal results.
Case 1: Video laryngoscopy showed a circumferential necrosis at the cervical part of the gastric conduit. Bedside chest X-ray film indicated a normal pulmonary film without pleural effusion.
Case 2: Video laryngoscopy and gastroscopy showed the continuity of digestive tract was well upper and below the pharyngeal fistula and tracheoesophageal fistula. The neck and chest computed tomography (CT) showed pharyngeal fistula communicated with cervical skin and tracheostoma, without fluid collection in the mediastinum and in the pleural cavity.
The final diagnosis of the presented case was a circumferential necrosis at the cervical part of the gastric conduit after total pharyngo-laryngo-esophagectomy with gastric pull-up, leading to sepsis and toxemia.
The final diagnosis of the presented case was pharyngeal fistula and tracheoesophageal fistula after total pharyngo-laryngo-esophagectomy with gastric pull-up.
The patient was taken up for emergency exploration and debridement. The exploration was performed through the original T-type incision. Intraoperatively, circumferential necrosis was found from the anastomotic line to the thoracic inlet in the anterior wall, and below the thoracic inlet in the posterior wall. Thus, debridement of necrotized tissues and extensive irrigation of the cavity with 3% hydrogen peroxide followed by sterile normal saline were performed. Then the cavity left after debridement was packed with iodoform gauze. The dressing was changed regularly for 1 mo with gauze packed in to keep the entrance to the pulled-up stomach open, and to maintain the tubular shape of the cervical cavity and a bed of fresh granulation tissue for the subsequent reconstruction.
Next, the patient was taken to the operation room for the third time. A 4 cm × 3 cm split thickness skin obtained from the right thigh, was applied to the posterior aspect and sidewall of the wound, in a tie-over fashion. In addition, a chest tube was put through the entrance of the thoracic inlet in order to avoid stricture. The tie-over dressing was removed on the 4th postoperative day and the graft was found completely successful (Figure 2A).
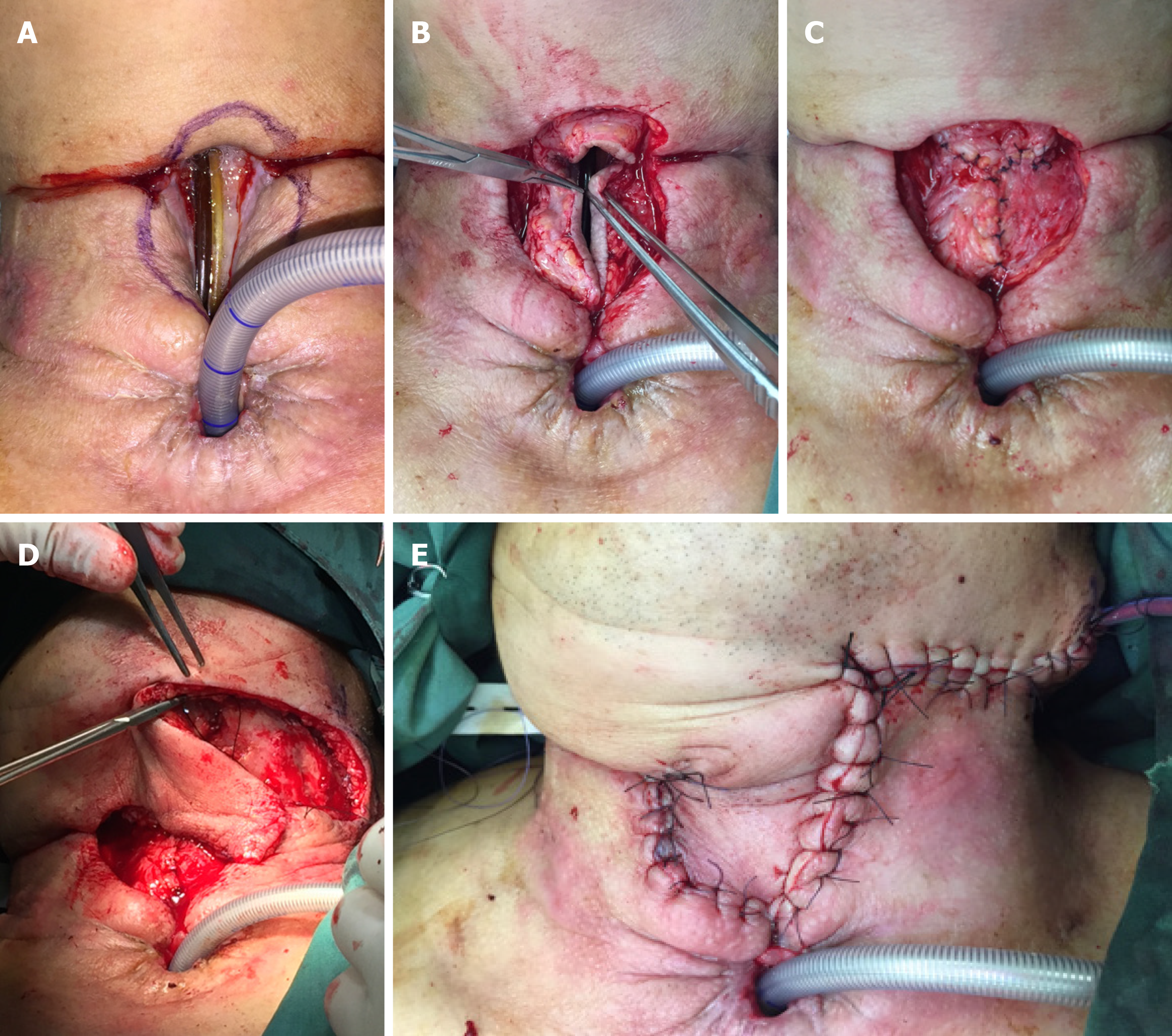
After another 20 d, the skin graft stably healed with the surrounding granulation and the cervical skin (Figure 2B). Therefore, a fourth operation was arranged to close the defect. The surrounding tissue including the skin was used as the anterior wall of the pharynx from three directions; the cephalic, left, and right sides (Figure 3A-C). Finally, a random flap was taken from the submandibular part and was used to cover the anterior surface defect of the neck, followed by putting a drainage under the flap (Figure 3D and E).
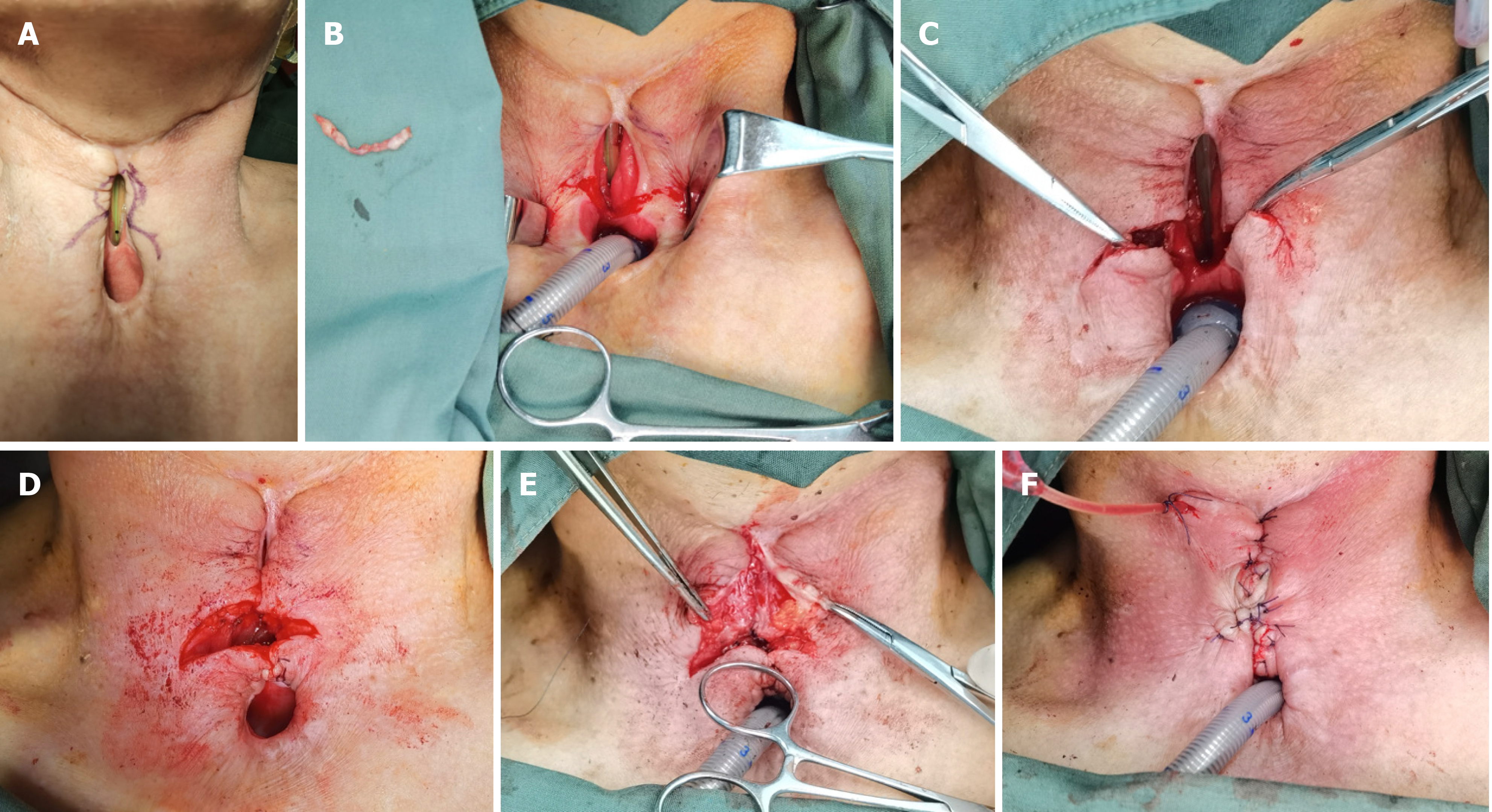
An operation was arranged with the aim of closing the pharyngeal fistula and tracheoesophageal fistula. The surrounding tissue including the skin was divided into two parts, the upper part and the lower part. The lower part used as random flap was turned over to close the tracheoesophageal fistula, and became the upper and posterior walls of the tracheostoma (Figure 4A-D). Next, the side walls of the pharyngeal fistula were used as the anterior wall of the pharynx (Figure 4E). Finally, the upper part of the surrounding skin and subcutaneous tissue, used as another local random flap, were sewed with the reconstructed upper wall tissue of the tracheostoma in an “inverted-T” fashion in order to close the skin defect (Figure 4F).
On the next day after debridement, the general condition of the patient recovered visibly. Leukocyte cell count (7.09 × 109/L), neutrophil count (4.89 × 109/L), neutrophilic granulocyte percentage (69%) and C-reactive protein (4.69 mg/dL) all declined. And, the body temperature returned to normal. Twelve days after the final step of the reconstruction process, the patient began to take a liquid diet. Furthermore, we performed upper gastrointestinal roentgenography, which found a small fistula. Conservative treatment was conducted with drainage and dressing change for 2 wk. And, the patient could finally take a solid diet without dysphagia.
On the 7th postoperative day, upper gastrointestinal roentgenography was performed which indicated that there was no obvious contrast medium extravasation. Therefore, the patient was started on a liquid diet and the drainage tube was removed on the 8th postoperative day. Results indicated that the recovery was smooth. No new fistula was found and the patient could take a solid diet without dysphagia.
Gastric pull-up is one of the most common reconstruction methods for patients using total pharyngo-laryngectomy or pharyngo-laryngo-esophagectomy. The method is effective because it provides sufficient tissue for the reconstruction of circumferential defect, with only one anastomotic stoma. Moreover, the morbidity of gastric necrosis is not so high, ranging from 0% to 24%[10,11]. Although the circumferential necrosis rate is even less, vigilance for the necrosis is always required because necrosis can lead to death[12]. There are several common risk factors for gastric necrosis, which can be divided into four parts: direct angiogenic factors, including twisting and overstretching the supplying vascular; gastric wall factors, including gastric ulcer, tight restrictive hiatus, and external beam irradiation; physical condition factors, including low perioperative cardiac output, postoperative hypotension, hypoproteinemia, and diabetic state; and finally the surgeons’ technique when creating and handling the stomach. Most risk factors can be avoided by careful preoperative preparation, delicate intraoperative manipulations, and postoperative treatment. A previous study reported that patients who have febrile and toxic symptoms for longer than 24 h or those who have coffee/dark drainage should be suspected for gastric necrosis[13]. CT scan can help to identify the necrosis by detecting an ischemic focus or anastomotic breakdown, but the sensitivity is low. Furthermore, endoscopy can help with direct detection of the necrosis and is usually used when there is a clinical suspicion.
Reconstruction of the hypopharyngeal or esophageal circumferential defect after gastric necrosis is a challenging task that influences the postoperative quality of life. It is worth noting that reconstruction should provide an unobstructed conduit without leak and should fulfill the dead space. There are several mature techniques and flaps used in the reconstruction process. Notably, local pedicled flaps were the earliest flaps used in the reconstruction process. They have several advantages including the ease of learning this surgical technique, providing sufficient tissue, and a stable blood supply. However, the donor site can be irradiated at the same time as the primary carcinoma, thereby leading to higher leak or necrosis rate, and excessive bulkiness of the flaps can lead to tracheostoma obstruction. On the other hand, free flaps are widely used in reconstructions involving the development of microvascular surgery, especially the anterolateral thigh free flap and the free jejunal flap. They can achieve adequate donor tissue outside the radiation field, good swallowing function, and little stricture rate. In addition, their cost-effectiveness is acceptable, except for centers that do not obtain microvascular surgery techniques. Several case reports have demonstrated the use of modified free flaps including tube-in-a-tube anterolateral thigh flap, flag-shaped anterolateral thigh free flap, and inverted-omega anterolateral thigh flap[14-16]. Although one study reported that a modified fasciocutaneous radial forearm free flap with two-layer closure achieved less risk of fistula and wound dehiscence[17], relatively high fistulation rates are usually reported when fasciocutaneous radial forearm free flaps are used in circumferential neck defects. Therefore, the flaps are not commonly used nowadays. Advanced hypopharygeal carcinoma treatment usually involves bilateral neck dissection that results in a lack of healthy donor vessels. Studies on combining double free flaps found that it enhanced the complexity of the procedure but did not increase flap-related complications, thereby suggesting that double free flaps is a worthy choice in instances where single free flap cannot close the complex defect[18].
In the first presented case, gastric necrosis was diagnosed with poor general condition. The patient suffered from septic shock caused by the necrosis. Therefore, the operation time was strictly limited for safety purposes. Hence, we only performed debridement and chose exclusion therapy in order to shorten the operation time, since reconstruction with flaps needs more time. Another advantage of the exclusion therapy is that the inflammation subsides and granulation tissue turns fresh after days of dressing changes. It provides a good basement for the next-step reconstruction which reduces the fistula rate. Therefore, both patients in this case report underwent exclusion therapy to drain the necrotic material and purulent exudate in order to provide fresh granulation tissue for next step reconstruction.
The split thickness skin graft is a type of skin flap reserve that only contains the epidermis and a portion of the dermis. It is normally used to cover skin defects or is placed over muscle. It must be put on wound bed with vascularity because it has the special characteristic of no blood supply. The main advantage of split thickness skin graft is that it is easy to harvest with abundant donor sites. Another advantage is that it can be used to cover defect that is greater than the donor skin due to its good epithelialization ability[19]. In the first presented case, necrosis of the posterior wall extended to the gastric wall below the thoracic inlet. We put the split thickness skin on the surface of the granulation tissue, which served as the side wall and posterior wall of the conduit. The epithelialization ability of the split thickness skin made it able to grow along the chest tube that we put through the thoracic inlet, thereby meeting the margin of the healthy gastric wall. In contrast, using a pedicled flap or a free flap would have required a sternotomy to suture the inferior margin with the gastric wall[20], thereby prolonging the operation time and causing more trauma to the patient.
For centuries, local random flap has been an important flap for performing anaplastic surgery. Its main advantage is that its blood supply does not rely on a specific vessel, which ensures that its harvest is not restricted to a certain position. Moreover, compared to pedicled flaps and free flaps, it is easier to harvest and takes less time. However, having no specific blood supply vessel is challenging to surgeons because they must design the flap well and they should carefully confirm the blood supply before and after the reconstruction procedure. In the first case, we used 4 local random flaps to accomplish the two-layer closure of the anterior wall of pharynx and the skin defect. In the second case, we used 6 local random flaps to accomplish the two-layer closure of the anterior wall of pharynx and the skin defect, as well as closure of the upper wall of the tracheostoma, which could hardly be achieved by using a single pedicled flap or a free flap. Therefore, we suggest that reconstruction using well prepared and designed local random flaps can achieve equal results as free flaps. However, it is more advantageous because it requires less operation time, causes less trauma, and requires no microsurgical technique.
To the best of our knowledge, this is the first case report that has reported reconstruction using local random flaps and a split thickness skin graft for cervical circumferential defects extending below the thoracic inlet. In addition, this case report provides a method for the reconstruction of tracheoesophageal fistula with a defect on the upper and posterior walls of the tracheostoma. Therefore, for selected patients, local random flaps (with a split thickness skin graft) can be used as a considerable option for treating the challenging tracheoesophageal fistula or cervical circumferential gastric necrosis, especially when the necrosis extends below the thoracic inlet.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Solaini L S-Editor: Yan JP L-Editor: Filipodia P-Editor: Xing YX
| 1. | Raghavan U, Quraishi S, Bradley PJ. Multiple primary tumors in patients diagnosed with hypopharyngeal cancer. Otolaryngol Head Neck Surg. 2003;128:419-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Huang YC, Lee YC, Tseng PH, Chen TC, Yang TL, Lou PJ, Ko JY, Liao LJ, Hsu WL, Chang YL, Wang CP. Regular screening of esophageal cancer for 248 newly diagnosed hypopharyngeal squamous cell carcinoma by unsedated transnasal esophagogastroduodenoscopy. Oral Oncol. 2016;55:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Nakaminato S, Toriihara A, Makino T, Kawano T, Kishimoto S, Shibuya H. Prevalence of esophageal cancer during the pretreatment of hypopharyngeal cancer patients: routinely performed esophagogastroduodenoscopy and FDG-PET/CT findings. Acta Oncol. 2012;51:645-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Ariyan S. The pectoralis major myocutaneous flap. A versatile flap for reconstruction in the head and neck. Plast Reconstr Surg. 1979;63:73-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 710] [Cited by in RCA: 621] [Article Influence: 13.5] [Reference Citation Analysis (1)] |
| 5. | Demergasso F, Piazza MV. Trapezius myocutaneous flap in reconstructive surgery for head and neck cancer: an original technique. Am J Surg. 1979;138:533-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 116] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Quillen CG. Latissimus dorsi myocutaneous flaps in head and neck reconstruction. Plast Reconstr Surg. 1979;63:664-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 107] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Song YG, Chen GZ, Song YL. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984;37:149-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 967] [Cited by in RCA: 930] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 8. | Seidenberg B, Rosenak SS, Hurwitt ES, Som ML. Immediate reconstruction of the cervical esophagus by a revascularized isolated jejunal segment. Ann Surg. 1959;149:162-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 375] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 9. | Sherman CD Jr, Waterston D. Oesophageal reconstruction in children using intrathoracic colon. Arch Dis Child. 1957;32:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Denewer A, Khater A, Hafez MT, Hussein O, Roshdy S, Shahatto F, Elnahas W, Kotb S, Mowafy K. Pharyngoesophageal reconstruction after resection of hypopharyngeal carcinoma: a new algorithm after analysis of 142 cases. World J Surg Oncol. 2014;12:182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Clark JR, de Almeida J, Gilbert R, Irish J, Brown D, Neligan P, Gullane PJ. Primary and salvage (hypo)pharyngectomy: Analysis and outcome. Head Neck. 2006;28:671-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Briel JW, Tamhankar AP, Hagen JA, DeMeester SR, Johansson J, Choustoulakis E, Peters JH, Bremner CG, DeMeester TR. Prevalence and risk factors for ischemia, leak, and stricture of esophageal anastomosis: gastric pull-up versus colon interposition. J Am Coll Surg. 2004;198:536-41; discussion 541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 256] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 13. | Oezcelik A, Banki F, Ayazi S, Abate E, Zehetner J, Sohn HJ, Hagen JA, DeMeester SR, Lipham JC, Palmer SL, DeMeester TR. Detection of gastric conduit ischemia or anastomotic breakdown after cervical esophagogastrostomy: the use of computed tomography scan versus early endoscopy. Surg Endosc. 2010;24:1948-1951. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Komorowska-Timek E, Lee GK. Tube-in-a-tube anterolateral thigh flap for reconstruction of a complex esophageal and anterior neck defect. Ann Plast Surg. 2014;72:64-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Oh TS, Kwon JG, Jeong WS, Nam SY, Choi SH, Choi JW. A flag-shaped anterolateral thigh free flap for complete circumferential hypopharyngeal reconstruction with dead space obliteration and monitoring flap inset. J Plast Reconstr Aesthet Surg. 2019;72:1785-1794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Scaglioni MF, Lin TS, Chen YC, Tsai YT, Yang CH, Wu CC, Kuo PJ, Hsieh CH, Yang JC. The free inverted omega-shaped flap for circumferential hypopharyngeal reconstruction with simultaneous neck skin defect. Microsurgery. 2018;38:51-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Abu-Serriah M, Loughran S. Modification of fasciocutaneous radial forearm free flap to achieve two-layer closure during reconstruction of circumferential hypopharyngeal defects. Eur Ann Otorhinolaryngol Head Neck Dis. 2018;135:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Stalder MW, Mundinger GS, Bartow M, Pharo A, Patterson C, Sharma S, Aslam R, St Hilaire H. Single Versus Simultaneous Double Free Flaps for Head and Neck Reconstruction: Comparison of Flap Outcomes and Donor-Site Morbidity. Ann Plast Surg. 2019;82:184-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Braza ME, Fahrenkopf MP. Split-Thickness Skin Grafts. 2021 Jul 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. [PubMed] |
| 20. | Granzow JW, Li AI, Boyd JB, Van Natta TL. Use of Dual, Tubularized Supraclavicular Artery Island Flaps in Series to Restore Gastrointestinal Continuity After a Failed Ileocolic Esophageal Reconstruction. Ann Plast Surg. 2015;75:306-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |