Published online Nov 26, 2021. doi: 10.12998/wjcc.v9.i33.10323
Peer-review started: July 6, 2021
First decision: July 26, 2021
Revised: August 1, 2021
Accepted: September 10, 2021
Article in press: September 10, 2021
Published online: November 26, 2021
Processing time: 138 Days and 21.3 Hours
Crab lice (Phthirus pubis) infestation can occur at any age, to either males or females, and across all regions of the world. However, cases involving the eyelashes and adjacent eyelids (phthiriasis palpebrarum) are rare. Usually occurring as a sexually transmitted disease, crab lice can be spread by poor hygiene or in a dirty environment through direct contact with contaminated skin (hands) or textiles (towels and clothing).
A 50-year-old woman presented to our hospital with a 2-wk history of chronic eyelid pain and itching in the right eye, which exacerbated in the evening hours and which had not resolved following a 1-wk course of antibiotics and corticosteroid ointments (for blepharitis diagnosis from another hospital). A careful ophthalmic slit-lamp and light microscope examination revealed multiple crab lice and nits on the right upper eyelashes; the right and left lower eyelashes were normal. Following the new diagnosis of phthiriasis palpebrarum, the patient was treated by removing the affected eyelashes, the crab lice, and their nits completely. Additionally, the eyelids were washed once with povidone-iodine. A follow-up examination at 2 wk later showed complete resolution of symptoms and no evidence of re-infection.
This case emphasizes the importance of correct diagnosis and complete removal of eyelashes, crab lice and nits to cure phthiriasis palpebrarum.
Core Tip: Crab lice (Phthirus pubis) infestation of the eyelids and lashes (phthiriasis palpebrarum), despite manifesting eyelid pain and itching, is easy to miss, even for ophthalmologists, as the lice and nits are translucent. For the case presented here, a light microscope revealed the features of crab lice and nits in unilateral eyelashes and adjacent eyelids. Complete removal of the affected eyelashes, by trimming or plucking, followed by a single povidone-iodine rinse appears to be a simple, safe and effective method of treatment.
- Citation: Tang W, Li QQ. Crab lice infestation in unilateral eyelashes and adjacent eyelids: A case report. World J Clin Cases 2021; 9(33): 10323-10327
- URL: https://www.wjgnet.com/2307-8960/full/v9/i33/10323.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i33.10323
Crab lice (Phthirus pubis) is a hematophagous parasite of humans[1]. Although the infection usually occurs as a sexually transmitted disease, it also can be spread by direct contact with contaminated skin (e.g., hands) or textiles (e.g., towels and clothing)[2]. Crab lice infestation involving the unilateral eyelashes and adjacent eyelids is rare among the overall spectrum of ocular surface diseases[3]. Many studies of such in the literature refer to the crab lice infection of the eyelid as phthiriasis palpebrarum[4-8]. The condition can occur in any decade of life, with case reports describing afflicted individuals ranging in age from 21 d (infant) to 75 years (elderly)[9,10]. Moreover, cases have originated from developing as well as developed countries. Here, we report a case of phthiriasis palpebrarum caused by poor hygiene or dirty environment.
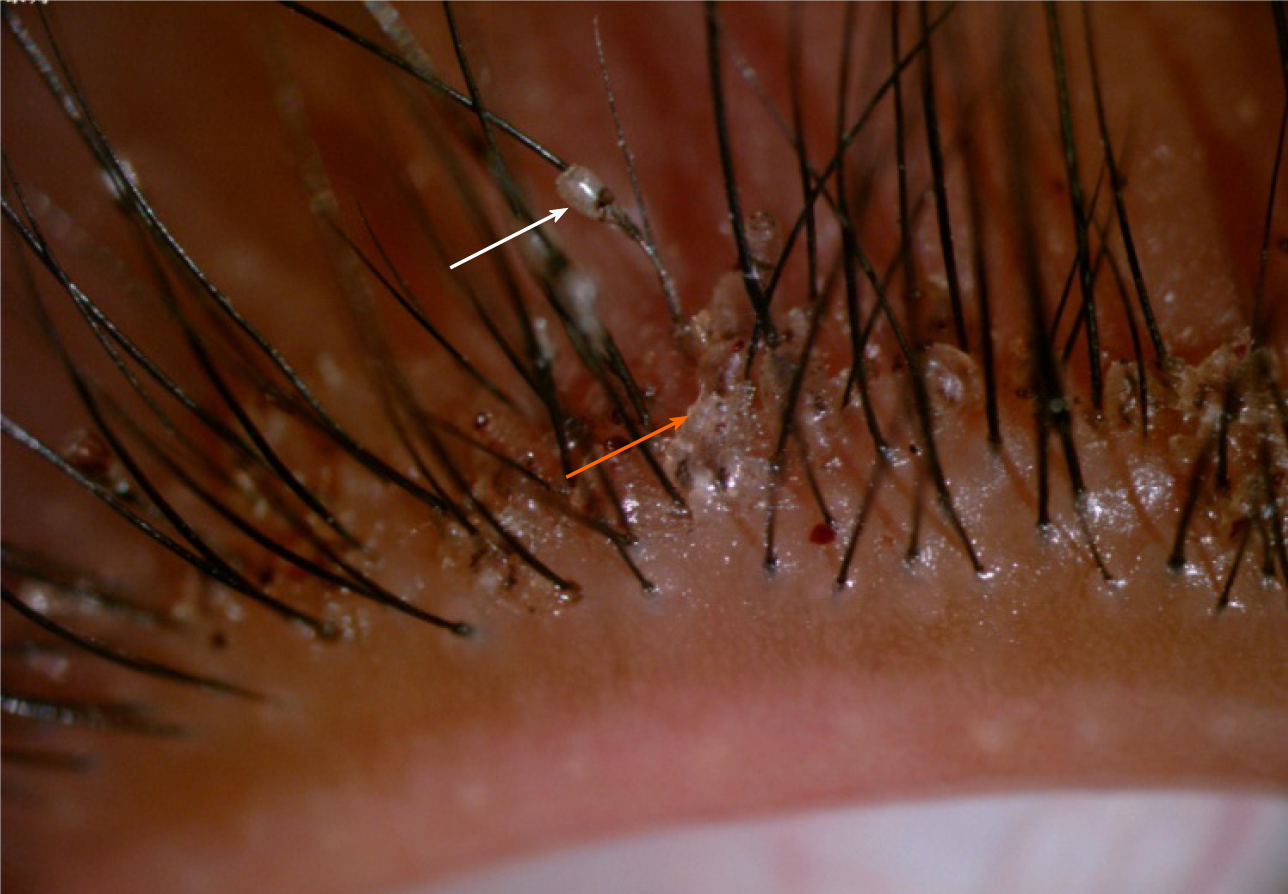
A 50-year-old woman presented at our hospital’s ophthalmology department in October 2019, with a 2-wk history of intermittent right upper eyelid pain and itching (Figure 1), which exacerbated in the evening hours.
The patient reported having previously presented to another hospital with the same complaint of symptoms. There, she had been diagnosed with blepharitis and prescribed a 1-wk course of antibiotics and corticosteroid ointments. When the symptoms did not resolve with treatment, she sought assessment at our hospital.
No relevant information.
Personal and family history-taking revealed no relevant information.
The patient’s best-corrected visual acuity was 20/20, in both eyes. A careful ophthalmic slit-lamp examination was conducted, and showed several parasites adherent to the right upper eyelashes of the right eye. A slight touch of the eyelashes stimulated the parasites to initiate a creeping movement in response (Video). In addition to the parasites, there were empty shells present on the eyelashes (Figure 2).
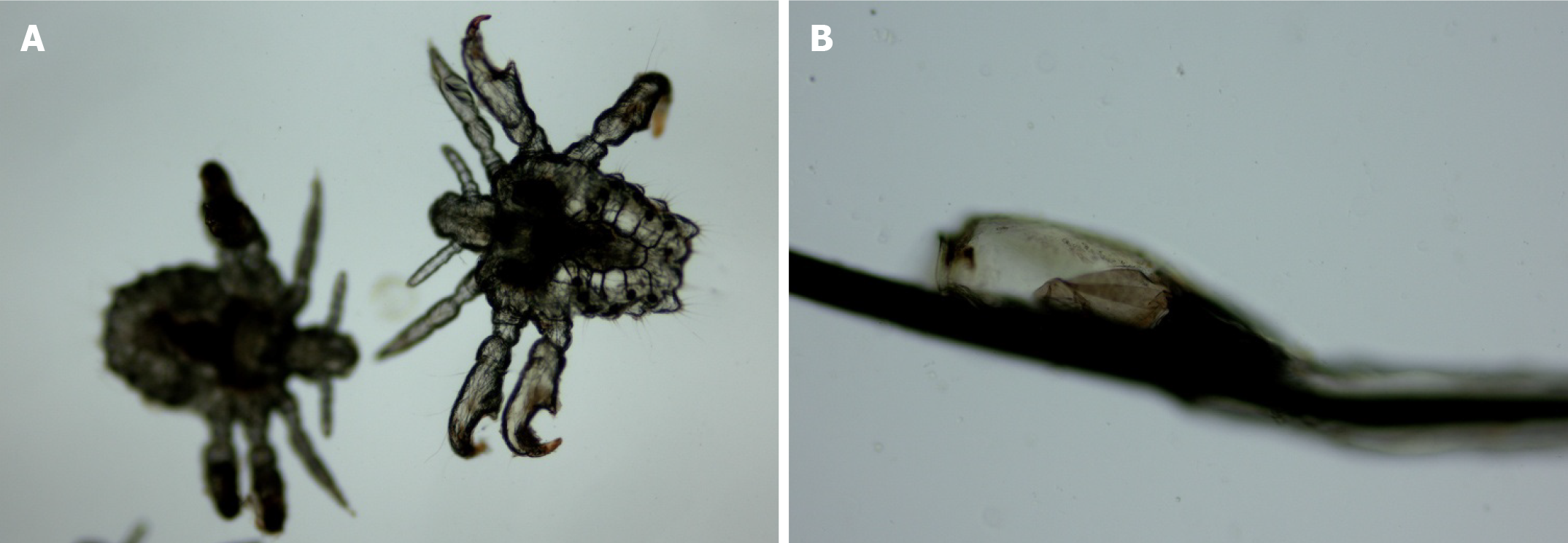
A few of the parasites and empty shells were collected and examined under a light microscope (Figure 3). The gross visual characteristics of both were consistent with crab lice and nits (eggs of the crab lice)[5].
Unilateral (right eye) crab lice infection of the eyelids and eyelashes: Phthiriasis palpebrarum.
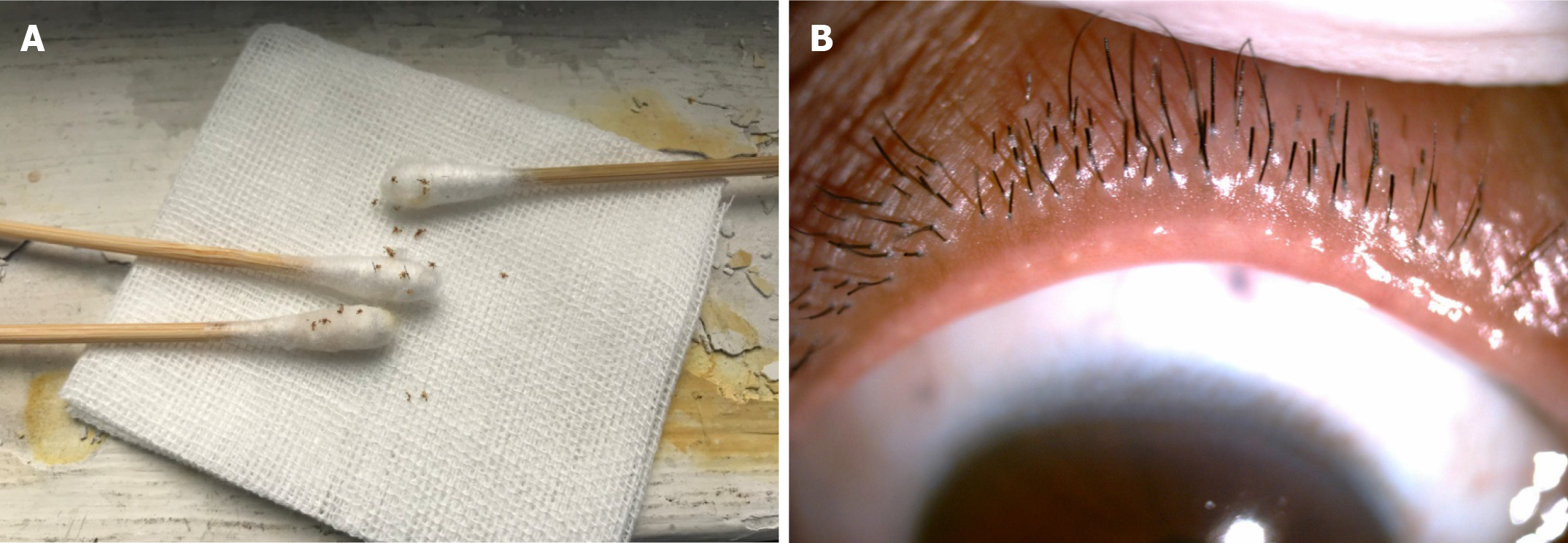
The right upper eyelashes were trimmed to the skin surface or plucked out, to ensure complete removal of the crab lice (Figure 4A) and nits. The eyelids were subsequently washed once with povidone-iodine.
A follow-up examination 2-wk later showed complete resolution of the patient’s eye symptoms and no evidence of re-infection (Figure 4B).
Parasitic eye infection is a rare ocular disease, without geographic, age or sex propensity. In our clinical work, we have come across eye diseases caused by infections with demodicosis (usually inhabiting hair follicles and largely involving those on the head), cysticercosis (primarily infecting brain and muscle), and crab lice (typically as a sexually transmitted disease). The various parasitic infections feature distinctive infection and symptomological profiles. When crab lice invade eyelid skin, their nits can be observed adhering to the eyelashes. Patients afflicted with phthiriasis palpebrarum always present with eyelid pain and itching, which are unfortunately the most common symptoms of all types of eye diseases. In addition, the adult crab lice are translucent, being easy to miss by an ophthalmologist and supporting the misdiagnosis of blepharitis. The parasitic nature of crab lice includes their derivation of nutrients from human blood, via an ex vivo sucking mechanism. The symptoms of itching and pain arise from the biting of the crab lice to penetrate the skin and obtain the blood meal.
There are three transmission mechanisms for crab lice, including sexual, direct and indirect contact. Vulva infestation of crab lice is most commonly transmitted by sexual contact. Eyelid infestation is mainly transmitted by direct or indirect contact with a contaminated source. In our case, the patient had worked as a hotel cleaner for 4 years, and declared no history of sexually transmitted diseases. She could have contracted the disease from contact with contaminated towels and clothing at her worksite. Good hygienic habits, including frequent bathing, hand washing and laundering of textiles (including personal clothing) are important ways to prevent this disease.
There are several topical drug-based treatments currently available for crab lice, namely ivermectin[11,12], pilocarpine drops[13], yellow mercuric oxide, and petro
This case emphasizes the importance of correct diagnosis for crab lice infestation. The mechanical removal of crab lice and nits, in addition to complete trimming or plucking of the affected eyelashes, appears to be a simple, safe and effective method of treatment for crab lice infestation of the eyelids and eyelashes.
The authors express their sincere gratitude to the patient for her cooperation in treatment and permission to share her case through publication.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Șurlin VM S-Editor: Fan JR L-Editor: A P-Editor: Wang LYT
| 1. | Slonka GF. Life cycle and biology of lice. J Sch Health. 1977;47:349-351. [PubMed] [DOI] [Full Text] |
| 2. | Anderson AL, Chaney E. Pubic lice (Pthirus pubis): history, biology and treatment vs. knowledge and beliefs of US college students. Int J Environ Res Public Health. 2009;6:592-600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Baskan C, Duman R, Balci M, Ozdogan S. A rare cause of blepharoconjunctivitis: Phthiriasis palpebrarum. Niger J Clin Pract. 2014;17:817-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Ashkenazi I, Desatnik HR, Abraham FA. Yellow mercuric oxide: a treatment of choice for phthiriasis palpebrarum. Br J Ophthalmol. 1991;75:356-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Droutsas К, Tzanetou К, Kafentzi M, Matemou-Lada E, Droutsas D. Phthiriasis palpebrarum-case report and photo essay. Int J Ophthalmol. 2007;7:618-620. |
| 6. | Wu N, Zhang H, Sun FY. Phthiriasis palpebrarum: A case of eyelash infestation with Pthirus pubis. Exp Ther Med. 2017;13:2000-2002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Lv Y, Xing X, Ma W. A Case of Unilateral Phthiriasis Palpebrarum Infestation. JAMA Ophthalmol. 2019;137:e184503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Dredge JH, Winter TW, Alset AE. Phthiriasis Palpebrarum Treated with Oral Ivermectin. Ophthalmology. 2019;126:791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Ozer PA, Kabatas EU, Gurkan A, Kurtul BE. Treatment of Phthiriasis Palpebrarum Mimicking Conjunctivitis in a Newborn. Indian J Pediatr. 2016;83:730-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Lacarrubba F, Micali G. The not-so-naked eye: phthiriasis palpebrarum. Am J Med. 2013;126:960-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Burkhart CN, Burkhart CG. Oral ivermectin therapy for phthiriasis palpebrum. Arch Ophthalmol. 2000;118:134-135. [PubMed] |
| 12. | Fox LM. Ivermectin: uses and impact 20 years on. Curr Opin Infect Dis. 2006;19:588-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 81] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 13. | Turgut B, Kurt J, Catak O, Demir T. Phthriasis palpebrarum mimicking lid eczema and blepharitis. J Ophthalmol. 2009;2009:803951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Padhi TR, Das S, Sharma S, Rath S, Tripathy D, Panda KG, Basu S, Besirli CG. Ocular parasitoses: A comprehensive review. Surv Ophthalmol. 2017;62:161-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |